The authors conclude that transvaginal hydrolaparoscopy appears to be a safe alternative to hysterosalpingography and laparoscopy for evaluation of tubal patency and pelvic pathology.
Keywords: Transvaginal laparoscopy, Laparoscopy, Hydrolaparoscopy, Chromopertubation, Tubal patency
Abstract
Transvaginal hydrolaparoscopy (THL) is being performed regularly in Europe and China, but rarely in the United States. The reasons may be physicians’ unfamiliarity with the procedure and their uneasiness over potential rectal puncturing due to the proximity of the rectum to the vaginal trocar insertion site. THL has the advantage over hysterosalpingography (HSG) in that it allows for direct visualization of the tubal mucosa in addition to determining tubal patency. THL has advantages over traditional laparoscopy in that it does not require an abdominal incision and has the capability of being conducted in an outpatient office setting with local anesthesia. Studies have shown that THL has comparable accuracy to laparoscopy with 96.1% concordance between THL and laparoscopic findings. THL may be combined with chromopertubation and salpingoscopy. In addition to diagnostic purposes, THL may be used for operative intervention including adhesiolysis, endometriosis ablation, and ovarian drilling. Studies from France and China report the occurrence of rectal injury from 0% to1%. Despite the advantages of THL and low reports of rectal injury, THL has not gained popularity in the United States. The purpose of this article is to familiarize gynecologists in the United States with THL.
INTRODUCTION
Transvaginal hydrolaparoscopy (THL) is an alternative procedure to hysterosalpingography (HSG) and laparoscopy that allows direct visualization of the female peritoneal cavity. THL is more commonly performed in Europe and China than in the United States. In this procedure, a trocar is passed through the vagina into the Pouch of Douglas, and an optic scope is placed through the trocar sleeve, allowing close examination of the uterus, ovaries, fallopian tubes, and peritoneum. No abdominal incision was required, and the procedure can be accomplished in an office setting. THL can also be performed in conjunction with chromopertubation, salpingoscopy, microsalpingoscopy, and hysteroscopy. Dr. Antoine Watrelot from France coined the term “fertiloscopy” for the combination of these procedures.1 In contrast to traditional HSG for evaluation of tubal patency, THL additionally permits direct inspection of the tubal mucosa. Because the vaginal trocar is passed parallel to the axis of the fallopian tubes, the optic scope can more easily enter the tubal lumen, permitting inspection of the inner tubal microarchitecture.2 The operative port on the vaginal trocar also allows insertion of a single operative instrument for adhesiolysis, ablation of endometriosis, and ovarian drilling.
THL was previously described by Dr. Stephan Gordts and later modified by Dr. Watrelot in the 1990s. The Fertiltoscope was developed specifically for the THL procedure and licensed by European Council Directive in 1993.3 Dr. Watrelot subsequently reported over 1500 cases with minimal complications.4 Despite its success in France, Italy, Belgium, and China, THL is seldom performed in the United States, as evidenced by the lack of Medline reports of THL procedures done in this country. This is perhaps due to lack of awareness about the procedure and concern of rectal injury potentially leading to a medical malpractice lawsuit. The purpose of this article is to help familiarize gynecologists in the United States with THL.
Transvaginal Hydrolaparoscopy Technique
Depending on patient and physician preference, the procedure can be done in the operating room or an office setting. A vaginal and rectovaginal examination is performed to evaluate the axis, size, and mobility of the uterus and to evaluate for pelvic masses or pathology in the Pouch of Douglas.4 A speculum is then placed in the vagina. If in an office setting, local anesthesia may be given by rubbing a lidocaine swab on the vaginal mucosa for 10 min followed by a paracervical block of lidocaine.
