Abstract
Background and methods
Fractures in elderly populations result from the combination of falls and osteoporosis. We report a systematic review of studies indexed in PubMed reporting annual rates of low-trauma falls and associated osteoporotic fractures among older community-dwelling people (age ≥ 50 years). An osteoporotic fracture was defined as either a fracture resulting from a low-impact fall in subjects with clinical osteoporosis, a fall resulting in an investigator-defined osteoporotic fracture, or a fall resulting in a low-trauma fracture. Rates are presented using descriptive statistics. Meta-analysis was conducted for statistically homogeneous data sets.
Results
The median (range) annual fall prevalence rates (median proportion of people who experienced one or more falls during the past year) for cohorts of women and men (10 determinations), women alone (seven determinations), and men alone (four determinations) were, respectively, 0.334 (0.217–0.625), 0.460 (0.372–0.517), and 0.349 (0.284–0.526). In studies that reported fall prevalence rates for Western men and women separately (four determinations), the pooled risk ratio (95% confidence interval [CI]) for men versus women was 0.805 (95% CI 0.721–0.900). The ranges of fall prevalence rates in East Asian women (two studies) and East Asian men (two studies) were, respectively, 0.163–0.258 and 0.087–0.184. The risk ratio (95% CI) for fall prevalence in East Asian men versus women was 0.634 (0.479–0.838) in studies (two determinations) reporting results for East Asian men and women separately. In cohorts of Western women and men (five determinations), the pooled rate (95% CI) of low-impact falls resulting in fractures was 0.041 (0.031–0.054). The proportion of low-trauma fractures attributable to falls among the Western community-dwelling elderly was within the range of 0.860–0.950 for fractures at all sites or the hip (five determinations). A range of 0.716–0.924 of all fractures were osteoporotic (eight determinations).
Conclusion
Fall rates are higher in women than in men in Western community-dwelling populations and lower in East Asian populations. Extrapolated to the US population, the statistics imply that low-impact falls cause approximately 0.53 million osteoporotic fractures annually among the US community-dwelling elderly.
Keywords: accidental falls, aged, bone density, fractures, osteoporosis
Introduction
Fractures in elderly populations arise predominantly from the combination of falls and low bone density. The odds of a fracture are 7–9 times higher among community-dwelling postmenopausal women with both a fall and osteoporosis or osteopenia, compared with women having a fall or osteoporosis/osteopenia only.1 Estimates of rates of falls and resulting osteoporotic fractures are needed to guide health care policy, but there is no recent overview of studies reporting these statistics. The objective of this report is to review evidence of the epidemiology of low-impact falls and resulting osteoporotic fractures among older community-dwelling adults.
Materials and methods
Literature search
Searches of PubMed were conducted in March 2012 for primary studies of falls among older community-dwelling populations. The last PubMed search was completed on March 16, 2012. Two search algorithms were run. First, “accidental falls”[MeSH Terms] AND “aged”[MeSH Terms] AND “fall*”[Title word] AND (“community*”[All Fields] OR “home*”[All fields] OR “population surveillance”[MeSH terms]). Second, “aged”[MeSH Terms] AND “fall*”[All fields] AND ((falls[Title word] AND fractures[Title word]) OR (“osteoporosis*”[MeSH terms] AND “fractures, bone”[MeSH terms])). These searches included the following conditional terms: AND (“humans”[MeSH Terms] AND English[lang]) NOT letter[publication type] NOT editorial[publication type] NOT review[publication type] NOT “clinical trial”[publication type] NOT “case reports”[publication type] NOT comment[publication type] AND hasabstract[text]. These searches identified 459 unique articles. In addition, primary studies were identified from review articles.2,3 Articles were screened and included if they were studies of older community-dwelling populations (age ≥ 50 years) and reported statistics on rates of falls and osteoporotic fractures (see below). A total of 34 articles reporting one or more of the relevant statistics were identified.1,4–36 In addition, studies of the costs of falls were searched for with the algorithm: fall*[title word] AND cost[title word], and articles reporting national costs identified.37–41
Definitions
The formal definition of a fall is “a sudden, unintentional change in position causing an individual to land at a lower level, on an object, the floor, or the ground, other than as a consequence of sudden onset of paralysis, epileptic seizure, or overwhelming external force”.42 In this review, a fall was any type of fall, whether from a height, down a gradient, or from standing height, and whether or not an injury resulted. A low-impact or low-trauma fall was a fall from standing height, such as from slipping, tripping, or stumbling on the same level or on stairs, and not from a height, such as from a ladder or scaffolding (specific definitions used in the articles reviewed are presented in the Results section). An osteoporotic fracture was: a low-trauma fracture occurring in a person with osteoporosis, where osteoporosis was defined by a T score ≤ −2.5;43 a fracture due to a low-impact fall, excluding falls with traumatic impact that would result in a fracture in a young, healthy person; a fracture defined by the investigators as an osteoporotic fracture; or a fracture defined by the investigators as a fragility fracture or, synonymously, a low-trauma or low-energy fracture.44,45
Data analysis
The following statistics were extracted from prospective cohort studies: annual prevalence of low-impact falls, annual incidence of low-impact falls, and the proportion of low-impact falls resulting in osteoporotic fracture (statistics were extracted independently by AM and LW). Data were analyzed for populations of women and men combined (“women/men”), women alone, and men alone, and for general Western populations and East Asian populations. A descriptive analysis was conducted, and the results presented as a median and/or range of values from individual studies, stratified by gender and race. Fall incidence rates were calculated from the number of falls and number of person-years. A meta-analysis was conducted for fall prevalence and incidence rates and for the proportion of low-trauma falls with fracture in prospective cohort studies using fixed-effects and random-effects models, and the results presented in forest plots. Ratios of fall prevalence and incidence rates in men versus women were calculated from cohort studies reporting results for both men and women, thereby controlling for variability between studies. Pooled risk or rate ratios were computed and stratified by race, using random-effects models. Heterogeneity across studies was examined using the P value of the Q statistic and I2 values (for Q, a P value < 0.10 was the threshold for statistical heterogeneity between studies; an I2 value of 0.0 indicates the absence of heterogeneity). Pooled statistics are reported within the text only for statistically homogeneous data sets. Meta-analytic calculations were conducted using Comprehensive Meta-Analysis, version 2.
The proportion of low-trauma fractures attributable to low-impact falls and the proportion of fractures that were osteoporotic were extracted from cohort or cross-sectional studies. The proportion of all fractures that are osteoporotic was determined from studies in which investigators directly reported this statistic, measured either by bone mineral density measurement in subjects with a fracture, or by degree of trauma associated with the fracture event. A descriptive analysis was conducted. Results were presented as ranges of values from individual studies. Statistical outliers were identified by applying Dixon’s test at an alpha value of 0.10.46
Results
Low-impact falls in prospective cohorts of older community-dwellers
A total of 16 articles reported the prevalence and/or incidence of low-impact falls in Western populations of older women/men,4–8,10,12,14,15,17,20,21,24,30,36 women alone,11,19,25,29,35 and men alone,13 and three articles reported these statistics for East Asian populations18,27,28 (Supplementary Table A).
