Abstract
The long-term consequences of traumatic brain injury (TBI), specifically the detrimental effects of inflammation on the neurogenic niches, are not very well understood. In the present in vivo study, we examined the prolonged pathological outcomes of experimental TBI in different parts of the rat brain with special emphasis on inflammation and neurogenesis. Sixty days after moderate controlled cortical impact injury, adult Sprague-Dawley male rats were euthanized and brain tissues harvested. Antibodies against the activated microglial marker, OX6, the cell cycle-regulating protein marker, Ki67, and the immature neuronal marker, doublecortin, DCX, were used to estimate microglial activation, cell proliferation, and neuronal differentiation, respectively, in the subventricular zone (SVZ), subgranular zone (SGZ), striatum, thalamus, and cerebral peduncle. Stereology-based analyses revealed significant exacerbation of OX6-positive activated microglial cells in the striatum, thalamus, and cerebral peduncle. In parallel, significant decrements in Ki67-positive proliferating cells in SVZ and SGZ, but only trends of reduced DCX-positive immature neuronal cells in SVZ and SGZ were detected relative to sham control group. These results indicate a progressive deterioration of the TBI brain over time characterized by elevated inflammation and suppressed neurogenesis. Therapeutic intervention at the chronic stage of TBI may confer abrogation of these deleterious cell death processes.
Introduction
In the United States alone, an estimated 1.7 million people suffer from traumatic brain injury (TBI), and nearly 52,000 deaths a year, accounting for 30% of all injury-related deaths [1]. Annually, the cost of TBI related expenses is estimated to be around 52 billion dollars [2], [3]. Patients who survive head injuries often present with disabilities persisting up to decades after the injury [4]. Although the severity of disabilities varies, which may be directly associated with the severity of the injury itself [5], the most common disabilities include sensory-motor problems, learning and memory deficits, anxiety, and depression [5], [6]. Notably, TBI may predispose long-term survivors to age-related neurodegenerative diseases such as Alzheimer's disease, Parkinson’s disease, and post-traumatic dementia [5], [6], [7], [8], [9], [10].
Long-term neurological deficits from TBI are associated with neuroinflammation, and may aggravate over time to more severe secondary injuries, making prevention and treatment a very complex task [1], [11], [12], [13], [14]. Currently, a very well characterized TBI model for chronic brain atrophy, which addresses proximal and distal subcortical regions vulnerable to injury, is not available. An in-depth histological examination of the brain at the chronic stage of TBI should provide insights into identifying therapeutic targets amenable to treatment interventions even when initiated at this late phase of disease progression. Unfortunately to date, many studies concentrate on specific subcortical regions, while others focus only on white matter, making it difficult to translate the findings on pathological mechanisms and therapies generated in TBI animal models to clinical applications [15], [16], [17], [18]. A better understanding of the neuropathology propagation associated with TBI, through investigations of neuro-inflammatory mechanisms will allow us to efficiently manage and treat the evolution of TBI-secondary neuropathologies and cognitive disabilities after the acute phase [11], [19]. In the present in vivo study, the neuro-inflammatory responses in subcortical regions, such as the dorsal striatum, thalamus, and white matter as corpus callosum, hippocampal fimbria-fornix, and cerebral peduncle were characterized in chronic TBI. Additionally, neuronal cell loss, cell proliferation and neuronal differentiation were examined in neurogenic niches to assess the detrimental influence of progressive secondary injury in these vital regenerative areas of the brain. Our overarching theme advances the concept that a massive neuroinflammation after TBI represents a second wave of cell death that impairs the proliferative capacity of cells, and impedes the regenerative capacity of neurogenesis in chronic TBI. Accordingly, we embarked on this study to test the hypothesis that chronic TBI-induced neuroinflammation interfered endogenous repair mechanisms.
Materials and Methods
Subjects
Experimental procedures were approved by the University of South Florida Institutional Animal Care and Use Committee (IACUC). All animals were housed under normal conditions (20°C, 50% relative humidity, and a 12-h light/dark cycle) All studies were performed by personnel blinded to the treatment condition.
Surgical Procedures
Ten-week old Sprague–Dawley rats (n = 24) were subjected to either TBI using a controlled cortical impactor (CCI) (n = 12) or sham control (no TBI) (n = 12) (Pittsburgh Precision Instruments, Inc, Pittsburgh, PA). Deep anesthesia was achieved using 1–2% isoflurane, and it was maintained using a gas mask. All animals were fixed in a stereotaxic frame (David Kopf Instruments, Tujunga, CA, USA). After exposing the skull, coordinates of −0.2 mm anterior and +0.2 mm lateral to the midline were used and impacted the brain at the fronto-parietal cortex with a velocity of 6.0 m/s reaching a depth of 1.0 mm below the dura matter layer and remained in the brain for 150 milliseconds (ms). The impactor rod was angled 15° degrees vertically to maintain a perpendicular position in reference to the tangential plane of the brain curvature at the impact surface. A linear variable displacement transducer (Macrosensors, Pennsauken, NJ), which was connected to the impactor, measured the velocity and duration to verify consistency. Sham control injury surgeries consisted of animals exposed to anesthesia, scalp incision, craniectomy, and suturing. An electric drill was used to perform the craniectomy of about 2.5 mm radius with coordinates calculated from the bregma at −0.2 anterior and +0.2 mm lateral right. An automated thermal blanket pad and a rectal thermometer allowed maintenance of body temperature within normal limits. All animals were closely monitored post-operatively with weight and health surveillance recording as per IACUC guidelines. Rats were kept hydrated at all times, and the analgesic ketoprofen was administered after TBI surgery and as needed thereafter. Pre and post TBI, rats were fed regular rodent diet (Harlan 2018, Harlan).
Hematoxylin and Eosin Analysis
Hematoxylin and eosin (H&E) staining was performed to confirm the core impact injury of our TBI model. As shown in our previous studies [3], [5], we also demonstrated here that the primary damage produced by the CCI TBI model was to the fronto-parietal cortex. In addition, H&E staining was analyzed in the hippocampus to reveal secondary cell loss. Starting at coordinates AP-2.0 mm and ending at AP-3.8 mm from bregma, coronal brain sections (40 µm) covering the dorsal hippocampus were selected. A series of 6 sections per rat was processed for staining. Cells presenting with nuclear and cytoplasmic staining (H&E) were manually counted in the CA3 neurons. CA3 cell counting spanned the whole CA3 area, starting from the end of hilar neurons to the beginning of curvature of the CA2 region in both the ipsilateral and contralateral side. Sections were examined with Nikon Eclipse 600 microscope at 20X All data are represented as mean values ±SEM, with statistical significance set at p<0.05.
