Summary
Objective
The ADVICE (ADherence in VItamin-D and Calcium Embedded or not) survey was aimed to evaluate the effect of a patient-focused motivation strategy on the adherence to calcium and vitamin D supplementation. The survey also intended to identify possible factors being able to influence the compliance (i.e. the existence of individual preferences towards different dosages or regimens of supplementation).
Methods
We planned to involve consecutive patients visited between 2010 and 2011 at 35 centres specialized in diagnosis and treatment of osteoporosis in different Italian regions. Each patient has been requested to declare if he/she was already assuming any supplementation with calcium and vitamin D (naïve or not naïve). All patients underwent a first visit (T0) and two follow up visits at 6 and 12 months (T6 e T12). The assessment of the adherence was measured through the Morinsky Medication Adherence Scale, a score based on 8 different questions, specifically validated to determine therapeutical compliance (0–5: not acceptable; 6–7: acceptable; 8: ideal).
Results
732 women (mean age: 66.9; average BMI: 25.3) and 30 men (mean age: 71.9; average BMI: 24.5) were enrolled; 34% of female patients (n=245) and 66% of males (n=20) reported previous fractures. Not naïve patients were 385 (54%). A total of 309 patients (43%) were concurrently assuming an antifracture drug; 229 subjects were osteoporotic (45%), while 224 were osteopenic (44%). The mean Morinsky score in not naïve patients was 5.72, 6.19 and 6.18 at T0, T6, and T12, respectively. Thus, no differences in the Morinsky score were observed between T6 and T12. Naïve patients showed an average Morinsky score of 5.78 at T6 and 6.39 at T12. Older age was not significantly associated with the observed changes in the scores. The onset of AEs related to the supplementation with calcium and vitamin D was able to negatively influence the adherence at the subsequent control point. Bone mineral density, previous fractures, and concurrent assumption of any antifracture drug did not significantly influence the adherence, as well as the differences in the dosages or regimens of calcium and vitamin D administration.
Conclusion
Activities aimed to strengthen motivation of the patients improved the adherence to calcium and vitamin D supplementations after only 6 months.
Keywords: calcium and vitamin D supplementation, compliance, motivation, preference
Introduction
Osteoporosis is a chronic systemic skeletal disorder characterized by low bone density and micro-architectural deterioration resulting in increased susceptibility to fragility fractures (1). Therapeutical options currently available for osteoporosis prevention and treatment include supplementation with calcium and vitamin D, as many studies suggest that they might be effective in increasing Bone Mineral Density (BMD) and reducing the risk of falls or osteoporotic fractures (2–12). Since there is no evidence of any negative effect on cardiovascular risk (13, 14), supplementation with calcium and vitamin D is widely prescribed alone or in combination with antiresorptive and anabolic drugs in daily clinical practice for the treatment/prevention of osteoporosis and fragility fractures (15, 16). As it happens for any therapy, compliance is the most important factor affecting the effectiveness of calcium and vitamin D supplementations. Actually, results from community-based trials in which the adherence to the supplementation was moderate or low have often been negative, whereas studies carried out on institutionalized patients with supervised pill administration resulted in significant benefits (17). According to recent studies, compliance to long calcium and vitamin D supplementations ranges between 20% and 60% (18–20). In this perspective, the ADVICE (ADherence in VItamin-D and Calcium Embedded or not) survey was aimed to evaluate the effect of a patient-focused motivation strategy (consisting in follow-up visits scheduled every 6 months) on the 1 year adherence to calcium and vitamin D supplementation. At the same time, we aimed to identify possible factors that are able to influence patients compliance, such as personal preferences towards specific dosages or regimens in assuming the supplementation.
