Abstract
Background
Chronic low back pain (CLBP) and chronic neck pain (CNP) have become a serious medical and socioeconomic problem in recent decades. Patients suffering from chronic pain seem to have a higher prevalence of sleep disorders.
Purpose
To calculate the prevalence of sleep deprivation in patients with CLBP and CNP and to evaluate the factors that may contribute to sleep impairment.
Methods
This study was a retrospective evaluation of 1016 patients with CNP and CLBP who consulted an orthopedic department at a university hospital. Factors assessed were gender, age, diagnosis, grade of sleep deprivation, pain intensity, chronification grade, and migrational background. Pearson’s chi-squared test was performed to calculate the relationship between these factors and the grade of sleep deprivation. Regression analysis was performed to explore the correlation between the grade of sleep deprivation and age, pain intensity, and chronification grade.
Results
A high prevalence of sleep deprivation (42.22%) was calculated in patients with CNP and CLBP, even when analgesics had been taken. About 19.88% of the patients reported serious sleep impairments (ie, <4 hours of sleep per night). The grade of sleep deprivation did not correlate with the gender or age distribution. A significant relationship was found between the grade of sleep deprivation and pain intensity, failed back surgery syndrome, and patients with a migrational background. There was a moderate relationship with intervertebral disc disease and no relationship with spinal stenosis.
Conclusion
Sleep disturbance should be assessed when treating patients with CNP or CLBP, especially in patients with higher pain intensity, failed back surgery syndrome, and a migrational background. Further research is needed to explore the complex relationship of sleep disturbance and chronic pain.
Keywords: sleep disturbance, impairment, chronic low back pain, failed back surgery, disc disease, spinal stenosis, spondylolisthesis, migrational background, prevalence
Introduction
Chronic low back pain (CLBP) and chronic neck pain (CNP) have become a major medical and socioeconomic burden over recent decades. Despite the fact that only approximately 10%–20% of patients with low back pain develop chronic pain, these patients use more than 80% of all health care costs, presenting only low treatment success rates.1 The major problem in the treatment of CLBP and CNP is that the biopsychosocial aspects of chronic pain are in many cases not adequately taken into consideration. CLBP and CNP are not only symptoms, they are conditions that impair all aspects of a patient’s life. One of these aspects is sleep, which may become seriously disturbed in these patients.2 Patients with low back pain seem to have a high prevalence of sleep disorders and are twice as likely to be hospitalized compared with low back pain patients without sleep disorders.3–5 Sleep disturbance impairs cognitive and physical functioning as well as quality of life,6 the pain threshold,7,8 and occupational performance,9 as well as incurring higher health care usage and costs.10,11 Current research suggests that while disturbed sleep is a consequence of chronic pain, it might also contribute to disturbed pain modulation, pain perception, and hyperalgesia and may be a risk factor for the exacerbation of chronic pain.12–15 Therefore, sleep disturbance should be assessed as a clinically important symptom in CLBP and CNP and should be addressed in the pain management. The purpose of this study was to analyze the (quantitative) sleep deprivation prevalence in a large cohort of patients suffering from CLBP and CNP.
Materials and methods
Between January and April 2012, a retrospective analysis of patients with CLBP and CNP, who consulted a university hospital department of orthopedics (RKU, Ulm, Germany) from 2009–2011, was performed.
Inclusion criteria
Included in the retrospective study were patients who met the following criteria: the patient suffered from CLBP or CNP, duration of pain was >12 weeks, the patient was >18 years, no spine surgery in the year preceding the consultation, the patient filled out the section of the Oswestry Disability Questionnaire (German version) regarding sleep impairment, the patient signed informed consent about the data collection for scientific purpose, and no exclusion criteria were found in the patient’s history.16–21
Data analysis
The assessed data in the Oswestry Disability Questionnaire regarding sleep deprivation were graded into: no disturbance, no disturbance when taking analgesics, sleep < 6 hours, and severe sleep deprivation (ie, <4 hours sleep) due to pain even when taking analgesics. Further assessed parameters were: diagnosis, pain intensity on the Numerical Rating Scale (NRS), age, gender, grade of chronification according to the Mainz Pain Staging System,22,23 and migrational background (from other countries). The diagnoses were categorized according to patient’s history, radiographic-, magnetic resonance tomographic- and clinical presentation into spondylarthrosis (lumbar/cervical), intervertebral disc disease (osteochondritis, cervical, or lumbar disc herniation), spinal canal stenosis, spondylolisthesis, osteoporotic fracture (chronic), and failed back surgery syndrome.