Definition of a low-impact fall
Most of the studies applied a standard definition of a fall that excluded falls from a height, so that the fall was in effect low-impact or low-trauma. Nevitt et al specified falling to the floor or falling and hitting an object such as a chair or steps, and excluded major impact.6 Other definitions were: landing on the floor or other lower level, including stairs, by accident,18 “an unintentional change in position resulting in coming to rest on the ground or another lower level, and not as a result of a major intrinsic event (eg, stroke, syncope) or overwhelming hazard (eg, car accident)”,4,30 “unintentionally coming down on the floor or to a lower level”,10,24,36 “an unintentional change in position to the floor or ground”,15 “losing your balance such that your hands, arms, knees, buttocks or body touch or hit the ground or floor”,17 “an unexpected event when the person fell to the ground on the same or from an upper level, taking the falls on stairs and those onto a piece of furniture into account”,14 “an event in which the participant unintentionally comes to rest on the ground or at a lower level”,29 “unintentionally coming to rest on the ground, floor, or other lower level for reasons other than sudden onset of acute illness or overwhelming external force”,35 or “an event which results in a person coming to rest unintentionally on the ground or other lower level, not due to any intentional movement, a major intrinsic event (eg, stroke) or extrinsic force (eg, forcefully pushed down, knocked down by a car)”.28
Prevalence and incidence of low-impact falls in Western populations
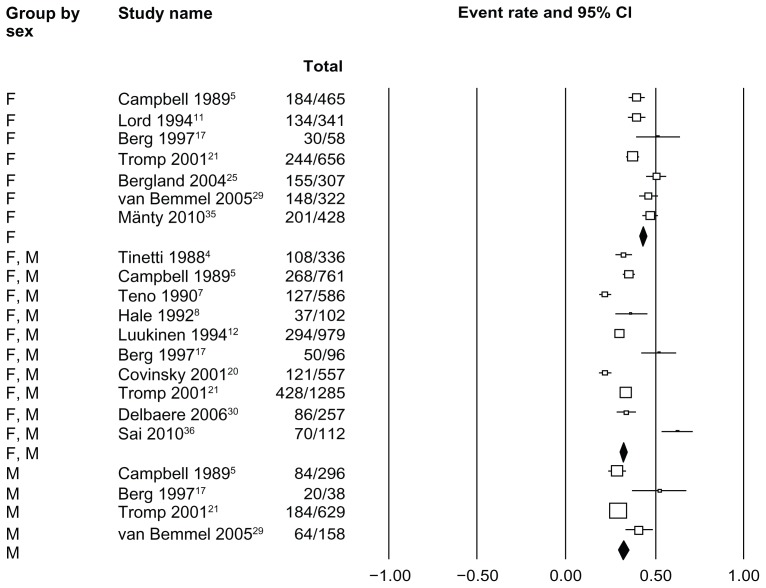
The median (range) annual fall prevalence rates for cohorts of women and men (10 studies), women alone (seven studies), and men alone (four studies) were, respectively, 0.334 (0.217–0.625), 0.460 (0.372–0.517), and 0.349 (0.284–0.526). All three of these data sets were statistically heterogeneous (Figure 1).
Figure 1.
Prevalence of low-impact falls in prospective cohorts of older community-based Western populations.
Notes: The event rate shown is the proportion of subjects with a low-impact fall per year. Abbreviations refer to women and men combined (F, M), women (F), and men (M). The median (range) fall prevalence rates for women/men (10 studies), women (seven studies), and men (four studies) are, respectively, 0.334 (0.217–0.625), 0.460 (0.372–0.517), and 0.349 (0.284–0.526). The pooled mean fall prevalence rates (95% confidence interval) for women/men (10 studies), women (seven studies), and men (four studies) are, respectively, 0.316 (0.303–0.329), 0.426 (0.407–0.445), and 0.316 (0.289–0.344) in the fixed-effects model and 0.343 (0.293–0.398), 0.437 (0.395–0.479), and 0.351 (0.288–0.431) in the random-effects model. P values of the Q statistic for the pooled studies of women/men, women, and men were, respectively, 0.000, 0.000, and 0.001; corresponding I2 values were 92.5%, 76.6%, and 81.2%.
Abbreviation: CI, confidence interval.
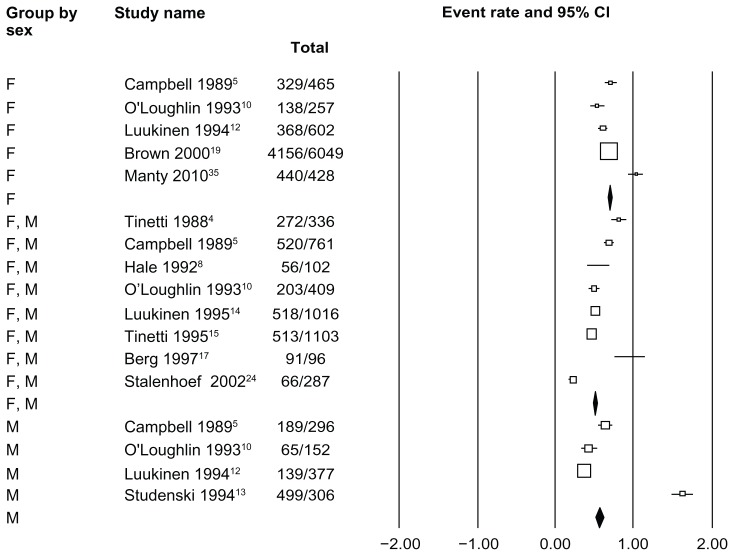
The median (range) fall incidence rates (95% confidence interval [CI]) for women/men (eight studies), women alone (five studies), and men alone (four studies) were, respectively, 0.530 (0.229–0.948), 0.687 (0.536–1.028), and 0.534 (0.368–1.630). The fall incidence rate of 1.630 per patient per year reported in a study of male veterans by Studenski et al13 is a statistical outlier among the studies of men; the median value (range) for studies of men excluding the one by Studenski et al (three determinations) is 0.428 (0.368–0.64). All of these data sets are statistically heterogeneous (Figure 2).
Figure 2.
Incidence of low-impact falls in prospective cohorts of older community-based Western populations.
Notes: The median (range) fall incidence rates (95% confidence interval) for women/men (eight studies), women (five studies), and men (four studies) are, respectively, 0.530 (0.229–0.948), 0.687 (0.536–1.028), and 0.534 (0.368–1.630). Among studies of men, the fall incidence rate of 1.630 per patient per year reported by Studenski et al13 (a study of male veterans) is a statistical outlier. The median (range) for studies of men excluding Studenski et al13 (three determinations) is 0.428 (0.368–0.640). The pooled fall incidence rates (95% confidence interval) for women/men (eight studies), women (five studies), and men (four studies) are, respectively, 0.498 (0.476–0.519), 0.688 (0.669–0.706), and 0.557 (0.51–0.601) in the fixed-effects model and 0.574 (0.453–0.694), 0.710 (0.601–0.820), and 0.763 (0.327–1.199) in the random-effects model. P values of the Q statistic for the pooled studies of women/men, women, and men were, respectively, 0.000, 0.000, and 0.000; corresponding I2 values were 93.9%, 96.4%, and 98.9%. The pooled fall incidence rate (95% confidence interval) in studies of men with Studenski et al13 excluded (three determinations) was 0.448 (0.402–0.494) in the fixed-effects model and 0.477 (0.309–0.645) in the random-effects model; P of Q 0.000, I2 91.6%.
