Abstract
Objectives.
To examine family caregiver involvement for long-term care (LTC) residents during the last month of life. Researchers examined direct (personal care and meals) and indirect (management and monitoring) types of caregiver involvement and the relationship between the type of involvement and predisposing, enabling, and need characteristics. Researchers also examined whether the frequency of involvement changed during the end-of-life (EOL) period.
Method.
Researchers used an expanded version of Andersen’s Behavioral Model to conceptualize predictors of family involvement for 438 residents in 125 residential care/assisted living and nursing home settings. Bivariate and multivariate analyses examined relationships among variables.
Results.
More than one-half of family caregivers monitored, managed care and assisted with meals, and 40% assisted with personal care tasks. The enabling characteristic of days visited and the need characteristic of caregiver role strain were related to each of the 4 types of involvement. However, the other correlates were distinct to the type of involvement.
Discussion.
Families are involved in EOL care in LTC settings. Higher role strain is related to more involvement in each of the 4 types of involvement, suggesting that whether involvement is by desire, perceived need, or both, there is cause to more critically examine the family caregiver’s desired role and need for support.
Key Words: Long-term care facilities, Family caregiver involvement, End of life.
Background
More than 2 million older adults in the United States live in nursing homes (NHs) and residential care/assisted living (RC/AL) settings (National Center for Assisted Living, 2011; National Center for Health Statistics, 2012). Although some may return to their previous homes, most will remain and die either in the long-term care (LTC) setting or in a hospital soon after transfer from the LTC residence (Froggatt et al., 2006; Hanson, 2003; Zerzan, Stearns, & Hanson, 2000; Zimmerman et al., 2005). During the time older adults are living and dying in these settings, their care is provided by the LTC staff and often by family members who provided care before the LTC placement.
In fact, family involvement in LTC settings is the norm rather than the exception. For example, family caregivers, typically unpaid relatives or friends who provide, arrange, or oversee care, average between 4.0 and 9hr/week visiting and/or performing tasks (Gaugler, Anderson, Zarit, & Pearlin, 2004; Port et al., 2005). Although there, caregiving often involves hands-on care in addition to new roles such as monitoring care, advocating for the resident, and maintaining the resident’s continuity and connectivity with other family members and friends (Bern-Klug & Thompson, 2008; Davies & Nolan, 2006; Dempsey & Pruchno, 1993; Gaugler, 2005; Keefe & Fancey, 2000; Port, 2004).
Consequently, family involvement in LTC is a multidimensional construct that includes visiting, advocacy, and monitoring, as well as providing personal hands-on and emotional care (Gaugler, 2005; Whitlatch, Schur, Noelker, Ejaz, & Looman, 2001). It has been conceptualized as direct and indirect and also as instrumental and socioemotional support (Keefe & Fancey, 2000; Penrod, Kane, & Kane, 2000; Ross, Carswell, & Dalziel, 2001). Direct or instrumental involvement tasks include providing physical support as well as personal comforts, whereas indirect tasks include managing and overseeing care, being “on-call,” and developing a relationship with LTC staff.
Despite its multidimensional components, family involvement in LTC is often conceptualized and examined simply as the number and/or frequency of visits (Gaugler, 2005). Further, although researchers know that community-based family caregivers report more involvement, as well as increased strain and burden, during the end-of-life (EOL) period of their family members (Penrod, Hupcey, Baney, & Loeb, 2011; Redinbaugh, Baum, Tarbell, & Arnold, 2003; Schulz et al., 2003; Wolff, Dy, Frick, & Kasper, 2007), remarkably little is known about EOL involvement of family caregivers of dying LTC residents (Forbes-Thompson & Gessert, 2005; Oliver, Porock, & Zweig, 2005b; Whitaker, 2009; Zarit, 2004).
Thus, not only has little research addressed the multidimensional nature of family involvement, but little is known about family involvement in LTC at the EOL. Also unknown is whether the involvement of family caregivers changes at the EOL. This lack of knowledge makes it difficult to understand the family caregiver’s role, how it can be supported, and perhaps how it can be better integrated with the services provided by the LTC staff. Surely, the EOL is an important time in the life of a family caregiver, and understanding its context in the LTC setting has become increasingly important as the numbers of individuals living and dying in these settings has and will continue to increase (Teno, 2003; Zerzan et al., 2000).
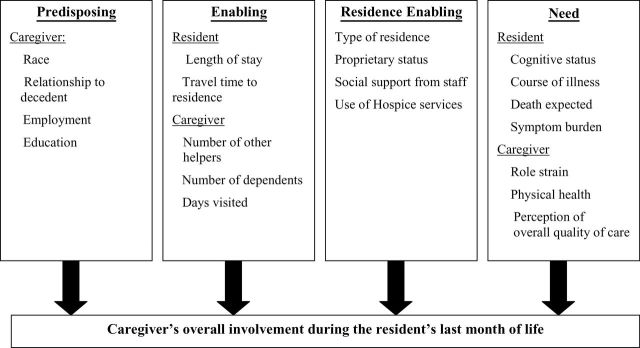
Researchers use the Behavioral Model of Health Services Use (Andersen, 1995; Andersen & Newman, 1973) to conceptualize family caregiver involvement at the EOL in LTC settings. The model outlines components that are predictive of health care utilization and has been successfully used to predict provision of family help in the community and also in LTC settings (Gaugler & Kane, 2001; Kwak, Haley, & Chiriboga, 2008; Lyons & Zarit, 1999; Montoro-Rodriguez, Kosloski, & Montgomery, 2003; Noelker & Bass, 1989). Gaugler and Kane (2001), in a study of informal help in assisted living, expanded the model by adding components of the LTC residence that may enable informal help. Researchers too add a residence-level component to the model (see Figure 1), thereby allowing this study to examine characteristics related to the family caregiver, resident, and residence.
Figure 1.
Conceptualization of family involvement based on Andersen’s Model of Health Service Use.
The model posits predisposing, enabling, and need characteristics to predict service provision and use of formal and informal support (Andersen, 1995; Andersen & Newman, 1973; Bass & Noelker, 1987; Bradley et al., 2002; Scharlach, Giunta, Chow, & Lehning, 2008). Predisposing characteristics are related to an individual’s propensity to use services; enabling characteristics enable or hinder informal or formal service use; and need characteristics are conditions, typically health conditions, that necessitate the need for services. Although researchers are unable to example causality in this article, the model does suggest an explanatory process whereby predisposing variables influence enabling variables, and enabling variables influence need, including perceived need (Andersen, 1995). For example, using the selected variables in this study, a predisposing characteristic such as employment may influence the enabling characteristic of number of days visited, which in turn may influence the need characteristic of caregiver role strain.
