Abstract
Objective
Using longitudinal and prospective measures of trauma during childhood, the authors assessed the risk of developing psychotic symptoms associated with maltreatment, bullying, and accidents in a nationally representative U.K. cohort of young twins.
Method
Data were from the Environmental Risk Longitudinal Twin Study, which follows 2,232 twin children and their families. Mothers were interviewed during home visits when children were ages 5, 7, 10, and 12 on whether the children had experienced maltreatment by an adult, bullying by peers, or involvement in an accident. At age 12, children were asked about bullying experiences and psychotic symptoms. Children’s reports of psychotic symptoms were verified by clinicians.
Results
Children who experienced maltreatment by an adult (relative risk=3.16, 95% CI=1.92–5.19) or bullying by peers (relative risk=2.47, 95% CI=1.74–3.52) were more likely to report psychotic symptoms at age 12 than were children who did not experience such traumatic events. The higher risk for psychotic symptoms was observed whether these events occurred early in life or later in childhood. The risk associated with childhood trauma remained significant in analyses controlling for children’s gender, socioeconomic deprivation, and IQ; for children’s early symptoms of internalizing or externalizing problems; and for children’s genetic liability to developing psychosis. In contrast, the risk associated with accidents was small (relative risk=1.47, 95% CI=1.02–2.13) and inconsistent across ages.
Conclusions
Trauma characterized by intention to harm is associated with children’s reports of psychotic symptoms. Clinicians working with children who report early symptoms of psychosis should inquire about traumatic events such as maltreatment and bullying.
Increasing evidence points toward a contribution of nongenetic factors to the etiology of psychotic disorders (1, 2), and associations between childhood trauma and psychotic illnesses have been demonstrated (3). However, given the use of retrospective reports of trauma, small samples, heterogeneous diagnostic groups, and lack of control for confounding variables (4, 5), the role of childhood trauma in the etiology of psychosis remains controversial.
In this study, we capitalized on six research strategies to further our understanding of the relationship between childhood trauma and the development of psychotic disorders. First, we examined psychotic symptoms in childhood. Early psychotic symptoms represent a developmental risk for adult schizophrenia (6) and thus provide a framework for investigating etiological factors for later psychosis. Second, we differentiated types of trauma based on the intention to harm. Different forms of trauma, such as neglect and sexual, physical, and emotional abuse, have been associated with psychosis (5, 7), yet these findings offer little insight into the mechanisms underlying this association. Disentangling whether the intention to harm is the key element involved in trauma risk may suggest causal pathways from childhood trauma to later psychosis. Third, we used prospective measures of childhood trauma reported by mothers and psychotic symptoms reported by children themselves. Reliable prospective reports of childhood trauma that are not confounded by current symptoms are essential to ascertain unbiased associations between trauma and psychosis. Fourth, we disentangled the effects of trauma in early childhood and in midchild-hood. Trauma early in childhood may be specifically associated with psychotic symptoms because young children may not yet have developed coping strategies to deal with the consequences of experiencing trauma. Fifth, we tested the risk for psychotic symptoms associated with childhood trauma over and above individuals’ genetic liability to developing psychosis. Psychotic symptoms in children who have been maltreated could be explained by genetic effects such as passive and evocative gene-environment correlations (8). Passive gene-environment correlations may come about if parents who suffer from psychotic illnesses pass on to their offspring genes involved in psychosis and also expose their children to harmful experiences. Evocative gene-environment correlations may occur if children with a genetic liability to psychotic symptoms evoke harmful experiences from their environment. Sixth, we investigated whether childhood trauma moderates the effect of children’s genetic vulnerability for developing psychotic symptoms early in life. Experiencing trauma in childhood could interact with children’s genetic susceptibility to increase their risk of developing early signs of psychosis.
Using prospective measures of trauma (maltreatment, bullying, and accidents) collected repeatedly across 7 years, we examined the risk of developing psychotic symptoms in childhood associated with early life trauma in a nationally representative U.K. cohort of twins.
Method
Participants
Participants were members of the Environmental Risk Longitudinal Twin Study (E-Risk), which tracks the development of a nationally representative birth cohort of 2,232 British children. The sample was drawn from a larger birth register of twins born in England and Wales in 1994 and 1995 (9). Briefly, the E-Risk sample was constructed in 1999 and 2000, when 1,116 families with same-sex 5-year-old twins (93% of those eligible) participated in home-visit assessments. Families were recruited to represent the U.K. population of families with newborns in the 1990s, based on residential location throughout England and Wales and mother’s age (older mothers who had twins via assisted reproduction were underselected, and teenage mothers with twins were overselected). We used this sampling to replace high-risk families who were selectively lost to the register via nonresponse and to ensure that the sample would have sufficient numbers of children growing up in high-risk environments. Follow-up home visits were conducted when the children were ages 7, 10, and 12 (participation rates were 98%, 96%, and 96%, respectively).
The sample includes 55% monozygotic twins and 45% dizygotic twins. Parents gave informed consent and children gave assent. Confidentiality was preserved, and the child’s general practitioner was notified only when a mother reported that her child was a risk to him- or herself or to others. The Joint South London and Maudsley and the Institute of Psychiatry Research Ethics Committee approved each phase of the study.
