Abstract
Objective:
Atraumatic Restorative Treatment (ART) is a minimal intervention technique in the management of carious lesions, which results in negligible discomfort to the patient. The aim of this study was to assess and compare the discomfort levels during Atraumatic Restorative Treatment and Minimal Cavity Preparation (MCP: a method using rotary instruments) treatment procedures in a sample of school children in Davangere city.
Materials and Methods:
An experimental study was performed aimed at comparing discomfort levels as measured by subjective (Venham index) and objective (Heart rate) methods at six specified moments during the treatment. A total of 200 children were randomly divided into two groups of 100 each. In each child, one class II restoration with GIC in a deciduous molar was performed. One group received treatment using rotary instruments (MCP) and the other group with ART. Discomfort levels were measured using Venham index (behavioural dimension) and heart rate (physiological dimension).
Results:
The behavioural measurement revealed that in ART group the majority of the children(64%) showed an overall Venham score of ‘<1’(relaxed) as compared to MCP group in which the majority of children (76%) showed a Venham score of ‘1’(uneasy). The physiological measurement revealed that the children in ART group experienced less discomfort when compared to children in MCP group.
Conclusion:
The results of the study suggest that ART induces less discomfort; is patient friendly and has a higher extent of community acceptance when compared to MCP.
Keywords: ART, Minimal Cavity Preparation, Discomfort, Venham Index, Heart Rate, Anxiety
INTRODUCTION
Dental caries is still a major oral health issue in India. Several studies conducted in India have clearly shown that the prevalence of dental caries among children is high and at the same time there is high pervasiveness of unmet needs [1–5]. Inadequate infrastructure to provide basic dental health care, especially in rural areas is a ground reality. Hence search for alternative treatment modalities, which entail minimal equipment, yet provide practical and comfortable treatment solutions have arrived at Atraumatic Restorative Treatment (ART) as one of the options. ART was introduced in pursuit of providing preventive and curative oral care for the major populace in economically deprived countries [6, 7].
The advantages of ART are procedures which ensure minimal trauma, avoiding use of anesthesia and rotary instruments. These are essentially key factors in promoting dental anxiety, as they are highly invasive measures unlike the ART approach [8–10].
Literature is replete with respect to studies on technicalities of application and material sciences [11–13].
Diverse studies in Pakistan and Indonesia investigating and comparing pain and discomfort levels during ART, modified ART and Minimal Cavity Preparation (MCP) have been performed [14,10]. However, in India studies related to the acceptance level of subjects which depends on the comfort and anxiety levels experienced by the patient, have not been given due importance.
Fear of pain and discomfort have been attributed as the major reasons for non-seeking and non-receival of oral health care [15]. The demand for health care approaches which are simple, less painful and cause minimal discomfort are ever-increasing. Any objective intervention is sure to result in subjective changes, especially at an emotional level. Anxiety and pain during dental procedures result in a feeling of discomfort in the patient. Discomfort is a multidimensional construct consisting of a behavioral, cognitive and physiological component [16, 17]. Any attempt to measure patient discomfort should involve and model the multidimensional aspects of discomfort [10]. A systematic exploration of available literature revealed ample studies done in other countries [10, 18], whereas in India such studies may be few and scarce. Hence the aim of this study was to assess and compare the discomfort levels experienced during ART and MCP treatment procedures in a sample of school children in Davangere city.
MATERIALS AND METHODS
The present study is an experimental study conducted to assess the discomfort levels experienced by a sample of school children aged 6–8 years while performing ART and MCP.
This study comprises of an objective (heart rate: physiological dimension) as well as subjective (Venham scores: behavioural dimension) components. Prior to scheduling the study, official permission was obtained from the Deputy Director of Public Instructions, as well as authorities of the concerned schools at Davangere. Voluntary written informed consent was obtained from the parents of the children participating in the study prior to the examination. The time limit set for collection of data, examination and treatment of subjects participating in the study was four months.
The schedule was kept flexible to accommodate any unforeseen lapses. A specially prepared and pre-tested proform a, exclusively designed for collecting all the required and relevant general information and clinical findings was utilized. Dental caries was recorded according to the criteria of dentition status and treatment need index as described by WHO-1997 [19]. A pilot study was designed and carried out to check the feasibility and relevance of the study and study format.
