Abstract
Background
Foreign-body ingestion is a common event most often seen in children from 6 months to 6 years of age. In adults, foreign bodies are usually ingested accidentally together with food. This happens more commonly in persons with certain pathological changes of the gastrointestinal tract.
Methods
We present a selective review of pertinent literature retrieved by a search in the PubMed database.
Results
The foreign bodies most commonly ingested by adults are fish bones and chicken bones. The clinical approach to the problem depends on the type of material ingested and on the patient’s symptoms and physical findings. In about 80% of cases, the ingested material passes uneventfully through the gastrointestinal tract; endoscopy is performed in about 20% of cases, and surgery in less than 1%. Emergency esophagogastroduodenoscopy (EGD) is recommended when the esophagus is completely occluded (because of the risk of aspiration and/or pressure necrosis), when the ingested object has a sharp point or edge (because of the risk of perforation, with ensuing mediastinitis or peritonitis), and when a battery has been ingested (because of the risk of necrosis and fistula formation). For non-occluding esophageal foreign bodies, including magnets, an urgent but non-emergency EGD within 12 to 24 hours is recommended.
Conclusion
Most patients can be treated conservatively by observation alone, but there should be a low threshold for deciding to proceed to endoscopic retrieval. Surgery is reserved for complicated cases.
Treating patients with ingested foreign bodies is common in clinical practice. A distinction is made between accidental ingestion of a foreign body and intentional ingestion with secondary gain. Furthermore, a bolus may become stuck during ingestion of food, resulting in the clinical presentation of a foreign body impacted in the esophagus.
Swallowing of foreign bodies is most common in children aged between 6 months and 6 years (1, 2). In adults, foreign body impactions are mostly seen in the context of a pre-existing pathology. Sung et al reported the following causes for impaction (3):
Strictures (about 37%)
Malignancy (about 10%)
Esophageal rings (about 6%)
Achalasia (about 2% of cases).
Eosinophilic esophagitis, which has a secondary role in foreign body impaction, has been described in up to 33% of cases of bolus impaction (4). However, in some cases no pathological predisposition is present. Furthermore, more cases of ingested foreign bodies are reported in patients of advanced age, those with mental retardation, and with psychiatric disorders (5). The physiologically and anatomically narrow parts of the gastrointestinal tract make the passage of the ingested body difficult and are predilected sites for foreign body impaction (1, 5).
According to the available data, frequencies of swallowed foreign bodies vary widely. The foreign bodies most commonly swallowed by adults are (3, 6, 7):
Fish bones (9–45%)
Bones (8–40%)
Dentures (4–18%).
Longstreth et al. reported an annual prevalence for bolus impaction as an independent subentity of 13/100 000 (8).
As long as no occlusion and/or other complications develop, the clinical signs are not necessarily dramatic and may even be lacking. Most patients present with the sensation of a foreign body, difficulty in swallowing, chest or abdominal pain, or vomiting (6).
The foreign body is passed naturally in some 80% of cases. In 20% of cases, endoscopic intervention is indicated. Surgical intervention is indicated in less than 1% of cases (1, 3, 5– 7, 9). In spite of the mostly benign natural course, ingestion of foreign bodies is associated with increased morbidity. In the USA alone, some 1500 deaths are reported every year (10).
