Abstract
Background
The workplace is used as a setting for interventions to prevent and reduce sickness absence, regardless of the specific medical conditions and diagnoses.
Aims
To give an overview of the general effectiveness of active workplace interventions aimed at preventing and reducing sickness absence.
Methods
We systematically searched PubMed, Embase, Psych-info, and ISI web of knowledge on 27 December 2011. Inclusion criteria were (i) participants over 18 years old with an active role in the intervention, (ii) intervention done partly or fully at the workplace or at the initiative of the workplace and (iii) sickness absence reported. Two reviewers independently screened articles, extracted data and assessed risk of bias. A narrative synthesis was used.
Results
We identified 2036 articles of which, 93 were assessed in full text. Seventeen articles were included (2 with low and 15 with medium risk of bias), with a total of 24 comparisons. Five interventions from four articles significantly reduced sickness absence. We found moderate evidence that graded activity reduced sickness absence and limited evidence that the Sheerbrooke model (a comprehensive multidisciplinary intervention) and cognitive behavioural therapy (CBT) reduced sickness absence. There was moderate evidence that workplace education and physical exercise did not reduce sickness absence. For other interventions, the evidence was insufficient to draw conclusions.
Conclusions
The review found limited evidence that active workplace interventions were not generally effective in reducing sickness absence, but there was moderate evidence of effect for graded activity and limited evidence for the effectiveness of the Sheerbrooke model and CBT.
Key words: Cognitive workplace interventions, composite interventions, systematic review, workplace exercise, workplace physical activity
Introduction
The cost of sickness absence and disability benefits represents a major challenge for many workplaces and for society as a whole. Work is beneficial for both physical and mental health and is important for identity and social status [1]. Sickness absence is a risk factor for permanently leaving the workforce[2], and receiving a disability pension is a risk factor for early mortality [3]. There may be much to gain from interventions aimed at preventing long-term sickness absence.
A large number of systematic reviews summarize the effectiveness of different workplace interventions [4,5], but this literature is mostly subdivided into diagnostic categories with health as the primary outcome. Musculoskeletal and mental-health problems are the most common main diagnoses associated with sickness absence [6]. However, patients with long-term sickness absence are characterized by comorbid or multimorbid conditions and multiple body distress symptoms [7–9]; e.g. between 30–100% of low back pain (LBP) patients have comorbid psychiatric symptoms [10]. The ‘main diagnosis’ represents only part of the total picture. A systematic review across various diagnostic groups is therefore a useful addition to the existing literature.
In this review, the term ‘active treatments’ refers to interventions requiring that the subject is active and where the goal is behavioural change. This definition excludes interventions such as surgery, massage, use of medication etc. Active interventions like cognitive behavioural therapy (CBT) [11] and instructions to stay active in the treatment of musculoskeletal pain have to a large degree replaced passive treatments as the preferred approach [12]. While passive treatments aim to change the physical condition of the treatment recipient, active interventions target behavioural change or negative cognitions.
The aim of this study was to review randomized controlled trials (RCTs) of active interventions implemented in the workplace or through the initiative of the employer, both to prevent and reduce sickness absence for employees over 18 years of age.
Methods
PubMed, Embase, Psych-Info, ISI Web of Science and the Cochrane Central Register Databases were searched by two of the authors (M.O and L.H.M) in March 2010. The search string had two parts, one for identifying RCTs and the other for identifying sickness absence. A combination of keywords, subject headings and free text terms were used in all searches, and each search was adapted to the database used (see Appendix 1, available as Supplementary data at Occupational Medicine Online, for search strategy). A research librarian assisted with the search. A supplemental search was performed on 27 December 2011 to include all articles published to this date. We searched the reference lists of two Cochrane reviews with similar inclusion criteria and outcome measures [4,13] for additional articles. Finally, www.clinicaltrials.gov was searched in March 2011 to identify ongoing trials.
Articles reporting RCTs of active interventions published in English in peer-reviewed journals were included. A scoping search indicated that English articles were sufficient to cover the relevant literature. The trial participants were employees above 18 years of age. At least some part of the intervention had to have taken place at the workplace or at the initiative of the employer. Furthermore, the intervention had to be aimed at one or several specific workplaces. Interventions recruiting participants from clinical settings or economic claim databases were excluded unless recruitment was done at a predefined set of workplaces.
Quantified sickness absence and/or return to work (RTW) were the only outcome measures. Qualitative reports and estimates of future sickness absence were not included; neither were non-quantified reports, e.g. ‘yes or no’ to sickness absence. Unadjusted values for the sickness absence outcome had to be reported separately for intervention and control groups. Finally, studies with a high overall risk of bias were excluded.