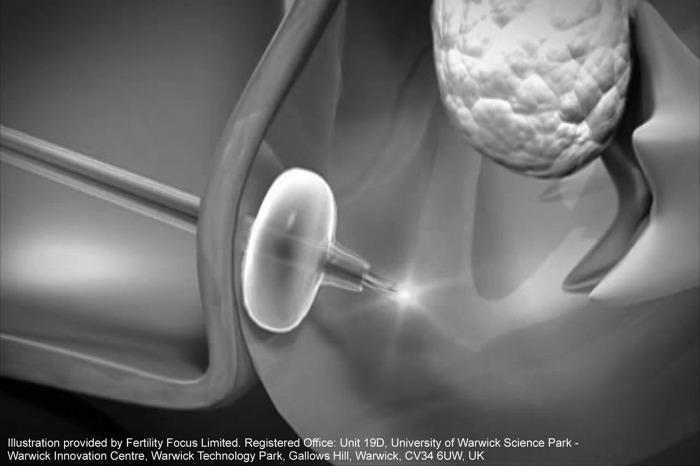
The cervix is grasped at the 8 o’clock position with a tenaculum, and a Veress needle is inserted 1cm below the cervix, allowing entrance into the Pouch of Douglas (Figure 1). To minimize the risk of rectal injury, it is important to insert the Veress needle parallel and above the posterior blade of the speculum, which displaces the rectum inferiorly.
Figure 1.
Balloon tip at the end of the introducer inserted transvaginally into the Pouch of Douglas.
Once the Veress needle is inserted, 150m: to 200mL of saline solution is instilled through it into the peritoneal cavity. The Veress needle is removed, and a 3-mm trocar is inserted through the vagina into the Pouch of Douglas.5 Saline solution exiting from the operative port of the trocar suggests that it has been placed correctly. A 2.9-mm diameter optic scope with a 30° telescope is introduced through the trocar sleeve, and the peritoneal cavity is visualized.6 Pelvic adhesions and endometriosis can easily be seen with the transvaginal optic scope.5 Mild pelvic adhesions and endometriosis may be treated through the transvaginal approach, using the operative port of the vaginal trocar sleeve, while severe adhesions and endometriosis may be better approached laparoscopically through an abdominal incision. Ovarian drilling and peritoneal biopsies for endometriosis can also be performed through the operative vaginal port.7
For evaluation of tubal patency, an additional catheter can be inserted into the uterus for injection of methylene blue dye. The 2.9-mm optic scope is usually small enough to pass into the lumen of the fallopian tubes to perform salpingoscopy and microsalpingoscopy, which specifically analyzes tubal mucosa with the magnified end of the optic scope.8 Studies propose that dye-stained nuclei represent injured cells. If many of them are discovered, it implies substantial tubal mucosa pathology, probably from cellular inflammation or apoptosis.9
Upon evaluation and treatment completion, the trocar sleeve is removed. The vagina is inspected for hemostasis; a suture is rarely needed. In a study of 1589 patients undergoing THL, 0.17% required a vaginal suture for hemostasis.10
The European and Chinese Experience Comparing THL to HSG and Laparoscopy
Previous European and Chinese studies suggest that THL is a viable alternative to traditional HSG for evaluation of tubal patency, as well as laparoscopy for examination of pelvic pathology. An Italian study, conducted in an outpatient office setting, compared usage of THL combined with hysteroscopy and chromopertubation under local anesthesia to HSG.11 Patient pain, procedure duration, and concordance between the 2 procedures in diagnosing tubal and uterine abnormalities were studied. In this investigation, 23 infertile women were randomly placed into 2 groups: those who received THL with hysteroscopy and chromopertubation followed by HSG 7 d later or those who received HSG followed by THL with hysteroscopy and chromopertubation 7 d later. It was found that THL combined with hysteroscopy and chromopertubation lasted a mean of 33 ± 8 min, while the HSG procedure lasted a mean of 13 ± 3 min. More pain was reported from the participants who underwent the HSG procedure than those who underwent THL with hysteroscopy and chromopertubation in an office setting. Regarding accuracy in evaluating tubal patency, a 95.5% concordance resulted between HSG findings and THL with chromopertubation findings. However, when evaluating for uterine abnormalities, only a 43% concordance between the findings of HSG and THL resulted combined with hysteroscopy and chromopertubation, the latter diagnosing uterine disorders more often than HSG alone. For example, several cases of endometrial polyps and endometriosis were undiscovered by HSG, but were detected by THL, hysteroscope, and chromopertubation collectively. So although the combination of THL, hysteroscopy, and chromopertubation takes longer to perform than HSG, its ability to uncover more pelvic abnormalities and decreased reports of postprocedure pain make it a viable alternative for infertility investigation.