Immunohistochemistry
Under deep anesthesia, rats were sacrificed 8 weeks after TBI surgery, and perfused through the ascending aorta with 200 ml of ice cold phosphate buffer saline (PBS), followed by 200 ml of 4% paraformaldehyde (PFA) in PBS. Brains were removed and post-fixed in the same fixative for 24 hours followed by 30% sucrose in phosphate buffer (PB) for 1 week. Coronal sectioning was carried out at a thickness of 40 µm by cryostat. H&E staining was done on every sixth coronal section spanning the dorsal hippocampus. Staining for the cell cycle–regulating protein Ki67, DCX, and OX6 was done on every sixth coronal section throughout the entire striatum and dorsal hippocampus. Sixteen free-floating coronal sections (40 µm) were incubated in 0.3% hydrogen peroxide (H2O2) solution followed by 1-h of incubation in blocking solution (0.1 M phosphate-buffered saline (PBS) supplemented with 3% normal goat serum and 0.2% Triton X-100). Sections were then incubated overnight with Ki67 (1∶400 Nocastra), DCX (1∶150 Santa Cruz), and OX6 (major histocompatibility complex or MHC class II; 1∶750 BD) antibody markers in PBS supplemented with 3% normal goat serum and 0.1% Triton X-100. Sections were then washed and biotinylated secondary antibody (1∶200; Vector Laboratories, Burlingame, CA) in PBS supplemented with 3% normal goat serum, and 0.1% Triton X-100 was applied for 1 h. Next, the sections were incubated for 60 minutes in avidin–biotin substrate (ABC kit, Vector Laboratories, Burlingame, CA). All sections were then incubated for 1 minute in 3,30-diaminobenzidine (DAB) solution (Vector Laboratories). Sections were then mounted onto glass slides, dehydrated in ethanol and xylene, and cover-slipped using mounting medium.
Stereological Analysis
Unbiased stereology was performed on brain sections immunostained with OX6, Ki67 and DCX. Sets of 1/6 section, about 240 µm apart, were taken from the brain spanning AP –0.2 mm to AP –3.8 mm in all 24 rats. Activated microglia cells, cell proliferation, and differentiation into immature neurons were visualized by staining with OX6, Ki67, and DCX, respectively. Positive stains were analyzed with a Nikon Eclipse 600 microscope and quantified using Stereo Investigator software, version 10 (MicroBrightField, Colchester, VT). The estimated volume of OX6-positive cells was examined using the Cavalieri estimator probe of the unbiased stereological cell technique [20] revealing the volume of OX6 in the cortex, striatum, thalamus, fornix, cerebral peduncle, and corpus callosum. Ki67 [21] and DCX positive cells were counted within the subgranular zone (SGZ) and the subventricular zone (SVZ), in both hemispheres (ipsilateral and contralateral), using the optical fractionator probe of unbiased stereological cell counting technique. The sampling was optimized to count at least 300 cells per animal with error coefficients less than 0.07. Each counting frame (100×100 µm for OX6, Ki67, and DCX) was placed at an intersection of the lines forming a virtual grid (125×125 µm), which was randomly generated and placed by the software within the outlined structure. Section thickness was measured in all counting sites.
Statistical Analysis
For data analyses, contralateral and ipsilateral corresponding brain areas were used as raw data providing 2 sets of data per treatment condition (TBI vs. sham control), therefore one-way analysis of variance (ANOVA) was used for group comparisons, followed by subsequent pairwise comparisons; post hoc tests Bonferonni test. All data are represented as mean values with ±SEM. Statistical significance was set at p<0.05 for all analyses.
Results
In the preliminary analyses of the data, comparisons between sham control ipsilateral and sham control contralateral side, across all brain regions studied, did not significantly differ (p>0.05). Thus, the data from both sides of the sham group were combined. Pair-wise comparisons are summarized in the Tables S1, S2, S3, S4, S5, S6, S7, S8, S9, including neuroinflammation in different regions of the brain (cortex, Table S1; striatum, Table S2; thalamus, Table S3; corpus callosum, Table S4; cerebral peduncle, Table S5; fornix, Table S6), CA3 neuronal cell loss (Table S7), cell proliferation in SVZ (Table S8), and cell proliferation in SGZ (Table S9).