The NRS is a well-accepted tool to access patients’ momentary back pain intensity with eleven possible grades from zero (no pain) to ten (maximal pain).18 The Oswestry Disability Index is also a well-accepted outcome measure used in the management of spinal disorders with good validity and reliability.16–19 The effect of pain on daily activities is evaluated by a ten-item questionnaire. Patients grade the impairment and pain and indicate the level of influence on their self-care, lifting, walking, sleeping, standing, sitting, travelling, social life, and sex life. Each item is scored on a six-point scale (zero to five). Sleep impairment is graded into no sleep disorder, no sleep disorder when taking analgesics, <6 hours of sleep even when taking analgesics, and <4 hours, <2 hours, or no sleep due to pain even when taking analgesics. The Oswestry Disability Questionnaire was originally described by Fairbank in 1980.20 Since then, it has undergone several modifications. The German version of the questionnaire, described by Osthus et al in 2006,21 was used in the current study. The main difference from other versions of the questionnaire is that sleep impairment is also evaluated for situations when patients are taking analgesics and it assesses the impairments during the day and at night when the questionnaire is filled out.
The Mainz Pain Staging System was first introduced by Gerbershagen in 1986 as a chronification grading system.22 It assesses four components in chronic pain: pain duration and frequency, localization of pain, analgesic medication intake, and previous treatments. Dividing patients into three grades of chronification it is a validated tool in the prediction of functional and psychical impairment, quality of life, and treatment success.23
Data collection was performed using Excel® 2010 (Microsoft Corporation, Redmond, WA) and analyzed with SPSS® version 17.0 (IBM Corporation, Chicago, IL). Pearson’s chi-squared test was performed to explore correlations between sleep deprivation and age, gender, diagnosis, pain intensity, and migrational background (significance level: P = 0.005). Regression analysis was performed to explore the correlation between sleep deprivation and age, pain intensity, and chronification grade. To avoid bias due to comorbidities or medications, which may contribute to sleep disorders, exclusion criteria were defined.
Exclusion criteria
Patients who met one or more of the following criteria were excluded from the evaluation: acute low back or neck pain, aged < 18 years, migraine, psychiatric disorders, substance abuse, rheumatic diseases (eg, fibromyalgia, rheumatoid arthritis), inflammatory disease of the spine (eg, discitis), arrhythmias, pacemaker, heart failure, restless legs syndrome, polyneuropathy, spinal cord injury, traumatic fractures of the spine, neurofibromatosis, malignancy, metastatic disease, thyroid disease, spinal surgery < 1 year before consultation, severe spinal deformities (eg, scoliosis), sleep apnea, or refusal to do the questionnaire.
Results
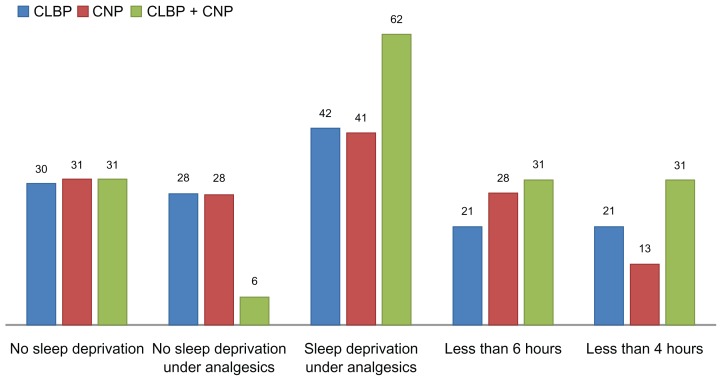
Between 2009 and 2011, a total of 1016 patients who consulted the department of orthopedic surgery at a university hospital because of CNP or CLBP fulfilled the criteria mentioned above (572 females and 444 males). The average age of the cohort was 57.07 years; average pain intensity was 6.09. The prevalence of sleep deprivation was 42.22% (n = 434). Of the 882 patients suffering from CLBP, 42% (n = 371) experienced sleep deprivation even when taking analgesics and 21% (n = 182) experienced severe sleep deprivation (<4 hours of sleep). Of the 118 patients suffering from CNP, 41% (n = 48) experienced sleep deprivation even when taking analgesics and 13% (n = 15) experienced severe deprivation. A small cohort of patients (n = 16) presented symptoms of both CLBP and CNP. For this group, the prevalence of sleep deprivation even when taking analgesics was 62% (n = 10) and the prevalence of severe sleep deprivation was 31% (n = 5). The characteristics of the analyzed cohort are described below (Tables 1 and 2; Figure 1).