Additional studies have compared THL to laparoscopy. In one French study involving 92 infertile patients, the concordance between THL and laparoscopy findings from a pelvic evaluation was analyzed to assess accuracy between the 2 procedures.12 In this particular study, endometriosis was diagnosed visually. The ovaries, tubes, peritoneum, and uterus were evaluated both by THL and laparoscopy for pelvic abnormalities, and their findings demonstrated 96.1% concordance. The κ index ranged from 0.78 (peritoneum) to 0.91 (right tube), with a κ index of 0.61 to 0.80 considered good, and an index of 0.81 to 1.0 considered excellent. This study suggested that due to accuracy of the THL evidenced by the concordance rates and κ index, performing THL could avoid laparoscopy in 93% of females.
A Belgium study13 investigated the accuracy of diagnosing endometriosis and adhesions by THL in comparison to laparoscopy. Two gynecologists performed each procedure in 10 infertile females, and their findings were compared. In this study, endometriosis was diagnosed visually. The findings were a 95% concordance between gynecologists for detecting tubo-ovarian adhesions with THL and 74% concordance between gynecologists with laparoscopy.13 The gynecologists had 63% concordance in detecting ovarian adhesions by THL and 37% by laparoscopy. Due to the high percentage of interobserver agreement seen with THL, the study deduced that its accuracy in discovering pelvic abnormalities, specifically endometriosis and adhesions, was comparable to laparoscopy.
The ability of THL to enter the Pouch of Douglas and clearly visualize and analyze peritoneal structures is noted in several studies. In a French study7 of 160 infertile women without pelvic pathologies, THL successfully entered the Pouch of Douglas in 96.2% of the participants, with a normal peritoneal examination noted in 37.5% of the participants. An immediate follow-up laparoscopy was performed in 32.5% of the cases, and delayed follow-up laparoscopy was performed in 15% of the participants who had THL performed with local anesthesia.7 Endometriosis, post-PID lesions, and mild abnormalities (para-tubal cysts, sacculation, and diverticula) were discovered in 13.1%, 36.2%, and 9.3% of the patients, respectively. A separate study14 performed in China involving 115 infertile women undergoing THL reported that THL was able to enter the Pouch of Douglas 95.7% of the time and assess for abnormalities. They concluded that THL was effective enough to be used as a first-line study to evaluate for pelvic irregularities and that transabdominal laparoscopy ought to be utilized as a supplement if any abnormal findings from THL were present.14 Another French study15 of 229 infertile women found that 88.6% of THL procedures succeeded in entering the Pouch of Douglas. Lesions that required follow-up with laparoscopy were detected in 28.6% of the cases.
The terms culdolaparoscopy and transvaginal laparoscopy describe a similar process to THL in which a laparoscope is inserted through the posterior cul-desac into the peritoneal cavity. The inclusion of “hydro” describes the distention media used in THL. The term culdolaparoscopy has also been described as a procedure in which culdoscopy is combined with abdominal laparoscopy. The author of the culdolaparoscopy report describes first performing abdominal laparoscopy with small 3-mm to 5-mm ports then placing a larger operative port up to 12mm in the posterior vaginal fornix to assist with removal of ovaries, fallopian tubes, and myomas.16 The vaginal port is inserted while the posterior cul-desac is visualized with the abdominal laparoscope. The principle benefit of using the larger vaginal port is that it can be used to facilitate removal of pelvic organs and allow the surgeon to use fewer and smaller abdominal trocars. In contrast to the description of culdolaparoscopy, THL does not incorporate abdominal laparoscopy and can be performed in an office setting.