In this study, researchers examined characteristics found to be related to family involvement in general and more specifically to family involvement in LTC settings. Therefore, researchers place demographics (i.e., race, employment, and education) and relationship to the decedent in the predisposing domain (Friedemann, Montgomery, Rice, & Farrell, 1999; Yamamoto-Mitani, Aneshensel, & Levy-Storms, 2002). Although, white family caregivers and spousal caregivers have been documented to visit more and also to provide more help with instrumental activities of daily living, those with higher levels of education and competing demands such as employment are found to visit less (Gaugler, Leitsch, Zarit, & Pearlin, 2000; Gladstone, Dupuis, & Wexler, 2006; Port et al., 2001; Ross, Rosenthal, & Dawson, 1997; Seddon, Jones, & Boyle, 2002).
Based on previous studies, researchers conceptualize the resident’s length of stay, along with the caregiver’s travel time to residence and days visited as enabling characteristics (Dempsey & Pruchno, 1993; Gaugler, Anderson, & Leach, 2003). The number of other helpers available to provide care to the resident as well as the caregiver’s number of dependents may also enable or hinder caregiver involvement (Gladstone et al., 2006). The enabling characteristics of shorter travel time and days visited are typically associated with increased family involvement (Gaugler & Kane, 2001; Port et al., 2001), whereas additional helpers and other dependents may decrease the family caregiver’s involvement (Dempsey & Pruchno, 1993). Although, some studies indicate that family caregivers tend to visit less as the resident’s length of stay increases (Gaugler, 2005; Pruchno & Rose, 2002), less is known about the resident’s length of stay in relationship to caregiver involvement.
Researchers include characteristics of the setting (i.e., type and proprietary status), use of hospice, and perception of staff support as residence-enabling characteristics (Friedemann, Montgomery, Maiberger, & Smith, 1997; Gaugler & Kane, 2001; Port et al., 2005). Researchers expect that perceptions of more staff support will be related to less family involvement and that involvement will be higher in RC/AL and for-profit settings due to fewer staff in RC/AL and evidence of poorer outcomes in for-profit sites (Amirkhanyan, Kim, & Lambright 2008; O’Neill, Harrington & Kitchener, 2003). Further, a core value of hospice is the inclusion of family as part of the unit of care (Karikari-Martin, McCann, Herbert, Haffer, & Phillips, 2012; Oliver, Porock, Demiris, & Courtney, 2005a). Therefore, the use of hospice and/or knowing that death is expected (included subsequently in the need domain), both pivotal turning points in the caregiving experience, may be associated with higher involvement.
Finally, prior evidence suggests that poorer health of the care recipient will be associated with more caregiver involvement and that poorer caregiver health (physical and emotional) will be associated with less caregiver involvement (McCann, Hebert, Bienias, Morris, & Evans, 2004; Pavalko & Woodbury, 2000). Researchers have also documented that perceptions of poorer quality of care and an awareness that the resident is dying are associated with more involvement from family caregivers (Dobbs & Montgomery, 2005; Gaugler, 2005; Tornatore & Grant, 2004; Vohra Brazil, Hanna, & Abelson, 2004).
Using this model, researchers ask three research questions:
1. What types of involvement (i.e., personal care, meals, management, and monitoring) do family caregivers provide during the last month of life of LTC residents?
2. What predisposing, enabling, and need characteristics are associated with each type of involvement?
3. Does involvement change in the last month of life, and if so, is such a change associated with recognition that the EOL is near?
Method
Sample
Data were collected from NHs and RC/AL settings across four states (Florida, Maryland, New Jersey, and North Carolina) that participated in the Collaborative Studies of Long-Term Care End of Life in Residential Care/Assisted Living and Nursing Homes project. The settings constituted a stratified random sample from states that exhibit variability in RC/AL regulations, as described elsewhere (reference removed for anonymous review). A facility liaison (the administrator, care supervisor, or a designee) was contacted once a month to identify deaths of residents within the last month. A death was considered eligible if the resident had lived in the facility for ≥15 days of the last month of life and died in the facility or within 3 days of leaving the facility by transfer or discharge. Residents who did not meet these criteria were ineligible because it was determined there was insufficient time to fully reflect having received EOL care in that setting.
For each eligible death, the facility liaison identified the family member who was most involved in decisions and who visited and/or spoke with the resident or staff at least once during the last month of life. Researchers sent the identified family member a letter expressing condolences and informing him/her about the study approximately 8 weeks following the resident’s death; within 2 weeks of sending the letter, the family member was called and asked to participate in a telephone interview. All procedures were approved by the University of North Carolina’s Institutional Review Board.
Between July 2002 and January 2005, interviews were completed with one family caregiver for 451 decedents from 30 NHs and 94 RC/AL settings (44% of eligible decedents; 68% of those for whom a family member was identified by the setting and could be contacted within a 6-month window). Three-quarters (74%) of interviews were completed within 4 months post death and almost all (97%) were completed within 6 months post death. The caregiver sample for this study includes the 438 family members who provided complete information on task provision in the last month of life.
Dependent Variables
Researchers examined involvement in four caregiving tasks; two direct tasks and two indirect tasks. Caregivers were asked: in the last month of the resident’s life, how often did you help in activities such as: (a) bathing, toileting, dressing, or grooming; (b) mealtime, such as feeding; (c) management activities, such as managing finances or legal matters, straightening up the room or checking and cleaning clothes; and (d) monitoring and overseeing the care given by staff such as asking questions about medical care, diet, or medication. Caregivers were then asked to think more broadly about the last year of life and to indicate how often they were involved in each of the four types of tasks the year before the resident died.
Based on the distribution of the data, researchers defined the two direct involvement tasks (personal care and meals) as helping more or less than once in the past month. Researchers defined the two indirect tasks (monitoring and management) as helping more or less than twice a week.
Independent Variables
Predisposing variables were the caregiver’s race, relationship to decedent, employment status, and education. Enabling variables included length of stay in the LTC setting, travel time to the setting, number of other informal helpers available in the last month of the decedent’s life, the number of dependents of the caregivers, and the number of days caregivers visited in the last month of life.
Residence-enabling variables included the type of setting (RC/AL or NH), proprietary status, hospice services (yes/no), and social support from staff based on a nursing assistant support for families scale (Whitlatch et al., 2001). The scale consists of 11 items with scores ranging from 0 (never/almost never or no instance) to 3 (always/almost always). Scores were summed with higher scores indicating more perceived staff support (Cronbach alpha = .89).
Need variables consisted of decedent and family caregiver variables. Decedent need variables were cognitive status (impaired vs. intact), course of illness in the last year of life (stable health; steady, slow decline in health; or a series of ups and downs in health), death expected (yes/no), and symptom burden. Symptom burden was based on the caregiver’s perception of the decedent’s severity and frequency of symptom occurrence in four areas during the last month of life: pain, shortness of breath, skin cleanliness, and nutrition. Scores for each area ranged from 0 to 9 and were summed to provide a total score ranging from 0 to 36, with higher scores indicating more symptom burden (Hanson et al., 2008).