Abbreviation: CI, confidence interval.
Rates of low-impact falls in Western men versus women
The median fall rates for men were lower than those for women, although ranges of values overlapped. However, in the four studies that reported data for both genders separately, fall rates in men and women were significantly different.5,17,21,29 The pooled risk ratio (95% CI) for fall prevalence in men versus women was 0.805 (95% CI 0.721–0.900; four determinations).5,17,21,29 The pooled rate ratio for fall incidence in men versus women was 0.757 (95% CI 0.578–0.991; three determinations).5,10,12
Prevalence and incidence of low-impact falls in older East Asian populations
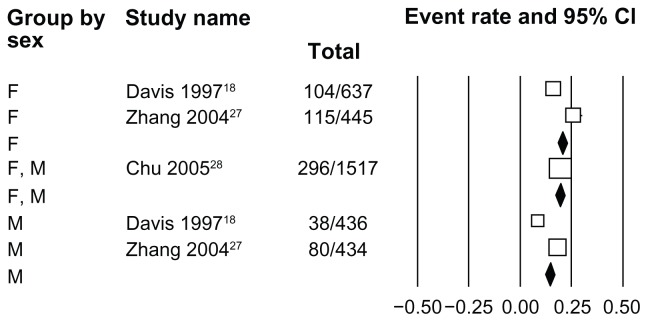
Three studies reported fall statistics for East Asian populations (Hawaiian Japanese, mainland Chinese, and Hong Kong Chinese, Supplementary Table A).18,27,28 The ranges of fall prevalence rates in East Asian women (two studies) and East Asian men (two studies) were, respectively, 0.163–0.258 and 0.087–0.184 (Figure 3). These ranges are lower than and do not overlap the corresponding ranges for Western women (0.372–0.517) and Western men 0.284–0.526.
Figure 3.
Prevalence of low-impact falls in prospective cohorts of older community-based East Asian populations.
Notes: The event rate is the proportion of subjects with a low-impact fall per year. Abbreviations refer to women and men combined (F, M), women (F), and men (M). The prevalence rate for the single study of women/men is 0.195. The ranges of prevalence rate values for women (two studies) and men (two studies) are, respectively, 0.163–0.258 and 0.087–0.184. The pooled mean fall prevalence rates (95% confidence interval) for women (two studies) and men (two studies) are, respectively, 0.206 (0.183–0.232) and 0.143 (0.121–0.169) in the fixed-effects model and 0.206 (0.128–0.315) and 0.129 (0.006–0.256) in the random-effects model. P values of Q statistic for the pooled studies of women, and men were, respectively, 0.000 and 0.000; corresponding I2 values were 93.1% and 94.0%.
Abbreviation: CI, confidence interval.
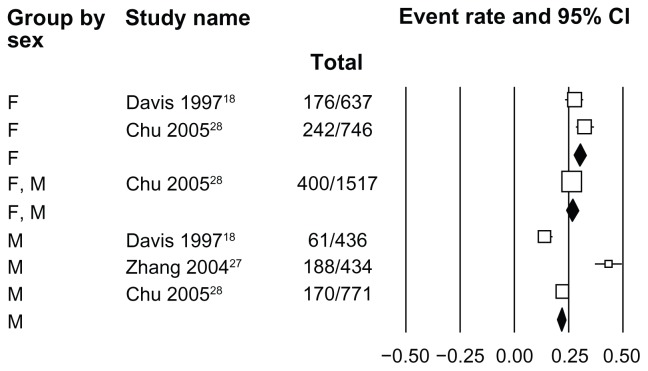
The fall incidence rates in East Asian women (two studies) and East Asian men (three studies) were 0.276–0.324 and 0.434–0.771 (Figure 4). The range of values for fall incidence in East Asian women is lower than and does not overlap that for Western women (0.536–1.028). The range for East Asian men overlaps that for Western men (0.368–1.630).
Figure 4.
Incidence of low-impact falls in prospective cohorts of older community-based East Asian populations.
Notes: The fall incidence rates in the two studies of women were 0.276 and 0.324; the median (range) of values in the three studies of men are 0.436 (0.434–0.771). The pooled fall incidence rates (95% confidence interval) for women (two studies) and men (three studies) are, respectively, 0.300 (0.271–0.347) and 0.215 (0.192–0.237) in the fixed-effects model, and 0.300 (0.253–0.347) and 0.261 (0.126–0.397) in the random-effects model. P values of Q statistic for the pooled studies of women and men were, respectively, 0.104 and 0.000; corresponding I2 values were 62.3% and 97.0%.
Abbreviation: CI, confidence interval.
Two studies reported fall prevalence rates for East Asian men and women separately.18,27 The risk ratio (95% CI) for fall prevalence in East Asian men versus women was 0.634 (0.479–0.838). Two studies reported fall incidence rates for East Asian men and women separately.18,28 The rate ratio (95% CI) for fall incidence in East Asian men versus women was 0.597 (0.447–0.798, P of Q 0.10).
Osteoporotic fractures resulting from low-impact falls
Proportion of low-impact falls resulting in osteoporotic fractures
Most of the data on fractures caused by low-impact falls comes from Western populations of community-dwelling women and men combined (Figure 5). In five cohorts of women and men (excluding one by Tinetti et al,15 which is an outlier), the pooled event rate (95% CI) was 0.041 (0.031–0.054) in the fixed-effects analysis (P of Q 0.15, I2 40.1%). In the Study of Osteoporotic Fractures, the largest (n = 6049) cohort study of (non-black) Western women, the proportion of falls resulting in nontraumatic, nonspinal fractures was 0.0445.19
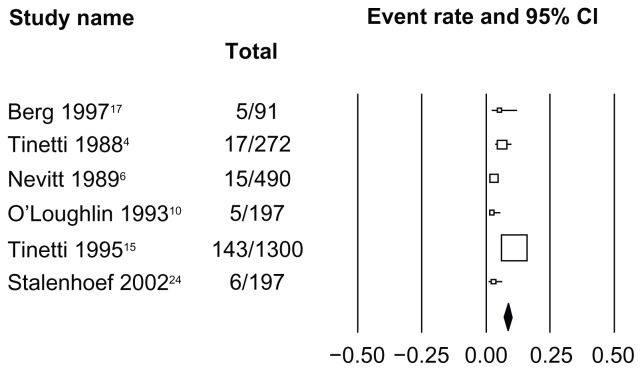
Figure 5.
Proportion of low-impact falls resulting in fractures in prospective cohorts of older community-based Western populations.
