The author contends that until the complication rate for single incision cholecystectomy and natural orifice procedures are established, traditional 4-port laparoscopic cholecystectomy should remain the standard technique.
Keywords: Laparoscopy, Cholecystectomy, Cholangiography, Complications
Abstract
Objectives:
To describe the surgical complications associated with laparoscopic cholecystectomy, as performed by a single surgeon over an 8-year period and to discuss how this compares to newer methods of cholecystectomy, such as single-incision surgery and natural orifice transluminal endoscopic surgery.
Methods:
The charts of 1000 consecutive patients who underwent consecutive cholecystectomies were reviewed to gather the following information: age, sex, prior abdominal procedures, type of procedure performed (laparoscopic vs open, with or without cholangiography), pre and postoperative diagnosis, and complications directly related to surgical technique, such as biliary injury, bile leak, infection, trocar-related injury, and incisional hernia.
Results:
The laparoscopic approach was attempted in all but one patient and was successful in 94.1% of patients. The conversion rate was higher with acute cholecystitis than with other forms of biliary tract disease. Successful cholangiography was accomplished in over 97% of patients. Nineteen complications directly related to the surgical procedure were found, including one bile duct injury.
Conclusion:
Laparoscopic cholecystectomy continues to offer a safe and effective treatment for patients with symptomatic biliary tract disease. Although other forms of minimally invasive cholecystectomy are being studied, there is little data to suggest any additional benefit, other than a slight improvement in cosmesis. Until larger series demonstrate that these techniques have a complication rate similar to those cited in the surgical literature, traditional 4-port laparoscopic cholecystectomy should remain the standard of care.
INTRODUCTION
Cholecystectomy is the most common intraabdominal surgical procedure performed in the United States. Laparoscopic removal is now the procedure of choice when cholecystectomy is indicated. However, newer, less invasive techniques, such as natural orifice transluminal endoscopic surgery (NOTES) and single incision laparoscopic cholecystectomy (SILC), are currently being investigated as alternatives to the traditional 4-port laparoscopic removal. Safety data and definitive benefits of these less invasive procedures are lacking. This report presents the outcomes of 1000 consecutive cholecystectomies with an emphasis on operative complications. Results similar to those presented in this report should be the goal in any large series of patients when cholecystectomy is performed using one of these newer techniques.
METHODS
The records of 1000 consecutive cases of cholecystectomy were reviewed. All records were available for review, and all cases were performed by a single surgeon in a nonteaching community hospital from April 2002 through August 2010. Data extracted for this review included age, sex, prior abdominal surgical procedures, pre and postoperative diagnosis, primary and secondary surgical procedures performed, pathology of the gallbladder, and complications directly related to the surgical procedure. Laparoscopic cholecystectomy (LC) was attempted in 99.9% of patients. The technique did not change over the course of the review. Briefly, initial peritoneal access was achieved using an open technique and a Hasson trocar placed at the umbilicus. Initial access using the open technique through a subcostal incision was used in those patients who had previous abdominal procedures through a midline incision. Three additional ports were used to perform the procedure: the 1 subxiphoid port (5mm or 10mm) and the 2 subcostal ports (5mm). After adequate retraction, dissection was carried out to identify the cystic duct and artery. An intraoperative cholangiogram (IOCG) using fluoroscopy was attempted in all cases. After the gallbladder was dissected free from the liver, it was placed in an endoscopic pouch and removed from the peritoneal cavity. After irrigation of the operative site, all trocars were removed under direct vision to ensure that there was no bleeding. Closure was performed with absorbable sutures for the fascia and skin.