Measures
Psychotic symptoms
When the children were 12 years old, we assessed psychotic symptoms in a private individual interview conducted by mental health trainees or professionals (10). Interviewers had no prior knowledge about the child. A different staff member interviewed the child’s parents. We investigated seven psychotic symptoms related to delusions (“Have you ever believed that you were sent special messages through TV or radio?,” “Have you ever felt like you were under the control of some special power?,” “Have other people ever read your thoughts?,” “Have you ever thought you were being followed or spied on?,” “Have you ever known what another person was thinking, even though that person was not speaking, like read their mind?”) and hallucinations (“Have you heard voices that other people cannot hear?,” “Have you ever seen something or someone that other people could not see?”). Our item choice was guided by the Dunedin Study’s age-11 interview protocol (6) and an instrument prepared for the Avon Longitudinal Study of Parents and Children (11, 12). Our protocol took a conservative approach to designating a child’s report as a symptom. First, when a child endorsed any symptom, the interviewer probed using standard prompts designed to discriminate between experiences that were plausibly real (e.g., “I was followed by a man after school”) and potential symptoms (e.g., “I was followed by an angel who guards my spirit”) and wrote down the child’s narrative description of the experience. Interviewers coded each experience 0, 1, or 2, indicating, respectively, “not a symptom,” “probable symptom,” and “definite symptom.” Second, a psychiatrist expert in schizophrenia, a psychologist expert in interviewing children, and a child and adolescent psychiatrist reviewed all the written narratives to confirm the interviewers’ codes (but without consulting other data sources about the child or family). Third, because ours was a sample of twins, experiences limited to the twin relationship (e.g., “My twin and I often know what each other are thinking”) were coded as “not a symptom.”
We created a dichotomous variable representing children who reported no definite psychotic experiences (N=2,002, 94.1%) and those who reported at least one definite psychotic experience (N=125, 5.9%).
Childhood trauma
We assessed maltreatment by an adult by interviewing mothers with the standardized clinical interview protocol from the Multi-Site Child Development Project (13, 14). The protocol included standardized probe questions, such as “When [name] was a toddler, do you remember any time when [he or she] was disciplined severely enough that [he or she] may have been hurt?” and “Did you worry that you or someone else [such as a babysitter, a relative, or a neighbor] may have harmed or hurt [name] during those years?” Interviewers coded the likelihood that the child had been harmed on the basis of the mothers’ narrative. This classification showed intercoder agreement on 90% of ratings (kappa=0.56) in the Dodge et al. study (15) and in ours. On the basis of the mother’s report of the severity of discipline and the interviewer’s rating of the likelihood that the child had been physically harmed, children were coded as having not been, possibly been, or definitely been physically harmed. For this study, we examined children who experienced definite harm by an adult (coded 1) compared with others (coded 0). In our sample, 64 children (2.9%) were definitely maltreated by age 7, and 62 (2.8%) were maltreated between ages 7 and 12 but not earlier. Under the U.K. Children Act, our responsibility was to secure intervention if maltreatment was current and ongoing. Such intervention on behalf of E-Risk families was carried out with parental cooperation in all but one case.
We assessed bullying by peers during interviews with mothers. We explained to mothers that “someone is being bullied when another child (a) says mean and hurtful things, makes fun, or calls a person mean and hurtful names; (b) completely ignores or excludes someone from their group of friends or leaves them out of things on purpose; (c) hits, kicks, or shoves a person or locks them in a room; (d) tells lies or spreads rumors about them; and (e) other hurtful things like these. We call it bullying when these things happen often and it is difficult for the person being bullied to stop it happening. We do not call it bullying when it is done in a friendly or playful way.” With the aid of a Life History Calendar (16), a visual data collection tool for dating life events, mothers indicated whether either twin had been bullied by another child, responding “never,” “yes,” or “frequent.” In a sample of 30 parents who were interviewed twice, between 3 and 6 weeks apart, the test-retest reliability of reports of bullying victimization was 0.87. According to mother reports, 116 children (5.3%) were frequently bullied by age 7, and 379 (17.4%) were bullied between ages 7 and 12 only.
We also assessed bullying by peers during a private interview with children when they were age 12, using the same definition of bullying we used with mothers. Notes taken by the interviewers were later checked by an independent rater to verify that the events reported could be classified as instances of bullying by looking for evidence of (a) repeated harmful actions (b) between children (c) where there is a power difference between the bully and the victim. A total of 239 children (11.2%) reported frequently being bullied by their peers by age 12.
We assessed accidents during interviews with mothers. Using the Life History Calendar, mothers indicated whether either twin had experienced seriously harmful or frightening accidents. Examples of accidents reported by mothers included instances of children involved in a car crash or a house fire and children being bitten by a dog or otherwise injured. In our sample, 252 children (11.6%) experienced an accident by age 7 and 401 children (18.5%) did between ages 7 and 12.
Confounding Variables
An index of socioeconomic deprivation at age 5 was constructed from a standardized composite of income, parents’ education, and social class. The three socioeconomic deprivation indicators were highly correlated (r values ranged from 0.57 to 0.67, with p values <0.05) and loaded significantly onto one latent factor (factor loadings were 0.80, 0.70, and 0.83 for income, education, and social class, respectively).
Children’s IQ at age 5 was individually tested using a short form of the Wechsler Preschool and Primary Scale of Intelligence–Revised (17). Using two subtests (vocabulary and block design), children’s IQs were prorated following procedures described by Sattler (18).
Internalizing and externalizing problems at age 5 were assessed using the Child Behavior Checklist (19) for mothers and the Teacher’s Report Form (20) for teachers. The instrument was administered to mothers in a face-to-face interview; teachers responded by mail. The reporting period was the 6-month period preceding the interview. The internalizing problems scale is the sum of items in the withdrawn and anxious/depressed subscales, which include items such as “cries a lot,” “withdrawn, does not get involved with others,” and “worries.” Mothers’ scores ranged from 0 to 36 (mean=6.70, SD=5.60), and teachers’ scores ranged from 0 to 43 (mean=5.43, SD=5.39). The internal consistency reliabilities were 0.84 and 0.85, respectively. The externalizing problems scale is the sum of items from the aggressive and delinquent behavior subscales, which include items such as “argues a lot” and “is cruel or nasty to other people.” Mothers’ scores ranged from 0 to 55 (mean=12.89, SD=9.14), and teachers’ scores ranged from 0 to 59 (mean=5.41, SD=8.10). The internal consistency reliabilities were 0.89 and 0.93. We combined mother and teacher scales by summing the ratings of the two informants.