Methods
The survey was designed to involve consecutive patients visited between 2010 and 2011 at 35 centres specialized in diagnosis and treatment of osteoporosis in different Italian regions. For each patient, detailed anamnestic and clinical information have been collected (including T-score and laboratory tests). Each patient has been requested to declare if he/she was already assuming any supplementation with calcium and vitamin D before the inclusion in the survey. All patients underwent a first visit (T0) and two follow up visits at 6 and 12 months (T6 e T12). During the follow up visits, physicians carefully registered any changes in clinical information. Particularly, adverse events (AEs) possibly related to the administration of calcium and vitamin D supplementations or antifracture drugs concurrently taken by the patients were reported. The assessment of the adherence was measured at each control point (and also at the time of the enrolment in case of patients not naïve to supplementation with calcium and vitamin D) by using the Morinsky Medication Adherence Scale, a score based on 8 different questions, already validated and specifically used (19) to determine therapeutical compliance to the treatments for osteoporosis (0–5: not acceptable compliance; 6–7: acceptable compliance; 8: ideal compliance). Descriptive and inferential statistical analyses (including t-test, ANOVA) were performed; multivariate models were implemented to test the association between the compliance levels and the main variables.
Results
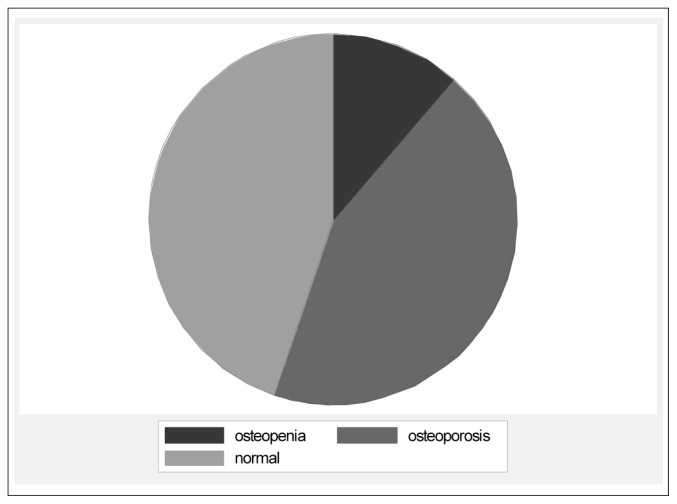
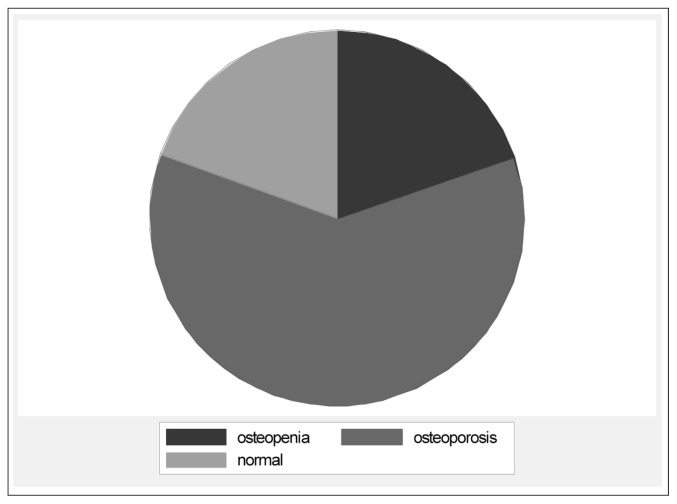
As resumed in Table 1, we have enrolled a total of 732 women (mean age: 66.9; average BMI: 25.3) and 30 men (mean age: 71.9; average BMI: 24.5), where 34% of female patients (n=245) and 66% of males (n=20) reported previous fractures caused by low energy traumas. Patients who had already taken calcium and vitamin D (not naïve patients) were 385 (54%). Patients who never assumed calcium and vitamin D supplementations (naïve patients) were 329 (46%). A total of 65 not naive patients (18%) declared at the time of the enrolment (T0) that they had already experienced AEs possibly related to the supplementation with calcium and vitamin D. A total of 309 patients both in not naïve and in naive groups (43%) were concurrently assuming an antifracture drug (bisphosphonates or any other). Concerning the evaluation of bone mineral density (BMD), DXA (X-ray densioabsorbiometry) data were available for 511 subjects (Figures 1A, 1B). Specifically, 229 subjects were found to be osteoporotic (45% of the overall enrolled population), while 224 were osteopenic (44% of the total). In women, the average Lumbar Spine (LS) T-score was −2.3 SD, with total hip (TH) T-score showing a mean value of −1.8 (average LS and TH T-score were −2.5 and −2.0 in men, respectively). The mean scores resulting from the Morinsky scale in not naïve patients were 5.72, 6.19 and 6.18 at T0, T6, and T12, respectively. Thus, no differences in the Morinsky score were observed between T6 and T12. Naïve patients showed an average Morinsky score of 5.78 at T6 and 6.39 at T12. Therefore, the adherence to supplementations with calcium and vitamin D was found to increase in both groups, as the Morinsky score passed from values of low compliance (0–5) to a level of acceptability (6–7), with this variation reaching statistical significance (p<0.01). In both groups, almost the same number of patients remained in the range of acceptable or ideal compliance at the subsequent control point (Table 2 and Table 3). Older age was not significantly associated with the observed improvements in the Morinsky scores with the only exception of not naïve patients. In these latter subject, for each year of age, an increase of 0.022 points in the adherence was noted between