Laparoscopic ventral hernia repair with carboxymethylcellulose-sodium hyaluronate coating appears to be safe, effective, and durable.
Keywords: Incisional hernia, Laparoscopic ventral hernia repair, Laparoscopic surgery, Mesh, Polypropylene, SEPRAMESH, Ventral hernia
Abstract
Background:
Repair of ventral hernias, including primary ventral hernias and incisional ventral hernias, is performed in the United States 90,000 times per year. Open or traditional ventral hernia repairs involve the significant morbidity and expense of a laparotomy and a significant risk of recurrent herniation. Laparoscopic ventral hernia repair (LVHR) may offer a less-invasive alternative with shorter length of hospital stay, fewer cardiopulmonary complications, and low recurrence rates.
Methods:
225 patients underwent laparoscopic ventral hernia repairs in which carboxymethylcellulose-sodium hyaluronate coating (Sepramesh, Davol, Providence, RI) was used primarily. All cases were included prospectively from the study period of 2002 through 2009. Patient characteristics were recorded, and follow-up analysis was performed over a period of 42 mo following surgery. Recurrence, reoperations, and all complications were recorded. Mesh awareness and mesh-related pain were assessed using the hernia-specific Carolinas Comfort Scale (CCS) instrument, completed by 72 patients.
Results:
Over 42 mo of follow-up, 2 ventral hernias have recurred, and no long-term bowel erosion or fistulization has occurred. Little or no mesh-related symptoms were reported, and mean scores for mesh awareness and mesh pain were 3.6 and 3.2, respectively, on a scale from 0–40 (lower scores signify less pain or awareness). Two serious early complications occurred related to intestinal ileus and metal tacks producing intestinal perforation, and this led to a change in the tacking devices used.
Conclusions:
LVHR with carboxymethylcellulose-sodium hyaluronate coating (Sepramesh) is safe and effective. Complications are rare, the repair is durable, and long-term results are good with rare recurrences, low awareness of mesh, and little pain. Technical lessons include use of at least one transfascial suture and the avoidance of metal tacks for fixation.
INTRODUCTION
Many ventral hernia repair methods have been described. Repair of ventral hernias is performed in the United States with a reported frequency of 90,000 procedures per year, including primary ventral hernias and incisional ventral hernias. Incisional ventral hernias occur after 3% to 20% of all laparotomies.1–3 A traditional repair involved a laparotomy with primary closure of the fascial defect. Recurrence rates after open primary closures are high, ranging from 41% to 52% during long-term follow-up.4 Ventral hernia repairs with implantation of mesh have also required laparotomy and extensive dissection but appear to result in lower recurrence rates in the range of 12% to 24%.4 Open or traditional ventral hernia repairs involve the significant morbidity of a laparotomy, significant expense associated with laparotomy, and a significant risk of recurrent herniation.
LVHR was first reported in 1993.5 Numerous studies have supported a belief that LVHR may offer a less-invasive alternative with shorter length of hospital stay, fewer cardiopulmonary complications, and low recurrence rates.2,4,6–8 The LVHR most commonly involves placement of a mesh material in the intraperitoneal position. The concern of visceral adhesion and erosion has been a reason cited for cautious adoption of these techniques.3,4,8,9 The development of dual or bilaminar mesh materials has led many surgeons to consider more liberal and frequent placement of mesh in the intraperitoneal position. It is believed that the veneer facing the viscera is safer and less likely to create opportunity for erosion or fistulization.4,10,11
Animal study evaluation of multiple mesh materials indicates that polypropylene with Sepramesh, and polyester with collagen-polyethylene glycol-glycerol coated (Parietex Composite, Covidien, Mansfield, MA) minimize adhesion formation and maximize mesh incorporate and tensile strength for incisional hernia repairs.4,12–14
This study reports the 42-month follow-up of 225 cases of LVHR, 196 of which were performed using Sepramesh, by a single surgeon. It is believed to be the first study reporting the safety, efficacy, and complications for this frequently used dual mesh material in laparoscopic ventral hernia repairs with follow-up beyond 3 years.