Upregulation of MHCll+ activated Microglia Cells in Chronic TBI
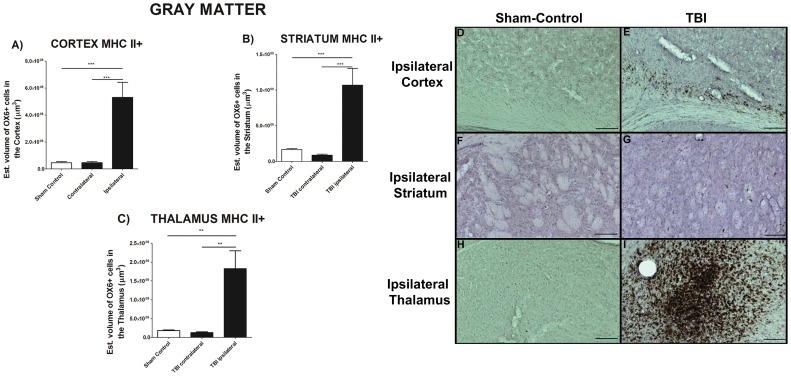
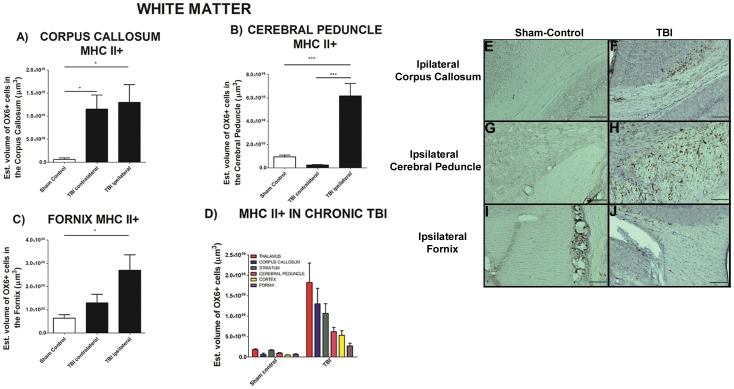
To test the hypothesis that the chronic stage of TBI was accompanied by upregulation of activated microglia cells (MHC ll+), gray and white matter areas were examined such as cortex, striatum, thalamus, olfactory bulb, dentate gyrus, corpus callosum, cerebral peduncle and fornix (Figure 1 and Figure 2). Of note, the dentate gyrus and olfactory bulbs displayed no detectable OX6-immunoreactive cells (see also Figure S1 and Figure S2). We calculated the volume of activated microglia cells (MHC ll +) in the ipsilateral and contralateral areas using an anti-OX6 antibody. Chronic TBI produced a robust upregulation in the volume of MHC II-labeled activated microglia cells in gray matter areas ipsilateral to TBI, whereas the volume in the contralateral side was not significantly different to that in sham control (Figure 1A, B, C). There was a 12-, 7- and a 10-fold increase in the volume of MHC Class ll in cortex (Figure 1A, D, E), striatum (Figure 1B, F,G), and thalamus (Figure 1C, H, I), respectively; cortex, F2, 45 = 18.49, p<0.005; striatum, F2, 45 = 15.71, p<0.005; thalamus, F2, 45 = 12.23, p<0.005. Similar analysis show that chronic TBI prompted an increase of activated MHC II-positive microglia cell volume in white matter areas ipsilateral and contralateral to TBI injury (Figure 2 and Figure S2). Chronic TBI resulted in an upregulation of activated microglia cells in corpus callosum, cerebral peduncle, and fornix around the injury side (Figure 2A, B, and C). There were no significant differences between ipsilateral and contralateral side of TBI animals, largely due to activation of microglia cells in corpus callosum in both hemispheres (p’s>0.05; Figure 2A). Additionally, significant increments in activated MHC II-positive microglia cells were detected in the ipsilateral cerebral peduncle (Figure 2A) and the ipsilateral hippocampal fornix (Figure 2C). ANOVA revealed significant treatment effects on MHC II-positive cells as follows: corpus callosum, F2, 45 = 5.656, p<0.05; cerebral peduncle, F2, 45 = 27.39, p<0.0005; fornix, F2, 45 = 5.541, p<0.05. A summary of all areas, comparing sham control and chronic TBI, is presented in Figure 2D. All data are represented as mean values ±SEM.
Figure 1. Upregulation of MHCll+ activated microglia cells in gray matter in chronic TBI.
Results indicate that there is a clear exacerbation of activated microglia cells in ipsilateral side of subcortical gray matter regions in chronic TBI relative to contralateral side and sham control. After 8 weeks from initial TBI injury, asterisks denote significant upregulation on the volume of MHC II expressing cells in A) cortex, B) striatum, C) thalamus. While contralateral side present an estimated volume of activated microglia cells similar to sham control animals. ANOVA revealed significant treatment effects as follows: cortex, F2,45 = 18.49; ***p<0.005; striatum, F2,45 = 15.71, ***p<0.005, and; thalamus, F2,45 = 12.23, ***p<0.005. Photomicrographs correspond to representative gray matter in coronal sections stained with OX6 (MHC ll) from ipsilateral sham control and TBI rats, cortex (Figure 1D, E), striatum (Figure 1F, G), thalamus (Figure 1H, I). Scale bars for D, E, F, G, H, I = 1 µm.
Figure 2. Upregulation of MHCll+ activated microglia cells in white matter in chronic TBI.
Results indicate that there is an upregulation of activated microglia cells after 8 weeks post TBI in proximal white matter areas. There is an upregulation of MHCll+ cells in the ipsilateral and contralateral side of corpus callosum relative to sham control (Figure 2A). In contrast, upregulation of MHCll+ activated microglia cells in the cerebral peduncle (Figure 2B) and fornix (Figure 2C) is only present in the ipsilateral side as compared with the contralateral and sham control. There were no significant differences between contralateral side and sham control animals in (Figure 2B) and (Figure 2C). ANOVA revealed significant treatment effects as follows: corpus callosum, F2,45 = 5.656; *p<0.05; cerebral peduncle, F2,45 = 27.39, ***p<0.0005, and; fornix, F2,45 = 5.541, *p<0.05. Representative photomicrographs, ipsilateral corpus callosum, sham-control Figure 2E and TBI Figure 2F, ipsilateral cerebral peduncle, sham-control Figure 2G and TBI Figure 2H, and ipsilateral Fornix, sham-control Figure 2I and TBI Figure 2J. Scale bars for Figure 2E, F, G, H, I, J = 1 µm. A summary of MHCll+ estimated volume is presented capturing different subcortical regions; including those proximal and distal from TBI insult (Figure 2D). Chronic TBI greatly upregulates the neuroinflammation in the thalamus expressing the highest upregulation of MHCll+ activated microglia cells, despite its distal subcortical location. Strong expression of MHCll+ activated microglia cells is also detected in the corpus callosum and striatum (Figure 2D).