We assessed maternal history of psychosis using the Diagnostic Interview Schedule for DSM-IV (21), which inquires about characteristic symptoms of schizophrenia: hallucinations, delusions, disorganized speech, grossly disorganized or catatonic behavior, and negative symptoms (avolition, flat affect, alogia). Our interview ruled out symptoms with plausible explanations and symptoms occurring solely under the influence of alcohol or drugs. Women were classified as having a psychosis syndrome if they had hallucinations plus at least two other symptoms as well as evidence of social, occupational, or self-care dysfunction (6). Our goal was not to diagnose clinical schizophrenia but to identify women who endorsed impairing psychotic-like experiences and beliefs, given compelling evidence that psychosis syndromes in the general population are more prevalent than diagnosed cases of psychotic disorders (22).
Genetic risk was computed by selecting, in turn, one twin from each twin pair as the “target twin” and the second twin as the “co-twin” (23, 24). Each twin pair thus was represented in the data set twice, first with the elder twin as the target and the younger twin as the co-twin, and then with the younger twin as the target and the elder twin as the co-twin. A continuum of genetic risk was computed as a function of zygosity and the presence of psychotic symptoms in the co-twin. Combining information on the co-twin’s definite psychotic symptoms with information on the pair’s zygosity, the target twin’s genetic risk was coded 3 (highest risk) if the monozygotic co-twin had reported at least one definite symptom (N=62, 2.9%). The target twin’s genetic risk was coded 2 (high risk) if the dizygotic co-twin reported at least one definite symptom (N=63, 3.0%). The target twin’s genetic risk was coded 1 (low risk) if the dizygotic co-twin did not report any definite psychotic symptoms (N=910, 42.6%). Finally, the target twin’s genetic risk was coded 0 (lowest risk) if the monozygotic co-twin did not report any definite psychotic symptoms (N=1,099, 51.5%); this group constituted the comparison group.
Statistical Analysis
We tested the relationship between childhood trauma and psychotic symptoms in a series of regression models predicting children’s psychotic symptoms. The model is a bivariate model to which we subsequently added, in separate steps, gender, IQ, and socioeconomic status; internalizing and externalizing problems; and genetic vulnerabilities. Because each study family contains two children, all statistical analyses were corrected conservatively for the nonindependence of the twin observations by using tests based on the sandwich or Huber/White variance estimator (25) in Stata, version 9.0 (Stata Corp., College Station, Tex.). Application of this technique allows for the relaxation of the assumption of independence of observations by penalizing estimated standard errors and therefore accounting for the dependence in the data due to analyzing sets of twins.
Results
Of the 2,232 twins in the study, 2,143 participated in the age-12 assessment; of these, complete data were available for 2,127 twins. Table 1 presents the associations between childhood trauma across time and by presence or absence of psychotic symptoms at age 12. Three findings stand out. First, all types of trauma were associated with a higher risk for psychotic symptoms at age 12, but the effect was especially strong and consistent across time for trauma characterized by intention to harm. Second, self-reports of being bullied were more strongly associated with psychotic symptoms than were mother reports of bullying. The risk computed from self-reports of being bullied was nearly twice that computed from maternal reports. Third, the associations with psychotic symptoms were not consistent for accidents, which are characterized by unintentional harm. The associations were weaker compared with the two other types of trauma, and they were not consistent across time.
TABLE 1.
Associations Between Childhood Trauma and Psychotic Symptoms at Age 12 in a Twin Cohort (N=2,127)
| Type of Childhood Trauma | Group
|
Relative Risk | 95% CI | |||
|---|---|---|---|---|---|---|
| No Definite Psychotic Symptoms (N=2,002)
|
At Least One Definite Psychotic Symptom (N=125)
|
|||||
| N | % | N | % | |||
| Maltreatment by an adult | ||||||
| Onset before age 7 | 51 | 2.55 | 12 | 9.60 | 3.48 | 1.93–6.26 |
| Onset between ages 7 and 12 | 50 | 2.50 | 8 | 6.40 | 2.44 | 1.10–5.39 |
| Lifetime | 101 | 5.04 | 20 | 16.00 | 3.16 | 1.92–5.19 |
| Bullying by peers | ||||||
| Mothers’ reports | ||||||
| Onset before age 7 | 96 | 4.88 | 13 | 10.74 | 2.19 | 1.25–3.83 |
| Onset between ages 7 and 12 | 334 | 16.96 | 39 | 32.23 | 2.19 | 1.50–3.20 |
| Lifetime | 435 | 21.73 | 53 | 42.40 | 2.47 | 1.74–3.52 |
| Children’s self-reports | ||||||
| Lifetime | 194 | 9.70 | 44 | 35.48 | 4.36 | 3.05–6.23 |
| Accidents | ||||||
| Before age 7 | 220 | 11.20 | 18 | 14.88 | 1.36 | 0.82–2.24 |
| Between ages 7 and 12 | 366 | 18.64 | 29 | 23.97 | 1.35 | 0.87–2.08 |
| Lifetime | 598 | 29.87 | 49 | 39.20 | 1.47 | 1.02–2.13 |
Psychotic symptoms at age 12 were significantly associated with socioeconomic deprivation, lower IQ, early symptoms of psychopathology (internalizing and externalizing problems), and genetic vulnerabilities (Table 2). Childhood trauma with intentional harm was also associated with these confounding variables, whereas accidents were associated with externalizing problems only (Table 3).