Risks and Disadvantages
The risks associated with THL range from bleeding to more adverse outcomes, such as rectal puncturing. In a French study10 of 400 patients, the occurrence of rectal injury was 0.5%. In a similar study7 of 160 infertile patients, the reported occurrence of rectal injury was 0.6% and was managed with conservative treatment consisting of prophylactic antibiotics for 2 d following laparoscopic confirmation of peritoneal integrity.7 In the separate French study15 of 229 infertile women undergoing THL mentioned above, 2 occurrences of rectal puncturing reported. In the Chinese study14 of 115 infertile women mentioned earlier, no negative consequences, including rectal puncturing, were noted. Like rectovaginal lacerations and episiotomies that occur with child birth, peritonitis is unlikely if the rectal injury occurs below the level of the peritoneal cavity.10 As stated in previous reports, failure to enter the peritoneal cavity occurred in 0.95% of 1589 THL procedures performed.10
For a surgeon accustomed to performing laparoscopy, adjusting to the viewing angle of THL may be disadvantageous for the initial operations. Upon insertion of the optic scope, the orientation of the structures is reversed from laparoscopy, and the visual field is limited compared to the panoramic presentation of structures by laparoscopy. It has been suggested that it takes a THL novice about 10 procedures to become familiar with the new orientation.4 Also, because of the vaginal approach, adhesions and endometriosis that are beyond the immediate vicinity of the vaginal apex may be difficult to access. Severe pelvic adhesions and severe endometriosis may be better approached laparoscopically.
CONCLUSION
Although transvaginal hydrolaparoscopy (THL) has an extensive history of use in Europe and China, it is rarely—if ever—performed in the United States. A Medline search fails to reveal any reports documenting THL performed in the United States. This is probably because of lack of knowledge and experience with THL in the country. It may also be due to concern about rectal injury during vaginal trocar insertion, owing to the close proximity of the rectum to the vagina, and subsequent fear of medical malpractice litigation that is more common in the United States. In a European study10 of 400 patients undergoing THL, the occurrence of rectal puncture was only 0.5%. The 2 incidences of rectal injury in this study were treated conservatively without complications. In a separate study14 performed in China involving 115 patients, no reports of rectal penetration were made.
THL has the advantage of not requiring an abdominal incision, thus perhaps being more cosmetically appealing to patients. Also, in contrast to traditional HSG for evaluation of tubal patency, THL is favorable in that it allows direct examination of the tubal mucosa, because the axis of optic scope insertion through the vagina permits easy access for salpingoscopy. Lysis of adhesions, ablation of endometriosis, and ovarian drilling also can be performed using the transvaginal approach. Patients with extensive adhesions and endometriosis are probably better served by a laparoscopic approach that permits insertion of more than one operative instrument at a time. THL also may be combined with hysteroscopy. Dr. Watrelot coined the term “fertiloscopy” as the combination of chromopertubation, salpingoscopy, microsalpingoscopy, and hysteroscopy with THL.1
THL can be performed in an outpatient office setting. In an Italian study of 23 patients, more pain was reported from the participants who underwent the HSG procedure than those who underwent THL with hysteroscopy and chromopertubation in an office environment.11 The concordance between laparoscopy and THL in detecting pelvic abnormalities has been reported as 96.1%.12
CONCLUSION
Based on the European and Chinese experience, THL appears to be a relatively safe alternative to HSG and laparoscopy for evaluation of tubal patency and pelvic pathology.
Footnotes
Norgenix, the distributor of the trocar used for transvaginal laparoscopy, paid for travel to France to learn the procedure, which is not well known in the United States. No funds were received, no financial incentive was given to prepare this manuscript, and no support was received from any other source.
Contributor Information
N. Adaobi Ezedinma, School of Medicine, University of Texas Medical Branch, Galveston, TX, USA..
John Y. Phelps, Department of Obstetrics & Gynecology, Division of Reproductive Endocrinology and Infertility, University of Texas Medical Branch, Galveston, TX, USA..
