Summary
Introduction
Vertebral fractures have been associated with back pain, functional limitations and reduced health-related quality of life (HRQoL). Teriparatide is the first effective anabolic agent that demonstrated to significantly reduce the risk of vertebral fracture by 65%, as compared to placebo.
The aims of this study were to evaluate the effectiveness of teriparatide treatment on back pain-related functional limitations and to investigate on patients HRQoL.
Materials and methods
In this prospective observational pilot study osteoporotic patients, who were prescribed teriparatide therapy and a supplementation of calcium and vitamin D, were asked to answer to two self-administered questionnaires: the Spine Pain Index (SPI) and the SF-12 (at the recruitment, after 6, 12, and 18 months).
Results
Fifty-two women were evaluated (mean age of 70.58 yrs). The mean SPI score passed from 50.01 at baseline to 32.20 at 18 months. The mean SF-12 PCS score passed from 30.00 at baseline to 36.79 at 18 months, while the mean SF-12 MCS score was already within the normality range at baseline, constantly improving during the 18 months.
Conclusion
In conclusion, 18 months of treatment with teriparatide has to be considered an effective therapeutic option for women with severe osteoporosis and vertebral fractures, in a real-life clinical setting, to improve both back pain related disability and quality of life.
Keywords: osteoporosis, teriparatide, back-pain, functional limitation, health-related quality of life
Introduction
Bone fragility due to osteoporosis is common in elderly people and is associated with a high incidence of fractures, especially at the spine and hip. Vertebral fractures represent the most common of all osteoporotic fractures leading to increased mortality, morbidity and financial burden (1–5). Most of these fractures have been associated with back pain, functional limitations and reduced health-related quality of life (HRQoL) (6, 7). Chronic back pain and disability, caused by prevalent vertebral fractures, may be explained both by the biomechanical modifications of the spine and by the fourfold increased risk for new vertebral fractures in women who already have a fracture (8, 9). Each additional new vertebral fracture results in further functional limitations, therefore the use of proven therapies for preventing recurrent fractures is undoubtedly important to reduce the burden of back-related disability in osteoporotic patients.
Measurement of the disability due to back pain and health-related quality of life (HRQL) provide a more complete representation of an individual’s experience with osteoporosis (10). These assessments are increasingly seen as sources of further information on the efficacy of pharmacological therapies of chronic disabling diseases such as osteoporosis and its consequences.
Recently, several pharmacological treatments demonstrated their efficacy in decreasing the risk of fragility fractures, especially at the spine. Teriparatide, the human (1–34) PTH peptide, is the first effective anabolic agent that demonstrated to significantly reduce the risk of vertebral fracture by 65% and the risk of non-vertebral fracture by 53%, as compared to placebo (11, 12).
Furthermore, in the prospective European Forsteo Observational Study (EFOS), mean back pain measured by the visuo-analogic scale (VAS) in patients using teriparatide, was significantly reduced after 18 months of treatment (13). The greatest reduction in back pain occurred during the first 6 months of treatment. There was also a significant improvement in each of the five domains of the EuroQoL-5D. More recently, in the same population, it was shown that the changes in back pain seen during the treatment were maintained for at least 18 months after teriparatide discontinuation (14). Nevitt, in a meta-analysis on the effects of teriparatide on the risk of back pain in patients with osteoporosis, had already shown that patients randomized to teriparatide had a reduced risk of new or worsening back pain compared to patients randomized to placebo, hormone replacement therapy or alendronate (15). Adami et al. recently analysed in a review paper the cost-effectiveness of the use of teriparatide in severe osteoporotic patients, concluding that this is the only therapeutic option able to revert at least in part this disabling disease (16).
The role of teriparatide in reducing back pain has been widely demonstrated, however its role in reducing the osteoporosis related disability has not been well investigated yet. In fact there are no studies analyzing the relationship among reduction of back pain and functional limitations and HRQoL in osteoporotic patients treated with teriparatide.
Therefore, the primary aim of this prospective pilot study was to evaluate, in a subgroup of the Persistence and Adherence to Teriparatide Treatment Study (PATT) population (17), the effectiveness of teriparatide treatment on back pain-related functional limitations and the secondary endpoint was to investigate on HRQoL.