Notes: Shown is the proportion of falls resulting in fracture(s) in prospective community-dwelling cohorts of women and men, where both the numbers of falls and resulting fractures were reported. The attribution of fractures as osteoporotic is based on a fall defined as low-trauma in an elderly population. The pooled event rate (95% confidence interval) for the six cohorts of women/men is 0.085 (0.074–0.098) in the fixed-effects analysis and 0.048 (0.026–0.087) in the random-effects analysis; P of Q 0.000, I2 88.8%. For the five cohorts of women/men after excluding Tinetti et al,15 which is a statistical outlier, the pooled event rate (95% confidence interval) is 0.041 (0.031–0.054) in the fixed-effects analysis and 0.040 (0.027–0.058) in the random-effects analysis; P of Q 0.154, I2 40.1%. Note that all the fractures in the Berg et al17 cohort occurred in women, and none occurred in men.
Abbreviation: CI, confidence interval.
Proportion of low-impact fractures attributable to falls
The proportion of low-trauma fractures attributable to falls among the community-dwelling elderly was reported for the Study of Osteoporotic Fractures and Osteoporotic Fractures in Men Study cohorts of, respectively, women and men, and in several cross-sectional studies of women and men (Supplementary Table B). The range of values for low-trauma fractures at all sites, pelvis, or femoral neck was 0.860–0.950 (five studies, excluding the value of 0.623, which is a statistical outlier, Table 1).34 The value for fractures at all sites in the Study of Osteoporotic Fractures cohort was 0.940. The range was 0.71–0.75 in the two Study of Osteoporotic Fractures studies of fractures of the arm.
Table 1.
Proportion of low-trauma fractures attributable to low-impact falls in older community-based populationsa
| Citation | Design | Sex | Fracture site | N with fracture | Proportion of fractures due to low-impact falls |
|---|---|---|---|---|---|
| Nyberg 199616 | Cross-sectional | F/M | Femoral neck | 123 | 0.950 |
| SOF31 | Cohort | F | All sites | 3,211 | 0.940 |
| Breuil 200833 | Cross-sectional | F/M | Pelvic | 60 | 0.892 |
| van Helden 200834 | Cross-sectional | F | All sites | 406 | 0.872 |
| MrOS31 | Cohort | M | All sites | 346 | 0.860 |
| SOF9 | Cohort | F | Proximal humerus | 79 | 0.750 |
| SOF9 | Cohort | F | Distal forearm | 171 | 0.710 |
| van Helden 200834 | Cross-sectional | M | All sites | 162 | 0.623b |
Notes:
Populations ≥ 65 years, except > 50 years in van Helden et al34 and mean age 80 years in Breuil et al.33 Studies ranked in decreasing order of percent fractures attributable to low-impact falls;
statistical outlier among fracture sites excluding upper extremities.
Abbreviations: SOF, Study of Osteoporotic Fractures; MrOS, Osteoporotic Fractures in Men Study.
Proportion of fractures that are osteoporotic
Ten studies reported the proportion of fractures that are osteoporotic in women and men,23,26,32 women alone,1,22,26,31,34 and men alone.31 These studies varied in design, in fracture site classification, and in osteoporotic fracture definition (Supplementary Table B). Fractures were defined as osteoporotic by investigators in several large cohort studies.26,47,48 Other studies reported the proportion of subjects experiencing a fracture who had low bone mineral density (osteopenia and/or osteoporosis).1,22,34 The degree of trauma involved in fracture was reported in some studies.23,31,32
A range of 0.716–0.924 for fractures at all sites were osteoporotic (Table 2, eight studies, excluding the value of 0.530, which was a statistical outlier, from a registry in Sweden32). The range of values for four studies of women was 0.800–0.924 and the range for four studies of women/men or men (at all sites) was 0.716–0.786. The range for two studies reporting fractures of the arm was 0.613–0.615.
Table 2.
Proportion of all fractures that are osteoporotic in older community-based populationsa
| Study | Country | Sex | Age | Fracture site | N fractures | Proportion of fractures that are osteoporotic |
|---|---|---|---|---|---|---|
| SOF 200731 | USA | F | ≥65 | All sites | 3475 | 0.924 |
| Sheffield 200426 | UK | F | ≥75 | All sites | 291 | 0.832 |
| van Helden 200834 | Netherlands | F | >50 | All sites | 406 | 0.825 |
| Geusens 20021 | Belgium | F | ≥45 | All sites | 45 | 0.800 |
| MrOS 200731 | USA | M | ≥65 | All sites | 440 | 0.786 |
| Rotterdam 200426 | Netherlands | F/M | ≥55 | All sites | 989 | 0.776 |
| DOES 200426 | Australia | F/M | ≥60 | All sites | 405 | 0.743 |
| van Helden 200834 | Netherlands | M | >50 | All sites | 162 | 0.716 |
| Melton 200223 | USA | F/M | ≥35 | Distal forearm | 496 | 0.615 |
| EPIDOS 200222 | France | F | ≥75 | Proximal humerus | 98 | 0.613 |
| Bergstrom 200832 | Sweden | F/M | >50 | All sites | 13,279 | 0.530 |
Notes:
Studies ranked in decreasing order of osteoporotic fracture rate. Study descriptions and definitions of osteoporotic fracture in Table B (Supplementary material).
Abbreviations: SOF, Study of Osteoporotic Fractures; MrOS, Osteoporotic Fractures in Men Study; DOES, Dubbo Osteoporosis Epidemiology Study; EPIDOS, Epidémiologie de l’Ostéoporose Study.
Discussion
In Western cohorts of older women and men, annual prevalence rates of low-impact falls were within the range of 0.217–0.625. Fall prevalence rates were 20% lower in men than in women. A median of 4.1% of low-impact falls resulted in fractures in cohorts of Western women and men. The percentages of all low-trauma fractures attributable to low-impact falls and all fractures that were osteoporotic were similar, ranging from 86.0% to 95.0% and 71.6% to 92.4%, respectively. Corresponding rates of fractures of the arm were lower.
The data set for fall rates in East Asians was small (three studies). Because our analysis was restricted to articles in English, it is possible that some studies were missed. Nevertheless, fall prevalence rates for East Asians in the studies analyzed were consistently lower than corresponding rates for Western populations. A lower rate of falls among East Asians than among Western populations was first noted by Davis et al, who suggested that this could explain the lower rate of hip fractures in East Asian populations than in White populations.18,49
With minor exceptions, fall incidence rates showed the same demographic differences as those seen with fall prevalence. The individual studies of both fall prevalence and incidence rates were highly statistically heterogeneous. We examined the contribution of two variables, ie, gender ratio and age, to this heterogeneity in meta-regression of cohorts of Western women and men (AM, LW, unpublished data). There was no statistically significant relationship between fall prevalence and gender ratio. Note also that the fall rate data sets for the individual genders were heterogeneous. There was a statistically significant inverse relationship between fall prevalence and mean age. A possible explanation for this counterintuitive finding is that individuals more likely to fall tend to leave the community. Consistent with this, rates of falls were higher in studies of the institutionalized elderly. Means of annual fall incidence rates reported in studies of the hospitalized elderly and those in long-term care were 1.4 and 1.6, respectively, compared with a median of 0.53 reported here for studies of community-dwelling populations.2
Values for rates of low-impact falls and fractures may be applied to national statistics in illustrative calculations of the burden and cost of falls in the US. Point estimates for women and men indicate that 1.4% of the community-dwelling elderly experience a fracture annually due to a low-impact fall (0.334 × 0.041 × 100). Extrapolating to the 39 million US population ≥ 65 years living outside of skilled nursing facilities in 201050 yields a total of 0.53 million such fractures per year. The value of 1.4% is similar to an estimate from the 1997 US Medical Expenditure Panel Survey, which indicated that 7.1% of the community-dwelling elderly (≥65 years) received medical care for a fall-related injury and that 24.6% of these injuries were fractures.38 These figures suggest that 1.7% (product of 7.1% and 0.246%) of the community-dwelling elderly experienced a fall-related fracture.