METHODS
Between 2002 and 2009, 225 patients underwent laparoscopic ventral hernia repairs with mesh implantation while under general anesthesia. Of these 225 patients, 196 had placement of Sepramesh. All patient data for LVHR were collected prospectively and reviewed retrospectively from the medical records. The data included the patient's age, sex, body mass index (BMI), surgical history, prior repairs, comorbid conditions, and follow-up evaluations, all depicted in Tables 1 and 2. Twenty-eight percent of the cases represented recurrences of previously performed ventral/incisional hernias. Fifty-four percent of cases represented incisional hernias. No conversions to open surgery were necessary (Table 1).
Table 1.
Initial data: Demographics and Hernia Characteristics
| Female/Male | 139/86 |
| Mean Age | 56.90 (±SD 13.86; Range, 20 to 86) |
| Mean Weight | 215.81 (±SD 61.73; Range, 99.40 to 463.00) |
| Mean BMI | 33.10 (±SD 9.30; Range, 18.00 to 68.40) |
| Previous hernia repairs | 28% |
| Incisional Hernias | 54% |
Table 2.
Patient Comorbid Conditions
| Condition/Disease | N | % |
|---|---|---|
| Asthma | 13 | 5.78 |
| Back pain/ DJD | 26 | 11.56 |
| Depression | 20 | 8.89 |
| Diabetes | 21 | 9.33 |
| Cancer (all types) | 14 | 6.22 |
| GERD | 19 | 8.44 |
| Heart Disease | 6 | 2.67 |
| High Cholesterol | 44 | 19.56 |
| Hypertension | 61 | 27.11 |
| Hypothyroidism | 11 | 9.89 |
| Sleep Apnea | 14 | 6.22 |
| Overweight (BMI 25–29.9) | 41 | 18.22 |
| Obese (BMI ≥30) | 105 | 46.67 |
| Urinary Stress Incontinence | 11 | 4.89 |
Laparoscopic Ventral Hernia Repair Technique
Our patients were assessed preoperatively and counseled as to the surgical options. Operative repair was performed with the patient in the supine position. Antibiotic prophylaxis was given in the form of cefazolin, 1 or 2 g IV within 60 min of cut time. Pneumoperitoneum was established with a Veress needle in over 90% of cases with the Veress needle placed remotely from the site of previous surgery or hernia, usually in the left upper lateral subcostal position angling the needle away from the location of the spleen. Bladeless trocars were placed in the extreme lateral position through the abdominal wall, on the side opposite the dominant bulge of the hernia. In most cases, two 5-mm bladeless trocars and a single 12-mm bladeless trocar were used.
Adhesiolysis was then performed to provide a full, clean exposure of the entire peritoneal surface of the anterior abdominal wall. A typical abdominal wall appearance is that of a dominant incisional hernia that is often accompanied by adjacent smaller hernias (Figure 1). This is accomplished sharply, normally with the use of endoscopic scissors and cautery. Frequently, omentum and intestine were adherent or incarcerated within the hernia site. Clips were used to occlude any vessels in the omentum that might be prone to bleeding during and after this resection. The abdominal wall is then ready for hernia repair (Figure 2).
Figure 1.
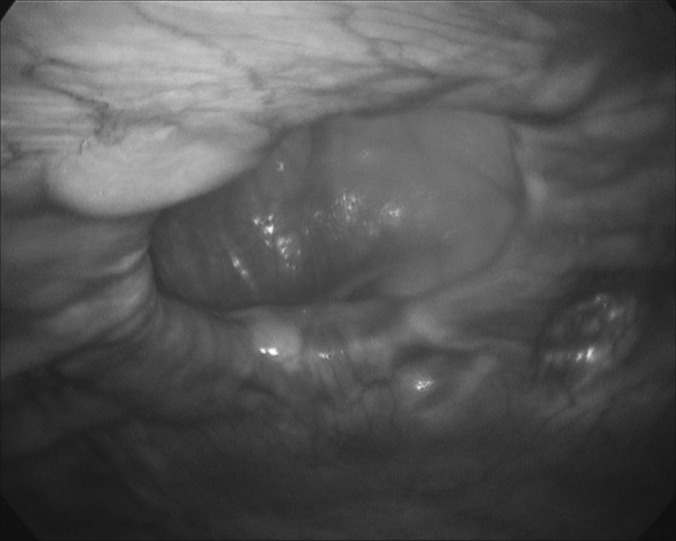
•••
Figure 2.

