Single-port laparoscopic cholecystectomy with a 10-mm telescope and inbuilt working channel has been found to be safe, effective, economical, and capable of producing virtually scarless results.
Keywords: Laparoscopic cholecystectomy, Laparoscopy, Single port, Single-incision, Children, Pediatric
Abstract
Background and Objectives:
Multiple single-port or single-incision techniques have been successfully implemented for laparoscopic cholecystectomy in adults and children. These techniques require either a large multichannel port or a larger skin incision to accommodate multiple ports or instruments. Inspired by a first generation single-port instrument, we developed a safe and effective technique for a single-port laparoscopic cholecystectomy with virtually scarless results.
Methods:
Over a 14-mo period, 20 patients (19 females, 1 male) underwent the hybrid single-port cholecystectomy. A straight 10-mm Storz telescope with inbuilt 6-mm working channel in combination with 2 portless 2.3-mm percutaneous graspers was used. The dissection is carried out with 43-cm bariatric length instruments. The cystic artery and duct are sealed with WECK Hem-o-lok clips or the Harmonic scalpel.
Results:
Range (mean) age: 7.7 y to 19.5 y (15.5), BMI: 11.6kg/m2 to 42.3kg/m2 (27), operative duration 48 min to 120 min (79), postoperative length of stay: 5 h to 78 h (24). Diagnosis: 13 patients cholecystolithiasis, 7 patients biliary dyskinesia. Conversion to conventional 4-port cholecystectomy was required in 2 patients. No intra- or postoperative complications occurred.
Conclusion:
The hybrid single-port technique is easy to master. It provides traditional anatomical exposure and allows application of conventional laparoscopic principles.
INTRODUCTION
Recent refinements in minimally invasive equipment and techniques have allowed a transition from traditional multiport operations to similar operations performed through either a single laparoscopic access port or a single skin incision. These techniques require either a large multichannel port with a sealing device to prevent loss of insufflation pressure, or a larger skin incision to accommodate placement of multiple ports or instruments directly through the abdominal wall. These alternatives to traditional laparoscopic surgery evolved from a desire to further reduce both procedure-related pain and the cosmetic drawbacks of multiple (albeit small) visible scars.
Numerous studies have confirmed the surgical efficacy and patient acceptance of single-port surgery in adults, and have also established their safety and efficacy in the pediatric population. The benefits of reduced pain and improved cosmesis enjoyed by adult patients have not, however, been reliably observed in children and adolescents. The larger incisions and port sizes have, in many instances, caused more postoperative discomfort and produced aesthetically inferior results compared to traditional laparoscopic techniques.
The often unsatisfactory application of these new single-port techniques to children has created an impetus to develop an age-appropriate method for conducting single-port surgery in smaller patients that is safe and effective, while still resulting in reduced pain and improved cosmesis. Encouraged by our experience with single-port appendectomy using a 10-mm operating laparoscope that comprises both a fiberoptic telescope and instrumentation channel, we developed a straightforward single-port technique for cholecystectomy that provides visualization and technical ergonomics similar to the standard laparoscopic procedure, and achieves the objectives of reduced pain and improved cosmesis in pediatric patients.
MATERIALS AND METHODS
Patients
Between November 2010 and December 2011, we performed hybrid single-port laparoscopic cholecystectomies in 20 pediatric patients, 19 females and 1 male. Institutional review board approval for retrospective review of the data was obtained (study number 11-1199). Thirteen patients had cholecystolithiasis with various degrees of cholecystitis, documented by ultrasound. Seven patients suffered from chronic right upper quadrant abdominal pain and were diagnosed with biliary dyskinesia with a HIDA scan ejection fraction below 30%.
Surgical Procedure
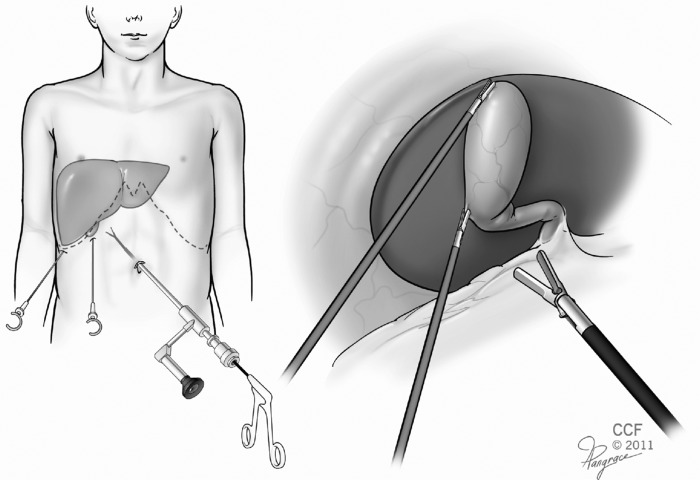
An 11-mm Step bladeless trocar (Covidien, Mansfield, MA) is placed into the abdominal cavity using the standard open transumbilical technique. Depending on patient size, a pneumoperitoneum of 12mm Hg to 15mm Hg is established. A 10-mm Storz Hopkins telescope with inbuilt 6-mm working channel is used. This telescope combines a 0-degree fiberoptic with a 6-mm working channel. All instruments must be a minimum of 43cm long (Figure 1).