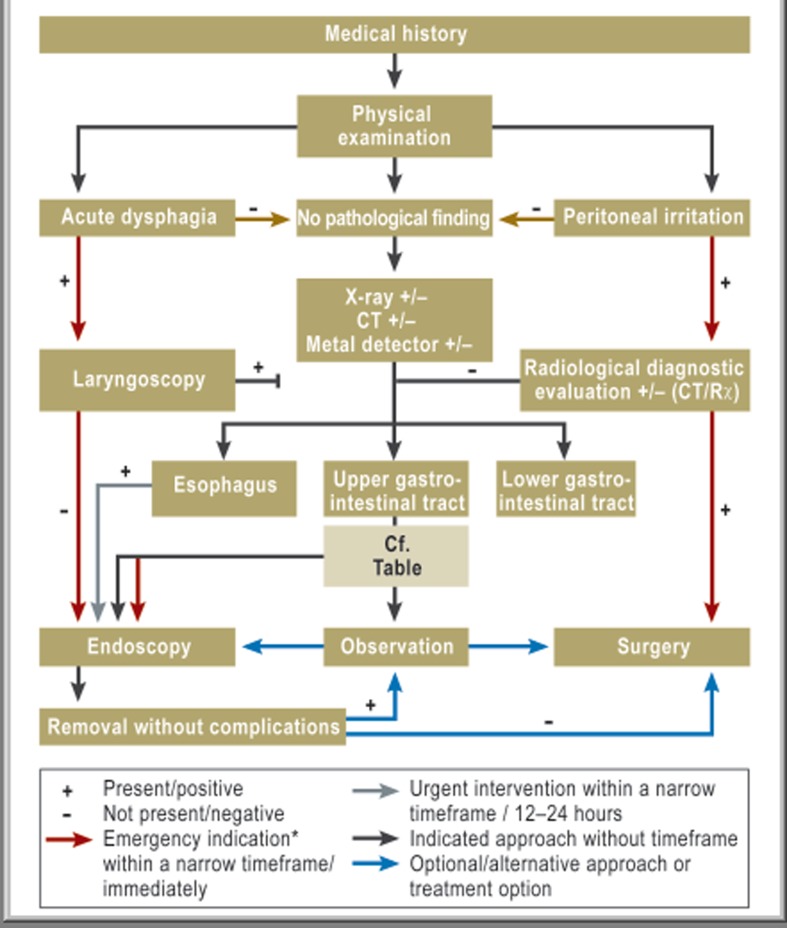
This article aims to provide a diagnostic and therapeutic algorithm (Figure 2) for the evaluation and treatment of a swallowed foreign body in the gastrointestinal tract in adults. Information on the management of ingested foreign bodies in the respiratory tract and in children can be obtained from articles written by specialists in ear, nose, and throat (ENT) and pediatrics (11, 12).
Figure 2.
Diagnostic and therapeutic algorithm in patients who have ingested foreign bodies; *cf. Table
Method
In order to compile this review article we conducted a selective literature search in PubMed (last accessed on 22 September 2012). 135 articles matched our search term “foreign body ingestion AND adult NOT child NOT case report”. Restricting the search to include only articles in English reduced the number of matches to 55 articles.
After excluding articles on intentional ingestion of foreign bodies and studies with fewer than 10 patients, we were left with 24 publications. Using the search terms “ingested foreign bodies” and “food bolus impaction” with the same settings in PubMed, we selected 15 and 18 more articles, respectively. We also filtered out 16 articles on the “body packing syndrome”.
Because data from randomized studies are lacking, we based our article exclusively on retrospective publications, reviews, and recommendations from medical specialty societies.
Categorizing ingested foreign bodies
It seems sensible to categorize ingested bodies by material, size, surface consistency, and chemical composition, because these characteristics help to determine the urgency of any intervention (1, 5, 13). The passage through the duodenum depends on the diameter as well as the length of the ingested foreign body. Foreign bodies longer than 6 cm and with a diameter of more than 2.5 cm make the duodenal passage difficult (9, 14). In our opinion, further categorization of ingested foreign bodies by radio density also makes sense. The Box provides a systematic categorization of foreign bodies; this will be used as the basis for developing a diagnostic and therapeutic algorithm.
Box. Classification of foreign bodies.
-
Size
Length greater/smaller than 6 cm
-
Surface consistency
Sharp/pointed versus blunt
Rounded versus sharp edges
-
Material/contents, for example
Food
Drugs
Battery
Magnet
-
Characteristics
Radio-dense+/-
Metallic+/-
Chemically inert +/-
Diagnostic evaluation
Patients usually seek medical attention after ingesting a foreign body and provide information about the foreign body. Furthermore patients may point out the possible location of ingested bodies (15). According to Connolly et al. (16) this does not always correspond with the actual location of the foreign body. The physical examination should therefore not be restricted to the symptomatic region. In some cases the diagnosis of an ingested foreign body is made days or months after the body was ingested (e1).
The diagnosis of an ingested foreign body is made primarily on the basis of the patient’s medical history. This means that the type of diagnostic evaluation and the extent and urgency of a possible intervention are decided on the basis of the information gained about the ingested foreign body, subjective complaints, and the clinical findings (1, 5, 6, 9, e2).