•••
In the first 54 cases, no anchoring permanent sutures were utilized to secure the mesh to the fascia. In all subsequent cases, at least one permanent transfascial suture was used to anchor the mesh to the fascia. This technique was performed by placing the 0-Prolene, 0-Ethibond, or comparable permanent suture through the mesh at the desired position and making a corresponding skin incision on the abdominal wall, normally at the superior aspect of the fascial edge, at the midline of the hernia. The mesh was then soaked in antibiotic solution, rolled into a tight cylinder and introduced into the peritoneal cavity via the 12-mm trocar.
The mesh material was then unfurled within the abdomen and oriented such that the polypropylene layer would lie against the abdominal wall to incorporate, and the Sepramesh would lie toward the viscera and omentum, to minimize adhesion formation. The ends of the Prolene suture were then retrieved using an Endoclose device via the abdominal wall anterior incision, and the Prolene then secured the mesh and centered it over the hernia and fixed it to the abdominal wall. The suture was then tied down externally and the overlying skin closed with a 4–0 Vicryl suture.
The mesh was then further secured to the anterior abdominal wall with the use of the Protac device, which deployed a corkscrew type metallic fixator to the abdominal wall. In the first 128 cases, 68 involved use of a metallic Protac device. After case #128 at which time a second postoperative bowel perforation occurred at a tack site, we switched to the AbsorbaTack device (Covidien, Mansfield, MA) exclusively. Tacks were secured with counter palpation along the external abdominal wall with numerous tacks placed on all aspects of the Sepramesh. The mesh is overlapped beyond the fascial edges by 3cm to 4cm in all directions.
After final inspections and confirmation of hemostasis, the pneumoperitoneum was evacuated. Ten-mm or 12-mm trocar sites in the upper abdomen were not routinely closed, and the 10-mm or 12-mm trocar sites in the lower abdomen were closed at the fascial level with 0-Vicryl suture. No drains were used. The skin sites were closed with 4–0 Vicryl absorbable suture.
The CCS was administered to all patients available for follow-up by personal visit or telephone interview. The scale measured how satisfied the patients were with their mesh hernia repair. Follow-up after LVHR was 71% of the 225 subjects; 72 patients (32%) completed the hernia-specific CCS during the study period. The CCS score is derived by adding the scores from each of the 23 items. The best possible score is 0 and the worst possible score is 115 depicted in Table 3.
Table 3.
Scale reliability of the Carolinas Comfort Scalea
| Domain | Mean Score /Standard Deviation | Content |
|---|---|---|
| Laying down | 0.417/1.097 | Sensation of mesh |
| 0.444/1.232 | Pain | |
| Bending over | 0.500/1.126 | Sensation of mesh |
| 0.431/1.124 | Pain | |
| 0.375/1.106 | Movement limitations | |
| Sitting | 0.347/1.140 | Sensation of mesh |
| 0.361/1.130 | Pain | |
| 0.306/1.070 | Movement limitations | |
| Activities of daily living | 0.569/1.254 | Sensation of mesh |
| 0.444/1.209 | Pain | |
| 0.333/1.151 | Movement limitations | |
| Coughing or deep breathing | 0.403/1.195 | Sensation of mesh |
| 0.389/1.181 | Pain | |
| 0.333/1.163 | Movement limitations | |
| Walking | 0.403/1.171 | Sensation of mesh |
| 0.319/1.124 | Pain | |
| 0.282/1.111 | Movement limitations | |
| Stairs | 0.417/1.172 | Sensation of mesh |
| 0.361/1.154 | Pain | |
| 0.264/1.100 | Movement limitations | |
| Exercise | 0.556/1.299 | Sensation of mesh |
| 0.444/1.277 | Pain | |
| 0.347/1.235 | Movement limitations | |
| Universal | 0.432/0.104 | Sensation of mesh |
| 0.399/0.049 | Pain | |
| 0.333/0.044 | Movement limitations |
The CCS score is derived by adding the scores from each of the 23 items. The best possible score is 0, and the worst possible score is 115.
RESULTS
There were 86 men and 139 women. The average age was 57. The mean BMI was 33kg/m2 depicted in Table 1. The LVHR was performed in each case. There were no conversions to open surgery. There were no intraoperative or anesthetic complications. In several cases, serosal injuries occurred to bowel during the adhesiolysis. These were often oversewn or imbricated using intracorporeal sutures. No enterotomies occurred. The most frequent size of mesh chosen was 6 inches by 8 inches (Table 4). This was often trimmed for shape and size somewhat. In nearly all patients, a single piece of mesh was used to cover the defect, but in 6 cases, more than one piece of mesh was required. In these 6 cases, the second piece was serially introduced and then secured in the same fashion using a second Prolene suture and more tacks. Mean operative time was 41 min (Table 5). All patients were given an elastic abdominal binder postoperatively and encouraged to wear it.