The most recent estimates of costs of fall-related injuries in US adults > 65 years are for the year 2000.39 Fall-related major injuries can include fracture, joint dislocation, laceration requiring suture, and head injury resulting in loss of consciousness and hospitalization.51,52 Nonfatal fall-related fractures cost approximately $12 billion in direct medical expenditure. Estimates from the present analysis indicate that 71.6%–92.4% of fractures in community-dwelling older populations are osteoporotic, so the estimated cost of fall-related osteoporotic fractures would range from 8.6 billion (71.6% of $12 billion) to 11.1 billion (92.4% of $12 billion) in 2000 dollars, translating to $12.9 to 16.6 billion in 2010 dollars (inflated using the medical component of the Consumer Price Index). This estimate does not include nursing home stays attributable to fractures, which are an important contributor to costs,53,54 or the costs of nonfatal falls in the institutionalized population.
Conclusion
Osteoporotic fractures largely result from the combination of two factors, ie, low bone mass and a fall. In this review, we have updated epidemiologic statistics for rates of low-impact falls in older community-dwelling populations and estimated rates of fractures that can be considered to be osteoporotic. Application of these statistics to published analyses of national survey data on falls and fractures in 2000 suggests that there were 0.53 million fall-related osteoporotic fractures among the community-dwelling elderly in 2010.
Supplementary tables
Table SA.
Description of prospective cohort studies of falls in older community-based populations
| Citation | Population/ location | Sex | Age | Sample size | Outcomes reported | ||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Fall prevalence/ year | Fall incidence/1000 person-years | Falls with osteoporotic fracture (%)a | |||||
| Western populations | |||||||
| Women/men | |||||||
| Tinetti, 19884 | Yale, CT | F, M | ≥75 | 336 | + | + | + |
| Campbell 19895 | Mosgiel, New Zealand | F, M | ≥70 | 761 | + | + | |
| Nevitt 19896 | San Francisco, CAb | F, M | ≥60 | 325 | + | + | + |
| Teno 19907 | Medicare patients, RI | F, M | ≥65 | 586 | + | ||
| Hale 19928 | Greensboro, NC | F, M | ≥65 | 102 | + | + | |
| O’Loughlin 199310 | Montreal, CA | F, M | ≥65 | 409 | + | + | |
| Luukinen 199412 | N Finland | F, M | ≥70 | 979 | + | ||
| Luukinen 199514 | N Finland | F, M | ≥70 | 1,016 | + | + | |
| Tinetti 199515 | Yale, CT | F, M | ≥72 | 1,103 | + | + | |
| Berg 199717 | Oxford, OH | F, M | ≥60 | 96 | + | + | + |
| Covinsky 200120 | Clearwater, FL | F, M | ≥70 | 557 | + | ||
| Tromp 200121 | LASA, Netherlands | F, M | ≥65 | 1,285 | + | ||
| Stalenhoef 200224 | Maastricht, Netherlands | F, M | ≥70 | 287 | + | + | |
| Delbaere 200630 | Ghent, Belgium | F, M | ≥60 | 257 | + | ||
| Sai 201036 | Omaha, NE | F, M | 65–85 | 112 | + | ||
| Women | |||||||
| Lord 199411 | Sydney, Australia | F | ≥65 | 341 | + | ||
| Brown 200019 | Non-black, SOF | F | ≥72 | 6,049 | + | + | |
| Bergland 200425 | Oslo, Norway | F | ≥75 | 307 | + | + | |
| van Bemmel 200529 | Leiden, Netherlands | F, M | 85–86 | 480 | + | ||
| Manty 201035 | Central Finland | F | 63–76 | 428 | + | + | |
| Men | |||||||
| Studenski 199413 | Veterans, NC | M | ≥70 | 306 | + | ||
| East Asian populations | |||||||
| Chu 200528 | Chinese (Hong Kong) | F, M | ≥65 | 1,517 | + | + | |
| Davis 199718 | Japanese (Hawaii) | F, M | ≥60 | 1,073 | + | + | + |
| Zhang 200427 | Chinese (Nanjing) | F, M | ≥60 | 879 | + | ||
Notes:
Attribution of fractures as osteoporotic based on a fall defined as low trauma in an elderly population;
subjects with a prior fall.
Abbreviations: LASA, Longitudinal Aging Study Amsterdam; SOF, Study of Osteoporotic Fractures.
Table SB.
Description of studies of fractures in older community-based populations, by study design
| Study | Sex | Age | Fracture site | N fractures | Fractures due to low impact falls (%) | Fractures that are osteoporotic (%) | Definition of osteoporotic fracture |
|---|---|---|---|---|---|---|---|
| Prospective cohort | |||||||
| EPIDOS22 | F | ≥75 | Proximal humerus | 98 | + | A | |
| DOES26 | F/M | ≥60 | All sites | 405 | + | B | |
| Rotterdam26 | F/M | ≥55 | All sites | 989 | + | B | |
| Sheffield26 | F | ≥75 | All sites | 291 | + | B | |
| MrOS31 | M | ≥65 | All sites | 440 | + | + | C |
| SOF9,31 | F | ≥65 | |||||
| All sites | 3,475 | + | + | C | |||
| Distal forearm | 171 | + | |||||
| Proximal humerus | 79 | + | |||||
| Cross-sectional | |||||||
| van Helden 200834 | F, M | >50 | All sites | 568 | + | + | D |
| Nyberg 199616 | F/M | ≥65 | Femoral neck | 123 | + | ||
| Breuil 200833 | F/M | 80 E | Pelvic | 60 | + | ||
| Retrospective | |||||||
| Geusens 20021 | F | ≥45 | All sites | 45 | + | F | |
| Melton 200223 | F/M | ≥35 G | Distal forearm | 496 | + | C | |
| Registry | |||||||
| Bergstrom 200832 | F/M | >50 | All sites | 13,279 | + | C | |
Notes: A: Osteoporotic fracture defined as facture with low bone mineral density (T score < −2.5); B: Osteoporotic fracture determined by investigator; C: Osteoporotic fracture defined as low-trauma fracture; D: Osteoporotic fracture defined as fracture and low bone density (T score < −1.0 on dual X-ray absorptiometry of hip or spine); E: Mean age; F: Osteoporotic fracture defined as a non-high trauma fracture in women with low bone density (T score < −1.0 on single-energy X-ray absorptiometry of proximal radius); G: Mean age 65 for women (N = 303) and 52 for men (N = 191).