Figure 1.
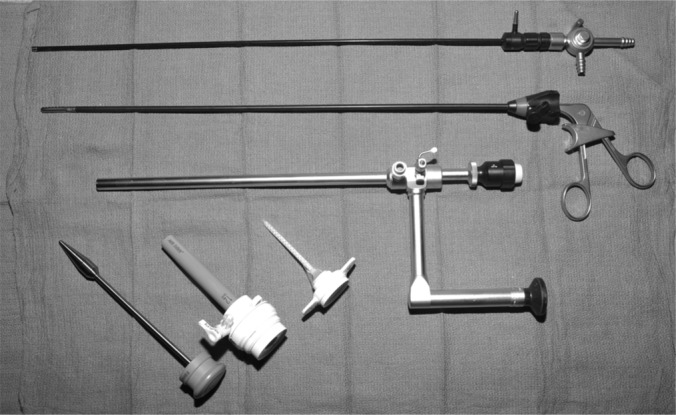
Storz 10-mm Hopkins telescope with inbuilt working channel, 43-cm long instruments, Step trocar.
Under direct vision, 2 portless 2.3-mm Clutch Graspers (Stryker, MiniLap, Kalamazoo, MI) are introduced into the abdominal cavity through stab incisions in the right subcostal area. The assistant manipulates the graspers. The lateral grasper is used to push the fundus of the gallbladder over the dome of the liver. With the medial grasper, the gallbladder infundibulum is pulled to the right. This maneuver exposes Calot's triangle. We mainly use a hook cautery, Maryland and atraumatic graspers to dissect the cystic artery and cystic duct. An intraoperative cholangiogram with a 48-cm Kumar cholangiography clamp (Nashville Surgical Instruments, Springfield, TN) can be performed. The cystic duct and cystic artery are clipped with medium size WECK Hem-o-lok clips (Weck Closure Systems, Research Triangle Park, NC) and sharply divided. The gallbladder is separated from the fossa with electrocautery and removed through the umbilical port site. In 6 cases, a laparoscopic Harmonic scalpel (Ethicon EndoSurgery, Cincinnati, OH) was used to seal the cystic duct and cystic artery and to dissect the gallbladder from the gallbladder bed (Figures 2, 3, 4).
Figure 2.
Instrument and trocar placement.
Figure 3.
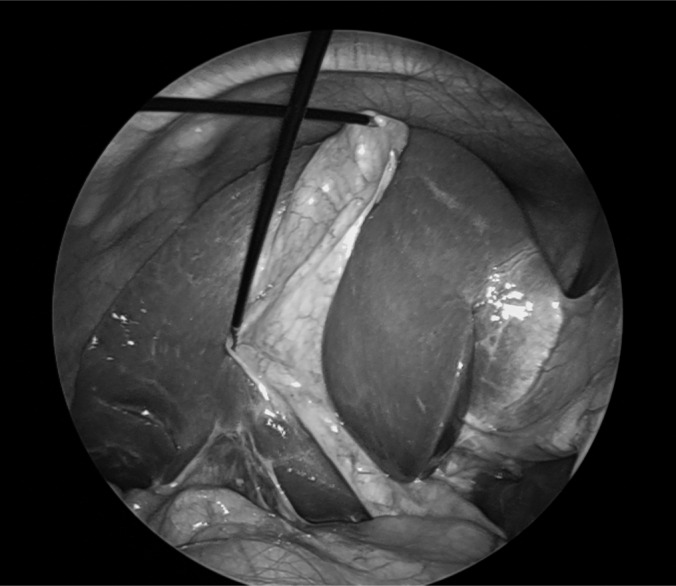
Retraction of gallbladder with percutaneous retractors.
Figure 4.

Surgical incisions 4 wk postoperatively.
The stab incisions are closed with Dermabond. The umbilical ring is closed with absorbable sutures, and the skin is closed and dressed cosmetically.