RESULTS
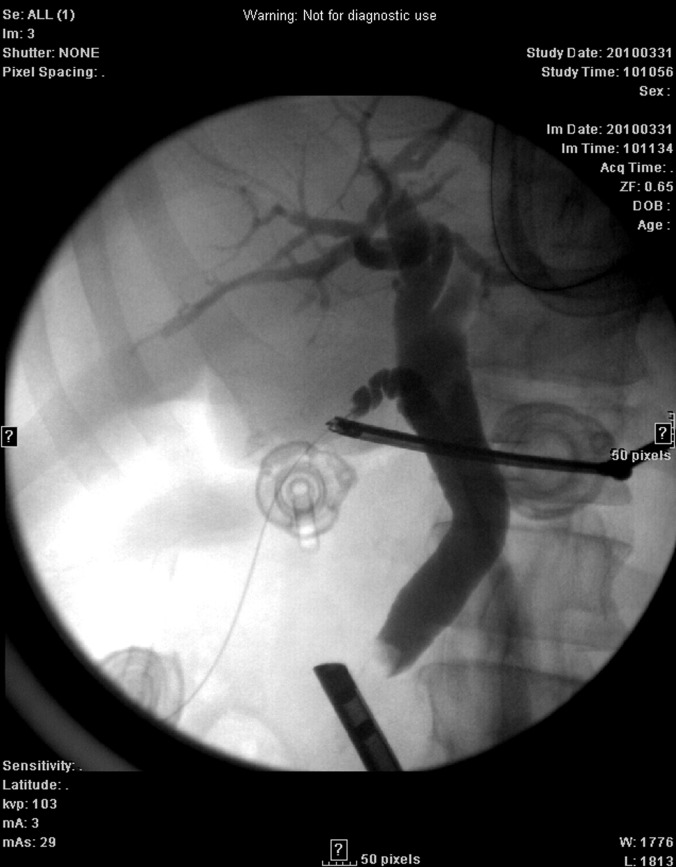
Patient ages ranged from 10 to 92 y (median, 52 y), with 73.7% women and 26.3% men. Preoperative diagnosis was acute cholecystitis in 11.7% of patients, chronic cholecystitis 59%, biliary dyskinesia 24.4%, biliary pancreatitis 3.9%, and gallbladder polyp 0.1%. Not including the cases of biliary dyskinesia, the pre and postoperative diagnosis matched in 98.7% of cases. One patient was found to have carcinoma of the gallbladder (T3 lesion). In those patients with biliary dyskinesia, 61.2% were found to have chronic acalculous cholecystitis, 5.7% had chronic calculous cholecystitis, and 33.1% had a normal gallbladder. A laparoscopic approach was attempted in all but one patient who had >10 common duct stones not retrievable with an endoscopic retrograde cholangiopancreatogram (ERCP). Laparoscopic cholecystectomy was completed in 94.1% of patients. Conversion of 5.9% of patients to open cholecystectomy was similar to that found in other reports.1 Acute cholecystitis was associated with a much higher incidence of conversion (26.7%) than with other forms of biliary tract disease (2.8%). All but one conversion to an open procedure were due to intense inflammation, infection, or adhesions precluding a safe laparoscopic approach. One patient with severe chronic cholecystitis was converted due to an abnormal IOCG showing only the distal common bile duct. No conversions were due to bleeding or injury to other organs. A total of 418 patients had prior abdominal surgery (Table 1). Of those who had a successful laparoscopic procedure, 42% had at least one previous abdominal procedure. Cholangiography was successfully performed in 97.1% of patients (83% success rate for open cholecystectomy, 98% for laparoscopic). Cholangiography was positive for a filling defect or stone in 4% of patients (Figure 1). Additional procedures during cholecystectomy were performed in 9% of patients (Table 2). The 2 most common procedures were repair of umbilical hernia and needle biopsy of the liver. Ten patients underwent common duct exploration due to choledocholithiasis found on IOCG; 2 of these were performed laparoscopically via the cystic duct, and 8 patients underwent open common duct exploration as part of an open cholecystectomy. An additional 2.3% of patients underwent a postoperative ERCP for a positive IOCG.
Table 1.
Prior Abdominal Procedures In Patients Undergoing Laparoscopic Cholecystectomy
| Procedure* | No. of patients |
|---|---|
| Hysterectomy, abdominal | 255 |
| Appendectomy | 119 |
| Gastric Procedure | 25 |
| Colectomy, partial | 13 |
| Hernia, ventral/incisional | 11 |
| Exploratory laparotomy | 10 |
| Oophorectomy | 8 |
| Prostatectomy | 6 |
| Small bowel resection | 5 |
| Hysterectomy, vaginal | 4 |
| Nephrectomy | 4 |
| Aortic aneurysm repair | 3 |
| Splenectomy | 2 |
| Peritoneal dialysis catheter | 2 |
71 patients had multiple procedures.