The data obtained from the pilot study were used to arrive at the final sample size by applying specific statistical methods by keeping ‘α’ (significance level)at 5% and ‘d’ (absolute precision) at 3%.
Sampling Methodology:
The department of education in the district headquarters of Davangere has divided the city of Davangere into two blocks as North and South for administrative purposes. In the present study, a three stage random sampling technique was employed. In the first stage, 10 government primary schools were randomly selected from each block, arriving at a total of 20 schools.
In the second stage, from each of the randomly selected schools, all the school children aged 6–8 years were screened to identify those children who satisfy the following selection criteria.
Exclusion criteria:
i) A grossly destructed-tooth ii) A non-vital tooth iii) A tooth with a deep carious lesion where pulp exposure is expected iv) Children with the history related to anxiety disorders or neurological disorders.
Inclusion criteria:
Children having at least one multi surface cavity in a deciduous molar where no pulp exposure was present.
In the third stage, of all the children who satisfied the above selection criteria, only 10 children were randomly selected from each of the 20 schools to obtain a final sample of 200 children. Examination of the selected children was done within the campus of their schools; all examinations were carried out by a single investigator in the selected schools. Clinical examination of the study subjects included recording of dental caries based on WHO standard criteria for dental caries using a plane mouth mirror and a CPI probe [19], following appropriate infection control methods.
The oral examination and the treatment of the selected carious lesion were comprehensively carried out by the investigator for every child. The investigator and the recording assistant were trained and calibrated in using modified Venham’s behavioural scale and recording heart rate monitor values during ART and MCP procedures.
Referral and appointment:
From each school ten children who satisfied the selection criteria were selected and appointments were scheduled for the treatment. The initial response rate was 96% and appropriate rescheduling of appointments was carried out when children were unable to attend. When subjects dropped out due to other reasons, randomly selected children from the same school who satisfied the selection criteria replaced them. The treatment was provided in the department of community dentistry, Bapuji Dental College and Hospital, Davangere. Further provision of a referral card through which they could receive future dental treatment free of cost was arranged.
Details of the treatment procedure:
Random allocation of subjects into ART and MCP groups ensuring equal distribution of subjects into two groups −100 for ART group and 100 for MCP group thus arriving at a total sample of 200. A treatment schedule of six patients per day, 2–3 times in a week was followed over a period of 4 months.
Children in the experimental group were treated according to the ART approach using only hand instruments, such as hatchets and excavators and in the control group (MCP) using rotary instruments. In both groups, only the demineralized carious tooth tissue and unsupported enamel were removed. After cavity debridement, a matrix band and wooden wedges were applied. Cotton roll isolation prevented contamination of the cleaned cavity from saliva/blood. After conditioning the dentin for 15 seconds, hand mix glass-ionomer (Fuji –IX) restorations of cavities were performed in both groups. No local anesthesia was used in either group. Treatment was allocated randomly; the patients could be considered blinded.
Measuring discomfort levels:
The extent of discomfort was assessed by measuring the behavioral (psychological) dimension by using 6-point modified Venham index scale [20,21] (Table 1) and the physiological dimension by measuring the heart rate of the children using a heart rate monitor (Polar) [10] at six specified moments during dental treatment. Those moments were;
Table 1.
Venham Index (Modified 6-Point Scale According to Venham)
| Score | Features |
|---|---|
| 0 | Relaxed: smiling, willing and able to converse, displays behavior desired by the dentist. |
| 1 | Uneasy: concerned, may protest briefly to indicate discomfort, remain down or partially raised. Tense facial expression, high chest. Capable of cooperating. |
| 2 | Tense: tone of voice, questions and answers reflect anxiety. During stressful procedure, verbal protest, crying, hands tense and raised, but not interfering very much. Protest more distracting and troublesome. Child still complies with request to cooperate. |
| 3 | Reluctant: pronounced verbal protest, crying. Using hands to try to stop procedure. Treatment proceeds with difficulty. |
| 4 | Interference: general crying, body movements sometimes needing physical restraint. Protest disrupts procedure. |
| 5 | Out of contact: hard loud crying, swearing, screaming. Unable to listen, trying to escape.Physical restraint required. |
When the child entered the treatment room
At the start of excavation
At the moment of deepest excavation
At the moment of application of matrix band and wedges
At the moment of restoration
After completion of the treatment
Both the recording of the heart rate and the Venham scores were carried out by a trained assistant, who underwent training and calibration, while remaining unaware regarding the intention of the study.