Abbreviations: DOES, Dubbo Osteoporosis Epidemiology Study; EPIDOS, Epidémiologie de l’Ostéoporose Study; MrOS, Osteoporotic Fractures in Men Study; SOF, Study of Osteoporotic Fractures.
Footnotes
Disclosure
Financial support for this work was provided by Merck and Co, Inc. The authors have no further conflicts of interest.
References
- 1.Geusens P, Autier P, Boonen S, Vanhoof J, Declerck K, Raus J. The relationship among history of falls, osteoporosis, and fractures in postmenopausal women. Arch Phys Med Rehabil. 2002;83(7):903–906. doi: 10.1053/apmr.2002.33111. [DOI] [PubMed] [Google Scholar]
- 2.Rubenstein LZ, Josephson KR. The epidemiology of falls and syncope. Clin Geriatr Med. 2002;18(2):141–158. doi: 10.1016/s0749-0690(02)00002-2. [DOI] [PubMed] [Google Scholar]
- 3.Ganz DA, Bao Y, Shekelle PG, Rubenstein LZ. Will my patient fall? JAMA. 2007;297(1):77–86. doi: 10.1001/jama.297.1.77. [DOI] [PubMed] [Google Scholar]
- 4.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319(26):1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 5.Campbell AJ, Borrie MJ, Spears GF. Risk factors for falls in a community-based prospective study of people 70 years and older. J Gerontol. 1989;44(4):M112–M117. doi: 10.1093/geronj/44.4.m112. [DOI] [PubMed] [Google Scholar]
- 6.Nevitt MC, Cummings SR, Kidd S, Black D. Risk factors for recurrent nonsyncopal falls. A prospective study. JAMA. 1989;261(18):2663–2668. [PubMed] [Google Scholar]
- 7.Teno J, Kiel DP, Mor V. Multiple stumbles: a risk factor for falls in community-dwelling elderly. A prospective study. J Am Geriatr Soc. 1990;38(12):1321–1325. doi: 10.1111/j.1532-5415.1990.tb03455.x. [DOI] [PubMed] [Google Scholar]
- 8.Hale WA, Delaney MJ, McGaghie WC. Characteristics and predictors of falls in elderly patients. J Fam Pract. 1992;34(5):577–581. [PubMed] [Google Scholar]
- 9.Kelsey JL, Browner WS, Seeley DG, Nevitt MC, Cummings SR. Risk factors for fractures of the distal forearm and proximal humerus. The Study of Osteoporotic Fractures Research Group. Am J Epidemiol. 1992;135(5):477–489. doi: 10.1093/oxfordjournals.aje.a116314. [DOI] [PubMed] [Google Scholar]
- 10.O’Loughlin JL, Robitaille Y, Boivin JF, Suissa S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol. 1993;137(3):342–354. doi: 10.1093/oxfordjournals.aje.a116681. [DOI] [PubMed] [Google Scholar]
- 11.Lord SR, Ward JA, Williams P, Anstey KJ. Physiological factors associated with falls in older community-dwelling women. J Am Geriatr Soc. 1994;42(10):1110–1117. doi: 10.1111/j.1532-5415.1994.tb06218.x. [DOI] [PubMed] [Google Scholar]
- 12.Luukinen H, Koski K, Hiltunen L, Kivela SL. Incidence rate of falls in an aged population in northern Finland. J Clin Epidemiol. 1994;47(8):843–850. doi: 10.1016/0895-4356(94)90187-2. [DOI] [PubMed] [Google Scholar]
- 13.Studenski S, Duncan PW, Chandler J, et al. Predicting falls: the role of mobility and nonphysical factors. J Am Geriatr Soc. 1994;42(3):297–302. doi: 10.1111/j.1532-5415.1994.tb01755.x. [DOI] [PubMed] [Google Scholar]
- 14.Luukinen H, Koski K, Laippala P, Kivela SL. Predictors for recurrent falls among the home-dwelling elderly. Scand J Prim Health Care. 1995;13(4):294–299. doi: 10.3109/02813439508996778. [DOI] [PubMed] [Google Scholar]
- 15.Tinetti ME, Doucette J, Claus E, Marottoli R. Risk factors for serious injury during falls by older persons in the community. J Am Geriatr Soc. 1995;43(11):1214–1221. doi: 10.1111/j.1532-5415.1995.tb07396.x. [DOI] [PubMed] [Google Scholar]
- 16.Nyberg L, Gustafson Y, Berggren D, Brannstrom B, Bucht G. Falls leading to femoral neck fractures in lucid older people. J Am Geriatr Soc. 1996;44(2):156–160. doi: 10.1111/j.1532-5415.1996.tb02432.x. [DOI] [PubMed] [Google Scholar]
- 17.Berg WP, Alessio HM, Mills EM, Tong C. Circumstances and consequences of falls in independent community-dwelling older adults. Age Ageing. 1997;26(4):261–268. doi: 10.1093/ageing/26.4.261. [DOI] [PubMed] [Google Scholar]
- 18.Davis JW, Ross PD, Nevitt MC, Wasnich RD. Incidence rates of falls among Japanese men and women living in Hawaii. J Clin Epidemiol. 1997;50(5):589–594. doi: 10.1016/s0895-4356(96)00430-1. [DOI] [PubMed] [Google Scholar]
- 19.Brown JS, Vittinghoff E, Wyman JF, et al. Urinary incontinence: does it increase risk for falls and fractures? Study of Osteoporotic Fractures Research Group. J Am Geriatr Soc. 2000;48(7):721–725. doi: 10.1111/j.1532-5415.2000.tb04744.x. [DOI] [PubMed] [Google Scholar]
- 20.Covinsky KE, Kahana E, Kahana B, Kercher K, Schumacher JG, Justice AC. History and mobility exam index to identify community-dwelling elderly persons at risk of falling. J Gerontol A Biol Sci Med Sci. 2001;56(4):M253–M259. doi: 10.1093/gerona/56.4.m253. [DOI] [PubMed] [Google Scholar]
- 21.Tromp AM, Pluijm SM, Smit JH, Deeg DJ, Bouter LM, Lips P. Fall-risk screening test: a prospective study on predictors for falls in community-dwelling elderly. J Clin Epidemiol. 2001;54(8):837–844. doi: 10.1016/s0895-4356(01)00349-3. [DOI] [PubMed] [Google Scholar]
- 22.Lee SH, Dargent-Molina P, Bréart G Epidos Group. Epidemiologie de l’Osteoporose Study. Risk factors for fractures of the proximal humerus: results from the EPIDOS prospective study. J Bone Miner Res. 2002;17(5):817–825. doi: 10.1359/jbmr.2002.17.5.817. [DOI] [PubMed] [Google Scholar]
- 23.Melton LJ, 3rd, Achenbach SJ, O’Fallon WM, Khosla S. Secondary osteoporosis and the risk of distal forearm fractures in men and women. Bone. 2002;31(1):119–125. doi: 10.1016/s8756-3282(02)00788-3. [DOI] [PubMed] [Google Scholar]
- 24.Stalenhoef PA, Diederiks JP, Knottnerus JA, Kester AD, Crebolder HF. A risk model for the prediction of recurrent falls in community-dwelling elderly: a prospective cohort study. J Clin Epidemiol. 2002;55(11):1088–1094. doi: 10.1016/s0895-4356(02)00502-4. [DOI] [PubMed] [Google Scholar]
- 25.Bergland A, Wyller TB. Risk factors for serious fall related injury in elderly women living at home. Inj Prev. 2004;10(5):308–313. doi: 10.1136/ip.2003.004721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kanis JA, Johansson H, Oden A, et al. A meta-analysis of prior corticosteroid use and fracture risk. J Bone Miner Res. 2004;19(6):893–899. doi: 10.1359/JBMR.040134. [DOI] [PubMed] [Google Scholar]