Table 1.
Characteristics of the analyzed cohort (n = 1016)
| Gender | |
| Females | 572 |
| Males | 444 |
| Age | |
| Mean (years) | 57.07 |
| 95% confidence interval | 56.19–57.95 |
| Standard deviation | 14.28 |
| Pain intensity | |
| Mean (Numerical Rating Scale) | 6.09 |
| 95% confidence interval | 5.93–6.25 |
| Standard deviation | 1.91 |
| Sleep deprivation | |
| No deprivation (n/%) | 309/30.41% |
| No deprivation under analgesics | 278/27.36% |
| Deprivation even under analgesics | 434/42.22% |
| Severe deprivation (<4 hours of sleep) | 202/19.88% |
Table 2.
Prevalence of sleep deprivation according to the location of chronic pain
| Pain location | Chronic back pain | Chronic neck pain | Both |
|---|---|---|---|
| Total (n) | 882 | 118 | 16 |
| No sleep deprivation | 268 (30%) | 36 (31%) | 5 (31%) |
| No sleep deprivation when using analgesics | 243 (28%) | 34 (28%) | 1 (6%) |
| Sleep deprivation < 6 hours (even when using analgesics) | 189 (21%) | 33 (28%) | 5 (31%) |
| Sleep deprivation < 4 hours (even when using analgesics) | 182 (21%) | 15 (13%) | 5 (31%) |
Figure 1.
Prevalence (%) of sleep deprivation in patients suffering from chronic neck pain, back pain, or both.
Abbreviations: CLBP, chronic low back pain; CNP, chronic neck pain.
Pearson’s chi-squared test was performed to analyze the relationship of age, gender, diagnosis, pain intensity, and migrational background to the intensity of sleep deprivation. No significant difference in the intensity of sleep deprivation was found between males and females (chi-square = 2.609, correlation = 0.051, P = 0.456). There was also no significant difference for patients aged < 50 years and >50 years (chi-square = 5.349, correlation = 0.072, P = 0.148) and patients aged < 60 years and >60 years (chi-square = 5.349, correlation = 0.0723, P = 0.148). No correlation was explored between the grade of sleep deprivation and age using the regression analysis (P = 0.5071). Strong evidence was found for a difference between pain intensity subgroups with NRS scores less than five and at least five (chi-square = 54.716, correlation = 0.303, P < 0.001). Very strong evidence was found for a difference between pain intensity subgroups with NRS scores less than five and more than seven (chi-square = 65.664, correlation = 0.474, P < 0.001). There was a significant positive correlation between the grade of sleep deprivation and pain intensity on the NRS (P < 0.00001, β = 0.23637) as well as for chronification grade (P < 0.00001, β = 0.59057) using the regression analysis. Very strong evidence was also found for a diagnosis-related relationship with the intensity of sleep deprivation. For the subgroups of patients with chronic osteoporotic vertebral fracture, intervertebral disc disease, spondylarthritis, spondylolisthesis, spinal stenosis, and failed back surgery syndrome, a chi-square of 32.867, a correlation of 0.164, and a P-value of 0.005 was calculated. Thus, patients with disc disease and failed back surgery syndrome presented a higher prevalence and degree of sleep deprivation. These groups were also tested separately against the collective without these diagnoses. Comparing patients with intervertebral disc disease to patients with other diagnoses, there was only moderate evidence for a relationship to sleep deprivation (chi-square = 9.308, correlation = 0.094, P = 0.024). There was no significant difference between the group of cervical and lumbar disc disease (chi-square = 1.424, correlation = 0.056, P = 0.7), nor was there a significant difference comparing these against the other diagnoses (cervical versus other: chi-square = 1.521, correlation = 0.039, P = 0.677; lumbar versus other: chi-square = 0.753, correlation = 0.027, P = 0.861). Comparing patients with failed back surgery syndrome to patients with other diagnoses, very strong evidence for a relationship was calculated (chi-square = 24.386, correlation = 0.156, P < 0.001). A separate comparison of patients with spinal stenosis to patients with other diagnoses could not reveal a significant relationship to sleep deprivation (chi-square = 4.442, correlation = 0.066, P = 0.217). Comparing the subgroup of patients with a migrational background (n = 129) to the native group (n = 887), very strong evidence for a relationship with the intensity of sleep deprivation was calculated (chi-square = 20.891, correlation = 0.142, P < 0.001).