Family caregiver need variables consisted of caregiver role strain, physical health, and a perception of overall perceived quality of the LTC setting. Role strain was assessed using seven items related to the stress and strain a caregiver felt as a result of having a relative in a LTC setting (Whitlatch et al., 2001). Scores ranged from 7 to 28, with higher scores indicating more emotional strain (Cronbach alpha = .89). The general health subscale of the Medical Outcomes Study was used to assess physical health (McHorney, Ware, Lu, & Sherbourne, 1994). Scores ranged from 0 to 100, with higher scores reflecting better health (Cronbach alpha = .82; Ware & Sherbourne, 1992). Caregivers also rated the overall care the resident received in the last month of life (poor, fair, good, and very good).
Analysis
Researchers used descriptive statistics and correlations among measures of involvement in different types of tasks to report the type and frequency of tasks family caregivers provided in the last month of life. The statistical significance of associations among dichotomous measures of involvement in different tasks was evaluated using Generalized Estimating Equations (GEE) applied to logistic regression; GEE is employed, specifying an exchangeable working correlation, to account for lack of independence (i.e., clustering) among responses within settings (Diggle, Heagerty, Liang, & Zeger, 2002). Similarly, GEE logistic regression models were used to examine correlates of involvement in each type of task. Finally, to examine change in involvement from 1 year to the month prior to death, researchers used McNemar’s test (paired analyses).
Results
Most family caregivers were white (91%) and women (72%) with 48% being adult daughters or daughters-in-law (see Table 1). Their average age was 60. Sixty-four percent of the caregivers were married, 58% were employed, and 79% had some college experience or a college degree. Residents had an average length of stay of about 2 years (X = 2.3; SD = 2.7) and most (79%) were cognitively impaired. The course of illness for most (67%) was a steady, slow decline; a series of ups and downs for 23%; and stable health until death for the other 10%. Caregivers reported awareness that death was expected for 53% of the residents.
Table 1.
Distribution of Predisposing, Enabling, and Need Characteristics (N = 438)a
| N (%) or mean (SD) | |
|---|---|
| Predisposing: Caregiver characteristics | |
| Race/ethnicity | |
| White, non-Hispanic | 396 (90.6) |
| White, Hispanic | 9 (2.1) |
| Black | 30 (6.9) |
| Other | 2 (0.5) |
| Relationship to decedent | |
| Spouse | 37 (8.5) |
| Daughter or daughter-in-law | 208 (47.7) |
| Son or son-in-law | 84 (19.3) |
| Other | 107 (24.5) |
| Employed full or part time | 254 (58.3) |
| Education | |
| <High school | 11 (2.5) |
| High school | 81 (18.6) |
| Some college/trade school | 131 (30.0) |
| College | 213 (48.9) |
| Enabling | |
| Resident’s length of stay (years) | 2.3 (2.7) |
| Travel time to residence | |
| <15 min | 183 (42.0) |
| 15–30 min | 112 (25.7) |
| 30 min–1 hr | 75 (17.2) |
| >1 hr | 66 (15.1) |
| Number of other helpers | |
| None | 198 (45.4) |
| One | 122 (28.0) |
| Two or more | 116 (26.6) |
| Number of dependents | |
| None | 162 (37.4) |
| One | 149 (34.4) |
| Two | 50 (11.5) |
| Three or more | 72 (16.6) |
| Days visited in last month | 15.4 (10.4) |
| Residence enablingb | |
| Type | |
| RC/AL < 16 beds | 68 (15.5) |
| Traditional RC/AL | 35 (8.0) |
| New model RC/AL | 108 (24.7) |
| Nursing home | 227 (51.8) |
| Proprietary status | 318 (72.8) |
| Received hospice services | 228 (52.8) |
| Social support from staff (0–33) | 20.3 (8.0) |
| Need | |
| Resident cognitive status—impaired | 344 (78.7) |
| Resident course of illness | |
| Stable health | 44 (10.1) |
| Steady, slow decline | 292 (67.1) |
| Series of ups and downs | 99 (22.8) |
| Death was expected | 230 (52.8) |
| Resident symptom burden (0–36) | 17.9 (7.1) |
| Family caregiver role strain (7–28) | 18.5 (5.4) |
| Family caregiver physical health (0–100) | 75.6 (16.1) |
| Quality of care | |
| Fair poor | 44 (10.1) |
| Good | 119 (27.2) |
| Very good | 274 (62.7) |
Notes. RC/AL = residential care/assisted living; SD = standard deviation.
aThe sample is family respondents with missing data for no more than one task (in last month); the actual sample size varies from 379 to 438 based on missing data for some characteristics.
bSome residence characteristics (type, size, proprietary status, % Medicaid) are measured at the facility level (N = 126 facilities) but are shown in this table applied at the person level.
The majority of the caregivers (68%) lived within 30min and visited an average of 15.4 (SD = 10.4) days in the last month of life. Ten percent of caregivers reported fair or poor quality of care, 27% reported good quality of care, whereas the other 63% reported very good quality of care.
In terms of types of tasks conducted in the last month of life, 69% of caregivers were involved in monitoring care; 61% in meals; 56% in management, and 40% were involved in the provision of personal care (see Table 2). The mean number of task in which they were involved was 2.3 (SD = 1.3). Caregivers reported monitoring care, 17 times on average in the last month of life; managing care, 13.2 times; helping with meals, 10.8 times; and providing personal care, 9.7 times.
Table 2.
Distribution of Family Involvement in Last Month of Life (N = 438)
| Taska | N (%) involved | Number of times family caregiver helped in past month | Correlations among tasksc | ||
|---|---|---|---|---|---|
| Mean (SD) | Meals | Management | Monitoring | ||
| Personal careb | 177 (40.4) | 9.7 (24.1) | .28**** | .16*** | .22**** |
| Meals | 269 (61.4) | 10.8 (16.1) | .18*** | .29**** | |
| Management | 247 (56.4) | 13.2 (12.7) | .36**** | ||
| Monitoring | 301 (68.7) | 17.0 (17.2) | |||
Notes. SD = standard deviation.
aFor personal care and meals, involvement is defined as helping > 1 time in the past month; for management and monitoring, involvement is defined as helping at least twice a week (i.e., >8.7 times per month).
bPersonal care includes bathing, toileting, and dressing (which were asked as a single item) and grooming.
cPhi correlations for involvement in pairs of tasks, with involvement (yes/no) defined previously.
*p < .05. **p < .01. ***p < .005. ****p < .001; tested using logistic regression using Generalized Estimating Equations to account for clustering within residences.
Personal Care
Multivariate analyses (Table 3) showed that the enabling characteristics of days visited as well as the facility-enabling characteristic of facility type were associated with provision of personal care. Family caregivers who visited more days (OR [odds ratio] = 1.05; p = .001) provided more personal care. Further, residents in both smaller RC/AL settings (OR = .37; p = .01) and new model settings (OR = .33) provided less personal care than those in NHs (p = .01). In addition, the need characteristic of higher caregiver role strain (OR = 1.06; p = .04) was associated with more provision of personal care. No predisposing variables were associated with personal care.
Table 3.