- 27.Zhang JG, Ishikawa-Takata K, Yamazaki H, Ohta T. Is a type A behavior pattern associated with falling among the community-dwelling elderly? Arch Gerontol Geriatr. 2004;38(2):145–152. doi: 10.1016/j.archger.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 28.Chu LW, Chi I, Chiu AY. Incidence and predictors of falls in the Chinese elderly. Ann Acad Med Singapore. 2005;34(1):60–72. [PubMed] [Google Scholar]
- 29.van Bemmel T, Vandenbroucke JP, Westendorp RG, Gussekloo J. In an observational study elderly patients had an increased risk of falling due to home hazards. J Clin Epidemiol. 2005;58(1):63–67. doi: 10.1016/j.jclinepi.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 30.Delbaere K, Van den Noortgate N, Bourgois J, Vanderstraeten G, Tine W, Cambier D. The Physical Performance Test as a predictor of frequent fallers: a prospective community-based cohort study. Clin Rehabil. 2006;20(1):83–90. doi: 10.1191/0269215506cr885oa. [DOI] [PubMed] [Google Scholar]
- 31.Mackey DC, Lui LY, Cawthon PM, et al. High-trauma fractures and low bone mineral density in older women and men. JAMA. 2007;298(20):2381–2388. doi: 10.1001/jama.298.20.2381. [DOI] [PubMed] [Google Scholar]
- 32.Bergstrom U, Bjornstig U, Stenlund H, Jonsson H, Svensson O. Fracture mechanisms and fracture pattern in men and women aged 50 years and older: a study of a 12-year population-based injury register, Umea, Sweden. Osteoporos Int. 2008;19(9):1267–1273. doi: 10.1007/s00198-007-0549-z. [DOI] [PubMed] [Google Scholar]
- 33.Breuil V, Roux CH, Testa J, et al. Outcome of osteoporotic pelvic fractures: an underestimated severity. Survey of 60 cases. Joint Bone Spine. 2008;75(5):585–588. doi: 10.1016/j.jbspin.2008.01.024. [DOI] [PubMed] [Google Scholar]
- 34.van Helden S, van Geel AC, Geusens PP, Kessels A, Nieuwenhuijzen Kruseman AC, Brink PR. Bone and fall-related fracture risks in women and men with a recent clinical fracture. J Bone Joint Surg Am. 2008;90(2):241–248. doi: 10.2106/JBJS.G.00150. [DOI] [PubMed] [Google Scholar]
- 35.Mänty M, Heinonen A, Viljanen A, et al. Self-reported preclinical mobility limitation and fall history as predictors of future falls in older women: prospective cohort study. Osteoporos Int. 2010;21(4):689–693. doi: 10.1007/s00198-009-0950-x. [DOI] [PubMed] [Google Scholar]
- 36.Sai AJ, Gallagher JC, Smith LM, Logsdon S. Fall predictors in the community dwelling elderly: a cross sectional and prospective cohort study. J Musculoskelet Neuronal Interact. 2010;10(2):142–150. [PubMed] [Google Scholar]
- 37.Ray NF, Chan JK, Thamer M, Melton LJ., 3rd Medical expenditures for the treatment of osteoporotic fractures in the United States in 1995: report from the National Osteoporosis Foundation. J Bone Miner Res. 1997;12(1):24–35. doi: 10.1359/jbmr.1997.12.1.24. [DOI] [PubMed] [Google Scholar]
- 38.Carroll NV, Slattum PW, Cox FM. The cost of falls among the community-dwelling elderly. J Manag Care Pharm. 2005;11(4):307–316. doi: 10.18553/jmcp.2005.11.4.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stevens JA, Corso PS, Finkelstein EA, Miller TR. The costs of fatal and non-fatal falls among older adults. Inj Prev. 2006;12(5):290–295. doi: 10.1136/ip.2005.011015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Davis JC, Robertson MC, Ashe MC, Liu-Ambrose T, Khan KM, Marra CA. International comparison of cost of falls in older adults living in the community: a systematic review. Osteoporos Int. 2010;21(8):1295–1306. doi: 10.1007/s00198-009-1162-0. [DOI] [PubMed] [Google Scholar]
- 41.Heinrich S, Rapp K, Rissmann U, Becker C, Konig HH. Cost of falls in old age: a systematic review. Osteoporos Int. 2010;21(6):891–902. doi: 10.1007/s00198-009-1100-1. [DOI] [PubMed] [Google Scholar]
- 42.Feder G, Cryer C, Donovan S, Carter Y. Guidelines for the prevention of falls in people over 65. The Guidelines’ Development Group. BMJ. 2000;321(7267):1007–1011. doi: 10.1136/bmj.321.7267.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organ Tech Rep Ser. 1994;843:1–129. [No authors listed] [PubMed] [Google Scholar]
- 44.Holmberg AH, Johnell O, Nilsson PM, Nilsson J, Berglund G, Akesson K. Risk factors for fragility fracture in middle age. A prospective population-based study of 33,000 men and women. Osteoporos Int. 2006;17(7):1065–1077. doi: 10.1007/s00198-006-0137-7. [DOI] [PubMed] [Google Scholar]
- 45.Holmberg AH, Johnell O, Nilsson PM, Nilsson JA, Berglund G, Akesson K. Risk factors for hip fractures in a middle-aged population: a study of 33,000 men and women. Osteoporos Int. 2005;16(12):2185–2194. doi: 10.1007/s00198-005-2006-1. [DOI] [PubMed] [Google Scholar]
- 46.Kanji G. 100 Statistical Tests. London, UK: SAGE Publications Ltd; 1999. [Google Scholar]
- 47.Hofman A, Grobbee DE, de Jong PT, van den Ouweland FA. Determinants of disease and disability in the elderly: the Rotterdam Elderly Study. Eur J Epidemiol. 1991;7(4):403–422. doi: 10.1007/BF00145007. [DOI] [PubMed] [Google Scholar]
- 48.Jones G, Nguyen T, Sambrook PN, Kelly PJ, Gilbert C, Eisman JA. Symptomatic fracture incidence in elderly men and women: the Dubbo Osteoporosis Epidemiology Study (DOES) Osteoporos Int. 1994;4(5):277–282. doi: 10.1007/BF01623352. [DOI] [PubMed] [Google Scholar]
- 49.Ross PD, Norimatsu H, Davis JW, et al. A comparison of hip fracture incidence among native Japanese, Japanese Americans, and American Caucasians. Am J Epidemiol. 1991;133(8):801–809. doi: 10.1093/oxfordjournals.aje.a115959. [DOI] [PubMed] [Google Scholar]
- 50.Werner C. The Older Population: 2010. Washington, DC: US Department of Commerce; 2011. [Google Scholar]
- 51.Nevitt MC, Cummings SR, Hudes ES. Risk factors for injurious falls: a prospective study. J Gerontol. 1991;46(5):M164–M170. doi: 10.1093/geronj/46.5.m164. [DOI] [PubMed] [Google Scholar]
- 52.Tinetti ME, Inouye SK, Gill TM, Doucette JT. Shared risk factors for falls, incontinence, and functional dependence. Unifying the approach to geriatric syndromes. JAMA. 1995;273(17):1348–1353. [PubMed] [Google Scholar]
- 53.Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med. 1997;337(18):1279–1284. doi: 10.1056/NEJM199710303371806. [DOI] [PubMed] [Google Scholar]
- 54.Rizzo JA, Friedkin R, Williams CS, Nabors J, Acampora D, Tinetti ME. Health care utilization and costs in a Medicare population by fall status. Med Care. 1998;36(8):1174–1188. doi: 10.1097/00005650-199808000-00006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table SA.