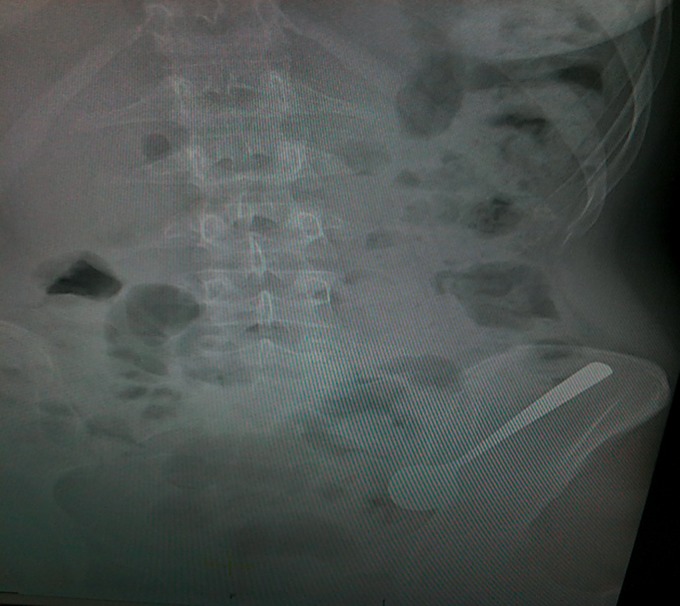
Radiography of the affected region of the body, on two planes if required, has been recommended by many authors as an initial screening method (e3, e4). Mosca et al. confirmed a positive finding in 144 of 414 patients with ingested foreign bodies on the basis of x-ray films (17). Such images make it possible to gain information not only on the location of the ingested body, but mostly also about the configuration, number, and size of the ingested foreign bodies. Furthermore they may indicate complicated courses with perforation—for example pneumoperitoneum or pneumomediastinum (Figure 1).
Figure 1.
Abdominal x-ray with a foreign body (a spoon) in the left lower abdomen
We support this approach if the foreign body is suspected to be radiodense. In our opinion, imaging in the context of the diagnostic evaluation helps not only to confirm the diagnosis but also contributes to documenting the findings.
For non-radiodense and some radiodense foreign bodies, native x-ray examination is mostly not sufficient to exclude ingestion of a foreign body. Ngan and colleagues showed a sensitivity of only 32% and a specificity of 91% for ingested fish bones in native x-ray films of 354 patients (18). Although small foreign bodies, such as fish bones and chicken bones are dense enough to show in the radiograph, they may be concealed by fluids and soft tissue mass (19, 20). Such foreign bodies can be excellently identified by using computed tomography (CT) scanning, as shown by Coulier et al. (20). With a sensitivity of 100% and a specificity of 91%, CT has an important role in the diagnostic evaluation of ingested foreign bodies (21).
Some authors have advised against using contrast medium in the setting of radiological diagnostic evaluation, because of the risk of aspiration, reduced ability to assess the mucosa, and possible concealment/masking of the ingested body (1, 5, 9).
The use of ultrasonography to diagnose ingested foreign bodies seems uncommon. This is confirmed by the limited number of published case reports (22). The largest series in an adult cohort was published by Coulier in 1997 and included only six patients (23). This also shows how rarely ultrasonography is used to detect ingested foreign bodies.
Some authors have described using metal detectors to diagnose swallowed foreign bodies (24, 25). Sacchetti et al. found a sensitivity of 94% and a specificity of 100% for metal detectors used to identify metal foreign bodies (25). The method is cheap, can be repeated as often as required, and does not entail radiation. Although metal detectors are used primarily in children, Ryan et al. recommend extensive application of this simple diagnostic instrument in adults too (24). In our opinion this approach does not yield any tangible information and is hardly used in adults in clinical practice.
It is important that imaging is performed directly before any planned intervention since the position of the ingested body may change substantially over time.
Treatment
The natural course after ingestion of a foreign body is asymptomatic in 80% of cases, and the foreign body passes without problems. Endoscopic intervention is indicated in some 20% of cases. Surgery is required in less than 1% of cases (1, 2, 5, 9, 13, 15, 17, 18, 26).
Conservative treatment
Most ingested foreign bodies pass through the gastrointestinal tract without any difficulty. Consequently, conservative treatment by means of close observation is justified in most cases. This is the treatment of choice for blunt, short (<6 cm), and narrow (<2.5 cm diameter) foreign bodies, especially once they have passed the pylorus (13– 15). Spontaneous passage can mostly be expected within 4–6 days. In rare cases this may take up to 4 weeks (1, 5, 9). Until the foreign body has passed through the patient’s body safely, the patient’s stools should be continuously observed. No change in eating behavior is required during this period. If the foreign body is not passed then weekly outpatient x-ray examination is recommended in asymptomatic patients, in order to document the foreign body’s passage (1, 5, 9, 13).