Materials and methods
This prospective observational pilot study was carried out in two of the sites recruiting patients for the PATT Study. Patients were prescribed teriparatide therapy (daily injection regimen) according to the Italian reimbursement criteria for osteoporosis, which requires diagnosis of severe osteoporosis (3 or more prevalent severe vertebral fractures; or 2 prevalent severe vertebral fractures and a historical hip fracture; or an incident vertebral fracture or hip fracture during treatment; or an antiresorptive treatment prescribed for prevalent hip or vertebral fracture assumed for at least 12 previous months) and a supplementation of 500–1000mg/day calcium and 400–800 IU/day vitamin D.
All patients signed an informed consent and this study was approved by the ethical committee of each site.
Assessment
A part from the clinical examination, the routine and bone-specific biochemical exams, the dorso-lumbar X-Ray, the lumbar and femoral BMD measurements by dual X-ray absorptiometry (DXA) required by the PATT protocol, patients from these 2 sites were also asked to answer to two self-administered questionnaires: the Spine Pain Index (SPI) (18) and the SF-12. Assessments were performed at the recruitment, after 6, 12, and 18 months.
The Spine Pain Index is a simple self-administered questionnaire investigating the impact of back pain on functional limitation and activities of daily living execution (Table 1). It combines the content of the Oswestry Low Back Disability Questionnaire and the Neck Disability Index in a format which reduces administrative burden. In fact it requires less than 5 minutes for a patient to complete it and about 20 seconds for a health care worker to score it. Moreover, this instrument can be used with cervical, thoracic or lumbar conditions, which reduces the need for multiple instruments for spine-related conditions. SPI has been tested, and the results have been published and presented at the “XXXI Italian Congress of Physical and Rehabilitation Medicine” (18). Based on the initial research, it demonstrates excellent reliability, validity, and responsiveness. The scale consists of ten items and the answer to each item is given by a visuo-analogical scale ranging from 0 to 10. The total score ranges from 0 (no pain or disability) to 100 (totally disabling back pain) and therefore it can be considered as a continuous variable.
Table 1.
Spine Pain Index.
| For answering the following questions please mark the appropriate point on the line with a cross which describes best your personal situation. During a typical day: | Score |
|---|---|
| 1. which is your back pain intensity? | 0–10 |
| 2. how much are you limited in the self care activities (washing, dressing, and so on) due to your back pain? | 0–10 |
| 3. how much does your back pain interfere with your sleep? | 0–10 |
| 4. how much does your back pain interfere with standing and/or sitting for a long period of time? | 0–10 |
| 5. how much does your back pain interfere with lifting objects? | 0–10 |
| 6. how much does your back pain interfere with your walking ability? | 0–10 |
| 7. how much does your back pain interfere with driving a car or taking public transportations? | 0–10 |
| 8. how much does your back pain interfere with your work? | 0–10 |
| 9. how much does your back pain interfere with your leisure activities? | 0–10 |
| 10. how much does you feel depressed due to your back pain? | 0–10 |
|
| |
| Total | 0–100 |
NOTE: For each question a 10 cm line VAS is provided.
SF-12, used to measure the perception of health related quality of life, is a self-administered questionnaire, developed and validated as a shorter alternative to SF-36 (19), which is the gold standard, among the generic measures, for the evaluation of perception of HRQoL. To calculate the physical composite (PCS) and the mental composite (MCS) scores, SF-12 items are scored and normalized by a standardized algorithm. PCS and MCS scores range from 0 to 100, with higher scores indicating better functioning. The MCS and PCS were designed to have a mean score of 50 and a standard deviation of 10 in a representative sample (20). SF-12 has been successfully tested in several European countries, including Italy, on large samples of the general population, where it has proved its comprehensiveness, reliability, validity and cross-cultural applicability (21).
Statistical analysis
Descriptive statistics such as frequencies, percentages, means, and standard deviations (SD) were used to describe the study population. Back pain related disability, and quality of life results were summarized over the teriparatide treatment period (6 and 12 months) and after completion of the 18 months of treatment. A one-way repeated measures ANOVA analysis was used to assess the changes over time.
According to “the treatment of symptomatic osteoporotic spinal compression fractures guideline and evidence report” by the American Academy of Orthopaedic Surgeons, we considered the effects of treatments in terms of the minimal clinically important improvement (MCII) in addition to whether their effects were statistically significant (22). As the Spine Pain Index can be assimilated to a pain VAS 0–100 scale we assumed that the minimal clinically important improvement was of 15 points.