RESULTS
The method was applied in 20 patients. Table 1 provides patient and case characteristics. All but one patient was female, and most were diagnosed with cholecystolithiasis.
Table 1.
Patient Characteristics (n=20)
| Age [years] (mean/range) | 15.5/7.7–19.5 |
| Gender (F/M) | 19/1 |
| Diagnosis (cholecystolithiasis/biliary dyskinesia) | 13/7 |
| Weight [kg] (mean/range) | 68.2/19.4–108.4 |
| BMI [kg/m2] (mean/range) | 27/11.6–42.3 |
| Operative time [min] (mean/range) | 79/48–120 |
| Postoperative length of stay [hours] (mean/range) | 24/5–78 |
No intra- or postoperative complications occurred in any patient. In 2 cases, severe pericystic adhesions were encountered, requiring conversion to conventional 4-port laparoscopic cholecystectomy. Three patients had an intraoperative cholangiogram. Blood loss was negligible in all cases. Average postoperative length of stay was 24 h (range, 5 to 78). Four patients (20%) were discharged the same day, 13 patients (65%) left the hospital on postoperative day 1, and 3 patients (15%) were discharged on postoperative day 2. Patients were seen for a postoperative follow-up examination after 4 wk to 6 wk. All patients reported complete resolution of postoperative pain after 5 d and were allowed to resume full physical activity after 3 wk.
DISCUSSION
In recent years, many surgical subspecialties have experienced a paradigm shift from open to minimally invasive surgery. This evolution has progressed to the development of different promising single-port and single-site laparoscopic procedures that are in strong demand by the public.1,2 Commercial single-port devices like the SILS Port (Covidien, Norwalk, CT) or the TriPort Access System (Advanced Surgical Concepts, Wicklow, Ireland) seal the umbilical incision and allow bundled umbilical introduction of the endoscope and working instruments without loss of the pneumoperitoneum. In children, laparoscopic single-site cholecystectomy is a viable alternative to the conventional 4-port technique. These techniques have been shown to be safe and effective with similar outcomes as the traditional multiport laparoscopy.3–6
The disadvantage of single-site surgeries with sealing devices or placement of multiple instruments through the same incision is the obligatory size of 20mm to 25mm for the main incision, which is comparatively large for a pediatric patient. The single-port devices are large enough to produce significant dilation of the umbilical ring in children. This not only creates more postoperative discomfort, but also often results in an unnatural abdominal wall appearance after umbilical closure. The use of a 10-mm operating laparoscope allows the use of a standard access port and results in a predictably excellent cosmetic outcome.
Single-incision multiport techniques demand considerable practice and advanced laparoscopic skills from the surgeon. They provide a limited degree of instrument range and compromised ergonomics. Furthermore, triangulation with mirror-inverted view of the working instruments violates traditional basic principles of laparoscopic surgery. The use of the 10-mm Storz telescope with inbuilt 6-mm working channel obviates some of the disadvantages of the described single-site techniques. It combines the benefits of minimally invasive single-port surgery with traditional exposure and in-line ergonomics of conventional laparoscopic surgery. The learning curve is comparatively shallow compared to the standard single-port technique. Khosla et al.7 and Rothenberg et al.8 described a comparable laparoscopic technique with a modified Frazee endoscope, accommodating a 4-mm 6-degree optic and a 5-mm working channel. Unlike the Storz telescope, it is not commercially available.
The 27-cm length and 0-degree optic are the main shortcomings of the Storz telescope; 43-cm instruments are required, which makes its use in very small patients more demanding. The in-line relationship of the operating channel and the 0-degree optic can create parallax view problems, but these are partially compensated by the excellent maneuverability of the gallbladder with the portless graspers.
The described technique provides adequate view and exposure of the cystic duct to perform a traditional cholangiography with a 48-cm Kumar cholangiography clamp (Nashville Surgical Instruments, Springfield, TN). This was successfully performed on 2 patients.
In the first 6 patients, we sealed the cystic artery and duct, and performed the dissection of the gallbladder from the fossa, with the laparoscopic Harmonic scalpel (Ethicon EndoSurgery). Numerous reports have documented the safety of ultrasonic devices for the gallbladder dissection and ligation of the cystic duct and artery.9,10,11 Although technically satisfactory, the use of the Harmonic scalpel for this limited purpose resulted in an unfavorable cost-per-case metric. For reasons of cost-containment, we adopted the use of self-locking polymer clips (Hem-o-lok, Weck Closure Systems, Research Triangle Park, NC) to control the cystic duct and larger cystic arteries in most our patients. Hem-o-lok clips are self-locking polymer clips with outstanding tissue sealing properties that provide secure closure of tubular structures, such as blood vessels, appendiceal stumps, or ureters.12,13
The gallbladder is removed directly through the umbilical port site. The fascial defect can be widened to remove a large gallbladder.