TABLE 2.
Associations Between Confounding Variables and Psychotic Symptoms at Age 12 in a Twin Cohort (N=2,127)
| Confounding Variable | Group
|
Relative Risk | 95% CI | |||
|---|---|---|---|---|---|---|
| No Definite Psychotic Symptoms (N=2,002) | At Least One Definite Psychotic Symptom (N=125) | |||||
|
| ||||||
| N | % | N | % | |||
| Individual and socioeconomic factors | ||||||
| Male | 963 | 48.10 | 71 | 56.80 | 1.39 | 0.95–2.03 |
| Socioeconomic deprivationa | 658 | 32.87 | 53 | 42.40 | 2.33 | 1.38–3.91 |
|
| ||||||
| Mean | SD | Mean | SD | |||
|
| ||||||
| IQ | 100.53 | 14.89 | 93.02 | 14.60 | 0.97 | 0.96–0.98 |
| Psychopathologyb | ||||||
| Internalizing problems | 12.00 | 8.23 | 14.25 | 9.63 | 1.03 | 1.01–1.04 |
| Externalizing problems | 18.08 | 13.58 | 22.76 | 15.64 | 1.02 | 1.01–1.03 |
|
| ||||||
| N | % | N | % | |||
|
| ||||||
| Genetic vulnerabilities | ||||||
| Mothers with psychosis syndrome | 99 | 5.08 | 14 | 11.67 | 2.28 | 1.25–4.18 |
| Genetic composite riskc | ||||||
| Low | 858 | 42.86 | 49 | 39.20 | 1.35 | 0.90–2.02 |
| High | 48 | 2.40 | 14 | 11.20 | 5.62 | 2.85–11.12 |
| Highest | 44 | 2.20 | 18 | 14.40 | 7.23 | 3.66–14.31 |
Constructed from a standardized composite of income, parents’ education, and social class.
Internalizing and externalizing problems were assessed at age 5 using the Child Behavior Checklist (for mothers) and the Teacher’s Report Form (for teachers). Scores represent summed subscales from the two instruments, as described in the text.
The target twin’s genetic risk was coded as “low” when the dizygotic co-twin did not report any definite psychotic symptoms; “high” when the dizygotic co-twin reported at least one definite symptom; and “highest” when the monozygotic co-twin reported at least one definite symptom. All groups were compared with the group that had the “lowest” genetic risk, that is, when the target twin’s monozygotic co-twin did not report any psychotic symptoms.
TABLE 3.
Associations Between Confounding Variables and Childhood Trauma in a Twin Cohort (N=2,127)
| Confounding Variable | Lifetime Childhood Trauma
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Maltreatment by an Adult
|
Bullying by Peers
|
Accidents
|
||||||
| Mothers’ Reports
|
Children’s Self-Reports
|
|||||||
| Relative Risk | 95% CI | Relative Risk | 95% CI | Relative Risk | 95% CI | Relative Risk | 95% CI | |
| Individual and socioeconomic factors | ||||||||
| Male | 1.49 | 0.95–2.32 | 1.25 | 1.04–1.51 | 1.16 | 0.88–1.53 | 0.93 | 0.79–1.09 |
| Socioeconomic deprivation | 3.81 | 2.11–6.88 | 1.83 | 1.45–2.31 | 2.10 | 1.49–2.97 | 1.06 | 0.87–1.30 |
| IQ | 0.97 | 0.96–0.98 | 0.99 | 0.98–1.00 | 0.98 | 0.97–0.99 | 1.00 | 0.99–1.01 |
| Children’s psychopathology | ||||||||
| Internalizing problems | 1.04 | 1.03–1.06 | 1.02 | 1.02–1.03 | 1.02 | 1.00–1.03 | 1.01 | 0.99–1.01 |
| Externalizing problems | 1.04 | 1.03–1.05 | 1.02 | 1.02–1.03 | 1.02 | 1.01–1.02 | 1.01 | 1.00–1.01 |
| Genetic vulnerabilities | ||||||||
| Mothers with psychosis syndrome | 4.58 | 2.76–7.61 | 2.24 | 1.75–2.88 | 1.94 | 1.21–3.11 | 1.32 | 0.98–1.77 |
| Genetic composite riska | ||||||||
| Low | 1.44 | 0.90–2.31 | 1.09 | 0.90–1.33 | 1.12 | 0.83–1.50 | 1.11 | 0.94–1.30 |
| High | 2.97 | 1.34–6.57 | 1.57 | 1.07–2.29 | 2.69 | 1.63–4.44 | 1.50 | 1.07–2.09 |
| Highest | 3.77 | 1.78–8.01 | 1.67 | 1.14–2.43 | 3.59 | 2.40–5.37 | 0.96 | 0.62–1.48 |
The target twin’s genetic risk was coded as “low” when the dizygotic co-twin did not report any definite psychotic symptoms; “high” when the dizygotic co-twin reported at least one definite symptom; and “highest” when the monozygotic co-twin reported at least one definite symptom. All groups were compared with the group that had the “lowest” genetic risk, that is, when the target twin’s monozygotic co-twin did not report any psychotic symptoms.
