Abstract
Smear and culture tests of corneal scrapings from a patient with a ring infiltrate confirmed significant growth of a Staphylococcus species resistant to fluoroquinolones. Because of nonresponse to medical management, the patient underwent therapeutic penetrating keratoplasty. Staphylococcal infection of the cornea may appear as a ring-like infiltrate that is recalcitrant to medical management.
CASE REPORT
A 66-year-old man presented with complaints of sudden diminution of vision in his left eye for 4 days. He had undergone left eye punctoplasty for lower lid punctal stenosis in the past and was receiving treatment for chronic meibomitis. He also had a history of recurrent uveitis and secondary glaucoma in this eye. At the time of presentation, he was using loteprednol etabonate (0.5%) and brimonidine tartrate (0.2%) eyedrops twice daily.
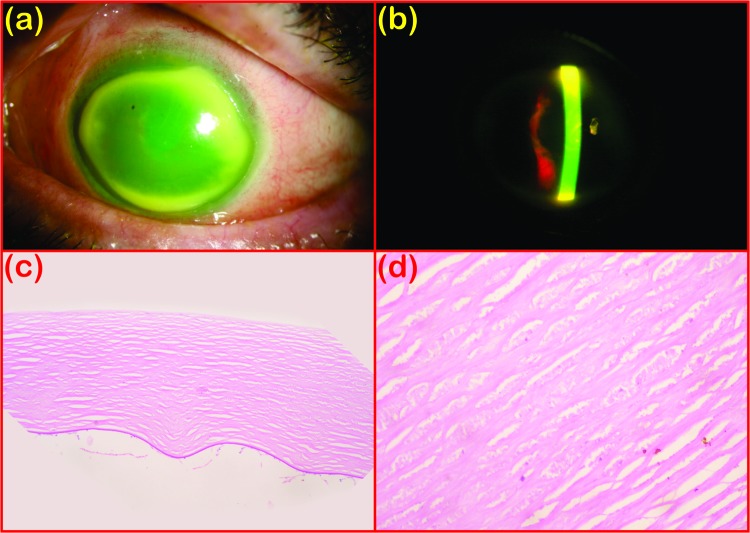
During presentation, his visual acuity was limited to hand movement close to the face. Corneal examination revealed a large epithelial defect measuring 8.0 by 7.5 mm. A stromal ring infiltrate corresponding to the dimensions of the epithelial defect was present (Fig. 1a and b). It was approximately 1.5 mm wide and away from the limbus with associated surrounding stromal edema. The anterior chamber showed a hypopyon measuring 2 mm in height. While staining with 10% potassium hydroxide with calcofluor white did not show any organism, Gram staining showed plenty of polymorphonuclear cells and Gram-positive cocci in groups.
Fig 1.
Slit lamp photograph showing a ring infiltrate in diffuse-illumination (a) and slit (b) views. (c) Corneal stroma showing diffuse loss of fibrokeratocytic nuclei with complete absence of inflammatory cells (periodic acid-Schiff staining, magnification, ×100). (d) Eosinophilic granular debris between the stromal fibers (hematoxylin-and-eosin staining; magnification, ×400).
The patient was put on fortified cefazolin (5%) and gatifloxacin (0.3%) eyedrops applied once an hour. Culture grew a Staphylococcus species (other than Staphylococcus aureus) that was significant (consistent with the direct microscopy result and confluent growth in two solid media) and sensitive to vancomycin, cefazolin, and methicillin. Hence, the application of 5% cefazolin eyedrops was continued.
On subsequent follow-up, a persistent epithelial defect with a size of >8 mm in all dimensions, a deep stromal ring infiltrate, and a hypopyon remained the same. Loteprednol etabonate eyedrops applied four times daily were added on day 5 after presentation to control the inflammatory component, along with intensive lubrication. They were tapered off over a period of 4 weeks. A repeat corneal scraping 26 days after presentation revealed no organisms in a direct smear test by Gram staining and staining with 10% potassium hydroxide plus calcofluor white or in culture. Finally, with the failure of resolution of clinical signs and symptoms, the patient was given the option of left eye therapeutic penetrating keratoplasty.
Culture of the corneal tissue for bacteria, fungi, and Acanthamoeba did not grow any organism. The histopathology evaluation of the corneal tissue showed a completely denuded epithelium with a continuous Bowman's membrane. The stroma showed diffuse loss of fibrokeratocytic nuclei (Fig. 1c and d). The peripheral stroma showed the presence of plump myofibroblastic cells. The central and paracentral corneal stroma showed patchy stromal necrosis with eosinophilic granular debris between the stromal fibers. Descemet's membrane was continuous with occasional subendothelial polymorphonuclear cells. Special stains did not show any organism.
Postoperatively, there was a large epithelial defect in the graft, which was managed with a bandage contact lens. At his last follow-up, his visual acuity was 20/125 with a clear graft.