Figure 1.
Positive IOCG showing stone in distal common bile duct.
Table 2.
Additional Procedures Performed During Laparoscopic Cholecystectomy
| Procedure | No. of Patients |
|---|---|
| Liver biopsy | 37 |
| Hernia: umbilical | 29 |
| Hernia: ventral | 8 |
| Lysis of adhesions | 4 |
| Duodenal ulcer rep | 2 |
| Implantable port | 1 |
| Hysterectomy, abdominal | 1 |
| Oophorectomy | 1 |
| Hernia: inguinal | 1 |
| Remove PD catheter | 1 |
| Chest tube thoacostomy | 1 |
| Remove Angelchik prosthesis | 1 |
| Hemorrhoidectomy | 1 |
| Gastrostomy, jejunostomy | 1 |
| Excision skin cancer | 1 |
| Cholecysto-duodenal fistula rep | 1 |
PD=peritoneal dialysis.
For the purposes of this review, only complications considered to be directly related to the operative procedure were considered. When comparing traditional laparoscopic cholecystectomy with NOTES or SILC, complications related to a patient's comorbid conditions would more than likely be similar no matter what the approach. The main issue is whether these new techniques will have a greater risk of complication directly related to the procedure or will improve upon the already low risk associated with 4-port LC. Therefore, the complications screened for in this review include accidental injury to the bowel or vasculature, biliary injury, postoperative bile leak, and infection. Delayed complications like incisional hernia were also included. Bile spillage during cholecystectomy is not included, because this was not consistently noted in the operative report, and almost always some bile, small stones, or debris is spilled during cholangiography. Copious irrigation was used in all patients to remove any blood, bile, or stones from the operative site prior to trocar removal.
A total of 19 complications (1.9%) directly related to the operative procedure occurred in this series (Table 3), including one postoperative death (0.1%). Postoperative bile leak occurred in 6 patients following a successful LC. When confirmed with imaging studies, all patients were taken back to the operating room for laparoscopic irrigation of the peritoneal cavity and drain placement. An ERCP with stent placement was then performed. Leakage resolved in all patients within 1 to 2 wk. Three patients developed an abscess in the liver bed and were treated with percutaneous drainage and antibiotics, and one patient developed a wound infection following open cholecystectomy. Four patients developed an incisional hernia at the site of the Hasson trocar placement. Three patients were repaired using an open technique with mesh, and one was repaired laparoscopically. One patient developed a small bowel obstruction one day following an uncomplicated LC. This occurred secondary to dehiscence of the fascial closure at the umbilicus following an episode of severe retching. Repair of the defect was performed through the same incision. One patient developed a pneumothorax after accidental injury to the diaphragm. This was caused when the instrument used to retract the fundus of the gallbladder slipped and punctured the diaphragm. The injury was detected laparoscopically, and because it was <1cm in diameter and located over the dome of the liver, no formal repair was performed. A chest tube was placed after LC to treat the pneumothorax. Only one major ductal injury occurred in this series. IOCG showed only the distal common bile duct (CBD), and the patient was converted to an open procedure. The small opening in the CBD was repaired; however, the patient had an accessory right hepatic duct that was injured during dissection of the gallbladder from the liver. This patient was referred to a hepato-biliary surgeon at a tertiary care center for definitive repair. Finally, there was one patient death. This patient underwent an attempted LC that was converted to open cholecystectomy secondary to acute and chronic cholecystitis. This patient had multiple medical problems including chronic kidney disease, diabetes, coronary artery disease, and chronic myelogenous leukemia and died 7 d postoperatively from complications related to his comorbid conditions.
Table 3.