Table 4 presents the associations between lifetime childhood trauma and psychotic symptoms at age 12, controlling for confounding variables that could account for the associations observed. Three findings stand out. First, the associations between psychotic symptoms and lifetime trauma were not accounted for by children’s gender, socioeconomic deprivation, IQ, early symptoms of psychopathology, or genetic vulnerabilities to developing psychotic symptoms. Second, the associations with accidents were weak and inconsistent across models controlling for confounders. Third, we found evidence for a dose-response relationship between a cumulative index of childhood trauma with intentional harm and children’s psychotic symptoms. A total of 589 children (28%) had been either maltreated by an adult or bullied by peers by age 12, and 70 (3%) experienced both types of trauma. Compared with children who did not experience any trauma with intentional harm by age 12, those who experienced either maltreatment or bullying were 3.27 times (95% CI=2.25–4.76) as likely to report psychotic symptoms, and those who experienced both were 5.68 times (95% CI=3.18–10.14) as likely to report psychotic symptoms (Figure 1). These elevated risks remained significant after controlling for confounding variables. Analyses further indicated that children’s genetic vulnerability for developing psychotic symptoms was not moderated by the cumulative history of childhood trauma whether genetic risk was indexed by a maternal history of psychosis (z=−1.36, p=0.174) or the co-twin’s symptoms (z=−0.55, p=0.582).
TABLE 4.
Risk for Psychotic Symptoms at Age 12 Among Children in a Twin Cohort Who Experienced Lifetime Trauma, Unadjusted and Adjusted for Confounding Variables
| Type of Childhood Trauma | Had at Least One Psychotic Symptom
|
Association Between Trauma and Children’s Psychotic Symptoms
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted
|
Adjusted for Confounding Variablesa
|
|||||||||
| Individual and Socioeconomic Factors
|
Children’s Psychopathology
|
Genetic Vulnerabilities
|
||||||||
| N | % | Relative Risk | 95% CI | Adjusted Relative Risk | 95% CI | Adjusted Relative Risk | 95% CI | Adjusted Relative Risk | 95% CI | |
| Lifetime maltreatment by an adult | 3.16 | 1.92–5.19 | 2.51 | 1.49–4.24 | 2.56 | 1.51–4.35 | 2.16 | 1.42–3.28 | ||
| No | 105 | 5.23 | ||||||||
| Yes | 20 | 16.53 | ||||||||
| Lifetime bullying by peers | ||||||||||
| Mother’s report | 2.47 | 1.74–3.52 | 2.09 | 1.44–3.03 | 2.20 | 1.52–3.17 | 2.12 | 1.49–3.02 | ||
| No | 72 | 4.39 | ||||||||
| Yes | 53 | 10.86 | ||||||||
| Children’s self-report | 4.36 | 3.05–6.23 | 3.55 | 2.47–5.12 | 4.04 | 2.82–5.79 | 3.35 | 2.28–4.91 | ||
| No | 80 | 4.24 | ||||||||
| Yes | 44 | 18.49 | ||||||||
| Lifetime accident | 1.47 | 1.02–2.13 | 1.47 | 1.02–2.13 | 1.40 | 0.96–2.02 | 1.40 | 0.99–1.97 | ||
| No | 76 | 5.14 | ||||||||
| Yes | 49 | 7.57 | ||||||||
| Cumulative childhood trauma with intentional harm | ||||||||||
| No trauma | 48 | 3.27 | ||||||||
| One type | 63 | 10.71 | 3.27 | 2.25–4.76 | 2.86 | 1.95–4.19 | 3.08 | 2.11–4.52 | 2.60 | 1.70–3.78 |
| Two types | 13 | 18.57 | 5.68 | 3.18–10.14 | 4.22 | 2.26–7.89 | 4.57 | 2.48–8.41 | 3.81 | 2.23–6.49 |
Individual and socioeconomic factors included gender, socioeconomic deprivation, and IQ; psychopathology included internalizing and externalizing problems; and genetic vulnerabilities included maternal psychosis syndrome and genetic composite risk.
FIGURE 1.
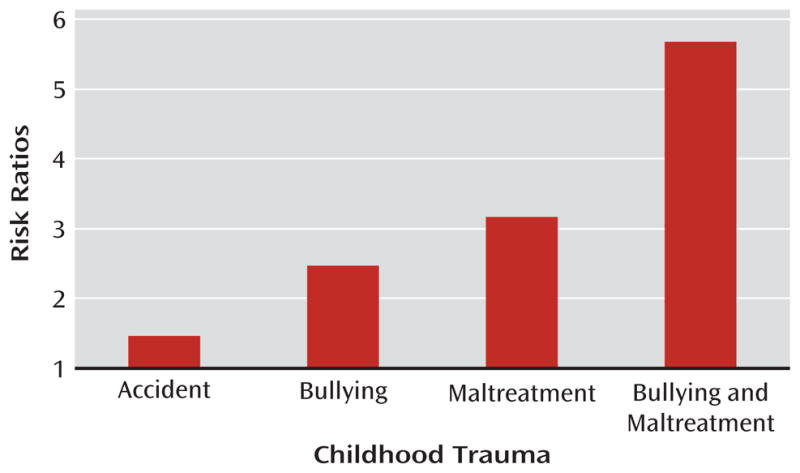
Risk of Psychotic Symptoms at Age 12 Associated With Cumulative Childhood Trauma
Discussion
Youths who report psychotic symptoms in their teens are at increased risk for developing psychotic illness later in life (6). In our sample of 12-year-olds, we found that a history of childhood trauma increased the likelihood that children would report such symptoms. Maltreatment by an adult and bullying by peers were strongly associated with children’s reports of psychotic symptoms. These findings concur with previous research but go a step further by showing that this effect is 1) consistent across early and late childhood trauma; 2) similar for maltreatment by adults and bullying by peers, which both involve intention to harm; and 3) independent of the confounding effect of socioeconomic deprivation, low IQ, early psychopathology, and genetic susceptibility to developing psychotic illnesses. Children who experience abuse early in life show adjustment problems such as posttraumatic disorders, depression, and conduct problems (26). Our study, along with other reports, indicates that psychotic symptoms can be added to this list of harmful outcomes.