Logistic Regression for Family Involvement in Each of Four Tasks (N = 416)a
| Characteristic | Family involvement in… | |||||||
|---|---|---|---|---|---|---|---|---|
| Personal care | Meals | Management | Monitoring | |||||
| Odds ratio (95% CI) | p Value | Odds ratio (95% CI) | p Value | Odds ratio (95% CI) | p Value | Odds ratio (95% CI) | p Value | |
| Predisposing | ||||||||
| Not white/non-Hispanic | 1.27 (0.73, 2.21) | .38 | 0.50 (0.20, 1.25) | .24 | 0.73 (0.34, 1.53) | .42 | 1.58 (0.71, 3.51) | .29 |
| Family relationship | ||||||||
| Spouse | 0.67 (0.28, 1.60) | .36 | 1.80 (0.67, 4.88) | .42 | 1.41 (0.54, 3.74) | .76 | 0.27 (0.09, 0.80) | .04 |
| Son or son-in-law | 0.67 (0.36, 1.24) | 1.01 (0.57, 1.77) | 1.05 (0.51, 2.18) | 0.86 (0.43, 1.73) | ||||
| Other | 0.60 (0.33, 1.11) | 0.84 (0.50, 1.41) | 1.25 (0.73, 2.14) | 0.46 (0.25, 0.84) | ||||
| Daughter or daughter-in-law | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | ||||
| Family working full or part-time | 1.14 (0.67, 1.93) | .64 | 1.18 (0.67, 2.07) | .59 | 1.28 (0.79, 2.08) | .33 | 1.13 (0.61, 2.09) | .70 |
| Caregiver has college degree | 1.17 (0.71, 1.92) | .56 | 0.93 (0.59, 1.47) | .76 | 1.10 (0.67, 1.80) | .71 | 1.83 (1.04, 3.22) | .04 |
| Enabling | ||||||||
| Length of stay (months) | 1.00 (1.00, 1.01) | .29 | 1.00 (0.99, 1.01) | .85 | 0.99 (0.99, 1.00) | .07 | 0.99 (0.98, 1.00) | .14 |
| Travel time to facility | ||||||||
| <15 min | 1.37 (0.63, 2.94) | .59 | 0.75 (0.42, 1.35) | .11 | 3.25 (1.66, 6.36) | .007 | 0.97 (0.51, 1.87) | .72 |
| 15–30 min | 0.92 (0.44, 1.96) | 1.48 (0.72, 3.03) | 1.70 (0.81, 3.56) | 0.86 (0.40, 1.86) | ||||
| 30min to 1 hr | 1.45 (0.62, 3.40) | 1.06 (0.55, 2.04) | 1.85 (0.92, 3.74) | 1.40 (0.64, 3.06) | ||||
| >1 hr | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | ||||
| No. of other helpers (0, 1, 2+) | 1.38 (1.01, 1.91) | .06 | 1.42 (1.05, 1.92) | .03 | 1.23 (0.94, 1.61) | .13 | 1.32 (0.93, 1.86) | .14 |
| No. of dependents (0, 1, 2, 3+) | 0.90 (0.69, 1.17) | .46 | 1.00 (0.80, 1.24) | .99 | 0.89 (0.74, 1.07) | .23 | 0.75 (0.59, 0.96) | .03 |
| Days visited in last month | 1.05 (1.02, 1.08) | .001 | 1.08 (1.04, 1.11) | <.001 | 1.04 (1.01, 1.07) | .01 | 1.12 (1.08, 1.16) | <.001 |
| Residence enabling | ||||||||
| Type | ||||||||
| RC/AL < 16 beds | 0.37 (0.18, 0.78) | .01 | 1.09 (0.59, 2.03) | .95 | 1.51 (0.71, 3.20) | .51 | 1.27 (0.62, 2.61) | .64 |
| Traditional RC/AL | 0.96 (0.45, 2.05) | 0.81 (0.32, 2.10) | 1.94 (0.79, 4.72) | 0.83 (0.43, 1.59) | ||||
| New model RC/AL | 0.33 (0.18, 0.62) | 0.99 (0.53, 1.83) | 1.43 (0.69, 2.96) | 0.82 (0.42, 1.60) | ||||
| Nursing home | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | ||||
| For-profit | 1.65 (0.94, 2.87) | .08 | 0.51 (0.30, 0.87) | .02 | 1.12 (0.63, 2.01) | .70 | 1.21 (0.63, 2.31) | .57 |
| Received hospice services | 1.24 (0.77, 1.98) | .38 | 0.82 (0.49, 1.38) | .47 | 0.85 (0.54, 1.35) | .50 | 1.27 (0.75, 2.14) | .37 |
| Social support from staff (0–33) | 1.00 (0.96, 1.04) | .97 | 1.02 (0.99, 1.06) | .21 | 0.99 (0.95, 1.03) | .57 | 1.04 (1.00, 1.09) | .08 |
| Need | ||||||||
| Cognitive status intact | 1.38 (0.79, 2.42) | .26 | 0.72 (0.39, 1.34) | .32 | 1.37 (0.78, 2.42) | .28 | 0.82 (0.46, 1.46) | .498 |
| Course of illness | ||||||||
| Stable health | 0.65 (0.30, 1.40) | .33 | 0.60 (0.31, 1.17) | .16 | 0.37 (0.17, 0.80) | .05 | 0.30 (0.11, 0.82) | .05 |
| Series of ups and downs | 1.27 (0.75, 2.14) | 0.67 (0.38, 1.18) | 0.98 (0.53, 1.81) | 0.56 (0.30, 1.05) | ||||
| Steady, slow decline | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | ||||
| Expected death | 1.05 (0.65, 1.70) | .85 | 0.83 (0.51, 1.37) | .48 | 0.90 (0.52, 1.57) | .72 | 0.57 (0.30, 1.08) | .08 |
| Symptom burden high (18+) | 0.75 (0.47, 1.20) | .25 | 0.81 (0.49, 1.33) | .41 | 1.04 (0.64, 1.68) | .88 | 1.43 (0.79, 2.59) | .24 |
| Caregiver role strain (7–28) | 1.06 (1.00, 1.11) | .04 | 1.06 (1.00, 1.11) | .05 | 1.07 (1.01, 1.13) | .01 | 1.07 (1.01, 1.13) | .02 |
| Caregiver general health score (0–100) | 1.00 (0.99, 1.01) | .83 | 0.99 (0.98, 1.01) | .48 | 0.99 (0.98, 1.01) | .44 | 1.00 (0.98, 1.01) | .50 |
| Quality of care | ||||||||
| Fair poor | 1.61 (0.61, 4.20) | .51 | 2.55 (1.01, 6.46) | .12 | 1.02 (0.36, 2.93) | .68 | 2.25 (0.49,10.32) | .54 |
| Good | 1.39 (0.77, 2.50) | 1.42 (0.81, 2.48) | 0.78 (0.44, 1.40) | 1.01 (0.53, 1.90) | ||||
| Very good | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | ||||
Notes. CI = confidence interval; RC/AL = residential care/assisted living.
aGeneralized Estimating Equations (GEE) applied to logistic model, specifying an exchangeable correlation structure for residents within facilities. A separate model is estimated for involvement in each of the four tasks. Odds ratios are adjusted for all characteristics shown as well as a dummy variable for unknown symptom burden. Confidence limits based on GEE robust standard error estimates; p value is for Type III score test.