Table 4.
Mesh Size
| Size of Mesh (Inches) | Percent (%) |
|---|---|
| 3*6 | 7.32 |
| 4*8 | 19.51 |
| 6*8 | 47.15 |
| 8*12 | 23.58 |
| 10*20 | 1.63 |
| 15*15 | 0.81 |
Table 5.
Operative and Postoperative Characteristics
| Length of Stay ≤24 Hr | 78.00% |
| Length of Stay ≥24 Hr | 22.00% |
| ≤30 Day Complication Rate | 4.00% |
| ≤30 Day Readmission | 0.89% |
| ≤30 Day Mortality Rate | 0.89% (Patient #1. Bowel perforation, Patient # 2. Choledocholithiasis) |
| Mean Operation Time | 41 minutes |
Median follow-up time was 42 months. Three patients were re-explored for unrelated reasons during the follow-up period. Two patients who were later re-explored exhibited significant adhesions to the mesh that were separable with the laparoscopic technique. One patient exhibited no adhesions whatsoever to the mesh at laparoscopic reoperation.
Thirty-four patients experienced postoperative seroma and reactive erythema or cellulitis treated with oral antibiotics. Two such cases occurred among the first 10 cases and advanced to severe cellulitis. Fourteen patients (6.22%) experienced postoperative ileus requiring hospital stay >48 hours (Table 6). Hospital stay was <24 hours for 78% of patients, and the median length of stay was 16 hours (Table 5). Two patients (0.89%) experienced recurrence of a ventral hernia during the follow-up period (Table 6).
Table 6.
Postoperative Complication
| Postoperative Complication | Percent (%) |
|---|---|
| Abdominal Wall Cellulitis or Reactive Erythema (Treated with antibiotics only) | 15.11 |
| Delayed Bowel Perforation | 0.89 |
| Large Seroma with Skin & Soft Tissue Necrosis | 0.44 |
| Prolonged Ileus | 6.22 |
| Recurrent Hernia | 0.89 |
| Seroma | 1.78 |
| Urinary Retention | 2.22 |
Two patients (0.89%) died within 30 d of LVHR surgery (Table 5), one of which was related to the procedure. This patient experienced early postoperative bowel obstruction and dilatation, followed by perforation where the metal tack in the abdominal wall penetrated the jejunum. The other died 3 wk after surgery of unrelated causes stemming from choledocholithiasis and complications of an endoscopic retrograde cholangiopancreatography (ERCP).
Two patients (one with Sepramesh and the other with Compsix mesh) experienced serious complications of a bowel perforation related to exposed metal tacks perforating dilated bowel in the early postoperative state. One of these led to peritonitis and eventual death, and the other was resolved with reoperation.
Follow-up after LVHR was 71%, and 32% of patients completed the hernia-specific CCS. On a scale from 0 to 40, mean reported score for “Sensation” was 3.6, and mean score for “Pain” was 3.2, indicating a low level of awareness or discomfort from the mesh (Table 7).
Table 7.
Mean scores of Carolinas Comfort Scale for Sensation, Pain, and Movement
| Pain | Movement | Sensation | |
|---|---|---|---|
| Count | 72 | 72 | 72 |
| Mean Score | 3.194 | 2.208 | 3.597 |
| Standard deviation | 8.974 | 7.605 | 8.852 |
| Min | 0 | 0 | 0 |
| Max | 40 | 35 | 40 |
| Dissatisfied Patients (%): Sensation/Pain/Movement | 9.7 | 6.9 | 9.7 |
DISCUSSION
Despite an average BMI of 33, and a series that includes 54% incisional hernias and 28% recurrent ventral hernias, 78% of the patients in this series left the hospital in <24 h after their procedure. In over 3 y of follow-up, no long-term erosion or fistulization has occurred, and the hernia recurrence rate has been slightly less than 1%. Among the 72 patients who completed the CCS survey, 90.3% reported little to no awareness or pain from the mesh.