Medical treatment in esophageal food bolus impaction has been described by some authors (27, 28). Because of its relaxant effect on the smooth muscles, glucagon is used to treat food bolus impaction in the esophagus (27, 28). Extending this effect of glucagon to include the treatment of swallowed foreign bodies in the upper gastrointestinal tract seems sensible, but its effectiveness has not been confirmed to date. It also remains questionable whether a similar effect can be achieved by using butylscopolamine.
Endoscopic intervention
Endoscopic intervention is necessary in 1 out of 5 cases of foreign body ingestion. A foreign body in the upper gastrointestinal tract is mostly removed by using esophagogastroduodenoscopy (1, 2, 5– 7, 9, 13– 15, 17, 18). The procedure is popular and accessible almost anywhere.
Ginsberg and Ciriza et al. recommend laryngoscopy in patients with acute dysphagia and a history indicating foreign body ingestion (5, 29). If the foreign body is detected during laryngoscopy, it can safely be removed without complications. If the foreign body is not visible but the patient has acute dysphagia, esophageal impaction has to be excluded (5). A sensation of a foreign body with dysphagia can remain for several hours after the foreign body has passed and can thus mimic foreign body impaction. Since the distinction cannot be made clinically, esophagogastroduodenoscopy is required in this emergency setting. The procedure may not only confirm the diagnosis but may as well rule out foreign body ingestion/impaction or provide definite treatment.
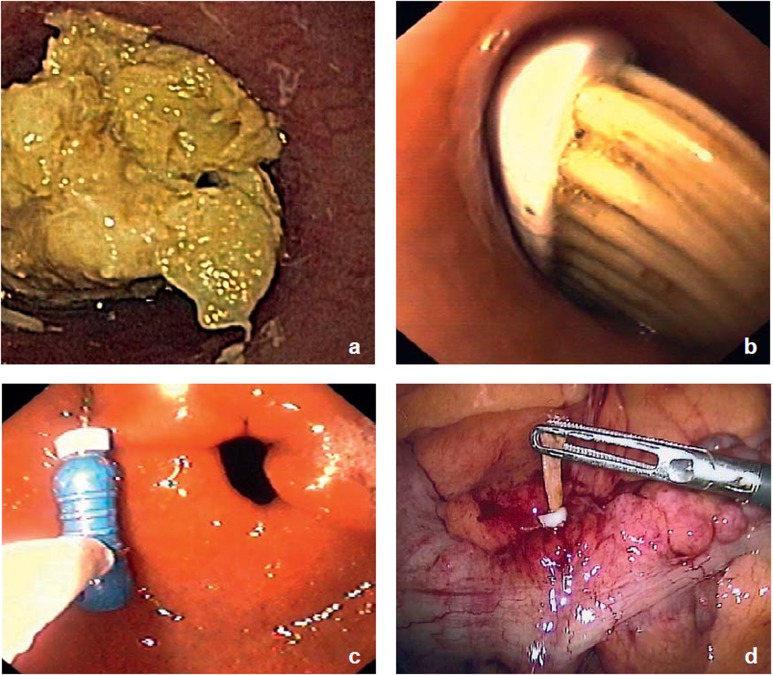
The range of indications for esophagogastroduodenoscopy is extensive (2, 3, 14, 17, 18, 26). Zhang et al. reported that all 561 patients in their study who presented after ingesting foreign bodies were referred to esophagogastroduodenoscopy (26). The urgent need for endoscopy depends on the risk of aspiration if the esophagus is completely occluded and on the risk of perforation caused by the foreign body, as well as the risk of the foreign body becoming stuck (Table). Emergency esophagogastroduodenoscopy is therefore indicated in complete occlusion of the esophagus, with salivary pooling (1, 8) (Figure 3a). This is also the case if sharp or pointed foreign bodies have been ingested, which can result in complications such as mediastinitis or peritonitis owing to perforation of the gastrointestinal tract (5, 9, 13, 17) (Figure 3b). The authors of these studies (5, 9, 13, 17) also recommend emergency esophagogastroduodenoscopy after ingestion of batteries as these contain alkaline substances and toxic metals, such as mercury. Necroses may develop subsequent to pressure on the mucosa (pressure necrosis) and/or subsequent to the release of alkaline substances (liquefactive necrosis), as may fistulas or mercury poisoning (30). Such patients should be admitted as inpatients.