Meals
Similar to personal care, enabling and facility-enabling characteristics were associated with provision of meals. In the case of enabling characteristics, caregivers who visited more days (OR = 1.08; p < .001) and those with more helpers (OR = 1.42; p < .03) provided more help with meals. For facility-enabling characteristics, residents in for-profit facilities (OR = .51; p = .02) had less family involvement with meals than residents in not for-profit settings. Although no predisposing characteristic was associated, the need characteristic of caregiver role strain (OR = 1.06; p = .05) was again significant, with those who reported higher levels of role strain providing more help with meals.
Management
Enabling characteristics were once again associated with involvement. For provision of management tasks, shorter distance from facility (OR = 3.25; p = .007) and days visited (OR = 1.04; p = .01) were associated with more management tasks. Similarly to the involvement with personal care and meals, higher role strain (OR = 1.07; p = .01) was associated with provision of more management. The need characteristic of course of illness, in this case stable health, was associated with providing less management (OR = .37; p = .05). Also similar to provision of personal care and meals, no predisposing variable was associated with the provision of management.
Monitoring
Results showed that the predisposing characteristics of family caregiver education and relationship to decedent were associated with monitoring. Spouses (OR = .27) and other relatives (OR = .46) provided less monitoring than adult daughters or daughters-in-law (p = .04). However, a college education (OR = 1.83; p = .04) was associated with more monitoring. The enabling characteristic of more days visited (OR = 1.12; p < .001) was also associated with more monitoring, whereas caregivers with more dependents (OR = .75; p = .03) provided less monitoring. In term of need characteristics, the course of illness, in this case a stable course of health (OR = .30; p = .05), was related to less monitoring, whereas higher role strain (OR = 1.07; p = .02) was again related to provision of more involvement.
Comparing involvement during the last year to the last month of life, there was a statistically significant change in the degree of involvement when an EOL period was recognized (data not shown). For example, when death was expected, the percent of family caregivers who reported involvement in care monitoring (at least two times per week) increased from 45% in the last year of life to 63% in the last month of life (p < .001). Similar increases in the percent of caregivers who helped with meals (52%–57%; p = .03) and management activities (47%–52%; p = .003) were noted when death was expected. However, there was no significant change in providing assistance in personal care when the EOL was expected.
Discussion
Researchers asked three research questions related to family involvement at the EOL in LTC settings. Answering the first question (types of involvement during the last month of life), researchers found that the family caregivers were involved in both direct and indirect tasks. More than one-half of family caregivers were involved with indirect tasks of monitoring and managing care and the direct task of assisting with meals. Further, although it has been suggested that family members often leave more direct tasks such hands-on personal care to staff, approximately 40% of the family caregivers in this study provided hands-on care such as bathing, toileting, dressing, or grooming.
Findings related to the third question (does involvement change in the last month of life, and if so, is such a change associated with recognition that the EOL is near) indicated that family caregivers tend to be more involved in all examined types of involvement, except personal care when an EOL period was recognized. Given that high levels of symptom burden are still evident at the EOL for many residents and that family members often want to be involved in EOL decision making and “accompany” their loved one on his/her EOL journey, this is an encouraging finding. It also adds to the growing and needed knowledge base related to EOL involvement of family caregivers of dying LTC residents (Forbes-Thompson & Gessert, 2005; Oliver et al., 2005; Whitaker, 2009; Zarit, 2004).
Together, these findings compel one to appreciate and highlight the benefits of family involvement at the EOL for residents of LTC settings, and question whether their care and outcomes would be worse if not for this involvement. It also calls into question the strain that caregivers experience. Researchers know, for example, that caregivers who reported higher emotional strain have increased mortality and stroke risk (Haley, Roth, Howard, & Stafford, 2010; Schulz & Beach, 1999).
For question two (what predisposing, enabling, and need characteristics are associated with each type of involvement), researchers found that the enabling characteristic of days visited and the need characteristic of caregiver role strain were related to all four types of involvement. When significant, all other correlates were distinct to the type of involvement. Therefore, not only is involvement multidimensional, the correlates are also distinct.
Similar to findings in other studies, caregivers who visited more often were more involved (Dempsey & Pruchno, 1993, Gaugler et al., 2000; Penrod et al., 2000), again attesting to their role as being more than visitors. However, the finding that caregivers who reported higher role strain were more involved is both intriguing and of potential concern. Of course, given the cross-sectional nature of this study, researchers cannot determine whether higher strain led to more involvement or whether more involvement led to higher strain. However, regardless of the direction of effect, whether involvement is by desire or perceived need, there is cause to more critically examine the family caregiver’s desired role and need for support. Further, as suggested by Ross and colleagues (2001), LTC staff should support the desired roles that family members are willing and able to provide.
Surprisingly, predisposing characteristics were related only to monitoring. Those with a college degree provided more monitoring than those without, perhaps because they were more aware of the need for monitoring. Also, spouses and other caregivers provided less monitoring than adult daughters. Again, it may well be that daughters are more sensitized to the need to monitor care. However, it is notable that daughters were not more involved in other care tasks, especially personal care. Also notable is that this finding differs from other studies documenting that spouses are typically more involved in care than other family caregivers (Ross et al., 1997; Seddon et al., 2002).
Researchers too found that the addition of the facility-enabling category was an informative and meaningful addition to Andersen’s model. Researchers found that caregivers in smaller RC/AL and new model settings provided less personal care (bathing, toileting, dressing, or grooming) than families of NH residents. The facility-enabling variable of for-profit facilities was related to less provision of help with meals. Interestingly, the facility-enabling correlates were related to less provision of the direct tasks of personal care and meals and not to the indirect tasks of monitoring and management, perhaps attesting to the need for more direct care from staff for the often sicker population in larger and more traditional care facility such as NHs.
Conversely, related to indirect tasks of management and monitoring was the need characteristic of a steady course of health during the last month of life. Lower levels of management and monitoring were reported when the resident had a steady course of health during the last month of life compared with those who exhibited a steady, slow decline, suggesting that families and staff both recognize and respond to residents who are in a declining state. The implications of this finding relate to its converse, that more attention may be needed when the trajectory of decline is less stable. Also noteworthy, is the absence of other need characteristics, such as resident’s cognitive status and caregiver’s physical health that are often found to be associated with level of involvement (Gaugler et al., 2003). Further, the need domain in the Andersen’s model is often the most relevant domain.