Description of prospective cohort studies of falls in older community-based populations
| Citation | Population/ location | Sex | Age | Sample size | Outcomes reported | ||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Fall prevalence/ year | Fall incidence/1000 person-years | Falls with osteoporotic fracture (%)a | |||||
| Western populations | |||||||
| Women/men | |||||||
| Tinetti, 19884 | Yale, CT | F, M | ≥75 | 336 | + | + | + |
| Campbell 19895 | Mosgiel, New Zealand | F, M | ≥70 | 761 | + | + | |
| Nevitt 19896 | San Francisco, CAb | F, M | ≥60 | 325 | + | + | + |
| Teno 19907 | Medicare patients, RI | F, M | ≥65 | 586 | + | ||
| Hale 19928 | Greensboro, NC | F, M | ≥65 | 102 | + | + | |
| O’Loughlin 199310 | Montreal, CA | F, M | ≥65 | 409 | + | + | |
| Luukinen 199412 | N Finland | F, M | ≥70 | 979 | + | ||
| Luukinen 199514 | N Finland | F, M | ≥70 | 1,016 | + | + | |
| Tinetti 199515 | Yale, CT | F, M | ≥72 | 1,103 | + | + | |
| Berg 199717 | Oxford, OH | F, M | ≥60 | 96 | + | + | + |
| Covinsky 200120 | Clearwater, FL | F, M | ≥70 | 557 | + | ||
| Tromp 200121 | LASA, Netherlands | F, M | ≥65 | 1,285 | + | ||
| Stalenhoef 200224 | Maastricht, Netherlands | F, M | ≥70 | 287 | + | + | |
| Delbaere 200630 | Ghent, Belgium | F, M | ≥60 | 257 | + | ||
| Sai 201036 | Omaha, NE | F, M | 65–85 | 112 | + | ||
| Women | |||||||
| Lord 199411 | Sydney, Australia | F | ≥65 | 341 | + | ||
| Brown 200019 | Non-black, SOF | F | ≥72 | 6,049 | + | + | |
| Bergland 200425 | Oslo, Norway | F | ≥75 | 307 | + | + | |
| van Bemmel 200529 | Leiden, Netherlands | F, M | 85–86 | 480 | + | ||
| Manty 201035 | Central Finland | F | 63–76 | 428 | + | + | |
| Men | |||||||
| Studenski 199413 | Veterans, NC | M | ≥70 | 306 | + | ||
| East Asian populations | |||||||
| Chu 200528 | Chinese (Hong Kong) | F, M | ≥65 | 1,517 | + | + | |
| Davis 199718 | Japanese (Hawaii) | F, M | ≥60 | 1,073 | + | + | + |
| Zhang 200427 | Chinese (Nanjing) | F, M | ≥60 | 879 | + | ||
Notes:
Attribution of fractures as osteoporotic based on a fall defined as low trauma in an elderly population;
subjects with a prior fall.
Abbreviations: LASA, Longitudinal Aging Study Amsterdam; SOF, Study of Osteoporotic Fractures.
Table SB.
Description of studies of fractures in older community-based populations, by study design
| Study | Sex | Age | Fracture site | N fractures | Fractures due to low impact falls (%) | Fractures that are osteoporotic (%) | Definition of osteoporotic fracture |
|---|---|---|---|---|---|---|---|
| Prospective cohort | |||||||
| EPIDOS22 | F | ≥75 | Proximal humerus | 98 | + | A | |
| DOES26 | F/M | ≥60 | All sites | 405 | + | B | |
| Rotterdam26 | F/M | ≥55 | All sites | 989 | + | B | |
| Sheffield26 | F | ≥75 | All sites | 291 | + | B | |
| MrOS31 | M | ≥65 | All sites | 440 | + | + | C |
| SOF9,31 | F | ≥65 | |||||
| All sites | 3,475 | + | + | C | |||
| Distal forearm | 171 | + | |||||
| Proximal humerus | 79 | + | |||||
| Cross-sectional | |||||||
| van Helden 200834 | F, M | >50 | All sites | 568 | + | + | D |
| Nyberg 199616 | F/M | ≥65 | Femoral neck | 123 | + | ||
| Breuil 200833 | F/M | 80 E | Pelvic | 60 | + | ||
| Retrospective | |||||||
| Geusens 20021 | F | ≥45 | All sites | 45 | + | F | |
| Melton 200223 | F/M | ≥35 G | Distal forearm | 496 | + | C | |
| Registry | |||||||
| Bergstrom 200832 | F/M | >50 | All sites | 13,279 | + | C | |
Notes: A: Osteoporotic fracture defined as facture with low bone mineral density (T score < −2.5); B: Osteoporotic fracture determined by investigator; C: Osteoporotic fracture defined as low-trauma fracture; D: Osteoporotic fracture defined as fracture and low bone density (T score < −1.0 on dual X-ray absorptiometry of hip or spine); E: Mean age; F: Osteoporotic fracture defined as a non-high trauma fracture in women with low bone density (T score < −1.0 on single-energy X-ray absorptiometry of proximal radius); G: Mean age 65 for women (N = 303) and 52 for men (N = 191).
Abbreviations: DOES, Dubbo Osteoporosis Epidemiology Study; EPIDOS, Epidémiologie de l’Ostéoporose Study; MrOS, Osteoporotic Fractures in Men Study; SOF, Study of Osteoporotic Fractures.