Chronic TBI Impairs Hippocampal Cell Survival and Proliferation
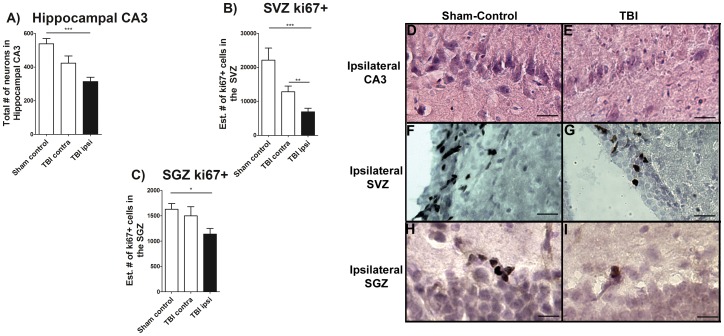
Next, in order to test the hypothesis that neuronal cell loss and impaired cell proliferation accompanied long term chronic TBI, the total number of surviving neurons in the hippocampal CA3 region, and the estimated number of positive dividing cells within SVZ and SGZ were examined. We found that long term chronic TBI significantly affected CA3 cell survival; F2,9 = 10.78, p<0.005, characterized by decreased neurons in the CA3 area of the ipsilateral hippocampus relative to sham control; p<0.05 (Figure 3A). There was no significant loss of neurons in the CA3 contralateral to chronic TBI animals compared to sham control (p>0.05; Figure 3A). Additionally, cell proliferation was examined by quantifying the cell proliferation marker Ki67 (Figure 3 and Figure S3). Chronic TBI significantly reduced cell proliferation in SVZ (F2, 45 = 10.45, p<0.0005) in both the ipsilateral and contralateral side compared with sham control (p’s<0.05; Figure 3B). Following this observation of chronic TBI-induced downregulation in the SVZ, we next inspected the cell proliferation in the SGZ, another neurogenic niche (Figure 3 and Figure S3). Again, chronic TBI was found to disturb cell proliferation in the SGZ (F2, 45 = 3.755, p<0.005). Quantification of cell proliferation within the SGZ demonstrated that there was a significant decrease in cell proliferation only in the ipsilateral side of chronic TBI compared with sham control (p<0.05). The contralateral SGZ did not show significant decrements in cell proliferation relative to sham control (p>0.05). The dentate gyrus (see Figure S3) and olfactory bulb (not shown) did not display overt cell loss.
Figure 3. Hippocampal CA3 cell loss and downregulation of cell proliferation.
H&E staining revealed a significant cell loss in the hippocampal CA3 region after chronic TBI (Figure 3A). Ki67, a cell proliferation marker, revealed a significant chronic TBI-related decrease in the SVZ of cell proliferation only in the ipsilateral side relative to contralateral side and sham control animals (Figure 3B). Contralateral measurements revealed that cell proliferation also decrease, but it does not show significant differences when compared with sham control animals (Figure 3B). Also, Ki67 revealed a significant decrease in cell proliferation in the SGZ of the hippocampus in the ipsilateral side compared to sham control (Figure 3C). In summary, ANOVA revealed significant treatment effects as follows: Hippocampal CA3 neurons, F2,9 = 10.78, ***p<0.005; SVZ, F2,45 = 10.45, ***p<0.005, and; SGZ, F2,45 = 3.755, ***p<0.005. Representative photomicrographs from coronal sections ipsilateral CA3 region stained with hematoxylin/eosin in sham control and TBI rats (Figure 3D, E). Ipsilateral SVZ from sham-control and TBI rats (Figure 3F, G) and ipsilateral SGZ from sham-control and TBI rats (Figure 3H, I) are shown. Scale bars for Figures 3D, E, F, G, H, I = 50 µm.
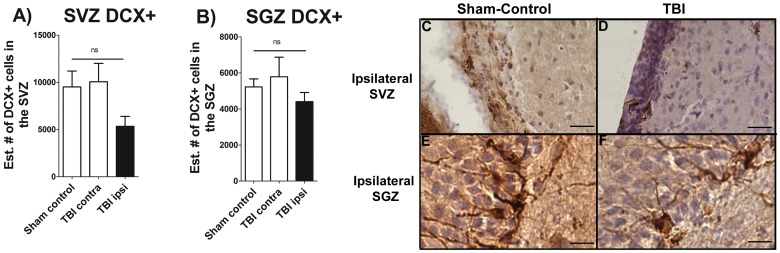
Chronic TBI does not Affect Neuronal Differentiation in Neurogenic Niches
Since chronic TBI induced extensive downregulation of cell proliferation in the two main neurogenic niches (SVZ and SGZ), neuronal differentiation was examined. Although there appeared a general downregulation of DCX-positive cells, the fraction of new cells generated in the SVZ and SGZ initiating down the neuronal path seems to be similar in the control compared to the TBI conditions (Figure 4A and B). Chronic TBI did not significantly impair cellular differentiation into neuronal lineage in the ipsilateral SVZ and SGZ when compared with the corresponding contralateral side or with sham control animals (p>0.05).
Figure 4. Neural differentiation is not affected by chronic TBI.
DCX staining, neural differentiation marker revealed that there is not significant impairment in neural differentiation in either SVZ of the lateral ventricle, or the SGZ of the hippocampus relative to contralateral side and sham control animals. The “ns” denotes non-significant differences (p>0.05). Representative coronal sections from ipsilateral SVZ stained with DCX in sham control and TBI rats (Figure 4C, D) and SGZ from sham-control and TBI rats (Figure 4E, F) are shown. Scale bars for Figure 4C, D, E, F = 50 µm.
Discussion
The present study demonstrated long-term neuroinflammation accompanied chronic TBI, which was closely associated with neuronal cell loss and impaired cell proliferation in discrete brain areas adjacent to and even in remote structures from the core injured region. At eight weeks post-TBI, a significant upregulation of activated microglia cells was detected not only in the directly TBI impacted cortical site, but also in proximal adjacent ipsilateral areas as well as in distal areas from injury. In tandem, a significant decrease of hippocampal neurons in the CA3 region ipsilateral to injury was detected relative to sham control. There was no cell loss found in the contralateral side after chronic TBI in the CA3 region. Examination of the neurogenic niches revealed significant declines in cell proliferation in both SVZ and SGZ ipsilateral to TBI. Of note, only the contralateral side of SVZ, but not the SGZ, seemed to be affected by chronic TBI showing a 40% decreased in cell proliferation compared with sham control. The present location of chronic inflammation seems to correlate with the observed cell loss and impaired cell proliferation. The SVZ and the dorsal hippocampus are located proximal to the area of CCI in the cortex. In addition, the proximity of the fornix and corpus callosum and thalamus to the hippocampus might have affected the CA3 cell survival and SGZ cell proliferation due to the chronic activated microglia cells present in these regions.