Even though studies document that family involvement positively affects the care of residents and the emotional health of residents and family caregivers (Gaugler & Teaster, 2006; Gaugler et al., 2003, Jablonski, Reed, & Maas, 2005; Levy-Storms & Miller-Martinez, 2005; Maas et al., 2004; Port et al., 2001; Robison et al., 2007), an important implication of this study is that researchers, LTC staff, and others need to be sensitive as to why, how, and how much family caregivers want to be involved (Andershed, 2006; Bauer & Nay, 2003; Duncan & Morgan, 1994; Reid, Chappell, & Gish, 2007; Tornatore & Grant, 2004). Whether they are providing more care to residents because of personal desire or based on perceptions of the existing quality of LTC may be important in terms of the caregiver’s emotional and physical health outcomes (Williams et al., 2008). Of course, the cross-sectional nature of these data make it difficult to discern the direction of effect, and information is missing to understand why (or why not) caregivers were involved and the extent to which their role was fulfilling.
The retrospective design that asks recently bereaved caregivers to reflect upon an emotional time and to reflect on two time points (1 month and 1 year before death) may affect recall and is a limitation of the study. Further, there was some bias in the sample, such that families from NHs were less likely to provide data than those from RC/AL settings. Although, the multidimensional examination of caregiver involvement as well as the intensity of the involvement were strengths of this study, additional findings related to satisfaction with involvement, and reasons for involvement would contribute to a more nuanced understanding of family involvement in LTC and further understanding of whether involvement is by personal desire or based on other perceptions such as quality of care.
On the other hand, this study has made important contributions in illuminating the family’s role in EOL care in LTC, and the conditions under which family caregiver involvement is more likely. Knowing that involvement is less when the resident course of illness is stable and that involvement increases when EOL is expected is highly relevant for communication between care providers and families. It implies, as does other work, that communication with physicians and other LTC staff is important not only for family satisfaction but also because it can prepare families for their important role in EOL care in LTC (Biola et al., 2007; Penrod et al., 2011; Stagno, Zhukovsky, & Walsh, 2000; Teno, 2003).
Although researchers and others recommend and encourage LTC staff to prepare families for impending death and to work with family caregivers in the ways they want to be involved (Bauer & Nay, 2003; Davies & Nolan, 2006; Forbes, Bern-Klug, Gessert, 2000; Hanson, Henderson & Menon, 2002; Vohra et al., 2004), it is important to acknowledge that the LTC workforce itself also needs support at the EOL, such as more training and more volunteer manpower (Caron, Griffith, & Arcand, 2005; Oliver et al., 2005; Wetle, Shield, Teno, Miller, & Welch, 2005; Zimmerman, Sloane, Hanson, Mitchell, & Shy, 2003). Thus, it may be that the best model to follow in moving forward is one that attends to the well-being of family caregivers at the EOL and also to the capacity of the LTC workforce.
Funding
This work was supported by the National Institute on Aging (Grants R01 AG18967 and K02 AG00970).
Author Contributions
Sharon Williams: Responsible for conceptualization of manuscript; selection of measures specific to manuscript and overall responsibility of manuscript.
Christianna Williams: Responsible for conceptualization and conduct of analyses and tables; participation in the discussion section and overall review of manuscript.
Sheryl Zimmerman: Responsible for conceptualization of parent study and overall oversight and conduct of parent study and conceptualization and completion of this manuscript.
Acknowledgments
We thank the staff, residents, and family members who participated in the Collaborative Studies of Long-Term Care for their time and commitment to learning more about and improving the quality of life in residential care/assisted living communities and nursing homes. Thanks also are given to Drs. Carol Whitlatch and the late Elizabeth Clipp for guidance on measures and conceptualization.
References
- Amirkhanyan A. A.,, Kim H. J.,, Lambright K. T. (2008). Does the public sector outperform the nonprofit and for-profit sectors? Evidence from a national panel study on nursing home quality and access. Journal of Policy Analysis and Management 27 326–353 [DOI] [PubMed] [Google Scholar]
- Andersen R. M. (1995). Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior 36 1–10 [PubMed] [Google Scholar]
- Andersen R.,, Newman J. F. (1973). Societal and individual determinants of medical care utilization in the United States. The Milbank Memorial Fund Quarterly: Health and Society 51 95–124 [PubMed] [Google Scholar]
- Andershed B. (2006). Relatives in end-of-life care - part 1: A systematic review of the literature the five last years, January 1999 – February 2004. Journal of Clinical Nursing 15 1158–1169 [DOI] [PubMed] [Google Scholar]
- Bass D. M.,, Noelker L. S. (1987). The influence of family caregivers on elder’s use of in-home services: An expanded conceptual framework. Journal of Health and Social Behavior 28 184–196 [PubMed] [Google Scholar]
- Bauer M.,, Nay R. (2003). Family and staff partnerships in long-term care. A review of the literature. Journal of Gerontological Nursing 29 46–53 [DOI] [PubMed] [Google Scholar]
- Bern-Klug M.,, Thompson S. (2008). Responsibilities of family members to nursing home residents: “She’s the only mother I got”. Journal of Gerontological Nursing 34 43–52 [DOI] [PubMed] [Google Scholar]
- Biola H.,, Sloane P. D.,, Williams C. S.,, Daaleman T. P.,, Williams S. W.,, Zimmerman S. (2007). Physician communication with family caregivers of long-term care residents at the end of life. Journal of the American Geriatrics Society 55 846–856 [DOI] [PubMed] [Google Scholar]
- Bradley E. H.,, McGraw S. A.,, Curry L.,, Buckser A.,, King K. L.,, Kasl S. V.,, Andersen R. (2002). Expanding the Andersen model: The role of psychosocial factors in long-term care use. Health Services Research 37 1221–1242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caron C. D., Griffith J., Arcand M. (2005). End-of-life decision making in dementia Dementia 4 113–136 [Google Scholar]
- Davies S.,, Nolan M. (2006). ‘Making it better’: Self-perceived roles of family caregivers of older people living in care homes: A qualitative study. International Journal of Nursing Studies 43 281–291 [DOI] [PubMed] [Google Scholar]