Complications
| Procedure | No. of patients |
|---|---|
| Bile leak (no ductal injury) | 6 |
| Hernia, port site | 4 |
| Abscess | 4 |
| Death | 1 |
| Diaphragm injury, pneumothorax | 1 |
| Umbilical incision dehiscence | 1 |
| Bowel obstruction | 1 |
| Bile duct injury | 1 |
DISCUSSION
LC rapidly replaced open cholecystectomy (OC) 20 y ago as the procedure of choice when cholecystectomy is indicated.2 Few randomized trials were performed comparing LC to OC given the significant difference between the 2 procedures with regard to pain, hospital length of stay, and postoperative recovery. Some investigators felt it would be unethical to subject patients to OC in a randomized trial given the benefits seen with LC.3 However, as the number of laparoscopic cholecystectomies increased, it became evident that certain complications rarely seen with OC were more frequent when LC was performed. These complications included intestinal and vascular injuries from trocar or Veress needle insertion and major bile duct injuries.4–6 Currently, novel new techniques for gallbladder removal, such as natural orifice transluminal endoscopic surgery (NOTES) and single incision laparoscopic cholecystectomy (SILC), are being investigated as an alternative to the traditional 4-port LC. While neither technique has been widely adopted, there is growing enthusiasm for SILC despite lack of data showing a distinct advantage over the traditional laparoscopic approach. Also unknown is how this increase in SILC will affect the currently low complication rate of LC, particularly as it pertains to bile duct injury.
One major difference between 4-port laparoscopic cholecystectomy and its less invasive counterparts, NOTES and SILC, is the technique to gain entry into the peritoneal cavity. In the traditional 4-port technique, access to the peritoneal cavity can be performed using either a closed or open technique. Complications related to initial trocar insertion include vascular and intestinal injury, with rate of injury reported in large series from 0% to 0.23%.4,7 The vast majority of trocar insertion-related injuries occur with the Veress needle technique. In an analysis of trocar-related injuries reported to the FDA in the mid 1990s, there were 182 visceral and 408 vascular injuries, all using the closed technique.8 In a review by Hasson totaling close to 560,000 laparoscopic procedures, the rate of injury for closed technique was vascular 0.2%, visceral 0.1%, and open technique 0.0% and 0.1%, respectively.9 Though extremely rare, major vascular injury using the open technique has been reported.10
Complications related to peritoneal access for SILC are likely to be similar to those seen with the 4-port technique. Like the 4-port LC, there is no consensus regarding the ideal method to gain access to the peritoneal cavity as reported series use both open11,12 and closed13,14 techniques. The number (12 to 150) of patients in these studies is too small to evaluate the incidence of vascular or intestinal complications from Veress needle or trocar insertion. However, there is no reason to believe that the frequency of these complications would be any different in SILC than in 4-port LC, because the entry techniques are identical. When choosing the technique to gain peritoneal access during either LC or SILC, one must remember that major vascular injury never occurs with open cholecystectomy. Using only an open technique, the injury rate was 0% for both vascular and intestinal injury in the author's personal series.
Peritoneal access is of a radically different nature with NOTES. Three primary access sites, stomach, vagina, and rectum, are currently being investigated for NOTES procedures. Of these, cholecystectomy has been performed most frequently through the vagina.15–17 Although NOTES has been studied for over 6 y, it has yet to achieve widespread use in the surgical community, unlike laparoscopic cholecystectomy, which virtually replaced the open technique in just 2 y to 3 y. The main limitations of NOTES are the lack of advanced instrumentation and closure techniques, particularly for the transgastric approach. Also, NOTES is not applicable to all patients. In the German registry for NOTES, 99.2% of patients were women and a transvaginal approach was used in almost all of these patients.17 Of the 1000 patients presented herein, over 50% would not be eligible for NOTES due the prior pelvic surgery or male sex. These patients would be candidates for the transgastric route; however, contamination of the peritoneal cavity is also much more likely with NOTES if the transgastric route is used versus the transvaginal approach. Studies looking at bacterial counts and cultures of the peritoneal cavity following gastrotomy show that bacterial counts are higher after gastrotomy18 and may result in peritonitis.19 Although this has not translated into increased incidence of peritonitis in the cases reported thus far,15,17 the potential exists should NOTES become more widely utilized.