Statistical procedures:
Statistical analysis was done using a personal computer with SPSS (Version 12) USA and Cystat software.
To analyze a difference in the Venham scores between both treatment groups, a chi-square test for trend was used.
Student’s t-test was used to analyze the heart rate of the patients recorded in both treatment groups. Confidence intervals were set at 95%. To investigate the effect of age and sex on the relationship between the treatment method and outcome measurements, a two-way ANOVA followed by Tukey’s honest significant difference test were done at each phase of the study.
RESULT
The results of the Venham scores during the specific phases of treatment session are summarized in Table 2.
Table 2.
Distribution and Comparison of Venham Scores Among Study Population (ART and MCP Groups) at Different Points of Time During Treatment
| Phases of treatment | Chi-square value | Degree of freedom ( df) | p-value |
|---|---|---|---|
| Entrance | 3.4280, | df=2 | p=0.1801 |
| Start | 59.7930, | df=2 | p=0.00000* |
| Deep Excavation | 88.6720 | df=2 | p=0.00000* |
| Matrix | 4.8060 | df=2 | p=0.09048 |
| Restoration | 8.4070 | df=2 | p=0.01495* |
| End | 3.2830 | df=2 | p=0.19368 |
| Overall | 40.1540 | df=2 | p=0.00000* |
Statistically significant
When the children entered the operating room, no significant difference between the ART and MCP groups for venham scores was found (p=0.180). During all five specific phases of treatment, the Venham scores of the children in the ART group were lower than those in the MCP group.
Highly significant differences were observed during the start of treatment (p=0.00) and deep excavation (p=0.00) phases of treatment reflecting that children in ART group were less anxious as compared to MCP. During the restorative phase, children were found to be more anxious in the MCP group as compared to ART group (p=0.01).
The overall Venham score showed that children treated with ART were significantly more comfortable and less anxious in comparison to children treated with MCP (p=0.00).
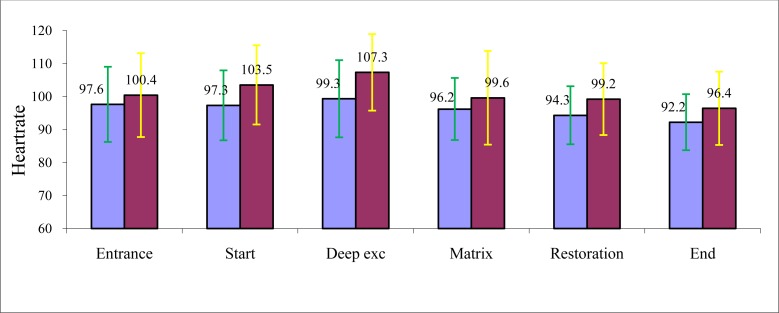
Student’s test on the heart rate measurements of the children showed significant difference between both treatment groups at all phases except at the entrance of children in to the operating room, clearly showing ART as more comfortable than MCP (Fig 1). Highly significant differences were observed at the start (p=0.0002) and during deep excavation (p=0.0000).To find out any effect of age and gender two way ANOVA followed by Tukey’s honest significant difference test were done in each phase of the study. Age did not show a significant influence on Venham scores in the subjects of ART group (F=0.4762) (p= 0.6227). The very nature of the treatment, which is less traumatic and more patient friendly could be aplausible reason. In the MCP group, age showed a significant influence on the outcome measurements with respect to Venham scores (F= 9.0743) (p=0.0002). Younger children showed higher Venham scores when compared to older children. The difference was statistically significant when comparing 6 and 7-year-old children (p=0.0369) and 6 and 8-year-old children (p=0.0002).Gender of the children did not show significant influence on Venham scores during ART and MCP procedures, indicating similar comfort and discomfort levels in both the groups. The influence of age appears to be strong on heart rate values of children in ART and MCP groups (p=0.0168 and p=0.0226, respectively). Tukey’s honest significant difference test shows this difference as statistically significant between 6 and 8-year-old children and 6 and 7-year-old children (p<0.05).
Fig 1.
Distribution and comparison of ART znd MCP groups with respect to heart rates of the children at six specified moments during dental treatment (vertical axis-heart rate)
The youngest age group (6-year-old children) showing higher heart rates, when compared to elder children (7 and 8-year-old children). Gender did not show any significant influence on the heart rate values, implying almost similar discomfort levels in both genders.