- Dempsey N. P., Pruchno R. A. (1993). The family’s role in the nursing home: Predictors of technical and non-technical assistance Journal of Gerontological Social Work 21 127–145 [Google Scholar]
- Diggle P., Heagerty P., Liang K. Y., Zeger S. Analysis of longitudinal data. Oxford University Press; (2002). [Google Scholar]
- Dobbs D., Montgomery R. J. V. (2005). Family satisfaction with residential care provision: A multi-level analysis Journal of Applied Gerontology 24 453–474 [Google Scholar]
- Duncan M. T.,, Morgan D. L. (1994). Sharing the caring: Family caregivers’ views of their relationships with nursing home staff. The Gerontologist 34 235–244 [DOI] [PubMed] [Google Scholar]
- Forbes S.,, Bern-Klug M.,, Gessert C. (2000). End-of-life decision making for nursing home residents with dementia. Journal of Nursing Scholarship 32 251–258 [DOI] [PubMed] [Google Scholar]
- Forbes-Thompson S.,, Gessert C. E. (2005). End of life in nursing homes: Connections between structure, process, and outcomes. Journal of Palliative Medicine 8 545–555 [DOI] [PubMed] [Google Scholar]
- Friedemann M. L.,, Montgomery R. J.,, Maiberger B.,, Smith A. A. (1997). Family involvement in the nursing home: Family-oriented practices and staff-family relationships. Research in Nursing & Health 20 527–537 [DOI] [PubMed] [Google Scholar]
- Friedemann M. L.,, Montgomery R. J.,, Rice C.,, Farrell L. (1999). Family involvement in the nursing home. Western Journal of Nursing Research 21 549–567 [DOI] [PubMed] [Google Scholar]
- Froggatt K. A.,, Wilson D.,, Justice C.,, MacAdam M., Leibovici K., Kinch J., Choi J. (2006). End-of-life care in long-term care settings for older people: A literature review. International Journal of Older People Nursing 1 45–50 [DOI] [PubMed] [Google Scholar]
- Gaugler J. E. (2005). Family involvement in residential long-term care: A synthesis and critical review. Aging & Mental Health 9 105–118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaugler J. E., Anderson K. A., Leach C. R. (2003). Predictors of family involvement in residential long-term care Journal of Gerontological Social Work 42 3–26 [Google Scholar]
- Gaugler J. E.,, Anderson K. A.,, Zarit S. H.,, Pearlin L. I. (2004). Family involvement in nursing homes: Effects on stress and well-being. Aging & Mental Health 8 65–75 [DOI] [PubMed] [Google Scholar]
- Gaugler J. E., Kane R. A. (2001). Informal help in the assisted living setting: A 1-year analysis Family Relations 50 335–347 [Google Scholar]
- Gaugler J. E., Leitsch S. A., Zarit S. H., Pearlin L. I. (2000). Caregiver involvement following institutionalization: Effects of preplacement stress Research on Aging 22 337–359 [Google Scholar]
- Gaugler J. E.,, Teaster P. (2006). The family caregiving career: Implications for community-based long-term care practice and policy. Journal of Aging & Social Policy 18 141–154 [DOI] [PubMed] [Google Scholar]
- Gladstone J. W.,, Dupuis S. L.,, Wexler E. (2006). Changes in family involvement following a relative’s move to a long-term care facility. Canadian Journal on Aging 25 93–106 [DOI] [PubMed] [Google Scholar]
- Haley W. E.,, Roth D. L.,, Howard G.,, Stafford M. M. (2010). Caregiving strain and estimated risk for stroke and coronary heart disease among spouse caregivers: Differential effects by race and sex. Stroke 41 331–336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson L. C. (2003). Creating excellent palliative care in nursing homes. Journal of Palliative Medicine 6 7–9 [DOI] [PubMed] [Google Scholar]
- Hanson L. C.,, Eckert J. K.,, Dobbs D.,, Williams C. S.,, Caprio A. J.,, Sloane P. D.,, Zimmerman S. (2008). Symptom experience of dying long-term care residents. Journal of the American Geriatrics Society 56 91–98 [DOI] [PubMed] [Google Scholar]
- Hanson L. C.,, Henderson M.,, Menon M. (2002). As individual as death itself: A focus group study of terminal care in nursing homes. Journal of Palliative Medicine 5 117–125 [DOI] [PubMed] [Google Scholar]
- Jablonski R. A.,, Reed D.,, Maas M. L. (2005). Care intervention for older adults with Alzheimer’s disease and related dementias: Effect of family involvement on cognitive and functional outcomes in nursing homes. Journal of Gerontological Nursing 31 38–48 [DOI] [PubMed] [Google Scholar]
- Karikari-Martin P.,, McCann J. J., Herbert L. E., Haffer S. C., Phillips M. (2012). Do community and caregiver factors influence hospice use at the end of life among older adults with Alzheimer Disease? Journal of Hospice & Palliative Nursing 14 225–237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keefe J., Fancey P. (2000). The care continues: Responsibility for elderly relatives before and after admission to a long term care facility Family Relations 49 235–244 [Google Scholar]
- Kwak J.,, Haley W. E.,, Chiriboga D. A. (2008). Racial differences in hospice use and in-hospital death among Medicare and Medicaid dual-eligible nursing home residents. The Gerontologist 48 32–41 [DOI] [PubMed] [Google Scholar]
- Levy-Storms L., Miller-Martinez D. (2005). Family caregiver involvement and satisfaction with institutional care during the 1st year after admission Journal of Applied Gerontology 24 160–174 [Google Scholar]
- Lyons K. S.,, Zarit S. H. (1999). Formal and informal support: The great divide. International Journal of Geriatric Psychiatry 14 183–192 [PubMed] [Google Scholar]
- Maas M. L.,, Reed D.,, Park M.,, Specht J. P., Schutte D., Kelley L. S., Buckwalter K. C. (2004). Outcomes of family involvement in care intervention for caregivers of individuals with dementia. Nursing Research 53 76–86 [DOI] [PubMed] [Google Scholar]
- McCann J. J.,, Hebert L. E.,, Bienias J. L.,, Morris M. C.,, Evans D. A. (2004). Predictors of beginning and ending caregiving during a 3-year period in a biracial community population of older adults. American Journal of Public Health 94 1800–1806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHorney C. A.,, Ware J. E.,, Jr., Lu J. F.,, Sherbourne C. D. (1994). The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Medical Care 32 40–66 [DOI] [PubMed] [Google Scholar]
- Montoro-Rodriguez J.,, Kosloski K.,, Montgomery R. J. (2003). Evaluating a practice-oriented service model to increase the use of respite services among minorities and rural caregivers. The Gerontologist 43 916–924 [DOI] [PubMed] [Google Scholar]
- National Center for Assisted Living (NCAL) (2011). Resident profile Retrieved June 17, 2011, from http://www.ahcancal.org/ncal/resources/Pages/ResidentProfile.aspx
- National Center for Health Statistics (NCHS) (2012). Health, United States, 2008 Retrieved May 17, 2012,from http://www.cdc.gov/nchs/data/hus/2010/117.pdf
- Noelker L. S.,, Bass D. M. (1989). Home care for elderly persons: Linkages between formal and informal caregivers. Journal of Gerontology 44 S63–S70 [DOI] [PubMed] [Google Scholar]