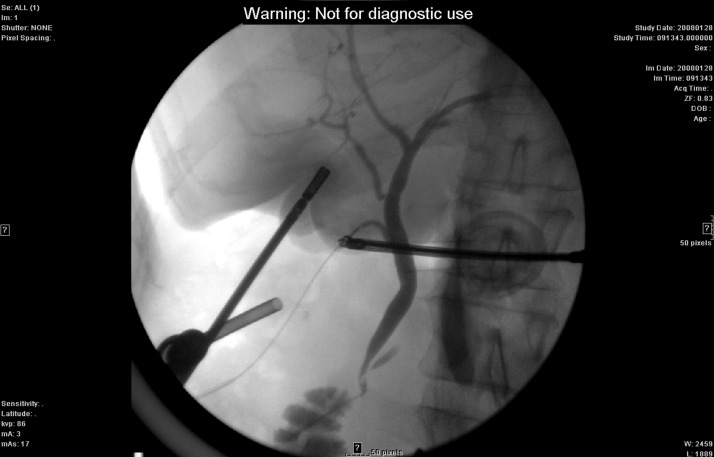
Biliary injury continues to be a significant complication seen with all forms of minimally invasive cholecystectomy. Although rare, injury to the common bile duct often results in additional surgical procedures and increased risk of morbidity and mortality. Bile duct injury is also a leading cause of litigation against general surgeons.20 An increase in the rate of major ductal injury was seen with the advent of LC; however, several reports with a large series of patients demonstrates that LC can be performed with a biliary injury rate comparable to that of OC.2,21,22 Key components in minimizing ductal injury include surgeon experience,2 adherence to well-defined dissection principals (critical view of safety),23 and cholangiography.20 Cholangiography remains controversial as a means to reduce biliary injury during laparoscopic cholecystectomy. While increased cost and operative time have been cited as reasons not to perform routine IOC, several large population-based studies have shown a substantial reduction of >50% in CBD injury when routine IOC is performed.20,24 Additional benefits to cholangiography include identification of occult choledocholithiasis (Figure 1) and precise delineation of biliary anatomy (Figures 2 and 3). Despite these potential advantages, IOC continues to be utilized in a minority of cases.20,25
Figure 2.
Anatomic variation: cystic duct draining into right hepatic duct.
Figure 3.
Anatomic variation: accessory right hepatic duct.
Biliary injury statistics are difficult to assess with SILC and NOTES, because many of the reports involve a relatively small number of patients. In a recent collective review of all types of single incision laparoscopic surgery, 73% of all reviewed studies contained 20 or fewer patients.26 In 3 articles published after the publication of this collective review, a total of 4 patients who underwent SILC experienced a major biliary injury; 3 required hepaticojejunostomy.27–29 In another published series of SILC,13 cholangiography was utilized in only 10% of patients. It is curious to see that IOCG is not used more liberally when SILS or NOTES is performed, especially if it could lead to reduced biliary tract injuries. Given the changes in visualization and difficulties in dissection due to loss of triangulation in SILC and NOTES, if these less-invasive procedures become more widespread among surgeons without adequate training and supervision, will we again see an increase in biliary injury similar to that seen with the adoption of LC?
Although rare, port-site hernias are a well-known, though late, complication of laparoscopic surgery. In a recent review,30 the overall incidence was 1.7%. Determining the true incidence is difficult, because follow-up is often limited after LC. In the current series, a port-site hernia was diagnosed only after the patient presented with a bulge. All were at the umbilicus, and time from laparoscopic cholecystectomy to surgical repair of the hernia averaged 28 mo (range, 11 to 73). Similar incidence of hernia is likely with SILC, given the similar incision at the umbilicus, though data are lacking as this complication is rarely seen. Incisional hernia is unlikely to be seen after a NOTES procedure, as the site of access is often not in the abdominal wall.