Discussion
Sleep impairment is strongly associated with chronic pain. Alsaadi et al provided a meta-analysis of 13 studies, which included nonspecific low back pain patients and described an estimated sleep disorder prevalence of of 58.7% (95% confidence interval 56.4%–60.7%).4 Marty et al assessed the sleep quality in CLBP and a control population, and demonstrated that 49.5% of patients with CLBP considered their sleep quality as poor or very poor.24 Tang et al reported that over half of the patients with CLBP suffered from moderate or severe comorbid insomnia,3 similar to Atkinson at al.25 The aim of the current study was to evaluate the quantitative aspect of sleep deprivation in patients suffering from CLBP and CNP. The results demonstrate a point prevalence of sleep deprivation in 42.22% of these patients.
No significant difference was found between sleep deprivation in patients with CNP or CLBP and gender, nor was there a relationship between sleep deprivation and age. Higher prevalence was found in a small subgroup of patients that presented symptoms of both CNP and CLBP. This subgroup has not been mentioned in the literature previously.
Significant differences were calculated by dividing the cohort into diagnosis-related subgroups, pain intensity subgroups, and patients with migrational background versus natives. A significant high prevalence of sleep deprivation was found in patients with failed back surgery syndrome, and patients with migrational background, while only low significance was calculated for patients with intervertebral disc disease. Patients with failed back surgery syndrome usually have a long patient career of chronification. This, as well as psychological factors could trigger the sleep deprivation. A migrational background may also be associated with higher social and psychological distress (social isolation, lower income, language, or adaptation problems), resulting in a higher prevalence of sleep deprivation. Among the group of intervertebral disc disease, there was no significant difference between the cervical and lumbar disc disease subgroup. No significant relationship to sleep deprivation was found for patients with spinal stenosis.
Pain intensity and chronification grade presented a positive correlation with the grade of sleep deprivation in the current study. In a follow-up study on workers in Norway, Eriksen et al concluded that sleep problems at baseline were predictive of long-term work disability.26 According to Miranda et al, a sleep disorder might also be a predictor for the future development of low back pain.27 Auvinen et al concluded that chronic and acute patients with low back pain present equal prevalence of sleep disturbance.28 Further research is needed to explore if sleep deprivation is a possible predictive factor of development and chronification of CNP and CLBP.
Two interesting observations from the current data analysis should be mentioned: elderly patients (70–85 years) and nonnative German speaking patients had problems filling out the questionnaires completely, which may bias questionnaire-based studies. Such questionnaires are usually filled out while patients wait for a consultation. These findings implicate the need to ask patients directly about sleep disturbance and the advisability of using translated questionnaires for patients with a migrational background. Some authors also propose educating patients and explaining the questions in the questionnaires.29
Sleep disturbance can be a sign of severe pain intensity and long-lasting intensive neck or low back pain should always indicate further diagnosis to exclude fracture, infection, or malignancy, but disturbed sleep can also point at emotional distress in a patient’s life (fear, anger, impairments in social life) or even a psychological comorbidity such as depression.30 Approximately 40% of adults with insomnia also have a diagnosable psychiatric disorder, in most cases depression or anxiety disorders, which may be a consequence of the sleep deprivation as well as a risk factor for its development.31,32 They can trigger the process of chronification in neck and low back pain or occur during the disease. In a recent study, Artner et al calculated a 54% prevalence of psychological disorders in CLBP patients in multimodal pain management.33
The aim of the study – to calculate a point prevalence of sleep deprivation in patients with CNP and CLBP, as well as analyzing factors like gender, age, diagnosis, pain intensity, chronification, and migrational background – was fulfilled. Further research is needed to explore the complex relationship of sleep disturbance and chronic pain. Sleep disturbance should be assessed when treating patients with CNP or CLBP, and be addressed in the treatment regimen for these patients. Possible treatment options include relaxation therapy (eg, meditation or progressive muscle relaxation), cognitive behavioral therapy, psychodynamic therapy, or combinations of these, which seem to maintain a long-term benefit and are as effective as pharmacologic treatments (eg, low-dose antidepressants).34–36 Multimodal pain therapy could be a promising option because of the intense and interdisciplinary approach to the patient, combining pain management, management of sleep, relaxation, cognitive behavioral treatment, and physical exercise.