Two pairs of reviewers (M.O and L.H.M; T.H.T and S.M) independently screened the titles and abstracts of the identified articles. Articles considered eligible for full text screening were retrieved. Four articles could not be retrieved even after emailing the corresponding authors [14–17] and were not included in the review. The retrieved articles were screened in full text, and disagreements were resolved by discussion among all the reviewers.
Data from each of the included articles were independently extracted by two reviewers, using a digital data extraction form in EPPI reviewer software [18]. Disagreements were resolved by discussion until consensus was reached. Data were extracted about the participants, the intervention(s), the workplace, health complaints, and whether there was a significant effect on sickness absence or not.
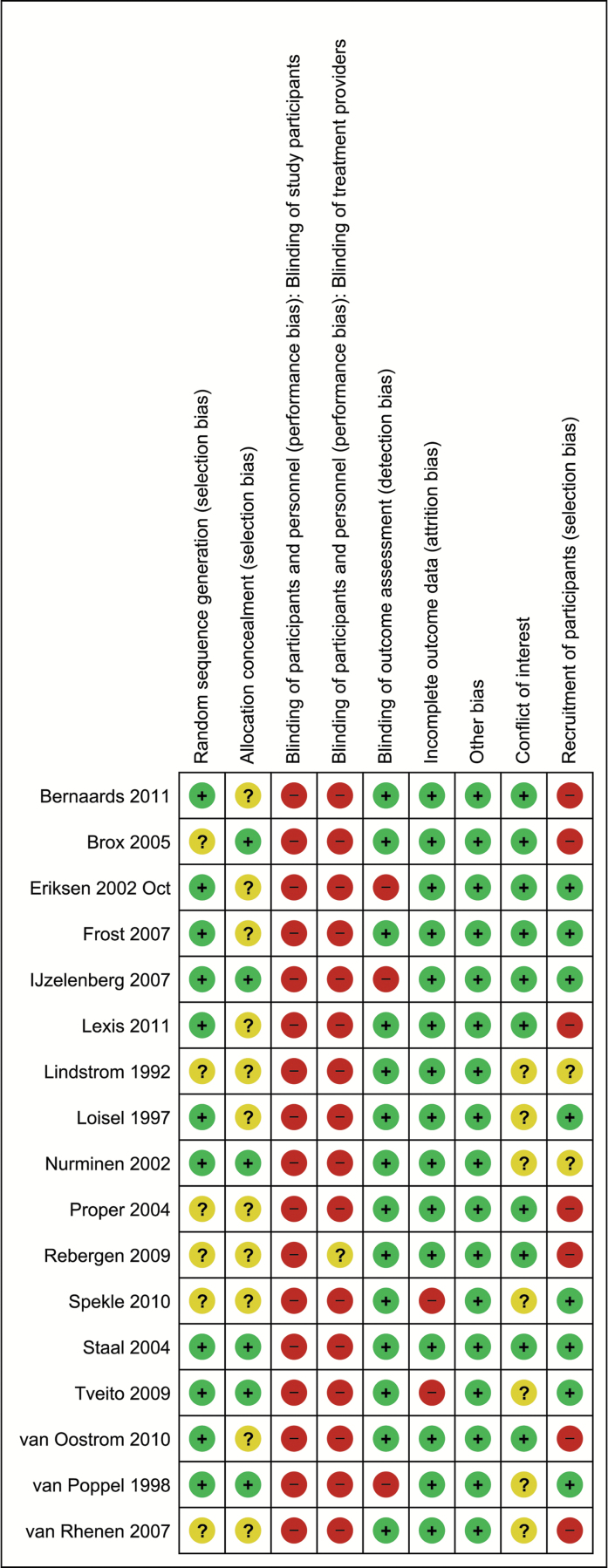
The Cochrane collaborations tool for risk of bias [19] was used to assess risk of bias. Assessments were based on the published information only. We included two additional items: (i) financial interests of authors that might be related to the study results and (ii) selection bias caused by systematic differences between participants in a study and those who refused participation. Samples where less than two-thirds of the invited populations agreed to participate were considered biased.
Active interventions require collaboration from the participants implying that they know which intervention they get. It is also impossible to blind the treatment providers. As all studies included in this review had a high risk of bias on blinding, we disregarded these criteria, except for outcome assessment. For this criterion, we considered register data as blinded and self-report data as un-blinded.