There are some limitations to this procedure. Severe cholelithiasis or tense adhesions can reduce the maneuverability of the gallbladder with the 2.3-mm graspers; hence, placement of more rigid 5-mm graspers is necessary. Anatomical variations or postinflammatory changes may demand an angulated optic for optimal view. In these cases, conversion to the traditional laparoscopic cholecystectomy is advised.
CONCLUSION
In the vast majority of children and adolescents with typical gallbladder disease, hybrid single-port laparoscopic cholecystectomy with the 10-mm Storz telescope with inbuilt working channel has been shown to be safe and effective, economical, with virtually scarless results. It has been successfully applied in patients of all sizes, from children to adult-sized adolescents. We have found the technique easy to learn, safe to perform, efficient, and well accepted by our patients.
Contributor Information
Federico G. Seifarth, Cleveland Clinic Foundation, Department of Pediatric Surgery, Pediatric Institute & Children's Hospital, Cleveland, OH USA..
José R. Ramirez, Cleveland Clinic Foundation, Department of General Surgery, Digestive Disease Institute, Cleveland, OH USA..
David K. Magnuson, Cleveland Clinic Foundation, Department of Pediatric Surgery, Pediatric Institute & Children's Hospital, Cleveland, OH USA..
References:
- 1. Romanelli JR, Earle DB. Single-port laparoscopic surgery: an overview. Surg Endosc. 2009; 23: 1419–1427 [DOI] [PubMed] [Google Scholar]
- 2. Bucher P, Pugin F, Buchs NC, Ostermann S, Morel P. Randomized clinical trial of laparoendoscopic single-site versus conventional laparoscopic cholecystectomy. Br J Surg. 2011; 98 (12): 1695–16702 doi:10.1002/bjs. 7689 Epub 2011 Sep 30 [DOI] [PubMed] [Google Scholar]
- 3. Chandler NM, Danielson PD. Single-incision laparoscopic cholecystectomy in children: a retrospective comparison with traditional laparoscopic cholecystectomy. J Pediatr Surg. 2011; 46: 1695–1699 [DOI] [PubMed] [Google Scholar]
- 4. de Armas IA, Garcia I, Pimpalwar A. Laparoscopic single port surgery in children using Triport: our early experience. Pediatr Surg Int. 2011; 27: 985–989 [DOI] [PubMed] [Google Scholar]
- 5. Holcomb GW., 3rd Single-site umbilical laparoscopic cholecystectomy. Semin Pediatr Surg. 2011; 20: 201–207 [DOI] [PubMed] [Google Scholar]
- 6. Garey CL, Laituri CA, Ostlie DJ, et al. Single-incision laparoscopic surgery in children: initial single-center experience. J Pediatr Surg. 2011; 46: 904–907 [DOI] [PubMed] [Google Scholar]
- 7. Khosla A, Ponsky TA. Use of operative laparoscopes in single-port surgery: The forgotten tool. J Minim Access Surg. 2011; 7: 116–120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rothenberg SS, Shipman K, Yoder S. Experience with modified single-port laparoscopic procedures in children. J Laparoendosc Adv Surg Tech A. 2009; 19: 695–698 [DOI] [PubMed] [Google Scholar]
- 9. El-Geidie AA. Single-Incision Laparoscopic Cholecystectomy (SILC) Using Harmonic Scalpel. J Surg Res. 2012; 176 (1): 50–54 Epub 2011 Aug 12 [DOI] [PubMed] [Google Scholar]
- 10. Huscher CG, Lirici MM, Di Paola M, et al. Laparoscopic cholecystectomy by ultrasonic dissection without cystic duct and artery ligature. Surg Endosc. 2003; 17: 442–451 [DOI] [PubMed] [Google Scholar]
- 11. Tebala GD. Three-port laparoscopic cholecystectomy by harmonic dissection without cystic duct and artery clipping. Am J Surg. 2006; 191: 718–720 [DOI] [PubMed] [Google Scholar]
- 12. Hanssen A, Plotnikov S, Dubois R. Laparoscopic appendectomy using a polymeric clip to close the appendicular stump. JSLS. 2007; 11: 59–62 [PMC free article] [PubMed] [Google Scholar]
- 13. Ponsky L, Cherullo E, Moinzadeh A, et al. The Hem-o-lok clip is safe for laparoscopic nephrectomy: a multi-institutional review. Urology. 2008; 71: 593–596 [DOI] [PubMed] [Google Scholar]