Corneal ring infiltrates have been reported to occur in infections with a variety of organisms. These include Acanthamoeba, Gram-negative bacilli like Pseudomonas aeruginosa or Moraxella, herpes simplex virus, fungi, and varicella-zoster virus, as well as immunity-related conditions like rheumatoid arthritis (1–3). Corneal ring infiltrates are most consistently associated with Acanthamoeba keratitis. Ring infiltration has been reported after a corneal collagen cross-linking procedure with the postoperative use of a contact lens because of a polymicrobial infection caused by Streptococcus salivarius, Streptococcus oralis, and a coagulase-negative Staphylococcus sp. (4). We report an atypical case of a corneal ring infiltrate associated with Staphylococcus infection with an unusual clinical course.
Staphylococcus keratitis occurs more frequently under conditions that compromise the cornea, such as bullous keratopathy, chronic herpetic keratitis, keratoconjunctivitis sicca, etc. While S. aureus tends to produce rapidly progressive corneal infiltration and a moderate anterior chamber reaction with a hypopyon, Staphylococcus species other than S. aureus tend to progress slowly and cause superficial localized infiltration. Although Staphylococcus has been known to cause ring infiltration, it is uncommon and there are limited reports of such cases (5, 6). More interesting was the clinical course of the disease in this patient, where the persistence of the epithelial defect and infiltrate despite medical therapy presented a diagnostic and therapeutic dilemma.
Ring infiltration with Staphylococcus is thought to be immunity mediated in pathogenesis. It is a type III hypersensitivity reaction to staphylococcal antigens or toxins that results in complement activation and influx of polymorphonuclear leukocytes and mononuclear cells that form the infiltrate (7). Clinically, differentiation of an infective infiltrate from a sterile infiltrate is difficult, although the two are managed significantly differently. While infective cases would be associated with pain, suppuration, and larger epithelial defects with anterior chamber reactions, sterile infiltrates would be milder in signs and symptoms and not usually associated with epithelial defects of greater than 2 mm (8).
In our patient, the risk factor of chronic meibomitis was present, which is most commonly associated with marginal infiltration by Staphylococcus infection and perhaps a localized immunocompromised state from chronic topical steroid use. Despite in vitro susceptibility-based treatment and steroid cover for any immunological component, the patient did not respond to the treatment. Repeat microbiological evaluation and culture of the corneal tissue failed to reveal any organism, while histopathologic examination showed nonspecific stromal necrosis and the absence of any inflammatory infiltrate. This might be due to chronic steroid use causing localized immunosuppression.
The significant growth of staphylococci in culture and the nonresponse of our patient to steroid treatment have proven the absence of an immunologic component in the pathogenesis of his ring infiltrate. The multidrug resistance of the bacteria may be either associated with the ring infiltrate or just a coincidental finding.
ACKNOWLEDGMENT
No financial support for this study was received, and we have no conflict of interest.
Footnotes
Published ahead of print 24 October 2012
REFERENCES
- 1.Meyers-Elliott RH, Pettit TH, Maxwell WA. 1980. Viral antigens in the immune ring of herpes simplex stromal keratitis. Arch. Ophthalmol. 98:897–904 [DOI] [PubMed] [Google Scholar]
- 2.Khan AO, Al-Assiri A, Wagoner MD. 2008. Ring corneal infiltrate and progressive ring thinning following primary varicella infection. J. Pediatr. Ophthalmol. Strabismus 45:116–117 [DOI] [PubMed] [Google Scholar]
- 3.Illingworth CD, Cook SD. 1998. Acanthamoeba keratitis. Surv. Ophthalmol. 42:493–508 [DOI] [PubMed] [Google Scholar]
- 4.Zamora KV, Males JJ. 2009. Polymicrobial keratitis after a collagen cross-linking procedure with postoperative use of a contact lens: a case report. Cornea 28:474–476 [DOI] [PubMed] [Google Scholar]
- 5.Thygeson P. 1947. Marginal corneal infiltrates and ulcers. Trans Am. Acad. Ophthalmol. Otolaryngol. 51:198–209 [PubMed] [Google Scholar]
- 6.Hogan MJ, Diaz-Bonnet V, Okumoto M, Kimura SJ. 1962. Experimental staphylococcic keratitis. Invest. Ophthalmol. 1:267–272 [PubMed] [Google Scholar]
- 7.Chignell AH, Easty DL, Chesterton JR, Thomsitt J. 1970. Marginal ulceration of the cornea. Br. J. Ophthalmol. 54:433–440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stein RM, Clinch TE, Cohen EJ, Genvert GI, Arentsen JJ, Laibson PR. 1988. Infected vs sterile corneal infiltrates in contact lens wearers. Am. J. Ophthalmol. 105:632–636 [DOI] [PubMed] [Google Scholar]