The studies were classified as high, low or medium overall risk of bias. The criteria were
Low: Studies with low risk of bias in randomization and allocation, no high risks of bias, and not more than two unknown risks of bias.
High (excluded): Two or more high risks of bias, or a total of five high or unknown risks of bias.
The remaining articles were classified as medium risk of bias.
A narrative data analysis considering study size, effect size and risk of bias was done. The interventions were classified into four broad categories: cognitive, educational, composite, and physical activity. The comparisons between interventions and control were the unit of analysis. Thus, if a study tested three different interventions against a control group, it would be counted as three comparisons.
The Cochrane Collaboration Back Review Group’s 2003 criteria for deciding quality of evidence [20] was used to determine the overall quality of evidence for each intervention type in the synthesis. Strong quality evidence required consistent findings among multiple high quality RCTs, moderate required consistent findings from multiple low quality RCTs and/or one high quality RCT, and limited evidence required consistent findings, with evidence from at least one low quality RCT [20].
In addition to the main synthesis, we checked for systematic differences in sickness absence and risk of bias between high- and low-quality studies and between studies with register and self-report data.
The protocol of the review was not published and trial registration was not done, as no suitable register was found during the start of the review. The protocol can be obtained by contacting the authors. No ethical approval was required as the study was a systematic review based on published data.
Results
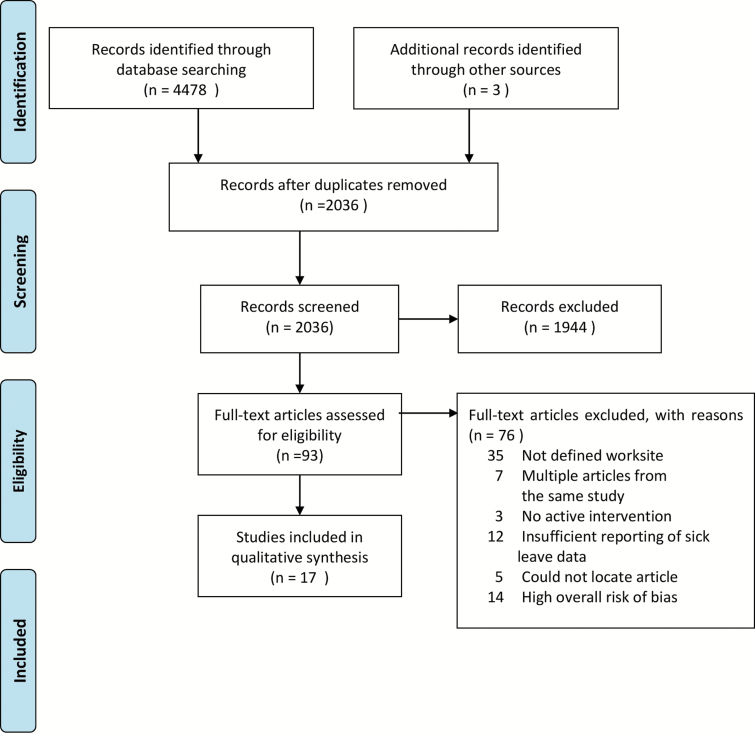
Ninety-three articles were retrieved in full text, and 17 of them fulfilled the inclusion criteria (see Figure 1). Eight of the included articles targeted musculoskeletal, three mental, and six multiple health complaints or general health. Seventy-six articles were excluded, mainly because they did not fulfil the workplace, sickness absence reporting, or active intervention criteria (see Appendix 1, available as Supplementary data at Occupational Medicine Online). Thirteen articles were excluded because of a high overall risk of bias (see Appendix 2, available as Supplementary data at Occupational Medicine Online).
Figure 1.
Flow diagram of article selection.
Two of the 17 studies had a low risk of bias; the rest had a medium risk of bias (see Figure 2). Fourteen studies used register data, and four of these reported a significant sickness absence reduction. Three studies used self-report data, none with significant results. The studies with no effect had a mean number of participants of 691, while the studies with effect had a mean number of participants of 120. Median values were 312 and 119, respectively. The control interventions were no treatment, treatment as usual or some minimal intervention such as a booklet. The studies are described in Table 1.
Figure 2.
Risk of bias in included studies.
Table 1.