One super morbidly obese patient developed a seroma in the region of the hernia sac following reduction of a large wad of chronically incarcerated omentum and placement of Sepramesh. The patient went on to develop necrosis of the paper-thin overlying skin and subcutaneous tissue that required debridement. The resulting exposed naked mesh was treated with wound packing and eventually with a wound vacuum-assisted closure (V.A.C., Wake Forest Baptist Health, Winston-Salem, NC) device. This granulated over a period of 12 wk and required no further medical or surgical intervention, and has resulted in an effective repair of the hernia.
Two patients died within 30 d of surgery. One patient who was discharged home on postoperative Day #2 developed a delayed intestinal perforation and sepsis. At reoperation, the patient was found to have an intestinal injury at the site of an exposed metallic tack from the laparoscopic metal tacking device. The patient had experienced ileus and intestinal distention, leading to direct contact with this exposed tack, and subsequent bowel perforation. The patient had chronic obstructive pulmonary disease (COPD) and an advance directive limiting prolonged care and life support, and the patient died after support was withdrawn. The second patient who died within 30 d after laparoscopic incisional hernia repair was readmitted 20 d after discharge with choledocholithiasis and died from complications of an ERCP procedure, unrelated to the hernia repair surgery.
In sum, 2 patients experienced a serious complication related to LVHR with mesh. Both patients suffered a delayed intestinal perforation at the site of one of the metal tacks used to secure the mesh. In both cases, the metal tacks were exposed, likely due to incomplete tissue purchase. Both experienced a significant postoperative ileus and had distended bowel that lead to direct contact with the sharp metallic tacks. In both cases, laparotomy was performed and a washout and enterotomy repair or resection was performed. In one case, the patient recovered uneventfully, but in the other case described above, a patient with serious comorbid conditions and COPD, support was withdrawn and the patient died.
Many patients exhibit a reactive erythema or cellulitis over the abdominal wall in the area where the mesh was implanted. This has always responded to oral antibiotic therapy with either a first-generation cephalosporin or oral quinolone therapy. Because of 2 early severe cases, and because this erythema or cellulitis is so frequent following this technique, a 1-wk postsurgical antibiotic course has become a part of our current protocol. Introduction of this protocol has eliminated the cellulitis that is otherwise frequently seen in the postoperative period. This remains a subject of evaluation in our center.
Hernia recurrence after laparoscopic repair was rare in this series. The laparoscopic repair technique affords a unique view of the hernia defect and often allows for recognition of additional adjacent fascial defects (Figure 2). This added visualization, in addition to the wide overlap of mesh beyond the fascial edges, results in a low recurrence rate.
Our experience from this study has lead to a change away from the metal tacking device for laparoscopic ventral hernia repairs. In this series, 2 patients developed a serious complication related to surgery and these specific tacks. Since changing to an absorbable tacking device without sharp exposed metal, no further bowel injuries or serious complications have occurred.
Two patients developed recurrent hernias in this series in 48 mo of follow-up. Both cases involved laparoscopic mesh repairs without transfascial anchoring abdominal wall sutures. Further supporting the concept that abdominal wall fixation sutures are necessary, others have noted that the spiral tacks are 4-mm long. Depending on the thickness of the mesh used and the angle at which the tacks are placed, it can be expected that only ≤2 mm of abdominal wall tissue will be penetrated by the tack. Abdominal sutures are believed to have higher tensile strength.
Other authors have also commented on the necessity of abdominal wall sutures.6,15 Our technique has evolved over time to now include placement of at least one transfascial suture to anchor the mesh and place it with optimal orientation and fascial overlap. Larger hernias warrant more transfascial sutures in our opinion.
Intestinal erosion or fistulization has been reported with polypropylene and polyester mesh materials.3,4,8,16 Multiple mesh materials have been devised in an effort to reduce intestinal fistulization. These include an expanded polytetrafluoroethylene Goretex Duel Mesh (ePTFE, Flagstaff, AZ) material with one smooth side serving as an adhesion barrier that is oriented toward the viscera. One material combines the ePTFE layer with a polypropylene layer (Composix, Bard Inc.). Sepramesh combines a Seprafilm layer on a polypropylene base. Animal studies suggest more intestinal adhesions but no greater abdominal wall in growth with polypropylene-based meshes than with purely ePTFE materials.4,14,17,18
In this study of 225 patients, 2 early bowel injuries occurred related to a phenomenon of intestinal ileus followed by perforation from contact with a sharp metal tack. No erosion or fistulization has occurred over 42 mo of follow-up with any of the other patients in the study.