Our findings show consistency across types of trauma and across timing of the events. First, children’s risks of reporting psychotic symptoms were similar across trauma characterized by intention to harm, whether these acts were perpetrated by adults or by peers. This finding suggests that an element of threat, or a perception of threat, could trigger psychotic symptoms, rather than the form the abuse may take (e.g., physical, sexual, or relational). However, our findings do not indicate that we can completely ignore the risk carried by forms of trauma that do not involve such intention. Children who experienced accidents at some point in their lives had a significantly higher risk of reporting psychotic symptoms (albeit before adjustment for confounding variables). Second, trauma was related to risk of psychotic symptoms in a dose-response fashion using a cumulative index of trauma, which is consistent with findings from another cohort of 12-year-olds (11). The cumulative effect of abuse from adults and peers, rather than its timing, appears to confer the highest risk for developing psychotic symptoms.
There is growing evidence supporting the risks associated with being bullied during childhood (27). Prospective data on trauma from population-based cohorts and samples of vulnerable youths converge in showing an elevated risk for psychosis among bullied children (11, 28, 29). Our results show a consistent pattern across informants, indicating that results did not differ depending on who reported on children’s bullying experiences, although the effects were larger for self-reports. It is conceivable that the use of self-reports of bullying and symptoms of psychosis may overestimate the risk for psychosis. First, the association may be inflated by having the same informant reporting on both bullying experiences and psychotic symptoms. Second, traumatic experiences and perception of threats may be part of the symptomatology of psychotic disorders. When children are asked about their experience of bullying, their report may be biased by their symptoms of psychosis. Alternatively, mothers and teachers may underreport instances of bullying because they are not fully aware of the children’s experiences.
Research is needed to identify mechanisms that could explain psychotic symptoms among children who have experienced trauma. Neurodevelopmental changes associated with the hypothalamic-pituitary-adrenal (HPA) axis could be one area of investigation (30). Alterations of the HPA axis are known to be associated with early experience of trauma (31, 32) as well as with psychotic illnesses (33). Childhood psychotic symptoms could be a result of neurodevelopmental changes in the HPA axis following repeated traumatic experiences. Cognitive distortion could also explain psychotic symptoms among people who experience trauma early in life (34). A childhood marked by a history of victimization could have an impact on threat perceptions and generate symptoms of psychosis—more specifically, symptoms of delusions and hallucinations.
Our study has limitations. First, we studied a cohort of twins, and our results may not be generalizable to singletons. However, previous studies have found no differences between twins and singletons in the prevalence rates of maltreatment and bullying (35, 36) or behavior problems (37–39). Second, we assessed a set of only seven psychotic symptoms. However, our questions are well established, have been validated, and have been used in other studies (6, 12, 40). Third, we remain uncertain about the timing of the psychotic symptoms, as they were not inquired about until age 12.
Early detection and targeted intervention for emerging psychotic symptoms have the potential to change the course of early psychopathology (41). Our study has implications for clinicians working with children who report symptoms of psychosis. Assessment of trauma should be part of clinical interviews to ensure that maltreatment or bullying is not ongoing. Furthermore, intervention strategies should consider the possibility that young children who show early symptoms of psychosis may be growing up in threatening environments. Further studies are needed to strengthen the hypothesis that early trauma leads to symptoms of psychopathology in childhood, and not the reverse. In addition, neurobiological research should follow the lead from epidemiological studies and investigate the pathophysiological mechanisms linking trauma to psychosis. This would help guide early prevention efforts to reduce risk for psychotic symptoms among vulnerable children by, for instance, advising about the risks of early substance use (42). Much remains to be learned about the etiology of psychosis and the development of preventive measures by broadening the scope of research to include the nonclinical phenotype (43).
Acknowledgments
The Environmental Risk Longitudinal Twin Study (E-Risk) is funded by the Medical Research Council (MRC grant G9806489). Additional support was provided by National Institute of Child Health and Human Development grant HD061298, NIMH grant MH077874, Economic and Social Research Council grant RES-177-25-0013, the Johan Jacobs Foundation, the British Academy, and the Nuffield Foundation. Dr. Arseneault is supported by a Career Scientist Award from the U.K. Department of Health. Dr. Cannon is funded by a Clinician Scientist Award from the Health Research Board, Ireland. Dr. Fisher is funded by a postdoctoral fellowship from the MRC and ESRC. Professors Moffitt and Caspi are supported by the Lady Davis Fellowship of the Hebrew University and the Caselberg Trust. Professor Caspi is a Royal Society Wolfson Research Merit Award holder.
The authors thank Michael Rutter and Robert Plomin for their contributions and Thomas Achenbach for kind permission to adapt the Child Behavior Checklist.
Footnotes
All authors report no financial relationships with commercial interests.