Results
A total of 52 women were evaluated, with mean age of 70.58 yrs (min 50, max 87). Demographic data and baseline characteristics are reported in Table 2. Only 6 of the 52 women had already had a hip fracture before starting the treatment; 2 were intracapsular fractures and the others were trochanteric fractures. The mean number of vertebral fractures at baseline was 3.7 (min. 2, max. 10). No one had had surgical treatment of stabilization or verte-broplasty or kyphoplasty. During the 18 months treatment period there weren’t any new fractures.
Table 2.
Demographic and baseline characteristics of the population.
| Demographic data | Mean ± SD | Range |
|---|---|---|
| Age | 70.58±8.4 | 50–87 |
| BMI | 25.63±3.73 | 19.56–36.65 |
| Number of previous fractures per patients | ||
| - femoral (n of patients, % of patients) | 6 | 11.54% |
| - vertebral | 3.70±1.68 | 2–10 |
| Baseline assessment | ||
| SPI | 50.01±21.92 | 10.90–90.70 |
| SF-12 PCS | 30.00±8.55 | 16.70–50.20 |
| SF-12 MCS | 40.48±11.80 | 20.10–64.60 |
NOTE. Values are expressed as mean ± standard deviation (SD). Ranges are provided for continuous variables.
The mean Spine Pain Index score at baseline was 50.01 testifying for a relevant impact on back pain related disability.
The mean SF-12 PCS score at baseline was 30.00, while the mean SF-12 MCS score was 40.48 corresponding to a poor perception of the HRQoL regarding the physical composite and a normal perception of the HRQoL regarding the mental composite.
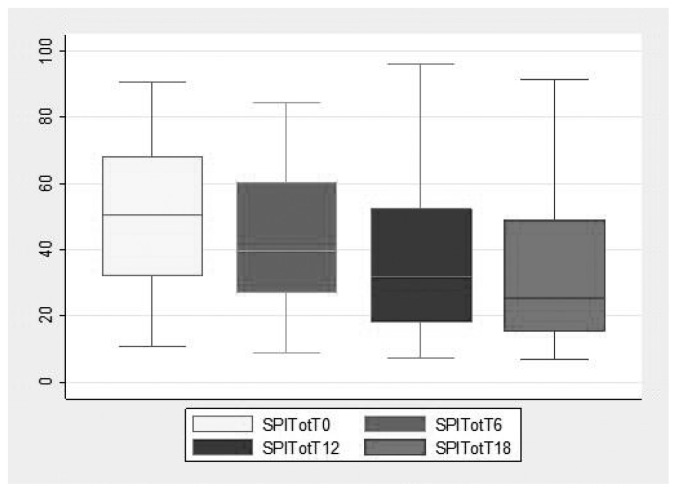
After starting the teriparatide treatment we have a continuous decrease at the back disability score during the 18 months, going from 50.01 at baseline to 32.20 at 18 months. The MCII (> 15 points) was already reached at the 12th month (Figure 1). The one-way repeated measures ANOVA analysis showed a p=0.004 at 12 months and p<0.0001 at 18 months.
Figure 1.
Box plot of the Spine Pain Index from baseline to the 18° month.
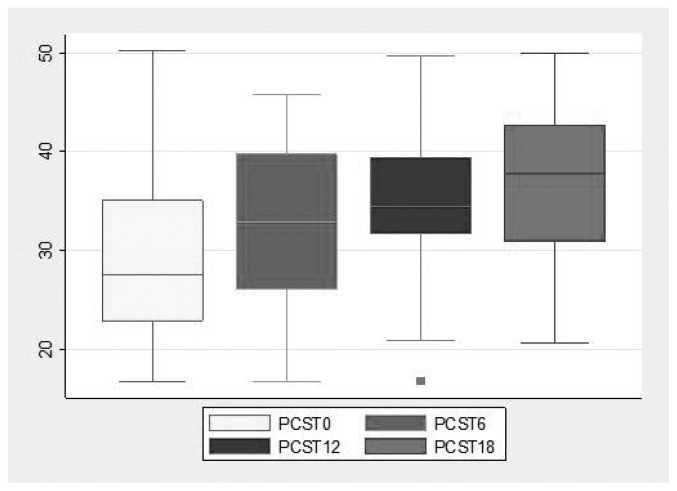
Figure 2 shows the constant improvement in the physical composite of the HRQoL during the 18 months, reaching a mean score of 36.79 at the last follow up. The one-way repeated measures ANO-VA analysis showed a p=0.013 at 12 months and p<0.0001 at 18 months.