DISCUSSION
Pain and discomfort are often reported by patients undergoing dental treatment even in routine restorative procedures [22, 23]. Treatment episodes associated with pain contribute to the development of dental fear and irregular dental visiting behavior, with improper follow-up [24, 25].Thus ‘pain breeds pain’ and a vicious circle develops, with painful experiences leading to delay of dental appointments. Irregular care prevents treatment of minor problems, which then necessitate stressful dental procedures involving a higher chance of painful stimulation [26]. ART and MCP are two clinical intervention techniques, which employ “NO” or ”LESS” traumatic techniques, respectively in the management of caries. According to the results of this study, ART appears to be less stressful for children as demonstrated by the behavioral (Venham index) and physiological measurements (heart rate) in comparison to usual methods like Minimal Cavity Preparation. At baseline, comfort levels were similar in both groups when they entered the dental operatory, akin to findings in other studies [10, 27]. Hence any differences in the discomfort levels, which crop up during the treatment period may be attributed to the nature of intervention alone. There was a statistically significant difference in the Venham scores assessed between the two groups at the start of the treatment. The children in the MCP group demonstrated significantly higher Venham scores (VS>1) when compared to the ART group.
MCP involves drilling and filling and the very sight of the dental hand piece, the sound generated by rotary instruments and the trauma during treatment might be responsible for occurrence of fear and anxiety in the subjects. Ronald [8] reported that the sight, sound and feeling of the drill as the most fear-producing stimuli next to the sight of the syringe and sensation of anesthetic injection.
The present study has revealed that the traumatic intervention although minimal such as MCP, yet triggers fear and elevates discomfort levels when compared to ART, in concordance with other studies [10, 27]. Children in the ART group showed significantly less discomfort than MCP group during deep excavation. Similar findings were reported by several other researchers [10, 27]. This may be attributed to the mechanism of deep excavation, which is different in the MCP group when compared to the ART group.
Use of micromotor for excavation of deep caries may cause heat generation, when coupled with improper cooling, it may promote pain, which automatically triggers fear and discomfort. Bhaskar et al. [28] reported that heat production during tooth preparation due to inadequate cooling, drop in the intra-pulpal temperature due to overcooling or improper cooling and mechanical damage are major sources of trauma and pain [28]. The atraumatic nature of ART, where only gentle scooping out of caries with an excavator is performed, can be cited as the valid reason for lower discomfort levels experienced by children in the ART group. Children in the ART group overall were found to experience less discomfort than the MCP group. This may be due to the vast difference in the very nature of the treatment modality. Research suggests that dental anxiety is mainly associated with the ‘injection needle’ and the ‘bur’ [8, 9]. Both instruments were absent during the ART approach and this could suitably elucidate the higher acceptance of this method. In the present study, focus was on the ‘bur’ as ‘needle’ (local anesthesia) was not used. Similar findings were observed in few other studies [8, 10, 14, 18]. Exploration of available literature revealed very few studies using Venham index and applying similar methodology as in the present study [10]. In a few studies the authors have developed their own exclusive questionnaire to assess the subjective response of the individual to ART and MCP [18]. Certain investigators have assessed discomfort level at only few stages of treatment unlike in the present study, where discomfort levels are assessed at six standardized stages. Benjamin [29] found that heart rate is positively correlated to both dental anxiety and pain. Based on the above findings, heart rate was considered as a suitable indicator in our study to represent the extent of discomfort felt during the dental treatment similar to other studies [10].
In the present study, age showed a significant influence on Venham scores and heart rate values only in the MCP group. This may be credited to the fact that, stress coping capacity of younger children is invariably lower when compared to older children because of their psychological development [30, 31] also emphasizing the atraumatic nature of ART irrespective of the age factor.
The excessive need for restorative care in rural areas of India can be met by extensive outreach programs, where ART can be employed and practiced in a field setting. Although the apparent limitation of our study is that it was conducted in a clinical setting, judicious application of these results to a field setting maybe attempted, using the aid of additional research to reaffirm these results.
To conclude, the results of this study entail that children receiving ART experienced less discomfort than children receiving MCP.