Neurodegeneration after the initial insult in TBI involves acute and chronic stages. Cell death processes in acute, but not chronic stages of TBI, as revealed by the CCI model, have been well characterized [5], [22], [23], [24]. Acute primary injury manifestations start to appear during the early stages of TBI, characterized by elevated intracerebral pressure, ruptured blood brain barrier, brain edema, and reduced cerebral blood flow at the area of injury [28], [29], [30]. In addition, at the molecular level, a massive innate immune response appears within minutes to ease elimination of cellular debris [24]. This wave of progressive injury contributes to long-term progressive damage post-TBI in animals and is seen also in patients even decades after the injury [6], [8], [9], [27]. After acute head trauma, increased cell proliferation and neural differentiation were detected within the neurogenic niches (SVZ and SGZ), likely corresponding to an endogenous regenerative mechanism to provide neuroprotection at the site of injury [3], [31], [32], [33], [34], [35], [36]. The recognition that the chronic stage of neuroinflammation alters endogenous reparative mechanism, i.e., proliferative properties of neurogenic niches especially the SVZ [38], requires the development of new strategies to mobilize these proliferative cells to specific injured brain areas for regenerative purposes [38]. Of note, only 10% of new cells in the SGZ survive for up to 4 weeks post injury in a close head injury mouse model of focal TBI, and 60% of new cells in the pericontusional cortex become astrocytes in response to brain injury [32], [33]. Additionally, a decreased survival of immature neurons can be seen as early as 7 days, in a mouse model of moderate TBI, and then at 4 weeks post-TBI both cell proliferation and neural differentiation greatly declined relative to sham control mice [37]. The observed preferential effect of TBI on cell proliferation, but not neuronal differentiation, may be due to a fraction of new cells undergoing neurogenesis not affected by TBI, even though overall proliferation rates are substantially reduced. In particular, this fraction of new cells generated in the SVZ and SGZ committed towards the neuronal lineage remains active in both control and TBI conditions. The type of insult (TBI, radiation, neurotoxin) may affect the brain microenvironment with varying levels of signaling cues for cell proliferation and differentiation, in turn resulting in an imbalance of new dividing cells and cells differentiating to a neuronal phenotype. This hypothesis clearly warrants further investigations.
Progressive injury to hippocampal, cortical, and thalamic areas contributes to long-term cognitive damage post-TBI as noted in military men and in civilian patients even decades after the injury [5], [6], [8], [9], [22], [24], [25], [26], [27], [30]. It is well recognized that hippocampal cell loss is a consequence of TBI [39], [40]. TBI patients have been shown to exhibit deficits in verbal declarative memory, which is modulated in part by the hippocampal formation, and executive functioning [41], [43]. Neuropsychological tests performed in US Army soldiers after deployment revealed that TBI is closely associated with functional impairments, while TBI co-morbid with PTSD and depression presents with chronic long lasting cognitive deficits [26]. In addition, cognitive functions modulated by the thalamic-cortical areas of the brain are also affected by chronic TBI as revealed by high resolution tensor magnetic resonance imaging [42]. Patients with a history of brain injury exhibit ventral thalamic atrophy, which correlates with impaired executive function, attention, and memory and learning deficits post-TBI [42]. Interestingly, cerebral blood flow to the thalamus is significantly reduced even by mild TBI and coincides with impairments in speech, learning and memory [43]. Taken together, impaired cognitive functions mediated by cortex, hippocampus, and thalamus may manifest in chronic TBI.
In the present study, cell proliferation was significantly affected by the cascade of events in chronic TBI, but while neuronal differentiation showed a trend of similar reduction, it did not reach statistical significance compared to sham control. These discrepant results may be due to the timing of histological analyses (acute vs. chronic), varying models of TBI (mild vs. moderate) and different animal species (mice vs. rat) [31], [32], [33], [37]. Despite the variability in experimental procedures and animal subjects, these studies, including ours, identify the susceptibility of newly formed cells within neurogenic niches, implicating the pivotal role of endogenous cells likely involved in the host reparative mechanism against TBI [37], [38].
Similar co-morbidity critical factors in the clinic, such as patient age, injury severity, and past medical history, influence the outcomes of TBI; however, neuroinflammation as a key cell death exacerbating factor appears consistent following brain injury [6], [8], [9], [10], [11], [16], [44], [45]. Upregulation of neuroinflammation in the present study was depicted by exacerbation of activated microglia cells in gray matter structures such as cortex, striatum, thalamus, and white matter including corpus callosum, fornix and cerebral peduncles. In the clinic, long-term microglia activation was visualized in vivo within the thalamus, putamen, occipital cortices, and white matter areas as the internal capsule, in patients exhibiting severe impairments in cognitive function up at least 11 months after moderate to severe TBI [44]. Consequently, microglial cells pose as a candidate target for abrogating cell death in an effort to develop novel anti-inflammation-based therapeutic modalities in TBI [4], [6], [7], [8], [9], [10].
The present findings of white matter changes, in chronic TBI, agree with previous reports demonstrating the negative influences of activated microglial cells after TBI [46], [47], [48]. White matter axonal injury is a very common feature in clinical setting after TBI, which accounts for impairments of cognitive function, and may result in high mortality rate [46], [47], [48]. Axonal degeneration, typical in white matter injury, interrupts the action potential throughout the cortex [46], [47], [49], and combined with overt activation of microglia cells in cortical and subcortical areas, may lead to impaired cell survival and cell proliferation in both immediate and remote areas of the impacted brain region [8], [9], [23], [50], [51]. In the present in vivo study, there were 70% and 34% decrements in cell proliferation in the SVZ and SGZ, respectively, in comparison to sham control. Our study suggests that cell proliferation is altered due to chronic neuroinflammation, but additional studies elucidating this cell death mechanism and its direct influence on impeding endogenous proliferation would be necessary to establish this point. Notwithstanding, these results advance the potential benefits of anti-inflammatory therapies during the chronic stage of TBI.
Taken together, these results indicate that while TBI is generally considered an acute injury, a chronic secondary cell death perturbation (i.e., neuroinflammation) and a diminished endogenous repair mechanism (i.e., cell proliferation) accompany the disease pathology over long-term. The recognition of long-term pathological disturbances associated with chronic inflammation and neuropsychological diseases suggests a vigilant follow-up monitoring of TBI patients in order to better manage the disease progression. A multi-pronged treatment targeting inflammatory and cell proliferative pathways may abrogate these chronic TBI pathological effects.