Table. Indication for esophagogastroduodenoscopy and recommendations for immediate further treatment (1, 3, 5 ,9, 13, 15, 17).
| Urgent need for endoscopy | Type of foreign body (FB) | Recommended treatment |
| Emergency esophagogastroduodenoscopy | Bolus impaction with complete occlusion of the esophagus | Inpatient/outpatient |
| Sharp/pointed FB | Inpatient | |
| Batteries | Inpatient | |
| Esophagogastroduodenoscopy within 12–24 hours | Magnets | Inpatient |
| FB >6 cm in length | Outpatient/inpatient | |
| Other FB in the esophagus | Outpatient/inpatient | |
| Elective esophagogastroduodenoscopy | FB >2.5 cm diameter | Outpatient |
| Prepyloric FB | Outpatient |
Figure 3.
Endoscopic and intraoperative confirmation of the diagnosis with simultaneous initiation of treatment after ingestion of a foreign body
Complete occlusion of the esophagus by a food bolus
Toothbrush in the esophagus with early signs of mucosal ulceration
Endoscopic recovery of a dental drill in prepyloric position
-
Laparoscopic removal of a chicken bone after foreign-body related perforation of the sigmoid colon
(Figure 3d from: Ambe P, Meyer A, Köhler L: Divertikulose als Risikofaktor für eine Fremdkörperperforation des Darms [Diverticulosis as a Risk Factor for Foreign Body Associated Bowel Perforation]. Zentralbl Chir 2012; with permission from Thieme-Verlag, Stuttgart)
If removal of the foreign body is not necessary—for example, in cases of food bolus impaction in the esophagus—then it can be gently pushed into the stomach by applying mild pressure (31). If the impaction is located in the middle third of the esophagus, the risk of perforation is particularly high because the cardia is very narrow. Esophageal foreign body impaction lasting 12–24 hours should be prevented under all circumstances (9).
For the remaining esophageal ingested foreign bodies and food boluses that are not completely occluding the esophagus, urgent esophagogastroduodenoscopy is indicated. This is also the case for long (>6 cm) foreign bodies (15) (Figure 3c). If magnets have been ingested there is a high risk of intestinal obstruction, perforation and fistula formation, owing to the attraction between the individual single magnets (or between the magnet and metallic foreign bodies swallowed at the same time) (e5). Inpatient observation is recommended in this scenario.
Recovery of a foreign body by means of colonoscopy is not common practice according to the available data. After Bauhin’s valve has been passed the foreign body is usually excreted without any complications. If the passage is difficult then colonoscopic removal is recommended, as reported by Chung et al. (32).
Surgical treatment
Surgical intervention is required in less than 1% of cases. Since endoscopic techniques have progressed, surgery takes more of a background seat. The absolute indication for surgery exists only in case of perforation. Relative indications for surgery after ingestion of foreign bodies exist in the case of complications that cannot be resolved endoscopically or after unsuccessful attempts at endoscopic recovery (33). Many authors recommend a surgical consultation in patients whose ingested foreign bodies have remained in the same place in the distal duodenum for longer than a week (1, 5, 9, 13). In the era of minimally invasive surgery, laparoscopic surgery is an option (Figure 3d) (e1).
Body packing
The term body packing refers to drug smuggling in the gastrointestinal tract. Several parcels containing 5–10 g of the drug (preferably cocaine or heroin) are swallowed (34). The incidence of body packing varies depending on the geographical location. An Amsterdam working group headed by de Bakker, for example, reported 143 cases in 5 years; by contrast, 193 cases were documented in New York alone within 7 months (35, 36). More than 90% of body packers remain asymptomatic. Surgery has to be undertaken in just under 10% of cases (35).
Asymptomatic body packers are usually admitted by the police. After a history and physical examination, an x-ray overview screening of the abdomen is performed (37). Gsell et al. described how all body packers were admitted to hospital and then accommodated in special rooms (37). In some cases the diagnosis can be obtained only via CT scanning (37). Urine testing is not recommended; its sensitivity of 35% is too low (38).
Body packers should be treated conservatively. Because of the risk that the parcel may rupture, leading to subsequent intoxication, endoscopic recovery should not be attempted (1, 5, 9, 15, 34, 39). Laxatives are recommended by the Swiss working group, as they help accelerate the passage of the drug parcels through the body (within 0–9 days) (37). Since not every hospital has rooms fitted out especially to admit body packers, we recommend putting body packers into an observation room with a commode chair. This is helpful for observing the passing of the parcels and changes in people’s vital signs, as a sign of intoxication. Since the failure rate is only 2% to 5%, the conservative approach is always advisable in asymptomatic body packers (39).