T0 and T6 (p<0.05; IC95%: 0.001–0.043); in other words, as older was the patient, more remarkable increases in the adherence to supplementations were recorded. The onset of AEs related to the supplementation with calcium and vitamin D was able to negatively influence the adherence at the subsequent control point, and this finding was statistically significant (p<0.05). Bone mineral density (i.e. being osteoporotic), previous fractures, and the concurrent assumption of any antifracture drug did not significantly influence the adherence to supplementation, as well as the differences in the dosages or regimens of calcium and vitamin D administration.
Table 1.
Main baseline characteristics of the population involved in the survey.
| Men (n=30) | Women (n=732) | |
|---|---|---|
| Mean age | 71,6 | 66,9 |
| BMI (average) | 24,5 | 25,3 |
| Previous fracture (low energy trauma) | 20 (66%) | 245 (34%) |
| Previous calcium and/or vit. D supplementation (not naïve) | 11 (38%) | 385 (54%) |
| Previous antifracture therapy | 13 (45%) | 309 (44%) |
Figure 1A.
Frequency of lumbar spine osteoporosis and osteopenia in the study population.
Figure 1B.
Frequency of femoral osteoporosis and osteopenia in the study population.
Table 2.
Distribution of not naïve patients among the three Morinsky score classes.
| Visit | 0–5 (Low compliance) | 6–7 (Acceptable) | 8 (Ideal) | Patients with these data available (n) |
|---|---|---|---|---|
| T0 | 157 (42%) | 127 (34%) | 88 (24%) | 372 |
| T6 | 103 (28%) | 173 (47%) | 92 (25%) | 368 |
| T12 | 90 (28%) | 141 (44%) | 92 (28%) | 323 |
Table 3.
Distribution of naïve patients among the three Morinsky score classes.
| Visit | 0–5 (Low compliance) | 6–7 (Acceptable) | 8 (Ideal) | Patients with these data available (n) |
|---|---|---|---|---|
| T6 | 129 (42%) | 82 (27%) | 93 (31%) | 304 |
| T12 | 73 (28%) | 85 (33%) | 100 (39%) | 258* |
Data missing for 46 patients between T6 and T12.
Discussion
This study points out the importance of fostering patients motivation at the moment they are prescribed with a calcium and vitamin D supplementation, as already suggested by other authors (21). Zafran et al. have already suggested that physician attitude to push the awareness of their patients on the benefits of the treatment and the risks related to a bad compliance is a crucial factor (22). Actually, significant difference in terms of acceptability of patients compliance were showed in our analyses between the time of the enrolment in the survey – which represented a motivation strategy itself – and the subsequent follow-up visit. At the same time, having found that in not naïve patients there were no further improvements in terms of compliance between T6 and T12, underline how it is important not to lose the opportunity of making the patient aware about his/her compliance to the therapy at the time of the first visit. From this survey, it also comes out that older patients are not more compliant than younger ones to calcium and vitamin D supplementation, with the only exception of not naïve patients between T0 and T6 (but not between T6 and T12). This exception in subjects who declared to be already on treatment with a supplementation could support the crucial role of fostering patients motivation, especially in older age groups. Compliance did not increase in case of concurrent assumption of antifracture drugs, low bone mineral density (both osteopenia and osteoporosis) or previous fractures. These results are of particular interest because antifracture drugs are usually prescribed together with calcium and/or vitamin D supplementation, thus we were expecting that patients simultaneously treated with antiresorptive or anabolic agents for their osteoporosis would have higher compliance to the supplementation. The same for patients who had already been diagnosed with osteoporosis or osteopenia.