Supporting Information
Upregulation of MHCll+ activated microglia cells in gray matter in chronic TBI. Results indicate that there is a clear exacerbation of activated microglia cells in ipsilateral side of subcortical gray matter regions in chronic TBI relative to contralateral side and sham control. After 8 weeks from initial TBI injury, asterisks denote significant upregulation on the volume of MHC II expressing cells in cortex, striatum, and thalamus. While contralateral side present an estimated volume of activated microglia cells similar to sham control animals. Photomicrographs correspond to representative gray matter in coronal sections stained with OX6 (MHC ll) in sham control and TBI. Arrows denote activated microglia cells. Upregulation of MHCll+ activated microglia cells in white matter in chronic TBI. Results indicate that there is an upregulation of activated microglia cells after 8 weeks post TBI in proximal white matter areas. There is an upregulation of MHCll+ cells in the ipsilateral and contralateral side of corpus callosum relative to sham control. In contrast, upregulation of MHCll+ activated microglia cells in the cerebral peduncle and fornix is only present in the ipsilateral side as compared with the contralateral and sham control. There were no significant differences between contralateral side and sham control animals. Photomicrographs correspond to representative coronal sections stained with OX6 in sham control and TBI. Arrows denote activated microglia cells. Chronic TBI greatly upregulates the neuroinflammation in the thalamus expressing the highest upregulation of MHCll+ activated microglia cells, despite its distal subcortical location. Strong expression of MHCll+ activated microglia cells is also detected in the corpus callosum and striatum.
(TIF)
Hippocampal CA3 cell loss and downregulation of cell proliferation. H&E staining revealed a significant cell loss in the hippocampal CA3 region after chronic TBI (A). Ki67, (cell proliferation marker) revealed a significant chronic TBI-related decrease in the SVZ of cell proliferation only in the ipsilateral side relative to contralateral side and sham control animals. Contralateral measurements revealed that cell proliferation also decrease, but it does not show significant differences when compared with sham control animals. Also, Ki67 revealed a significant decrease in cell proliferation in the SGZ of the hippocampus in the ipsilateral side in compared to both contralateral side and sham control. Representative coronal sections stained with H&E in sham control and TBI are shown. Arrows denote neuronal cell loss in hippocampal CA3 area. In addition, representative images of SVZ and SGZ areas stained with Ki67 in sham control and TBI are shown. Arrows denote proliferating cells in SVZ and SGZ.
(TIF)
Neuronal differentiation is not affected by chronic TBI. DCX staining, neuronal differentiation marker revealed that there is not significant impairment in neuronal differentiation in either SVZ of the lateral ventricle, or the SGZ of the hippocampus relative to contralateral side and sham control animals. Representative coronal sections stained with DCX in sham control and TBI are shown. Arrows denote DCX positive cells in SVZ and in the SGZ.
(TIF)
MHC Class ll Cortex.
(DOCX)
MHC Class ll Striatum.
(DOCX)
MHC Class ll Thalamus.
(DOCX)
MHC Class ll Corpus Callosum.
(DOCX)
MHC Class ll Cerebral Peduncle.
(DOCX)
MHC Class ll Fornix.
(DOCX)
CA3 Neuronal Cell Loss.
(DOCX)
Cell Proliferation SVZ.
(DOCX)
Cell Proliferation SGZ.
(DOCX)
Funding Statement
Financial support for this study was through the Department of Defense W81XWH-11-1-0634, the University of South Florida Signature Interdisciplinary Program in Neuroscience funds, the University of South Florida and Veterans Administration Reintegration Funds, and the University of South Florida Neuroscience Collaborative Program. CVB is funded by the National Institutes of Health 1R01NS071956-01A1, James and Esther King Biomedical Research Foundation 1KG01-33966, SanBio Inc., KMPHC and NeuralStem Inc. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Faul M, Xu L, Wald MM, Coronado VG (2010) Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations and Deaths 2002–2006. Atlanta (GA): Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. [Google Scholar]
- 2.Mammis A, McIntosh TK, Maniker AH (2009) Erythropoietin as a neuroprotective agent in traumatic brain injury Review. Surg Neurol 71: 527–531; discussion 531. [DOI] [PubMed] [Google Scholar]
- 3. Glover LE, Tajiri N, Lau T, Kaneko Y, van Loveren H, et al. (2012) Immediate, but not delayed, microsurgical skull reconstruction exacerbates brain damage in experimental traumatic brain injury model. PLoS One 7: e33646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Liu CY (2008) Combined therapies: National Institute of Neurological Disorders and Stroke funding opportunity in traumatic brain injury research. Neurosurgery 63: N12. [DOI] [PubMed] [Google Scholar]
- 5. Yu S, Kaneko Y, Bae E, Stahl CE, Wang Y, et al. (2009) Severity of controlled cortical impact traumatic brain injury in rats and mice dictates degree of behavioral deficits. Brain Res 1287: 157–163. [DOI] [PubMed] [Google Scholar]
- 6. Starkstein SE, Jorge R (2005) Dementia after traumatic brain injury. Int Psychogeriatr 17 Suppl 1S93–107. [DOI] [PubMed] [Google Scholar]
- 7. Johnson VE, Stewart W, Smith DH (2012) Widespread tau and amyloid-beta pathology many years after a single traumatic brain injury in humans. Brain Pathol 22: 142–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ho L, Zhao W, Dams-O'Connor K, Tang CY, Gordon W, et al. (2012) Elevated plasma MCP-1 concentration following traumatic brain injury as a potential “predisposition” factor associated with an increased risk for subsequent development of Alzheimer's disease. J Alzheimers Dis 31: 301–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Goldman SM, Tanner CM, Oakes D, Bhudhikanok GS, Gupta A, et al. (2006) Head injury and Parkinson's disease risk in twins. Ann Neurol 60: 65–72. [DOI] [PubMed] [Google Scholar]
- 10. Mannix RC, Whalen MJ (2012) Traumatic brain injury, microglia, and Beta amyloid. Int J Alzheimers Dis 2012: 608732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rovegno M, Soto PA, Saez JC, von Bernhardi R (2012) Biological mechanisms involved in the spread of traumatic brain damage. Med Intensiva 36: 37–44. [DOI] [PubMed] [Google Scholar]