Symptomatic body packers either present with signs of intoxication or bowel obstruction (34, 35, 39). If signs of intoxication are observed then a parcel rupture should be assumed. The lethal dose for cocaine has been reported to be 1 to 3 g (35). Mortality in this setting has drastically changed over the years. In the 1980s Wetli and Mittlemann reported alarming death rates of more than 50% (40), compared with 2% mortality published by de Bakker et al. in 2012 (35). This clear drop in mortality can be partly explained by improved packaging materials.
Key Messages.
Ingestion of foreign bodies is common. The clinical approach is determined by the type of foreign body (size, length, chemical composition, etc), subjective symptoms, and clinical findings.
In the overwhelming majority of patients the ingested body passes without any problems; endoscopic intervention is required in 20% of cases and surgical intervention in less than 1% of cases.
The range of indications for endoscopy should be extensive; bolus impaction with complete occlusion of the esophagus, sharp/pointed foreign bodies, and batteries constitute indications for emergency esophagogastroduodenoscopy, magnets and long (>6 cm) foreign bodies should be removed within 24 hours.
Asymptomatic “body packers” should be placed under observation, on the intensive care ward if required; endoscopic retrieval should not be attempted.
Symptomatic body packers with signs of intoxication should undergo laparotomy immediately once they have been medically stabilized, as a lethal dose must be suspected.
Acknowledgments
Translated from the original German by Dr Birte Twisselmann.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
References
- 1.Webb WA. Management of foreign bodies of the upper gastrointestinal tract: update. Gastrointest Endosc. 1995;41:39–51. doi: 10.1016/s0016-5107(95)70274-1. [DOI] [PubMed] [Google Scholar]
- 2.Cheng W, Tam PK. Foreign-body ingestion in children: experience with 1,265 cases. J Pediatr Surg. 1999;34:1472–1476. doi: 10.1016/s0022-3468(99)90106-9. [DOI] [PubMed] [Google Scholar]
- 3.Sung SH, Jeon SW, Son HS, et al. Factors predictive of risk for complications in patients with oesophageal foreign bodies. Dig Liver Dis. 2011;43:632–635. doi: 10.1016/j.dld.2011.02.018. [DOI] [PubMed] [Google Scholar]
- 4.Kerlin P, Jones D, Remedios M, Campbell C. Prevalence of eosinophilic esophagitis in adults with food bolus obstruction of the esophagus. J Clin Gastroenterol. 2007;41:356–361. doi: 10.1097/01.mcg.0000225590.08825.77. [DOI] [PubMed] [Google Scholar]
- 5.Ginsberg GG. Management of ingested foreign objects and food bolus impactions. Gastrointest Endosc. 1995;41:33–38. doi: 10.1016/s0016-5107(95)70273-3. [DOI] [PubMed] [Google Scholar]
- 6.Chiu YH, Hou SK, Chen SC, et al. Diagnosis and endoscopic management of upper gastrointestinal foreign bodies. Am J Med Sci. 2012;343:192–195. doi: 10.1097/MAJ.0b013e3182263035. [DOI] [PubMed] [Google Scholar]
- 7.Peng A, Li Y, Xiao Z, Wu W. Study of clinical treatment of esophageal foreign body-induced esophageal perforation with lethal complications. Eur Arch Otorhinolaryngol. 2012;269:2027–2036. doi: 10.1007/s00405-012-1988-5. [DOI] [PubMed] [Google Scholar]
- 8.Longstreth GF, Longstreth KJ, Yao JF. Esophageal food impaction: epidemiology and therapy. A retrospective, observational study. Gastrointest Endosc. 2001;53:193–198. doi: 10.1067/mge.2001.112709. [DOI] [PubMed] [Google Scholar]
- 9.Ikenberry SO, Jue TL, Anderson MA, et al. Management of ingested foreign bodies and food impactions. Gastrointest Endosc. 2011;73:1085–1091. doi: 10.1016/j.gie.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 10.Schwartz GF, Polsky HS. Ingested foreign bodies of the gastrointestinal tract. Am Surg. 1976;42:236–238. [PubMed] [Google Scholar]