Figure 2.
Box plot of the PCS SF-12 from baseline to the 18° month.
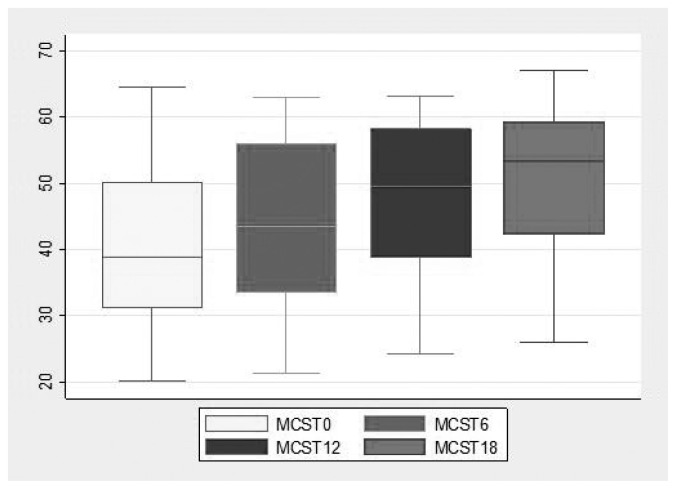
Figure 3 instead shows the mean scores of the SF-12 mental composite at the 4 time points that are always higher than 40, meaning that patients had a perception of acceptable quality of life for the mental composite. Nevertheless there was a constant improvement as shown by the one-way repeated measures ANO-VA analysis (p=0.016 at 12 months and p=0.001 at 18 months).
Figure 3.
Box plot of the MCS SF-12 from baseline to the 18° month.
Discussion
Vertebral fractures represent a huge health problem. They, frequently, cause a typical syndrome, characterized by back pain, functional limitation, height loss, changes in lung function, loss of self-esteem and depression. Back pain, and the resulting functional limitations are the major factors of the disability in activities of daily living in patients affected by fragility fractures.
Both factors correlate significantly with the number of vertebral fractures so that those individuals who have more than two vertebral fractures are likely to suffer more pain and greater disability.
Patients who are prescribed teriparatide are most frequently affected by severe osteoporosis with at least two vertebral fractures from medium to severe degree, according to the Genant score (23).
The efficacy of teriparatide in reducing the risk of new osteoporotic vertebral fractures has been well documented in randomized controlled trials (24). Also the effectiveness of this drug in reducing back pain and improving the quality of life in treated patients has been shown.
We conducted a pilot multicenter study with the primary aim of evaluating the effectiveness of the teriparatide treatment on back pain-related functional limitations in individuals affected by severe osteoporosis. In our sample, subjects treated with teriparatide were evaluated with a new assessment scale that examines the impact of pain to limit some activities of daily living. The results confirm the effectiveness of teriparatide in reducing back pain constantly over the 18 months time in patients with severe osteoporosis (more than two prevalent vertebral fractures). We considered a change of 15 points at the SPI as the threshold for the clinical significant improvement according to the recent guidelines of the AAOS. Our patients had a constant decrease in pain related disability during the teriparatide treatment period. This improvement resulted to be clinically and statistically significant starting from the 12th month.
The effectiveness of the drug in improving the perception of quality of life was measured by the SF-12 score that provide us information on both the physical and mental composites of HRQoL. As for the physical composite our pilot study showed that patients with severe osteoporosis experience a perception of poor quality of life due to the relevant impact of the vertebral fractures on their functional ability during the daily living activities. Even though teriparatide treatment does not vary the biomechanical factors of the pathogenesis of spine pain significantly, it reduces the incidence of new micro- and macro- fractures, and improves the bone structure and quality at the vertebral site, thus reducing pain and functional limitation and consequently patients perception of the physical component of quality of life.
The mean scores of the SF-12 mental composite of our patients show that even before starting the teriparatide treatment their perceived quality of life related to the psyco-emotional aspects was acceptable, although even for this aspect there was a constant and statistically significant improvement during the 18 months of treatment.