- O’Neill C.,, Harrington C.,, Kitchener M. (2003). Quality of care in nursing homes: An analysis of relationships among profit, quality, and ownership. Medical Care 41 1318–1330 [DOI] [PubMed] [Google Scholar]
- Oliver D. P.,, Porock D.,, Demiris G.,, Courtney K. (2005a). Patient and family involvement in hospice interdisciplinary teams. Journal of Palliative Care 21 270–276 [PubMed] [Google Scholar]
- Oliver D. P.,, Porock D.,, Zweig S. (2005b). End-of-life care in U.S. nursing homes: A review of the evidence. Journal of the American Medical Directors Association 6 S21–S30 [DOI] [PubMed] [Google Scholar]
- Pavalko E. K.,, Woodbury S. (2000). Social roles as process: Caregiving careers and women’s health. Journal of Health and Social Behavior 41 91–105 [PubMed] [Google Scholar]
- Penrod J.,, Hupcey J. E.,, Baney B. L.,, Loeb S. J. (2011). End-of-life caregiving trajectories. Clinical Nursing Research 20 7–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penrod J. D. Kane R. A. Kane R. L. (2000).Effects of post-hospital informal care on nursing home discharge Research on Aging 22 66–82 [Google Scholar]
- Port C. L. (2004). Identifying changeable barriers to family involvement in the nursing home for cognitively impaired residents The Gerontologist 44 770–778 [DOI] [PubMed] [Google Scholar]
- Port C. L.,, Gruber-Baldini A. L.,, Burton L.,, Baumgarten M.,, Hebel J. R.,, Zimmerman S. I.,, Magaziner J. (2001). Resident contact with family and friends following nursing home admission. The Gerontologist 41 589–596 [DOI] [PubMed] [Google Scholar]
- Port C. L.,, Zimmerman S.,, Williams C. S.,, Dobbs D.,, Preisser J. S.,, Williams S. W. (2005). Families filling the gap: Comparing family involvement for assisted living and nursing home residents with dementia. The Gerontologist 45 87–95 [DOI] [PubMed] [Google Scholar]
- Pruchno R. A., Rose M. S. (2002). Time use by frail older people in different care settings Journal of Applied Gerontology, 21 5–23 [Google Scholar]
- Redinbaugh E. M.,, Baum A.,, Tarbell S.,, Arnold R. (2003). End-of-life caregiving: What helps family caregivers cope? Journal of Palliative Medicine 6 901–909 [DOI] [PubMed] [Google Scholar]
- Reid R. C., Chappell N. L., Gish J. A. (2007). Measuring family perceived involvement in individualized long-term care Dementia 6 89–104 [Google Scholar]
- Robison J.,, Curry L.,, Gruman C.,, Porter M.,, Henderson C. R.,, Jr., Pillemer K. (2007). Partners in caregiving in a special care environment: Cooperative communication between staff and families on dementia units. The Gerontologist 47 504–515 [DOI] [PubMed] [Google Scholar]
- Ross M. M.,, Carswell A.,, Dalziel W. B. (2001). Family caregiving in long-term care facilities. Clinical Nursing Research 10 347–363 [DOI] [PubMed] [Google Scholar]
- Ross M., Rosenthal C., Dawson P. (1997). Spousal caregiving in the institutional setting: Task performance Canadian Journal of Aging 16 51–69 [PubMed] [Google Scholar]
- Scharlach A. E.,, Giunta N.,, Chow J. C.,, Lehning A. (2008). Racial and ethnic variations in caregiver service use. Journal of Aging and Health 20 326–346 [DOI] [PubMed] [Google Scholar]
- Schulz R.,, Beach S. R. (1999). Caregiving as a risk factor for mortality: The Caregiver Health Effects Study. Journal of the American Medical Association 282 2215–2219 [DOI] [PubMed] [Google Scholar]
- Schulz R.,, Mendelsohn A. B.,, Haley W. E.,, Specht J. P., Schutte D., Kelley L. S., Buckwalter K. C. (2003). End-of-life care and the effects of bereavement on family caregivers of persons with dementia. The New England Journal of Medicine 349 1936–1942 [DOI] [PubMed] [Google Scholar]
- Seddon D., Jones K., Boyle M. (2002). Committed to caring: Carer experiences after a relative goes into nursing or residential care Quality in Ageing 3 16–26 [Google Scholar]
- Stagno S. J.,, Zhukovsky D. S.,, Walsh D. (2000). Bioethics: Communication and decision-making in advanced disease. Seminars in Oncology 27 94–100 [PubMed] [Google Scholar]
- Teno J. M. (2003). Now is the time to embrace nursing homes as a place of care for dying persons. Journal of Palliative Medicine 6 293–296 [DOI] [PubMed] [Google Scholar]
- Tornatore J. B.,, Grant L. A. (2004). Family caregiver satisfaction with the nursing home after placement of a relative with dementia. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences 59 80–88 [DOI] [PubMed] [Google Scholar]
- Vohra J. U.,, Brazil K.,, Hanna S.,, Abelson J. (2004). Family Perceptions of End-of-Life Care in long-term care facilities. Journal of Palliative Care 20 297–302 [PubMed] [Google Scholar]
- Ware J. E., Sherbourne C. D. (1992). The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care 30 473–483 [PubMed] [Google Scholar]
- Wetle T.,, Shield R.,, Teno J.,, Miller S. C.,, Welch L. (2005). Family perspectives on end-of-life care experiences in nursing homes. The Gerontologist 45 642–650 [DOI] [PubMed] [Google Scholar]
- Whitaker A. (2009). Family involvement in the institutional eldercare context. Towards a new understanding Journal of Aging Studies 23 158–167 [Google Scholar]
- Whitlatch C. J.,, Schur D.,, Noelker L. S.,, Ejaz F. K.,, Looman W. J. (2001). The stress process of family caregiving in institutional settings. The Gerontologist 41 462–473 [DOI] [PubMed] [Google Scholar]
- Williams S. W.,, Williams C. S.,, Zimmerman S.,, Munn J.,, Dobbs D.,, Sloane P. D. (2008). Emotional and physical health of informal caregivers of residents at the end of life: The role of social support. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences 63 171–183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff J. L.,, Dy S. M.,, Frick K. D.,, Kasper J. D. (2007). End-of-life care: Findings from a national survey of informal caregivers. Archives of Internal Medicine 167 40–46 [DOI] [PubMed] [Google Scholar]
- Yamamoto-Mitani N.,, Aneshensel C. S.,, Levy-Storms L. (2002). Patterns of family visiting with institutionalized elders: The case of dementia. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences 57 234–246 [DOI] [PubMed] [Google Scholar]
- Zarit S. J. (2004). Family care and burden at the end of life Canadian Medical Association Journal 170 1811–1812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zerzan J.,, Stearns S.,, Hanson L. (2000). Access to palliative care and hospice in nursing homes. Journal of the American Medical Association 284 2489–2494 [DOI] [PubMed] [Google Scholar]
- Zimmerman S.,, Sloane P. D.,, Eckert J. K.,, Gruber-Baldini A. L., Morgan L. A., Hebel J. R., Chen C. K. (2005). How good is assisted living? Findings and implications from an outcomes study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences 60 195–204 [DOI] [PubMed] [Google Scholar]
- Zimmerman S.,, Sloane P. D.,, Hanson L.,, Mitchell C. M.,, Shy A. (2003). Staff perceptions of end-of-life care in long-term care. Journal of the American Medical Directors Association 4 23–26 [DOI] [PubMed] [Google Scholar]