As expected, the onset of adverse events related to the supplementation with calcium and vitamin D (or perceived by the patients as being due to it) significantly influenced in a negative way the compliance monitored at the subsequent control point (after 6 months).
Another interesting issue directly addressed in the design of the study was the hypothesis that different dosages or regimens of calcium and vitamin D supplementation could be associated to different level of compliance (as measured through the Morinsky scale), being influenced by individual preferences. Actually, in daily clinical practice, physicians may prescribe calcium and vitamin D alone or combined by using about hundred combinations of doses, pharmaceutical formulations, and intervals of administration. Although quite interesting and possibly rationale, this hypothesis has not been confirmed in this study as we were not able to observe statistically significant differences in terms of compliance. It must be pointed out that some dosages or regimens of calcium and vitamin D supplementation consisted in very small number of patients, but no influence on the compliance was observed neither in the most frequent formulations, regimes or doses of the medications.
It is obviously impossible to extensively apply to other major chronic diseases the findings of this survey carried out on calcium and vitamin D supplementation to other kind of therapies, but emphasizing the importance of being compliant with medical prescriptions it is something crucial in case of long term treatments such as those used for the prevention of osteoporosis and fractures (23). It is indubitable that the best opportunity (often the only one) to do that is at the moment of the first contact between the physician and the patient, as resulted from our survey on calcium and vitamin D supplementation. A recent study carried out in Florida showed the effectiveness of such strategy as verbal counseling and electronic prescription in fostering patients compliance to supplementation with calcium and vitamin D (24).
Conclusion
Specific activities aimed to strengthen motivation of the patients – as those carried out in the present survey by scheduling periodic follow-up visits every 6 months – seem to improve the adherence to calcium and vitamin D supplementations after only 6 months. This effect has been highlighted both in not naïve and naïve patients and it seems to reach a maximal level of plateau within the first six months.
Acknowledgements and disclosures
This study has been supported by the Italian Society for Orthopaedics and Medicine (OrtoMed).
Contributors to the ADVICE survey: Parma A. - Trieste; Braga V. - Verona; Bertoli M. - Padova; Cossu R. - Bologna; Annovi M. - Modena; Caffetti M.C. - Voghera; Delfitto M. - Voghera; Delvino PG. - Vercelli; Mosconi S. - Bergamo; Falchetti A. - Firenze; Marin G. - Firenze; Zoppi P. - Sarzana (SP); Conti F. - Roma; Santonati A. - Roma; Chiatti R. - Roma; Ruggiero C. - Perugia; Filipponi P. - Perugia; Gennari L. - Siena; La Malfa D. - Piombino (LI); Scendoni P. - Fermo; Capone A. - Cagliari; Ruiu F. - Nuoro; Sozzi G. - Urbino (PU); Di Salvo F. - Palermo; Letizia Mauro G. - Palermo; Russo E. - Messina; D’Avola G. - Catania; Iolascon G. - Napoli; Tripodi F. - Salerno; Colì G. - Gallipoli (LE); Muratore M. - San Cesareo (LE); Italiano G. - Caserta; Forlenza R. - Potenza; Castellitto D. - Frosinone.