- 12. Potts MB, Adwanikar H, Noble-Haeusslein LJ (2009) Models of traumatic cerebellar injury. Cerebellum 8: 211–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wagner AK, Kline AE, Ren D, Willard LA, Wenger MK, et al. (2007) Gender associations with chronic methylphenidate treatment and behavioral performance following experimental traumatic brain injury. Behav Brain Res 181: 200–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Holschneider DP, Guo Y, Roch M, Norman KM, Scremin OU (2011) Acetylcholinesterase inhibition and locomotor function after motor-sensory cortex impact injury. J Neurotrauma 28: 1909–1919. [DOI] [PubMed] [Google Scholar]
- 15. Dietrich WD, Truettner J, Zhao W, Alonso OF, Busto R, et al. (1999) Sequential changes in glial fibrillary acidic protein and gene expression following parasagittal fluid-percussion brain injury in rats. J Neurotrauma 16: 567–581. [DOI] [PubMed] [Google Scholar]
- 16. Kelley BJ, Lifshitz J, Povlishock JT (2007) Neuroinflammatory responses after experimental diffuse traumatic brain injury. J Neuropathol Exp Neurol 66: 989–1001. [DOI] [PubMed] [Google Scholar]
- 17. Onyszchuk G, LeVine SM, Brooks WM, Berman NE (2009) Post-acute pathological changes in the thalamus and internal capsule in aged mice following controlled cortical impact injury: a magnetic resonance imaging, iron histochemical, and glial immunohistochemical study. Neurosci Lett 452: 204–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rodriguez-Paez AC, Brunschwig JP, Bramlett HM (2005) Light and electron microscopic assessment of progressive atrophy following moderate traumatic brain injury in the rat. Acta Neuropathol 109: 603–616. [DOI] [PubMed] [Google Scholar]
- 19. Shitaka Y, Tran HT, Bennett RE, Sanchez L, Levy MA, et al. (2011) Repetitive closed-skull traumatic brain injury in mice causes persistent multifocal axonal injury and microglial reactivity. J Neuropathol Exp Neurol 70: 551–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mayhew TM (1991) The new stereological methods for interpreting functional morphology from slices of cells and organs. Exp Physiol 76: 639–665. [DOI] [PubMed] [Google Scholar]
- 21. Scholzen T, Gerdes J (2000) The Ki-67 protein: from the known and the unknown. J Cell Physiol 182: 311–322. [DOI] [PubMed] [Google Scholar]
- 22. Gao X, Deng P, Xu ZC, Chen J (2011) Moderate traumatic brain injury causes acute dendritic and synaptic degeneration in the hippocampal dentate gyrus. PLoS One 6: e24566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Yang J, You Z, Kim HH, Hwang SK, Khuman J, et al. (2010) Genetic analysis of the role of tumor necrosis factor receptors in functional outcome after traumatic brain injury in mice. J Neurotrauma 27: 1037–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Harting MT, Jimenez F, Adams SD, Mercer DW, Cox CS Jr (2008) Acute, regional inflammatory response after traumatic brain injury: Implications for cellular therapy. Surgery 144: 803–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Elder GA, Dorr NP, De Gasperi R, Gama Sosa MA, Shaughness MC, et al. (2012) Blast exposure induces post-traumatic stress disorder-related traits in a rat model of mild traumatic brain injury. J Neurotrauma 29: 2564–2575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Vasterling JJ, Brailey K, Proctor SP, Kane R, Heeren T, et al. (2012) Neuropsychological outcomes of mild traumatic brain injury, post-traumatic stress disorder and depression in Iraq-deployed US Army soldiers. Br J Psychiatry 201: 186–192. [DOI] [PubMed] [Google Scholar]
- 27. Rogers JM, Read CA (2007) Psychiatric comorbidity following traumatic brain injury. Brain Inj 21: 1321–1333. [DOI] [PubMed] [Google Scholar]
- 28. Cernak I, Stoica B, Byrnes KR, Di Giovanni S, Faden AI (2005) Role of the cell cycle in the pathobiology of central nervous system trauma. Cell Cycle 4: 1286–1293. [DOI] [PubMed] [Google Scholar]
- 29. Cernak I (2005) Animal models of head trauma. NeuroRx 2: 410–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Schmidt OI, Heyde CE, Ertel W, Stahel PF (2005) Closed head injury–an inflammatory disease? Brain Res Brain Res Rev 48: 388–399. [DOI] [PubMed] [Google Scholar]
- 31. Parent JM (2003) Injury-induced neurogenesis in the adult mammalian brain. Neuroscientist 9: 261–272. [DOI] [PubMed] [Google Scholar]
- 32. Bye N, Ng SY, Morganti-Kossmann MC (2010) Characterizing endogenous neurogenesis following experimental focal traumatic brain injury (TBI), and investigating the effect of treatment with minocycline. Injury 41 Suppl 1S42. [Google Scholar]
- 33. Bye N, Carron S, Han X, Agyapomaa D, Ng SY, et al. (2011) Neurogenesis and glial proliferation are stimulated following diffuse traumatic brain injury in adult rats. J Neurosci Res 89: 986–1000. [DOI] [PubMed] [Google Scholar]
- 34.Richardson RM, Sun D, Bullock MR (2007) Neurogenesis after traumatic brain injury. Neurosurg Clin N Am 18: 169–181, xi. [DOI] [PubMed] [Google Scholar]
- 35. Shojo H, Kaneko Y, Mabuchi T, Kibayashi K, Adachi N, et al. (2010) Genetic and histologic evidence implicates role of inflammation in traumatic brain injury-induced apoptosis in the rat cerebral cortex following moderate fluid percussion injury. Neuroscience 171: 1273–1282. [DOI] [PubMed] [Google Scholar]
- 36. Hayashi T, Kaneko Y, Yu S, Bae E, Stahl CE, et al. (2009) Quantitative analyses of matrix metalloproteinase activity after traumatic brain injury in adult rats. Brain Res 1280: 172–177. [DOI] [PubMed] [Google Scholar]
- 37. Rola R, Mizumatsu S, Otsuka S, Morhardt DR, Noble-Haeusslein LJ, et al. (2006) Alterations in hippocampal neurogenesis following traumatic brain injury in mice. Exp Neurol 202: 189–199. [DOI] [PubMed] [Google Scholar]
- 38. Pluchino S, Muzio L, Imitola J, Deleidi M, Alfaro-Cervello C, et al. (2008) Persistent inflammation alters the function of the endogenous brain stem cell compartment. Brain 131: 2564–2578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hicks RR, Smith DH, Lowenstein DH, Saint Marie R, McIntosh TK (1993) Mild experimental brain injury in the rat induces cognitive deficits associated with regional neuronal loss in the hippocampus. J Neurotrauma 10: 405–414. [DOI] [PubMed] [Google Scholar]