CONCLUSION
Laparoscopy has transformed the way we do many procedures with great benefits to the patients. However, with these benefits come rare but substantial risks including vascular and intestinal injuries secondary to peritoneal access misadventures and major biliary injuries. At the beginning of what may be the next era of minimally invasive surgery, we must keep in mind that results are more important than cosmesis. The leap from open cholecystectomy to the laparoscopic version had substantial benefits: a 3- to 4-d hospitalization became an outpatient procedure, several weeks of recovery became 1 wk, and pain was substantially reduced. However, these benefits did not come without risk, most notably a doubling of the rate of major biliary tract injury. Other than cosmesis, the advantages of SILC or NOTES are less clear.26 Complications of LC, especially biliary tract injury, have been well defined over the past 20 y. The true incidence of complications following SILC is less clear due to the rarity of these complications and the small volume of patients in most of the reports on SILC. Until the data is better defined, are surgeons willing to accept a potentially higher complication rate with SILC in order to achieve little more than a better looking scar? Most patients are grateful for a well-conducted laparoscopic procedure free from complications and are less concerned about the size or location of the incisions used to complete the operation. As we move forward with these new techniques, let us be sure not to repeat the mistakes of the past.
References:
- 1. Sakpal SV, Bindra SS, Chamberlain RS. Laparoscopic cholecystectomy conversion rates two decades later. JSLS. 2010; 14: 476–483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Litwin DE, Cahan MA. Laparoscopic cholecystectomy. Surg Clin North Am. 2008; 88: 1295–1313 [DOI] [PubMed] [Google Scholar]
- 3. Neugebauer E, Troidl H, Spangenberger W, Dietrich A, Lefering A. Conventional versus laparoscopic cholecystectomy and the randomized controlled trial Cholecystectomy Study Group. Brit J Surg. 1991; 78: 150–154 [DOI] [PubMed] [Google Scholar]
- 4. Azevedo JL, Azevedo OC, Miyahira SA, et al. Injuries caused by Veress needle insertion for creation of pneumoperitoneum: A systematic literature review. Surg Endosc. 2009; 23: 1428–1432 [DOI] [PubMed] [Google Scholar]
- 5. Adamsen S, Hansen OH, Funch-Jensen P, Schulze S, Stage JG, Wara P. Bile duct injury during laparoscopic cholecystectomy: A prospective nationwide series. J Am Coll Surg. 1997; 184: 571–578 [PubMed] [Google Scholar]
- 6. Way LW, Stewart L, Gantert W, et al. Causes and prevention of laparoscopic bile duct injuries. Ann Surg. 2003; 237: 460–469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shäfer M, Läuper M, Krähenbühl L. Trocar and Veress needle injuries during laparoscopy. Surg Endosc. 2001; 15: 275–280 [DOI] [PubMed] [Google Scholar]
- 8. Bhoyrul S, Vierra MA, Nezhat CR, Krummel TM, Way LW. Trocar injuries in laparoscopic surgery. J Am Coll Surg. 2001; 192: 677–683 [DOI] [PubMed] [Google Scholar]
- 9. Hasson HM. Open laparoscopy as a method of access in laparoscopic surgery. Gynaecol Endosc. 1999; 8: 353–362 [Google Scholar]
- 10. Hanney RM, Carmalt HL, Merrett N, Tait N. Use of the Hasson cannula producing major vascular injury at laparoscopy. Surg Endosc. 1999; 13: 1238–1240 [DOI] [PubMed] [Google Scholar]
- 11. Chow A, Purkayastha S, Aziz O, Pefanis D, Paraskeva P. Single-incision laparoscopic surgery for cholecystectomy. Arch Surg. 2010; 145: 1187–1192 [DOI] [PubMed] [Google Scholar]
- 12. Hernandez j, Ross S, Morton C, et al. The learning curve of laparoendoscopic single-site cholecystectomy: Definable, short and safe. J Am Coll Surg. 2010; 211: 652–657 [DOI] [PubMed] [Google Scholar]