References:
- 1. Brosens I, Campo R, Gordts S. Office hydrolaparoscopy for the diagnosis of endometriosis and tubal infertility. Curr Opin Obstet Gynecol. 11: 371–377, 1999. August Review [DOI] [PubMed] [Google Scholar]
- 2. Transvaginal hydrolaparoscopy for infertility investigation and diagnosis of chronic pelvic pain [OBGYN.net website]. Available at: http://www.obgyn.net/women/□women.asp?page=/hysteroscopy/articles/gortz_int Accessed February 28, 2011
- 3.Fertility Focus. Fertiloscope™- Primary Screening for Infertility [flier]. Fertility Focus, Ltd. [Accessed February 28, 2011]. Available at: http://www.fertility-focus.com/images/product/Fertiloscope□%202%20page%20flyer%20-%20Sep%202008%20V8.pdf.
- 4. Watrelot A. Place of transvaginal fertiloscopy in the management of tubal factor disease. Reprod Biomed Online. 2007. March; 35(3): 281–281 Epub 2007 Feb 23. French [DOI] [PubMed] [Google Scholar]
- 5. Gordts S, Campo R, Rombauts L, et al. Transvaginal hydrolaparoscopy as an outpatient procedure for infertility investigation. Hum Reprod. 1998. January; 13(1): 99–103 [DOI] [PubMed] [Google Scholar]
- 6. Watrelot A, Dreyfus JM, Andine JP. Fertiloscopy: anatomo-technical basis and indications. Ref Gynecol Obstet. 1999; 6: 47–52 [Google Scholar]
- 7. Watrelot A, Dreyfus JM, Andine JP. Evaluation of the performance of fertiloscopy in 160 consecutive infertile patients with no obvious pathology. Hum Reprod. 14: 707–711, 1999. March [DOI] [PubMed] [Google Scholar]
- 8. Papaioannou S, Afnan M, Jafettas J. Tubal assessment tests: still have not found what we are looking for. Reprod Biomed Online. 15(4): 376–82, 2007. October Review [DOI] [PubMed] [Google Scholar]
- 9. Marconi G, Quintana R. Methylene blue dyeing of cellular nuclei during salpingoscopy, a new in-vivo method to evaluate vitality of tubal epithelium. Hum Reprod. 13(12): 3414–3417, 1998. December [DOI] [PubMed] [Google Scholar]
- 10. James M. Synopsis of adverse events when using the fertiloscope. Fertility Focus, Ltd; September 2008. http://www.fertility-focus.com/images/memberstuff/SYNOPSIS.pdf Accessed February 28, 2011
- 11. Cicinelli E, Matteo M, Causio F, et al. Tolerability of the mini-panendoscopic approach (transvaginal hydrolaparoscopy and minihysteroscopy) versus hysterosalpingography in an outpatient infertility investigation. Fertil Steril. 76(5): 1048–1051, 2001. November [DOI] [PubMed] [Google Scholar]
- 12. Watrelot A, Nisolle M, Chelli H, et al. ; International Group for Fertiloscopy Evaluation Is laparoscopy still the gold standard in infertility assessment? A comparison of fertiloscopy versus laparoscopy in infertility. Results of an international multicentre prospective trial: the ‘FLY’ (Fertiloscopy-LaparoscopY) study. Hum Reprod. 18(4): 834–839, 2003. April [DOI] [PubMed] [Google Scholar]
- 13. Campo R, Gordts S, Rombauts L, et al. Diagnostic accuracy of transvaginal hydrolaparoscopy in infertility. Fertil Steril. 1999. June; 71(6): 1157–1160 [DOI] [PubMed] [Google Scholar]
- 14. Hu XL, Xu HL, Wang DN, et al. Application of fertiloscopy in infertile women. Zhonghua Fu Chan Ke Za Zhi. 2005. December; 40(12): 840–843 Chinese [PubMed] [Google Scholar]
- 15. Nohuz E, Pouly JL, Bolandard F, et al. Fertiloscopy: Clermont-Ferrand's experiment. Gynecol Obstet Fertil. 2006. October; 34(10): 894–9 Epub 2006 Sep 18. French [DOI] [PubMed] [Google Scholar]
- 16. Tsin D. Culdolaparoscopy: a preliminary report. JSLS. 5(1): 69–71, 2001. Jan-Mar [PMC free article] [PubMed] [Google Scholar]