- 40. Ariza M, Serra-Grabulosa JM, Junque C, Ramirez B, Mataro M, et al. (2006) Hippocampal head atrophy after traumatic brain injury. Neuropsychologia 44: 1956–1961. [DOI] [PubMed] [Google Scholar]
- 41. Mathias JL, Mansfield KM (2005) Prospective and declarative memory problems following moderate and severe traumatic brain injury. Brain Inj 19: 271–282. [DOI] [PubMed] [Google Scholar]
- 42. Little DM, Kraus MF, Joseph J, Geary EK, Susmaras T, et al. (2010) Thalamic integrity underlies executive dysfunction in traumatic brain injury. Neurology 74: 558–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Ge Y, Patel MB, Chen Q, Grossman EJ, Zhang K, et al. (2009) Assessment of thalamic perfusion in patients with mild traumatic brain injury by true FISP arterial spin labelling MR imaging at 3T. Brain Inj 23: 666–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Ramlackhansingh AF, Brooks DJ, Greenwood RJ, Bose SK, Turkheimer FE, et al. (2011) Inflammation after trauma: microglial activation and traumatic brain injury. Ann Neurol 70: 374–383. [DOI] [PubMed] [Google Scholar]
- 45. Laskowitz DT, Song P, Wang H, Mace B, Sullivan PM, et al. (2010) Traumatic brain injury exacerbates neurodegenerative pathology: improvement with an apolipoprotein E-based therapeutic. J Neurotrauma 27: 1983–1995. [DOI] [PubMed] [Google Scholar]
- 46. Gunning-Dixon FM, Raz N (2000) The cognitive correlates of white matter abnormalities in normal aging: a quantitative review. Neuropsychology 14: 224–232. [DOI] [PubMed] [Google Scholar]
- 47. Filley CM (1998) The behavioral neurology of cerebral white matter. Neurology 50: 1535–1540. [DOI] [PubMed] [Google Scholar]
- 48.Jia X, Cong B, Wang S, Dong L, Ma C, et al.. (2012) Secondary damage caused by CD11b+ microglia following diffuse axonal injury in rats. J Trauma Acute Care Surg. [DOI] [PubMed] [Google Scholar]
- 49. Roher AE, Weiss N, Kokjohn TA, Kuo YM, Kalback W, et al. (2002) Increased A beta peptides and reduced cholesterol and myelin proteins characterize white matter degeneration in Alzheimer's disease. Biochemistry 41: 11080–11090. [DOI] [PubMed] [Google Scholar]
- 50. Iijima T, Shimase C, Sawa H, Sankawa H (1998) Spreading depression induces depletion of MAP2 in area CA3 of the hippocampus in a rat unilateral carotid artery occlusion model. J Neurotrauma 15: 277–284. [DOI] [PubMed] [Google Scholar]
- 51. Grady MS, Charleston JS, Maris D, Witgen BM, Lifshitz J (2003) Neuronal and glial cell number in the hippocampus after experimental traumatic brain injury: analysis by stereological estimation. J Neurotrauma 20: 929–941. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Upregulation of MHCll+ activated microglia cells in gray matter in chronic TBI. Results indicate that there is a clear exacerbation of activated microglia cells in ipsilateral side of subcortical gray matter regions in chronic TBI relative to contralateral side and sham control. After 8 weeks from initial TBI injury, asterisks denote significant upregulation on the volume of MHC II expressing cells in cortex, striatum, and thalamus. While contralateral side present an estimated volume of activated microglia cells similar to sham control animals. Photomicrographs correspond to representative gray matter in coronal sections stained with OX6 (MHC ll) in sham control and TBI. Arrows denote activated microglia cells. Upregulation of MHCll+ activated microglia cells in white matter in chronic TBI. Results indicate that there is an upregulation of activated microglia cells after 8 weeks post TBI in proximal white matter areas. There is an upregulation of MHCll+ cells in the ipsilateral and contralateral side of corpus callosum relative to sham control. In contrast, upregulation of MHCll+ activated microglia cells in the cerebral peduncle and fornix is only present in the ipsilateral side as compared with the contralateral and sham control. There were no significant differences between contralateral side and sham control animals. Photomicrographs correspond to representative coronal sections stained with OX6 in sham control and TBI. Arrows denote activated microglia cells. Chronic TBI greatly upregulates the neuroinflammation in the thalamus expressing the highest upregulation of MHCll+ activated microglia cells, despite its distal subcortical location. Strong expression of MHCll+ activated microglia cells is also detected in the corpus callosum and striatum.
(TIF)
Hippocampal CA3 cell loss and downregulation of cell proliferation. H&E staining revealed a significant cell loss in the hippocampal CA3 region after chronic TBI (A). Ki67, (cell proliferation marker) revealed a significant chronic TBI-related decrease in the SVZ of cell proliferation only in the ipsilateral side relative to contralateral side and sham control animals. Contralateral measurements revealed that cell proliferation also decrease, but it does not show significant differences when compared with sham control animals. Also, Ki67 revealed a significant decrease in cell proliferation in the SGZ of the hippocampus in the ipsilateral side in compared to both contralateral side and sham control. Representative coronal sections stained with H&E in sham control and TBI are shown. Arrows denote neuronal cell loss in hippocampal CA3 area. In addition, representative images of SVZ and SGZ areas stained with Ki67 in sham control and TBI are shown. Arrows denote proliferating cells in SVZ and SGZ.
(TIF)
Neuronal differentiation is not affected by chronic TBI. DCX staining, neuronal differentiation marker revealed that there is not significant impairment in neuronal differentiation in either SVZ of the lateral ventricle, or the SGZ of the hippocampus relative to contralateral side and sham control animals. Representative coronal sections stained with DCX in sham control and TBI are shown. Arrows denote DCX positive cells in SVZ and in the SGZ.
(TIF)
MHC Class ll Cortex.
(DOCX)
MHC Class ll Striatum.
(DOCX)
MHC Class ll Thalamus.
(DOCX)
MHC Class ll Corpus Callosum.
(DOCX)
MHC Class ll Cerebral Peduncle.
(DOCX)
MHC Class ll Fornix.
(DOCX)
CA3 Neuronal Cell Loss.
(DOCX)
Cell Proliferation SVZ.
(DOCX)
Cell Proliferation SGZ.
(DOCX)