- 11.Tiago RS, Salgado DC, Correa JP, et al. Foreign body in ear, nose and oropharynx: experience from a tertiary hospital. Braz J Otorhinolaryngol. 2006;72:177–181. doi: 10.1016/S1808-8694(15)30052-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Winkler U, Henker J, Rupprecht E. Fremdkörperingestionen im Kindesalter. Dtsch Arztebl. 2000;97(6):A316–A319. [Google Scholar]
- 13.Smith MT, Wong RK. Foreign bodies. Gastrointest Endosc Clin N Am. 2007;17:361–382. doi: 10.1016/j.giec.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 14.Palta R, Sahota A, Bemarki A, et al. Foreign-body ingestion: characteristics and outcomes in a lower socioeconomic population with predominantly intentional ingestion. Gastrointest Endosc. 2009;69:426–433. doi: 10.1016/j.gie.2008.05.072. [DOI] [PubMed] [Google Scholar]
- 15.Eisen GM, Baron TH, Dominitz JA, et al. Guideline for the management of ingested foreign bodies. Gastrointest Endosc. 2002;55:802–806. doi: 10.1016/s0016-5107(02)70407-0. [DOI] [PubMed] [Google Scholar]
- 16.Connolly AA, Birchall M, Walsh-Waring GP, Moore-Gillon V. Ingested foreign bodies: patient-guided localization is a useful clinical tool. Clin Otolaryngol Allied Sci. 1992;17:520–524. doi: 10.1111/j.1365-2273.1992.tb01710.x. [DOI] [PubMed] [Google Scholar]
- 17.Mosca S, Manes G, Martino R, et al. Endoscopic management of foreign bodies in the upper gastrointestinal tract: report on a series of 414 adult patients. Endoscopy. 2001;33:692–696. doi: 10.1055/s-2001-16212. [DOI] [PubMed] [Google Scholar]
- 18.Ngan JH, Fok PJ, Lai EC, et al. A prospective study on fish bone ingestion Experience of 358 patients. Ann Surg. 1990;211:459–462. doi: 10.1097/00000658-199004000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Watanabe K, Kikuchi T, Katori Y, et al. The usefulness of computed tomography in the diagnosis of impacted fish bones in the oesophagus. J Laryngol Otol. 1998;112:360–364. doi: 10.1017/s0022215100140460. [DOI] [PubMed] [Google Scholar]
- 20.Coulier B, Tancredi MH, Ramboux A. Spiral CT and multidetector-row CT diagnosis of perforation of the small intestine caused by ingested foreign bodies. Eur Radiol. 2004;14:1918–1925. doi: 10.1007/s00330-004-2430-1. [DOI] [PubMed] [Google Scholar]
- 21.Marco De Lucas E, Sadaba P, Lastra Garcia-Baron P, et al. Value of helical computed tomography in the management of upper esophageal foreign bodies. Acta Radiol. 2004;45:369–374. doi: 10.1080/02841850410005516. [DOI] [PubMed] [Google Scholar]
- 22.Piotto L, Gent R, Kirby CP, Morris LL. Preoperative use of ultrasonography to localize an ingested foreign body. Pediatr Radiol. 2009;39:299–301. doi: 10.1007/s00247-008-1096-2. [DOI] [PubMed] [Google Scholar]
- 23.Coulier B. [Diagnostic ultrasonography of perforating foreign bodies of the digestive tract] J Belge Radiol. 1997;80:1–5. [PubMed] [Google Scholar]
- 24.Ryan J, Perez-Avila CA, Cherukuri A, Tidey B. Using a metal detector to locate a swallowed ring pull. J Accid Emerg Med. 1995;12:64–65. doi: 10.1136/emj.12.1.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sacchetti A, Carraccio C, Lichenstein R. Hand-held metal detector identification of ingested foreign bodies. Pediatr Emerg Care. 1994;10:204–207. doi: 10.1097/00006565-199408000-00005. [DOI] [PubMed] [Google Scholar]
- 26.Zhang S, Cui Y, Gong X, et al. Endoscopic management of foreign bodies in the upper gastrointestinal tract in South China: a retrospective study of 561 cases. Dig Dis Sci. 2010;55:1305–1312. doi: 10.1007/s10620-009-0900-7. [DOI] [PubMed] [Google Scholar]
- 27.Ferrucci JT, Jr, Long JA., Jr Radiologic treatment of esophageal food impaction using intravenous glucagon. Radiology. 1977;125:25–28. doi: 10.1148/125.1.25. [DOI] [PubMed] [Google Scholar]