References
- 1.NIH Consensus Development Panel on Osteoporosis. Prevention, Diagnosis and Therapy Consensus Conference. JAMA. 2001;285:785–795. doi: 10.1001/jama.285.6.785. [DOI] [PubMed] [Google Scholar]
- 2.Boonen S, Vanderschueren D, Haentjens P, Lips P. Calcium and vitamin D in the prevention and treatment of osteoporosis - a clinical update. J Intern Med. 2006 Jun;259(6):539–52. doi: 10.1111/j.1365-2796.2006.01655.x. [DOI] [PubMed] [Google Scholar]
- 3.Gatto S, Gimigliano F, Gimigliano R, Iolascon G. Prevention of falls and role of calcium and vitamin D. Aging Clin Exp Res. 2011 Apr;23(2 Suppl):20–1. [PubMed] [Google Scholar]
- 4.Baeksgaard L, Andersen KP, Hyldstrup L. Calcium and vitamin D supplementation increases spinal BMD in healthy, postmenopausal women. Osteoporos Int. 1998;8(3):255–60. doi: 10.1007/s001980050062. [DOI] [PubMed] [Google Scholar]
- 5.Häuselmann HJ, Rizzoli R. A comprehensive review of treatments for postmenopausal osteoporosis. Osteoporos Int. 2003 Jan;14(1):2–12. doi: 10.1007/s00198-002-1301-3. [DOI] [PubMed] [Google Scholar]
- 6.Bischoff-Ferrari HA, Willett WC, Wong JB, Giovannucci E, Dietrich T, Dawson-Hughes B. Fracture prevention with vitamin D supplementation: a meta-analysis of randomized controlled trials. JAMA. 2005 May11;293(18):2257–64. doi: 10.1001/jama.293.18.2257. [DOI] [PubMed] [Google Scholar]
- 7.Boonen S, Rizzoli R, Meunier PJ, Stone M, Nuki G, Syversen U, Lehtonen-Veromaa M, Lips P, Johnell O, Reginster JY. The need for clinical guidance in the use of calcium and vitamin D in the management of osteoporosis: a consensus report. Osteoporos Int. 2004 Jul;15(7):511–9. doi: 10.1007/s00198-004-1621-6. [DOI] [PubMed] [Google Scholar]
- 8.Nurmi-Lüthje I, Lüthje P, Kaukonen JP, Kataja M, Kuurne S, Naboulsi H, Karjalainen K. Post-fracture prescribed calcium and vitamin D supplements alone or, in females, with concomitant anti-osteoporotic drugs is associated with lower mortality in elderly hip fracture patients: a prospective analysis. Drugs Aging. 2009;26(5):409–21. doi: 10.2165/00002512-200926050-00005. [DOI] [PubMed] [Google Scholar]
- 9.Roux C, Bischoff-Ferrari HA, Papapoulos SE, de Papp AE, West JA, Bouillon R. New insights into the role of vitamin D and calcium in osteoporosis management: an expert roundtable discussion. Curr Med Res Opin. 2008 May;24(5):1363–70. doi: 10.1185/030079908x301857. Epub 2008 Apr 2. Review. [DOI] [PubMed] [Google Scholar]
- 10.Boonen S, Bischoff-Ferrari HA, Cooper C, Lips P, Ljunggren O, Meunier PJ, Reginster JY. Addressing the musculoskeletal components of fracture risk with calcium and vitamin D: a review of the evidence. Calcif Tissue Int. 2006 May;78(5):257–70. doi: 10.1007/s00223-005-0009-8. Epub 2006 Apr 21. [DOI] [PubMed] [Google Scholar]
- 11.Kärkkäinen MK, Tuppurainen M, Salovaara K, Sandini L, Rikkonen T, Sirola J, Honkanen R, Arokoski J, Alhava E, Kröger H. Does daily vitamin D 800 IU and calcium 1000 mg supplementation decrease the risk of falling in ambulatory women aged 65–71 years? A 3-year randomized population-based trial (OSTPRE-FPS) Maturitas. 2010 Apr;65(4):359–65. doi: 10.1016/j.maturitas.2009.12.018. Epub 2010 Jan 8. [DOI] [PubMed] [Google Scholar]
- 12.Flicker L, MacInnis RJ, Stein MS, Scherer SC, Mead KE, Nowson CA, Thomas J, Lowndes C, Hopper JL, Wark JD. Should older people in residential care receive vitamin D to prevent falls? Results of a randomized trial. J Am Geriatr Soc. 2005 Nov;53(11):1881–8. doi: 10.1111/j.1532-5415.2005.00468.x. [DOI] [PubMed] [Google Scholar]