References
- 1.van Os J, Krabbendam L, Myin-Germeys I, Delespaul P. The schizophrenia envirome. Curr Opin Psychiatry. 2005;18:141–145. doi: 10.1097/00001504-200503000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Welham J, Isohanny M, Jones P, McGrath J. The antecedents of schizophrenia: a review of birth cohort studies. Schizophr Bull. 2009;35:603–623. doi: 10.1093/schbul/sbn084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Read J, van Os J, Morrison AP, Ross CA. Childhood trauma, psychosis, and schizophrenia: a literature review with theoretical and clinical implications. Acta Psychiatr Scand. 2005;112:330–350. doi: 10.1111/j.1600-0447.2005.00634.x. [DOI] [PubMed] [Google Scholar]
- 4.Morgan C, Fisher HL. Environmental factors in schizophrenia: childhood trauma: a critical review. Schizophr Bull. 2007;33:3–10. doi: 10.1093/schbul/sbl053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bendall S, Jackson HJ, Hulbert CA, McGorry PD. Childhood trauma and psychotic disorders: a systematic, critical review of the evidence. Schizophr Bull. 2008;34:568–579. doi: 10.1093/schbul/sbm121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Poulton R, Caspi A, Moffitt TE, Cannon M, Murray R, Harrington H. Children’s self-reported psychotic symptoms and adult schizophreniform disorder. Arch Gen Psychiatry. 2000;57:1053–1058. doi: 10.1001/archpsyc.57.11.1053. [DOI] [PubMed] [Google Scholar]
- 7.Fisher HL, Jones PB, Fearon P, Craig TK, Dazzan P, Morgan K, Hutchinson G, Doody GA, McGuffin P, Leff J, Murray RM, Morgan C. The varying impact of type, timing, and frequency of exposure to childhood adversity on its association with adult psychotic disorder. Psych Med. doi: 10.1017/S0033291710000231. (Epub ahead of print, Feb 24, 2010) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Plomin R, DeFries JC, Loehlin JC. Genotype-environment interaction and correlation in the analysis of human behavior. Psychol Bull. 1977;84:309–322. [PubMed] [Google Scholar]
- 9.Trouton A, Spinath FM, Plomin R. Twins Early Development Study (TEDS): a multivariate, longitudinal genetic investigation of language, cognition, and behaviour problems in childhood. Twin Res. 2002;38:444–448. doi: 10.1375/136905202320906255. [DOI] [PubMed] [Google Scholar]
- 10.Polanczyk G, Moffitt TE, Arseneault L, Cannon M, Ambler A, Keefe RSE, Houts R, Odgers CL, Caspi A. Childhood psychotic symptoms share etiological and clinical features with adult schizophrenia: results from a representative birth cohort. Arch Gen Psychiatry. 2010;67:328–338. doi: 10.1001/archgenpsychiatry.2010.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schreier A, Wolke D, Thomas K, Horwood J, Hollis C, Gunnell D, Lewis G, Thompson A, Zammit S, Duffy L, Salvi G, Harrison G. Prospective study of peer victimization in childhood and psychotic symptoms in a nonclinical population at age 12 years. Arch Gen Psychiatry. 2009;66:527–536. doi: 10.1001/archgenpsychiatry.2009.23. [DOI] [PubMed] [Google Scholar]
- 12.Horwood J, Salvi G, Thomas K, Duffy L, Gunnell D, Hollis C, Lewis G, Menezes P, Thompson A, Wolke D, Zammit S, Harrison G. IQ and non-clinical psychotic symptoms in 12-year-olds: results from the ALSPAC birth cohort. Br J Psychiatry. 2008;193:185–191. doi: 10.1192/bjp.bp.108.051904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dodge KA, Bates JE, Pettit GS. Mechanisms in the cycle of violence. Science. 1990;250:1678–1683. doi: 10.1126/science.2270481. [DOI] [PubMed] [Google Scholar]
- 14.Lansford JE, Dodge KA, Pettit GS, Bates JE, Crozier J, Kaplow J. Long-term effects of early child physical maltreatment on psychological, behavioral, and academic problems in adolescence: a 12-year prospective study. Arch Pediatr Adolesc Med. 2002;156:824–830. doi: 10.1001/archpedi.156.8.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dodge KA, Pettit GS, Bates JE, Valente E. Social information-processing patterns partially mediate the effect of early physical abuse on later conduct problems. J Abnorm Psychol. 1995;104:632–643. doi: 10.1037//0021-843x.104.4.632. [DOI] [PubMed] [Google Scholar]
- 16.Caspi A, Moffitt TE, Thornton A, Freedman D, Amell JW, Harrington H, Smeijers J, Silva PA. The life history calendar: a research and clinical assessment method for collecting retrospective event-history data. Int J Methods Psychiatr Res. 1996;6:101–114. [Google Scholar]
- 17.Wechsler D. Wechsler Preschool and Primary Scale of Intelligence–Revised. San Antonio, Tex: Psychological Corporation; 1991. [Google Scholar]
- 18.Sattler JM. Assessment of Children: WISC-III and WPPSI-R Supplement. San Diego: JM Sattler; 1992. [Google Scholar]
- 19.Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 Profile. Burlington: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- 20.Achenbach MT. Manual for the Teacher’s Report Form and 1991 Profile. Burlington: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- 21.Robins LN. Diagnostic Interview Schedule for DSM-IV. St Louis: Washington University School of Medicine; 1995. [Google Scholar]
- 22.Myin-Gerneys I, Krabbendam L, van Os J. Continuity of psychotic symptoms in the community. Curr Opin Psychiatry. 2003;16:443–449. [Google Scholar]