The main strength of observational studies is the applicability of the results to a general population. Our study was designed to enroll only subjects affected by severe osteoporosis according to the Italian reimbursement criteria for osteoporosis, which requires diagnosis of severe osteoporosis (3 or more prevalent severe vertebral fractures; or 2 prevalent severe vertebral fractures and a historical proximal hip fracture; or an incident vertebral fracture or hip fracture during treatment; or an antiresorptive treatment prescribed for prevalent hip or vertebral fracture assumed for at least 12 previous months) so it is not representative of general population of osteoporotic patients. Another limitation of the study is that our patients received a particular attention from the prescribing doctors (in terms of quality of information and motivations given to patients and frequency of visits) and this might have influenced the patients’ perception of quality of life. Furthermore being only a pilot study the number of patients recruited is too small to extrapolate definitive conclusions. However, the strength of the study is due to its real life setting with a population with several other diseases which could have negatively influenced the quality of life of our cohort.
In conclusion, in our pilot study it has been shown that 18 months of treatment with teriparatide is an effective therapeutic option for women with severe osteoporosis and vertebral fractures, in a real-life clinical setting, to improve both back pain related disability and quality of life. This drug seems to give a progressive and constant improvement of these two parameters all over the treatment period.
Acknowledgements
Contribution of the first and the last two authors have to be considered equal.
References
- 1.O’Neill TW, Felsenberg D, Varlow J, Cooper C, Kanis JA, Silman AJ. The prevalence of vertebral deformity in European men and women: the European Vertebral Osteoporosis Study. J Bone Miner Res. 1996;11:1010–1018. doi: 10.1002/jbmr.5650110719. [DOI] [PubMed] [Google Scholar]
- 2.Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359:1761–1767. doi: 10.1016/S0140-6736(02)08657-9. [DOI] [PubMed] [Google Scholar]
- 3.Hasserius R, Karlsson MK, Nilsson BE, Redlund-Johnell I, Johnell O. European Vertebral Osteoporosis Study: prevalent vertebral deformities predict increased mortality and increased fracture rate in both men and women: a 10-year population-based study of 598 individuals from the Swedish cohort in the European Vertebral Osteoporosis Study. Osteoporos Int. 2003;14:61–68. doi: 10.1007/s00198-002-1316-9. [DOI] [PubMed] [Google Scholar]
- 4.Ismail AA, O’Neill TW, Cooper C, Finn JD, Bhalla AK, Cannata JB, et al. Mortality associated with vertebral deformity in men and women: results from the European Prospective Osteoporosis Study (EPOS) Osteoporos Int. 1998;8:291–297. doi: 10.1007/s001980050067. [DOI] [PubMed] [Google Scholar]
- 5.Kanis JA, Oden A, Johnell O, Jonsson B, de Laet C, Dawson A. The burden of osteoporotic fractures: a method for setting intervention thresholds. Osteoporos Int. 2001;12(5):417–427. doi: 10.1007/s001980170112. [DOI] [PubMed] [Google Scholar]
- 6.Ettinger B, Black DM, Nevitt MC, Rundle AC, Cauley JA, Cummings SR, et al. Contribution of vertebral deformities to chronic back pain and disability: the study of Osteoporotic Fractures Research Group. J Bone Miner Res. 1992;7:449–456. doi: 10.1002/jbmr.5650070413. [DOI] [PubMed] [Google Scholar]
- 7.Nevitt MC, Ettinger B, Black DM, Stone K, Jamal SA, Ensrud K, et al. The association of radiographically detected vertebral fractures with back pain and function: a prospective study. Ann Intern Med. 1998;128:793–800. doi: 10.7326/0003-4819-128-10-199805150-00001. [DOI] [PubMed] [Google Scholar]
- 8.Lindsay R, Silverman SL, Cooper C, Hanley DA, Barton I, Broy SB, et al. Risk of new vertebral fracture in the year following a fracture. JAMA. 2001;285:320–323. doi: 10.1001/jama.285.3.320. [DOI] [PubMed] [Google Scholar]