While gender was not found to show significant differences, age did play a pivotal role in the degree of discomfort experienced, confirming the importance of the age factor in cooperative abilities. The demonstration of improved comfort levels experienced by children while ART procedures were performed can be an excellent indicator for implementing ART in the practical scenario. Oral health policymakers could include this measure as a major strategy in their outreach programs endeavoring caries control in the rural populace.
REFERENCES
- 1.Goyal A, Gauba K, Chawla HS, Kaur M, Kapur A. Epidemiology of dental caries in Chandigarh school children and trends over the last 25 years. J Indian SocPedodPrev Dent. 2007 Jul-Sep;25(3):115–8. doi: 10.4103/0970-4388.36559. [DOI] [PubMed] [Google Scholar]
- 2.Bali RK, Mathur VB, Talwar PP, Channa HB. National Oral Health Survey & Fluoride Mapping. 2002–2003. India, Dental Council of India, India, 2004. www.iaphd.org. Accessed on 22:06:2011.
- 3.Singh A, Purohit B, Sequeira P, Acharya S. Oral health status of 5-year-old Aborigine children compared with similar aged marginalised group in south western India. Int Dent J. 2011 Jun;61(3):157–62. doi: 10.1111/j.1875-595X.2011.00033.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grewal H, Verma M, Kumar A. Prevalence of dental caries and treatment needs in the rural child population of Nainital District, Uttaranchal. J Indian SocPedodPrev Dent. 2009 Oct-Dec;27(4):224–6. doi: 10.4103/0970-4388.57657. [DOI] [PubMed] [Google Scholar]
- 5.Dhar V, Bhatnagar M. Dental caries and treatment needs of children (6–10 years) in rural Udaipur, Rajasthan. Indian J Dent Res. 2009 Jul-Sep;20(3):256–60. doi: 10.4103/0970-9290.57352. [DOI] [PubMed] [Google Scholar]
- 6.Frencken J, Makoni FA. A treatment technique for tooth decay in deprived communities. World health. 1994;47:15–7. [Google Scholar]
- 7.World health Organization . Revolutionary new procedure for treating dental caries. Apr 7, 1994. Press release WHO/28. [Google Scholar]
- 8.Kleinknecht RA, Klepac RK, Alexander LD. Origins and characteristics of fear of dentistry. J Am Dent Assoc. 1973 Apr;86(4):842–8. doi: 10.14219/jada.archive.1973.0165. [DOI] [PubMed] [Google Scholar]
- 9.Ten Berge M, Hoogstraten J, Veerkamp JS, Prins PJ. The dental subscale of the children’s fear survey schedule: a factor analytic study in the Netherlands. Community Dent Oral Epidemiol. 1998 Oct;26(5):340–3. doi: 10.1111/j.1600-0528.1998.tb01970.x. [DOI] [PubMed] [Google Scholar]
- 10.Schriks MC, Van Amerongen WE. Atraumatic perspectives of ART: psychological and physiological aspects of treatment with and without rotary instruments. Community Dent Oral Epidemiol. 2003 Feb;31(1):15–20. doi: 10.1034/j.1600-0528.2003.00021.x. [DOI] [PubMed] [Google Scholar]
- 11.Phantumvanit P, Songpaisan Y, Pilot T, Frencken JE. Atraumatic restorative treatment (ART): a 3-year community field trial in Thailand--survival of one-surface restorations in the permanent dentition. J Public Health Dent. 1996;56:141–5. doi: 10.1111/j.1752-7325.1996.tb02424.x. [DOI] [PubMed] [Google Scholar]
- 12.Frencken JE, Makoni F, Sithole WD, Hackenitz E. Three-year survival of one surface ART restorations and glass-ionomer sealants in a school oral health programme in Zimbabwe. Caries Res. 1998;32(2):119–26. doi: 10.1159/000016441. [DOI] [PubMed] [Google Scholar]
- 13.Holmgren CJ, Lo EC, Hu D, Wan H. ART restorations and sealants placed in Chinese school children – results after 3 years. Community Dent Oral Epidemiol. 2000 Aug;28(4):314–20. doi: 10.1034/j.1600-0528.2000.280410.x. [DOI] [PubMed] [Google Scholar]