- 28.Trenkner SW, Maglinte DD, Lehman GA, et al. Esophageal food impaction: treatment with glucagon. Radiology. 1983;149:401–403. doi: 10.1148/radiology.149.2.6622682. [DOI] [PubMed] [Google Scholar]
- 29.Ciriza C, Garcia L, Suarez P, et al. What predictive parameters best indicate the need for emergent gastrointestinal endoscopy after foreign body ingestion? J Clin Gastroenterol. 2000;31:23–28. doi: 10.1097/00004836-200007000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Litovitz T, Schmitz BF. Ingestion of cylindrical and button batteries: an analysis of 2382 cases. Pediatrics. 1992;89:747–757. [PubMed] [Google Scholar]
- 31.Vicari JJ, Johanson JF, Frakes JT. Outcomes of acute esophageal food impaction: success of the push technique. Gastrointest Endosc. 2001;53:178–181. doi: 10.1067/mge.2001.111039. [DOI] [PubMed] [Google Scholar]
- 32.Chung YS, Chung YW, Moon SY, et al. Toothpick impaction with sigmoid colon pseudodiverticulum formation successfully treated with colonoscopy. World J Gastroenterol. 2008;14:948–950. doi: 10.3748/wjg.14.948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Siewert J, Rothmund M, Schumpelick V, editors. In: Praxis der Viszeralchirurgie. Heidelberg: Springer Medizin Verlag; 2006. Fremdkörper im Ösophagus und Magen. [Google Scholar]
- 34.Traub SJ, Hoffman RS, Nelson LS. Body packing–the internal concealment of illicit drugs. N Engl J Med. 2003;349:2519–2526. doi: 10.1056/NEJMra022719. [DOI] [PubMed] [Google Scholar]
- 35.de Bakker JK, Nanayakkara PW, Geeraedts LM, Jr, et al. Body packers: a plea for conservative treatment. Langenbecks Arch Surg. 2012;397:125–130. doi: 10.1007/s00423-011-0846-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Claffey M. Stampede of drug mules at Kennedy: after 9/11 lull, heroin & ecstasy busts soar. New York Daily News. 2002 [Google Scholar]
- 37.Gsell M, Perrig M, Eichelberger M, et al. [Body-packer & body-stuffer - a medical challenge] Praxis (Bern 1994) 2010;99:533–544. doi: 10.1024/1661-8157/a000103. [DOI] [PubMed] [Google Scholar]
- 38.Bogusz MJ, Althoff H, Erkens M, et al. Internally concealed cocaine: analytical and diagnostic aspects. J Forensic Sci. 1995;40:811–815. [PubMed] [Google Scholar]
- 39.Mandava N, Chang RS, Wang JH, et al. Establishment of a definitive protocol for the diagnosis and management of body packers (drug mules) Emerg Med J. 2011;28:98–101. doi: 10.1136/emj.2008.059717. [DOI] [PubMed] [Google Scholar]
- 40.Wetli CV, Mittlemann RE. The „body packer syndrome“-toxicity following ingestion of illicit drugs packaged for transportation. J Forensic Sci. 1981;26:492–500. [PubMed] [Google Scholar]
- e1.Ambe P, Meyer A, Kohler L. Divertikulose als Risikofaktor für eine Fremdkörperperforation des Darms. Zentralbl Chir. 2011 doi: 10.1055/s-0031-1283799. [DOI] [PubMed] [Google Scholar]
- e2.Faigel DO B. R, Stotland BR, et al. „Device choice and experience level in endoscopic foreign object retrieval: an in vivo study“. Gastrointest Endosc. 1997;45:490–492. doi: 10.1016/s0016-5107(97)70179-2. [DOI] [PubMed] [Google Scholar]
- e3.Velitchkov NG, Grigorov GI, Losanoff JE, Kjossev KT. Ingested foreign bodies of the gastrointestinal tract: retrospective analysis of 542 cases. World J Surg. 1996;20:1001–1005. doi: 10.1007/s002689900152. [DOI] [PubMed] [Google Scholar]
- e4.Lee JH, Kim HC, Yang DM, et al. What is the role of plain radiography in patients with foreign bodies in the gastrointestinal tract? Clin Imaging. 2012;36:447–454. doi: 10.1016/j.clinimag.2011.11.017. [DOI] [PubMed] [Google Scholar]
- e5.Butterworth J, Feltis B. Toy magnet ingestion in children: revising the algorithm. J Pediatr Surg. 2007;42:e3–e5. doi: 10.1016/j.jpedsurg.2007.09.001. [DOI] [PubMed] [Google Scholar]