- 9.Fechtenbaum J, Cropet C, Kolta S, Verdoncq B, Orcel P, Roux C. Reporting of vertebral fractures on spine X-rays. Osteoporos Int. 2005;16:1823–1826. doi: 10.1007/s00198-005-1939-8. [DOI] [PubMed] [Google Scholar]
- 10.Silverman SL, Cranney A. Quality of life measurement in osteoporosis. J Rheumatol. 1997;24(6):1218–21. [PubMed] [Google Scholar]
- 11.Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY, et al. Effect of parathyroid hormone (1–34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med. 2001;344(19):1434–41. doi: 10.1056/NEJM200105103441904. [DOI] [PubMed] [Google Scholar]
- 12.Gallagher JC, Genant HK, Crans GG, Vargas SJ, Krege JH. Teriparatide reduces the fracture risk associated with increasing number and severity of osteoporotic fractures. J Clin Endocrinol Metab. 2005;90(3):1583–7. doi: 10.1210/jc.2004-0826. Epub 2004 Dec 21. [DOI] [PubMed] [Google Scholar]
- 13.Rajzbaum G, Jakob F, Karras D, Ljunggren O, Lems WF, Langdahl BL, et al. Characterization of patients in the European Forsteo Observational Study (EFOS): postmenopausal women entering teriparatide treatment in a community setting. Curr Med Res Opin. 2008;24(2):377–84. doi: 10.1185/030079908x261087. [DOI] [PubMed] [Google Scholar]
- 14.Fahrleitner-Pammer A, Langdahl BL, Marin F, Jakob F, Karras D, Barrett A, et al. Fracture rate and back pain during and after discontinuation of teriparatide: 36-month data from the European Forsteo Observational Study (EFOS) Osteoporos Int. 2010 Nov 27; doi: 10.1007/s00198-010-1498-5. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nevitt MC, Chen P, Kiel DP, Reginster JY, Dore RK, Zanchetta JR, et al. Reduction in the risk of developing back pain persists at least 30 months after discontinuation of teriparatide treatment: a meta-analysis. Osteoporos Int. 2006;17(11):1630–7. doi: 10.1007/s00198-006-0177-z. [DOI] [PubMed] [Google Scholar]
- 16.Adami S, Brandi ML, Canonico PL, Minisola G, Minisola S, Tarantino U. Appropriate use of anabolic treatment for severe osteoporosis. Clin Cases Miner Bone Metab. 2010;7(2):114–122. [PMC free article] [PubMed] [Google Scholar]
- 17.Migliaccio S, Resmini G, Buffa A, Fornari R, Di Pietro G, Cerocchi I, et al. Evaluation of persistence and adherence to teriparatide treatment in patients affected by severe osteoporosis (patt): a multicenter observational real life study. doi: 10.11138/ccmbm/2013.10.1.056. Submitted to: International Journal of Clinical Practice. (Unpublished observations) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iolascon G, Gimigliano F, Gison A, Di Domenico F, Gimigliano R. Validazione di un nuovo score di disabilità da lombalgia: lo Spine Pain Index. Europa Medicophysica. 2003;39(suppl 1):600–603. [Google Scholar]
- 19.Ware JE. SF-36 Health Survey manual and interpretation guide. Boston: The Health Institute, New England Medical Center; 1993. [Google Scholar]
- 20.Ware J, Kosinski M, Keller S. How to score the SF-12 physical and mental health summary scales. 2nd edn. Boston, MA: The Health Institute; 1995. [Google Scholar]
- 21.Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, et al. Cross-validation of items selection and scoring for the SF-12 Health Survey in 9 countries: results from the IQOLA project. J Clin Epidemiol. 1998;51:1171–1178. doi: 10.1016/s0895-4356(98)00109-7. [DOI] [PubMed] [Google Scholar]
- 22.McGuire R. AAOS Clinical Practice Guideline: the Treatment of Symptomatic Osteoporotic Spinal Compression Fractures. J Am Acad Orthop Surg. 2011;19(3):183–4. doi: 10.5435/00124635-201103000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Genant HK, Wu CY, van Kuijk C, Nevitt MC. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res. 1993;8:1137–1148. doi: 10.1002/jbmr.5650080915. [DOI] [PubMed] [Google Scholar]
- 24.Gallagher JC, Genant HK, Crans GG, Vargas SJ, Krege JH. Teriparatide reduces the fracture risk associated with increasing number and severity of osteoporotic fractures. J Clin Endocrinol Metab. 2005;903:1583–7. doi: 10.1210/jc.2004-0826. [DOI] [PubMed] [Google Scholar]