- 13.Heaney RP, Kopecky S, Maki KC, Hathcock J, Mackay D, Wallace TC. A review of calcium supplements and cardiovascular disease risk. Adv Nutr. 2012 Nov 1;3(6):763–71. doi: 10.3945/an.112.002899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Avenell A, MacLennan GS, Jenkinson DJ, McPherson GC, McDonald AM, Pant PR, Grant AM, Campbell MK, Anderson FH, Cooper C, Francis RM, Gillespie WJ, Robinson CM, Torgerson DJ, Wallace WA. RECORD Trial Group, Long-term follow-up for mortality and cancer in a randomized placebo-controlled trial of vitamin D(3) and/or calcium (RECORD trial) Clin Endocrinol Metab. 2012 Feb;97(2):614–22. doi: 10.1210/jc.2011-1309. Epub 2011 Nov 23. [DOI] [PubMed] [Google Scholar]
- 15.Marcus R, Wong M, Heath H, 3rd, Stock JL. Antiresorptive treatment of postmenopausal osteoporosis: comparison of study designs and outcomes in large clinical trials with fracture as an endpoint. Endocr Rev. 2002 Feb;23(1):16–37. doi: 10.1210/edrv.23.1.0453. [DOI] [PubMed] [Google Scholar]
- 16.Meunier PJ. Anabolic agents for treating postmenopausal osteoporosis. Joint Bone Spine. 2001 Dec;68(6):576–81. doi: 10.1016/s1297-319x(01)00329-3. [DOI] [PubMed] [Google Scholar]
- 17.Lips P, Bouillon R, van Schoor NM, Vanderschueren D, Verschueren S, Kuchuk N, Milisen K, Boonen S. Reducing fracture risk with calcium and vitamin D. Clin Endocrinol (Oxf) 2010 Sep;73(3):277–85. doi: 10.1111/j.1365-2265.2009.03701.x. [DOI] [PubMed] [Google Scholar]
- 18.Castelo-Branco C, Cortés X, Ferrer M. Treatment persistence and compliance with a combination of calcium and vitamin D. Climacteric. 2010 Dec;13(6):578–84. doi: 10.3109/13697130903452804. Epub 2009 Dec 1. [DOI] [PubMed] [Google Scholar]
- 19.Sanfelix-Genovés J, Gil-Guillén VF, Orozco-Beltran D, Giner-Ruiz V, Pertusa-Martínez S, Reig-Moya B, Carratalá C. Determinant factors of osteoporosis patients’ reported therapeutic adherence to calcium and/or vitamin D supplements: a cross-sectional, observational study of postmenopausal women. Drugs Aging. 2009;26(10):861–9. doi: 10.2165/11317070-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 20.Díez A, Carbonell C, Calaf J, Caloto MT, Nocea G. Observational study of treatment compliance in women initiating antiresorptive therapy with or without calcium and vitamin D supplements in Spain. Menopause. 2012 Jan;19(1):89–95. doi: 10.1097/gme.0b013e318223bd6b. [DOI] [PubMed] [Google Scholar]
- 21.Berry SD, Misra D, Hannan MT, Kiel DP. Low acceptance of treatment in the elderly for the secondary prevention of osteoporotic fracture in the acute rehabilitation setting. Aging Clin Exp Res. 2010 Jun;22(3):231–7. doi: 10.1007/bf03324801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zafran N, Liss Z, Peled R, Sherf M, Reuveni H. Incidence and causes for failure of treatment of women with proven osteoporosis. Osteoporos Int. 2005 Nov;16(11):1375–83. doi: 10.1007/s00198-005-1838-z. Epub 2005 Apr 2. [DOI] [PubMed] [Google Scholar]
- 23.Netelenbos JC, Geusens PP, Ypma G, Buijs SJ. Adherence and profile of non-persistence in patients treated for osteoporosis--a large-scale, long-term retrospective study in The Netherlands. Osteoporos Int. 2011 May;22(5):1537–46. doi: 10.1007/s00198-010-1372-5. Epub 2010 Sep 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hill DA, Cacciatore M, Lamvu GM. Electronic prescribing influence on calcium supplementation: a randomized controlled trial. Am J Obstet Gynecol. 2010 Mar;202(3):236.e1–5. doi: 10.1016/j.ajog.2009.10.886. Epub 2009 Dec 30. [DOI] [PubMed] [Google Scholar]