- 23.Jaffee SR, Caspi A, Moffitt TE, Taylor A. Physical maltreatment victim to antisocial child: evidence of an environmentally mediated process. J Abnorm Psychol. 2004;113:44–55. doi: 10.1037/0021-843X.113.1.44. [DOI] [PubMed] [Google Scholar]
- 24.Kendler KS, Kessler RC. Stressful life events, genetic liability, and onset of an episode of depression in women. Am J Psychiatry. 1995;152:833–842. doi: 10.1176/ajp.152.6.833. [DOI] [PubMed] [Google Scholar]
- 25.Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000;56:645–646. doi: 10.1111/j.0006-341x.2000.00645.x. [DOI] [PubMed] [Google Scholar]
- 26.Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009;373:68–81. doi: 10.1016/S0140-6736(08)61706-7. [DOI] [PubMed] [Google Scholar]
- 27.Arseneault L, Bowes L, Shakoor S. Bullying victimization in youths and mental health problems: “Much ado about nothing”? Psych Med. 2010;40:717–729. doi: 10.1017/S0033291709991383. [DOI] [PubMed] [Google Scholar]
- 28.Kelleher I, Harley M, Lynch F, Arseneault L, Fitzpatrick C, Cannon M. Associations between childhood trauma, bullying, and psychotic symptoms among a school-based adolescent sample. Br J Psychiatry. 2008;193:378–382. doi: 10.1192/bjp.bp.108.049536. [DOI] [PubMed] [Google Scholar]
- 29.Lataster T, van Os J, Drukker M, Henquet C, Feron F, Gunther N, Myin-Gerneys I. Childhood victimisation and developmental expression of non-clinical delusional ideation and hallucinatory experiences: victimisation and non-clinical psychotic experiences. Soc Psychiatry Psychiatr Epidemiol. 2006;41:423–428. doi: 10.1007/s00127-006-0060-4. [DOI] [PubMed] [Google Scholar]
- 30.Cotter D, Pariante CM. Stress and the progression of the developmental hypothesis of schizophrenia. Br J Psychiatry. 2002;181:363–365. doi: 10.1192/bjp.181.5.363. [DOI] [PubMed] [Google Scholar]
- 31.Heim C, Newport J, Heit S, Graham YP, Wilcox M, Bonsall R, Miller AH, Nemeroff CB. Long-term neuroendocrine effects of childhood maltreatment. JAMA. 2000;284:592–597. [PubMed] [Google Scholar]
- 32.Heim C, Mletzko T, Purselle D, Musselman DL, Nemeroff CB. The dexamethasone/corticotropin-releasing factor test in men with major depression: role of childhood trauma. Biol Psychiatry. 2008;63:398–405. doi: 10.1016/j.biopsych.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 33.Mondelli V, Dazzan P, Hepgul N, Di Forti M, Aas M, D’Albenzio A, Di Nicola M, Fisher HL, Handley R, Marques TR, Morgan C, Navari S, Taylor H, Papadopoulos A, Aitchison KJ, Murray RM, Pariante CM. Abnormal cortisol levels during the day and cortisol awakening response in first-episode psychoses: the role of stress and antipsychotic treatment. Schizophr Res. 2009;116:234–242. doi: 10.1016/j.schres.2009.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Freeman D, Garety PA, Kuipers E, Fowler D, Bebbington PE. A cognitive model of persecutory delusions. Br J Clin Psychiatry. 2002;41:331–347. doi: 10.1348/014466502760387461. [DOI] [PubMed] [Google Scholar]
- 35.Jaffee SR, Caspi A, Moffitt TE, Dodge KA, Rutter M, Taylor A, Tully L. Nature x nurture: genetic vulnerabilities interact with physical maltreatment to promote conduct problems. Dev Psychopathol. 2005;17:67–84. doi: 10.1017/s0954579405050042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arseneault L, Walsh E, Trzesniewski K, Newcombe R, Caspi A, Moffitt TE. Bullying victimization uniquely contributes to adjustment problems in young children: a nationally representative cohort study. Pediatrics. 2006;118:130–138. doi: 10.1542/peds.2005-2388. [DOI] [PubMed] [Google Scholar]
- 37.Gjone H, Novik TS. Parental ratings of behaviour problems: a twin and general population comparison. J Child Psychol Psychiatry. 1995;36:1213–1224. doi: 10.1111/j.1469-7610.1995.tb01366.x. [DOI] [PubMed] [Google Scholar]
- 38.van den Oord EJ, Koot HM, Boomsma DI, Verhulst FC, Orlebeke JF. A twin-singleton comparison of problem behaviour in 2–3-year-olds. J Child Psychol Psychiatry. 1995;36:449–458. doi: 10.1111/j.1469-7610.1995.tb01302.x. [DOI] [PubMed] [Google Scholar]
- 39.Johnson W, Krueger RF, Bouchard TJ, McGue M. The personalities of twins: just ordinary folks. Twin Res. 2002;5:125–131. doi: 10.1375/1369052022992. [DOI] [PubMed] [Google Scholar]
- 40.Kelleher I, Harley M, Murtagh A, Cannon M. Are screening instruments valid for psychotic-like-experiences? a validation study of screening questions for psychotic-like experiences using in-depth clinical interview. Schizophr Bull. doi: 10.1093/schbul/sbp057. (Epub ahead of print, June 19, 2009) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Compton MT, Goulding SM, Ramsay CE, Addington J, Corcoran C, Walker EF. Early detection and intervention for psychosis: perspectives from North America. Clin Neuropsychiatry. 2008;5:263–272. [PMC free article] [PubMed] [Google Scholar]
- 42.Harley M, Kelleher I, Clarke M, Lynch F, Arseneault L, Connor D, Fitzpatrick C, Cannon M. Cannabis use and childhood trauma interact additively to increase the risk of psychotic symptoms in adolescence. Psychol Med. 2010;40:1627–1634. doi: 10.1017/S0033291709991966. [DOI] [PubMed] [Google Scholar]
- 43.Kelleher I, Cannon M. Psychotic-like experiences in the general population: characterizing a high-risk group for psychosis. Psychol Med. doi: 10.1017/S0033291710001005. (Epub ahead of print, May 19, 2010) [DOI] [PubMed] [Google Scholar]