Long-term risk of erosion from intraperitoneal placement of mesh remains a potential concern, and future studies will determine if the bilaminar mesh materials such as Sepramesh do effectively discourage the type of adhesions from the viscera to the mesh that could lead to fistulization over a longer time period.
Mesh awareness and pain have been reported in previous studies of ventral hernia repairs.15 Because the polypropylene mesh matrix is a permanent material forever present and affixed to the peritoneum, it is reasonable to expect some long-term mesh awareness. On the CCS instrument, 9.7% (7 people) reported a score of >10, indicating that 90.3% of patients (65 people) experienced neither awareness nor pain (Table 7).
CONCLUSIONS
Laparoscopic ventral incisional hernia repair using polypropylene with Sepramesh is a safe, effective, and durable technique. Follow-up past 3 y indicates a durable repair with rare hernia recurrences and very low pain sensation. Re-exploration in 3 patients shows variable adhesions to the mesh, with 1 patient exhibiting no adhesions and 2 exhibiting adhesions that allowed laparoscopic adhesiolysis. The 2 episodes of bowel perforation due to the metal tacker device in the setting of postoperative ileus and bowel distention has led us to change away from this metal device to lower profile absorbable tacker device.
Follow-up has taken place over an average of 3.4 y. In the follow-up period, 2 of the ventral hernias recurred and were rerepaired with a laparoscopic ventral hernia technique. These recurrences happened among the first 50 cases and did not involve any transfascial sutures. The mesh appeared to have slid or migrated exposing the fascial defect and leading to a recurrence. The subsequent repair was successful.
During the follow-up period, 3 patients were re-explored in a delayed fashion more than 1 y after surgery. One of these with the recurrent hernia mentioned above and 2 were for unrelated reasons. In 2 of the cases, adhesions were present to the anterior abdominal wall. These were reducible with laparoscopic adhesiolysis techniques. The adherent omentum and viscera peeled away from the mesh relatively easily. In the third case, no adhesions were present to the anterior abdominal wall except for one thin single band.
Incisional hernia is the most long-term common complication of a laparotomy. LVHR has emerged as an effective technique with a short hospital stay, low recurrence rate, and low complication rate. Lessons learned from this longitudinal experience are that the procedure can be safe and effective with durable long-term results and little long-term pain or awareness of the mesh. In addition, technical lessons learned include avoidance of metallic tacks, use of at least one transfascial anchoring suture, and liberal use of postoperative oral antibiotics for overlying cellulitis.
Mesh awareness or mesh-related pain appears to represent a minimal concern at 42 months of follow-up. This compares favorably to other reports of mesh awareness or pain from traditional repair techniques.19–21 In addition, mesh erosion or fistulization over time appears to be nonexistent with Sepramesh in this time frame.
Weaknesses of this study include its case-series methodology, which precludes a control arm or trial format. While our community of Northern Nevada is a small one and generally results in a high degree of knowledge of long-term complications among former patients, the possible bias introduced by those patients lost to follow-up is always a concern. Longer term reporting will be necessary to address the long-term rate of hernia recurrence and fistulization.