- 14.Rahimtoola S, van Amerongen E, Maher R, Groen H. Pain related to different ways of minimal intervention in the treatment of small caries lesions. ASDC J Dent Child. 2000 Mar-Apr;67(2):123–7. 83. [PubMed] [Google Scholar]
- 15.Savanheimo N, Vehkalahti MM, Pihakari A, Numminen M. Reasons for and parental satisfaction with children’s dental care under general anesthesia. Int J Paediatr Dent. 2005 Nov;15(6):448–54. doi: 10.1111/j.1365-263X.2005.00681.x. [DOI] [PubMed] [Google Scholar]
- 16.Gatchel RJ. Managing anxiety and pain during dental treatment. J Am Dent Assoc. 1992 Jun;123(6):37–41. doi: 10.14219/jada.archive.1992.0194. [DOI] [PubMed] [Google Scholar]
- 17.Aartman IH, van Everdingen T, Hoogstraten J, Schuurs AH. Self report measurements of dental anxiety and fear in children: a critical assessment. ASDC J Dent Child. 1998 Jul-Aug;65(4):252–8. 229–30. [PubMed] [Google Scholar]
- 18.Van Amerongen WE, Rahimtoola S. Is ART really atraumatic? Community Dent Oral Epidemiol. 1999 Dec;27(6):431–5. doi: 10.1111/j.1600-0528.1999.tb02044.x. [DOI] [PubMed] [Google Scholar]
- 19.WHO . Oral Health survey-Basic Methods. WHO. 4th edition. Geneva: 1997. [Google Scholar]
- 20.Venham L, Bengston D, Cipes M. Childrens response to sequential dental visits. J Dent Res. 1977 May;56(5):454–9. doi: 10.1177/00220345770560050101. [DOI] [PubMed] [Google Scholar]
- 21.Veerkamp JSJ, Gruythuysen RJM, van Amerongen WE, Hoogstraten J. Dental treatment of fearful children using nitrous oxide. Part 3; Anxiety during sequential visits. ASDC J Dent Child. 1993 May-Jun;60(3):175–82. [PubMed] [Google Scholar]
- 22.Litt MD. A model of pain and anxiety associated with acute stressors: distress in dental procedure. Behav Res Ther. 1996 May-Jun;34(5–6):459–76. doi: 10.1016/0005-7967(96)00015-0. [DOI] [PubMed] [Google Scholar]
- 23.Lindsay SJ, Wege P, Yates J. Expectations of sensations, discomfort and fear in dental treatment. Behav Res Ther. 1984;22(2):99–108. doi: 10.1016/0005-7967(84)90098-6. [DOI] [PubMed] [Google Scholar]
- 24.Locker D, Shapiro D, Liddel A. Negative dental experiences and their relationship to dental anxiety. Community Dent Health. 1996 Jun;13(2):86–92. [PubMed] [Google Scholar]
- 25.Skaret E, Raadal M, Berg E, Kvale G. Dental anxiety and dental avoidance among 12–18 year olds in Norway. Eur J Oral Sci. 1999 Dec;107(6):422–8. doi: 10.1046/j.0909-8836.1999.eos107602.x. [DOI] [PubMed] [Google Scholar]
- 26.Klags U, Kianifard S, Ulusoy O, Wehbein H. Anxiety sensitivity as predictor of pain in patients undergoing restorative dental procedures. Community Dent Oral Epidemiol. 2006 Apr;34(2):139–45. doi: 10.1111/j.1600-0528.2006.00265.x. [DOI] [PubMed] [Google Scholar]
- 27.Van Gemert-Schriks MC. Discomfort during atraumatic restorative treatment (ART) versus conventional restorative treatment. Ned Tijdschr Tandheelkd. 2007 May;114(5):213–7. [PubMed] [Google Scholar]
- 28.Bhaskar SN, Lilly GE. Intrapulpal temperature during cavity preparation. J Dent Res. 1965 Jul-Aug;44:644–7. doi: 10.1177/00220345650440040601. [DOI] [PubMed] [Google Scholar]
- 29.Benjamin C. Psychopysiological measurement of dental anxiety. Amsterdam: Academic centre for dentistry; 1995. [Google Scholar]
- 30.Kohnstamm R. Klein Ontwikkelingspsy chologie L 1993 ISBN 9031312061.
- 31.Liddell A, Locker D. Gender and age differences in attitudes to dental pain and dental control. Community Dent Oral Epidemiol. 1997 Aug;25(4):314–8. doi: 10.1111/j.1600-0528.1997.tb00945.x. [DOI] [PubMed] [Google Scholar]