Conclusion
The data demonstrate the need for further research on the coincidence of sleep deprivation in patients suffering from chronic pain syndromes, particularly CNP and CLBP. More attention should be paid to their treatment, especially in patients with higher pain intensity, failed back surgery syndrome, and migrational background.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Waddell G. The clinical course of low back pain. In: Waddell G, editor. The Back Pain Revolution. 1st ed. Edinburgh: Churchill Livingstone; 1998. pp. 103–117. [Google Scholar]
- 2.Hagen EM, Svensen E, Eriksen HR, Ihlebaek CM, Ursin H. Comorbid participative health complaints in low back pain. Spine (Phila Pa 1976) 2006;31(13):1491–1495. doi: 10.1097/01.brs.0000219947.71168.08. [DOI] [PubMed] [Google Scholar]
- 3.Tang NK, Wright KJ, Salkovskis PM. Prevalence and correlates of clinical insomnia co-occuring with chronic back pain. J Sleep Res. 2007;16(1):85–95. doi: 10.1111/j.1365-2869.2007.00571.x. [DOI] [PubMed] [Google Scholar]
- 4.Alsaadi SM, McAuley JH, Hush JM, Maher CG. Prevalence of sleep disturbance in patients with low back pain. Eur Spine J. 2011;20(5):737–743. doi: 10.1007/s00586-010-1661-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kaila-Kangas L, Kivimaki M, Harma M, et al. Sleep disturbances as predictors of hospitalization for back disorders: a 28-year follow-up of industrial employees. Spine (Phila Pa 1976) 2006;31(1):51–56. doi: 10.1097/01.brs.0000193902.45315.e5. [DOI] [PubMed] [Google Scholar]
- 6.Simon GE, Von Korff M. Prevalence, burden, and treatment of insomnia in primary care. Am J Psychiatry. 1997;154(10):1417–1423. doi: 10.1176/ajp.154.10.1417. [DOI] [PubMed] [Google Scholar]
- 7.O’Donoghue GM, Fox N, Heneghan C, Hurley DA. Objective and subjective assessment of sleep in chronic low back pain patients compared with healthy age and gender matched controls: a pilot study. BMC Musculoskelet Disord. 2009;10:122–130. doi: 10.1186/1471-2474-10-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith MT, Perlis ML, Carmody TP, Smith MS, Giles DE. Presleep cognitions in patients with insomnia secondary to chronic pain. J Behav Med. 2001;24(1):93–114. doi: 10.1023/a:1005690505632. [DOI] [PubMed] [Google Scholar]
- 9.Salo P, Oksanen T, Sivertsen B, et al. Sleep disorder as a predictor of cause-specific work disability and delayed return to work. Sleep. 2010;33(10):1323–1331. doi: 10.1093/sleep/33.10.1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Novak M, Mucsi I, Shapiro CM, Rethelyi J, Kopp MS. Increased utilization of health services by insomniacs – an epidemiological perspective. J Psychosom Res. 2004;56(5):527–536. doi: 10.1016/j.jpsychores.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 11.Leger D, Guilleminault C, Bader G, Levy E, Paillard M. Medical and socio-professional impact of insomnia. Sleep. 2002;25(6):625–629. [PubMed] [Google Scholar]
- 12.Smith MT, Haythornthwaite JA. How do sleep disorder and chronic pain inter-relate? Insights from the longitudinal and cognitive-behavioral clinical trials literature. Sleep Med Rev. 2004;8(2):119–132. doi: 10.1016/S1087-0792(03)00044-3. [DOI] [PubMed] [Google Scholar]
- 13.Smith MT, Edwards RR, McCann UD, Haythornwaite JA. The effect of sleep deprivation on pain inhibition and spontaneous pain in women. Sleep. 2007;30(4):494–505. doi: 10.1093/sleep/30.4.494. [DOI] [PubMed] [Google Scholar]
- 14.Roehrs T, Hyde M, Blaisdell B, Greenwald M, Roth T. Sleep loss and REM sleep loss are hyperalgesic. Sleep. 2006;29(2):145–151. doi: 10.1093/sleep/29.2.145. [DOI] [PubMed] [Google Scholar]
- 15.Haack M, Sanchez E, Mullington JM. Elevated inflammatory markers in response to prolonged sleep restriction are associated with increased pain experience in healthy volunteers. Sleep. 2007;30(9):1145–1152. doi: 10.1093/sleep/30.9.1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976) 2000;25(22):2940–2952. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 17.Bombardier C. Outcome assessments in the evaluation of treatment of spinal disorders: summary and general recommendations. Spine (Phila Pa 1976) 2000;25(24):3100–3103. doi: 10.1097/00007632-200012150-00003. [DOI] [PubMed] [Google Scholar]