- 13. Rawlings A, Hodgett S, Matthews B, Strasberg SM, Quasebarth M, Brunt LM. Single-incision laparoscopic cholecystectomy: Initial experience with critical view of safety and routine intraoperative cholangiography. J Am Coll Surg. 2010; 211: 1–7 [DOI] [PubMed] [Google Scholar]
- 14. Tacchino R, Greco F, Matera D. Single-incision laparoscopic cholecystectomy: surgery without a visible scar. Surg Endosc. 2009; 23: 896–899 [DOI] [PubMed] [Google Scholar]
- 15. Meadows MC, Chamberlain RS. A review on the status of natural orifice transluminal endoscopic surgery (NOTES) cholecystectomy: techniques and challenges. Open Access Surgery. 2010; 3: 73–86 [Google Scholar]
- 16. Lehmann KS, Ritz JP, Wibmer A, et al. The German registry for natural orifice transluminal endoscopic surgery: report of the first 551 patients. Ann Surg. 2010; 252: 263–270 [DOI] [PubMed] [Google Scholar]
- 17. Lehmann KS, Ritz JP, Wibmer A, et al. The German Registry for Natural Orifice Transluminal Endoscopic Surgery (NOTES): Report of the First 24 Months. Presented at ACS 96th annual Clinical Congress, Bariatric and Foregut session, 2009. [Google Scholar]
- 18. Narula VK, Happel LC, Volt K, et al. Transgastric endoscopic peritoneoscopy does not require decontamination of the stomach in humans. Surg Endosc. 2009; 23: 1331–1336 [DOI] [PubMed] [Google Scholar]
- 19. Lomanto D, Chua HC, Myat MM, So J, Shabbir A, Ho L. Microbiological contamination during transgastric and transvaginal endoscopic techniques. J Laparoendo Adv Surg Techn. 2009; 19: 603–606 [DOI] [PubMed] [Google Scholar]
- 20. Flum DR, Dellinger EP, Cheadle A, Chan L, Koepsell T. Intraoperative cholangiography and risk of common bile duct injury during cholecystectomy. JAMA. 2003; 289: 1639–1644 [DOI] [PubMed] [Google Scholar]
- 21. Misra M, Schiff J, Rendon G, Rothschild J, Schwaitzberg S. Laparoscopic cholecystectomy after the learning curve: What should we expect? Surg Endosc. 2005; 19: 1266–1271 [DOI] [PubMed] [Google Scholar]
- 22. Tantia O, Jain M, Khanna S, Sen B. Iatrogenic biliary injury: 13305 cholecystectomies experienced by a single surgical team over more than 13 years. Surg Endosc. 2008; 22: 1077–1086 [DOI] [PubMed] [Google Scholar]
- 23. Strasberg SM, Brunt M. Rationale and use of the critical view of safety in laparoscopic cholecystectomy. J Am Coll Surg. 2010; 211: 132–138 [DOI] [PubMed] [Google Scholar]
- 24. Fletcher ER, Hobbs MS, Tan P, et al. Complications of cholecystectomy: risks of the laparoscopic approach and protective effects of operative cholangiography. A population based study. Ann Surg. 1999; 218: 371–379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ingraham AM, Cohen ME, KO CY, Hall BL. A current profile and assessment of North American cholecystectomy: Results from the American College of Surgeons National Surgical Improvement Program. J Am Coll Surg. 2010; 211: 176–186 [DOI] [PubMed] [Google Scholar]
- 26. Pfluke JM, Parker M, Stauffer JA, et al. Laparoscopic surgery performed through a single incision: A systematic review of the current literature. J Am Coll Surg. 2010; 212: 113–118 [DOI] [PubMed] [Google Scholar]
- 27. Lau KN, Sindram D, Agee N, Martinie JB, Iannitti DA. Bile duct injury after single incision laparoscopic cholecystectomy. JSLS. 2010; 14: 587–591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chiruvella A, SSarmiento JM, Sweeney JF, Lin E, Davis SS. Iatrogenic combined bile duct and right hepatic artery injury during single incision laparoscopic cholecystectomy. JSLS. 2010; 14: 268–271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Han H, Choi S, Kim WW, Choi S. Single incision multiport laparoscopic cholecystectomy. Arch Surg. 2011; 146: 68–74 [DOI] [PubMed] [Google Scholar]
- 30. Bunting DM. Port-site hernia following laparoscopic cholecystectomy. JSLS. 2010; 4: 490–497 [DOI] [PMC free article] [PubMed] [Google Scholar]