References:
- 1. Cobb WS, Kercher KW, Heniford BT. Laparoscopic repair of incisional hernias. Surg Clin North A. 2005; 85 (1): 91–103 [DOI] [PubMed] [Google Scholar]
- 2. DeMaria EJ, Moss JM, Sugerman HJ. Laparoscopic intraperitoneal polytetrafluoroethylene (PTFE) prosthetic patch repair of ventral hernia. Prospective comparison to open prefascial polypropylene mesh repair. Surg Endosc. 2000; 14 (4): 326–329 [DOI] [PubMed] [Google Scholar]
- 3. Leber GE, Garb JL, Alexander AI, Reed WD. Long term complications associated with prosthetic repair of incisional hernias. Arch Surg. 1998; 133 (4): 378–382 [DOI] [PubMed] [Google Scholar]
- 4. Heniford. B, Park. T, Ramshaw B.J, Voller G. Laparoscopic repair of ventral hernia: Nine Years experiences with 850 consecutive hernia. Ann Surg. 2003; 238 (3): 391–399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. LeBlanc KA, Booth WV. Laparoscopic repair of incisional abdominal hernias using expanded polytetrafluoroethylene: preliminary findings. Surg Laparosc Endosc. 1993; 3 (1): 39–41 [PubMed] [Google Scholar]
- 6. Heniford BT, Ramshaw BJ. Laparoscopic ventral hernia repair: a report of 100 consecutive cases. Surg Endosc. 2000; 14 (5): 419–423 [DOI] [PubMed] [Google Scholar]
- 7. Beldi G, Ipaktchi R, Wagner M, Gloor B, Candinas D. Laparoscopic ventral hernia repair is safe and cost effective. Surg Endosc. 2006; 20 (1): 92–95 [DOI] [PubMed] [Google Scholar]
- 8. Park A, Birch DW, Lovrics P. Laparoscopic and open incisional hernia repair: a comparison study. Surgery. 1998; 124 (4): 816–821 [DOI] [PubMed] [Google Scholar]
- 9. McGreevy JM, Goodney PP, Birkmeyer CM, Finlayson SR, Laycock WS, Birkmeyer JD. A prospective study comparing the complication rates between laparoscopic and open ventral hernia repairs. Surg Endosc. 2003; 17 (11): 1778–1780 [DOI] [PubMed] [Google Scholar]
- 10. Cobb WS, Kercher KW, Heniford BT. The argument of lightweight polypropylene mesh in hernia repair. Surgical Innov. 2005; 12 (1): 63–71 [DOI] [PubMed] [Google Scholar]
- 11. Olmi S, Magnone S, Erba Luigi. Results of Laparoscopic versus open abdominal and incisional hernia repair. JSLS. 2005; 9 (2): 189–195 Was 5 is [PMC free article] [PubMed] [Google Scholar]
- 12. van't Riet M, Burger JW, Bonthuis F, Jeekel J, Bonjer HJ. Prevention of adhesion formation to polypropylene mesh by collagen coating: a randomized controlled study in a rat model of ventral hernia repair. Surg Endosc. 2004; 18 (4): 681–685 [DOI] [PubMed] [Google Scholar]
- 13. van 't Riet M, de Vos van Steenwijk PJ, Bonthuis F, et al. Prevention of adhesion to prosthetic mesh: comparison of different barriers using an incisional hernia model. Ann Surg. 2003; 237 (1): 123–128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Matthews BD, Pratt BL, Pollinger HS, et al. Assessment of adhesion formation to intra-abdominal polypropylene mesh and polytetrafluoroethylene mesh. J Surg Res. 2003; 114 (2): 126–32 [DOI] [PubMed] [Google Scholar]
- 15. Craft RO, Harold KL. Laparoscopic repair of incisional and other complex abdominal wall hernias. Permanente J. 2009; 13 (3): 38–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Basoglu M, Yildirgan MI, Yilmaz I, et al. Late complications of incisional hernias following prosthetic mesh repair. Acta Chir Belg. 2004; 104 (4): 425–428 [PubMed] [Google Scholar]
- 17. Felemovicius I, Bonsack ME, Hagerman G, Delaney JP. Prevention of adhesions to polypropylene mesh. J Am Coll Surg. 2004; 198 (4): 543–548 [DOI] [PubMed] [Google Scholar]
- 18. Alimoglu O, Akcakaya A, Sahin M, et al. Prevention of adhesion formations following repair of abdominal wall defects with prosthetic materials (an experimental study). Hepatogastroenterology. 2003; 50 (51): 725–728 [PubMed] [Google Scholar]
- 19. Heniford BT, Walters AL, Lincourt AE, Novitsky YW, Hope WW, Kercher KW. Comparison of generic versus specific quality-of-life scales for mesh hernia repairs. J Am Coll Surg. 2008; 206 (4): 638–644 [DOI] [PubMed] [Google Scholar]
- 20. Lawrence K, McWhinnie D, Goodwin A, et al. Randomised controlled trial of laparoscopic versus open repair of inguinal hernia: early results. BMJ. 1995;14:311(7011):981–985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Douek M, Smith G, Oshowo A, Stoker DL, Wellwood JM. Prospective randomised controlled trial of laparoscopic versus open inguinal hernia mesh repair: five year follow up. BMJ. 2003;10:326(7397):1012–1013 [DOI] [PMC free article] [PubMed] [Google Scholar]