- 18.Maughan EF, Lewis JS. Outcome measures in chronic low back pain. Eur Spine J. 2010;19(9):1484–1494. doi: 10.1007/s00586-010-1353-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Junge A, Mannion AF. Questionnaire for patients with back pain. Diagnosis and treatment outcome. Orthopade. 2004;33(5):545–552. doi: 10.1007/s00132-003-0613-0. German. [DOI] [PubMed] [Google Scholar]
- 20.Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66(8):271–273. [PubMed] [Google Scholar]
- 21.Osthus H, Cziske R, Jacobi E. Cross-cultural adaptation of a German version of the Oswestry Disability Index and evaluation of its measurement properties. Spine (Phila Pa 1976) 2006;31(14):E448–E453. doi: 10.1097/01.brs.0000222054.89431.42. [DOI] [PubMed] [Google Scholar]
- 22.Gerbershagen U. Organized treatment of pain. Determination of status. Internist (Berl) 1986;27(7):459–469. German. [PubMed] [Google Scholar]
- 23.Frettloh J, Maier C, Gockel H, Huppe M. Validation of the German Mainz Pain Staging System in different pain syndromes. Schmerz. 2003;17(4):240–251. doi: 10.1007/s00482-003-0227-9. German. [DOI] [PubMed] [Google Scholar]
- 24.Marty M, Rozenberg S, Duplan B, Thomas P, Duquesnoy B, Allaert F. Quality of sleep in patients with chronic low back pain: a case-control study. Eur Spine J. 2008;17(6):839–844. doi: 10.1007/s00586-008-0660-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Atkinson JH, Ancoli-Israel S, Slater MA, Garfin SR, Gillin JC. Subjective sleep disturbance in chronic back pain. Clin J Pain. 1998;4(4):225–232. [Google Scholar]
- 26.Eriksen W, Natvig B, Bruusgaard D. Sleep problems: a predictor of long-term work disability? A four-year prospective study. Scand J Public Health. 2001;29(1):23–31. [PubMed] [Google Scholar]
- 27.Miranda H, Viikari-Juntura E, Punnett L, Riihimaki H. Occupational loading, health behavior and sleep disturbance as predictors of low-back pain. Scand J Work Environ Health. 2008;34(6):411–419. doi: 10.5271/sjweh.1290. [DOI] [PubMed] [Google Scholar]
- 28.Auvinen JP, Tammelin TH, Taimela SP, et al. Is insufficient quantity and quality of sleep a risk factor for neck, shoulder and low back pain? A longitudinal study among adolescents. Eur Spine J. 2010;19(4):641–649. doi: 10.1007/s00586-009-1215-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mehra A, Baker D, Disney S, Pynsent PB. Oswestry Disability Index scoring made easy. Ann R Coll Surg Engl. 2008;90(6):497–499. doi: 10.1308/003588408X300984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Opavsky J. Odber anamnezy a hodnoceni bolesti v bezne ambulantni praxi. In: Opavsky J, editor. Bolest v Ambulantni Praxi. [Pain in the Outpatient Setting]. Praha: Maxdorf Jessenius; 2011. pp. 44–76. Czech. [Google Scholar]
- 31.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262(11):1479–1484. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 32.McCall WV. A psychiatric perspective on insomnia. J Clin Psychiatry. 2001;62(Suppl 10):27–32. [PubMed] [Google Scholar]
- 33.Artner J, Lattig F, Cakir B, Gundel H, Reichel H, Spiekermann JA. Prevalence of psychological disorders in the multimodal therapy of chronificated back pain. Orthopade. 2012 doi: 10.1007/s00132-012-1980-1. Forthcoming. German. [DOI] [PubMed] [Google Scholar]
- 34.Morin CM, Culbert JP, Schwartz SM. Nonpharmacological interventions for insomnia: a meta-analysis of treatment efficacy. Am J Psychiatry. 1994;151(8):1172–1180. doi: 10.1176/ajp.151.8.1172. [DOI] [PubMed] [Google Scholar]
- 35.Murtagh DR, Greenwood KM. Identifying effective psychological treatments for insomnia: a meta-analysis. J Consult Clin Psychol. 1995;63(1):79–89. doi: 10.1037//0022-006x.63.1.79. [DOI] [PubMed] [Google Scholar]
- 36.Jungquist CR, O’Brien C, Matteson-Rusby S, et al. The efficacy of cognitive-behavioral therapy for insomnia in patients with chronic pain. Sleep Med. 2010;11(3):302–309. doi: 10.1016/j.sleep.2009.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]