Characteristics of included studies, subdivided by intervention types
| Author, year, country, reference | Study sample (N) | Intervention(s) | Comparator | Significant sickness absence reduction | Diagnostic group | Risk of bias |
|---|---|---|---|---|---|---|
| Cognitive interventions | ||||||
| Eriksen et al. 2002, Norway [26] | Blue collar postal workers (860) | Stress management training | No intervention | No | General sickness absence prevention | Medium |
| Lexis et al. 2011, Netherlands [21] | Bank employees (139) | CBT with problem solving therapy | No intervention | Yes | Depression | Medium |
| Proper et al. 2004, Netherlands [27] | White collar workers (299) | Counselling on physical activity and life style | Booklet | No | General sickness absence prevention | Medium |
| Rebergen et al. 2009 Netherlands [30] | Police officers (240) | Guideline based cognitive treatment | No intervention | No | Mental health | Medium |
| van Oostrom et al. 2010, Netherlands [28] | Mixed group workers (145) | Participatory problem solving training | No intervention | No | Mental health (distress) | Medium |
| van Rehnen et al. 2007, Netherlands [29] | Telecom workers (792)a | Brief cognitive intervention | No intervention | No | Mental health (stress) | Medium |
| Educational interventions | ||||||
| Bernaards et al. 2011, Netherlands [33] | Computer workers (446) | Education about physical activity and work style | No intervention | No | Musculoskeletal | Medium |
| Frost et al. 2007, Denmark [31] | Industrial and health care workers (3808) | Information booklet | Information given to the organization | No | Musculoskeletal | Medium |
| Speklé et al. 2010, Netherlands [32] | Computer workers (1183) | Education and ergonomic advice | Limited general advice, referral if required (usual care) | No | Musculoskeletal | Medium |
| van Poppel et al. 1998, Netherlands [34] | Manual labourers at airport (312) | Education in lifting techniques | No intervention | No | Musculoskeletal | Medium |
| van Poppel et al. 1998, Netherlands [34] | Manual labourers at airport (312) | Education in lifting techniques and lumbar support belt | No intervention | No | Musculoskeletal | Medium |
| Composite interventions | ||||||
| Frost et al. 2007, Denmark [31] | Industrial and health care workers (3808) | Information booklet and ergonomic screening | Information given to the organization | No | Musculoskeletal | Medium |
| IJzelenberg et al. 2007, Netherlands [25] | Workers in physically demanding jobs (489) | Education, exercise, and ergonomic advice | No intervention | No | Musculoskeletal | Medium |
| Loisel et al. 1997, Canada [23] | Manufacturing, health care, and services (104) | Back school and multidisciplinary treatment if necessary | Video on back pain, no further intervention | No | Musculoskeletal | Medium |
| Loisel et al. 1997, Canada [23] | Manufacturing, health care, and services (104) | Back school, ergonomic screening, ‘therapeutic RTW’ | Video on back pain, no further intervention | Yes | Musculoskeletal | Medium |
| Loisel et al. 1997, Canada [23] | Manufacturing, health care, and services (104) | Back school, multidisciplinary, ergonomic screening, ‘therapeutic RTW’ (Sheerbrooke model) | Video on back pain, no further intervention | Yes | Musculoskeletal | Medium |
| Physical activity interventions | ||||||
| Brox et al. 2005, Norway [35] | Nursing home (129) | Stress management, nutrition, and exercise | No intervention | No | General sickness absence prevention | Medium |
| Eriksen et al. 2002, Norway [26] | Postal workers (blue collar) (860) | Exercise, education, and workplace adjustment | No intervention | No | General sickness absence prevention | Medium |
| Eriksen et al. 2002, Norway [26] | Postal workers (blue collar) (860) | Exercise with stress management | No intervention | No | General sickness absence prevention | Medium |
| Lindström et al. 1992, Sweden [22] | Auto workers (103) | Graded activity and back school | No intervention | Yes | Musculoskeletal | Medium |
| Nurminen et al. 2002, Finland [36] | Laundry workers (260) | Exercise | No intervention | No | Combination/ other | Low |
| Staal et al. 2004, Netherlands [24] | Airline employees (blue collar) (134) | Graded activity and exercise | No intervention | Yes | Musculoskeletal | Low |
| Tveito and Eriksen 2009, Norway [37] | Nurses and nursing aids (40) | Exercise, stress management training, and ergonomic examination of workplace | No intervention | No | Combination/ other | Medium |
| van Rehnen et al. 2007, Netherlands [29] | Telecom workers (792)a | Brief physical intervention | No intervention | No | Mental health (stress) | Medium |
aOf the 792 invited participants, 242 participated in the intervention, but all invited participants were analysed (intention to treat).
Four of 24 interventions reported a statistically significant reduction of sickness absence [21–24]. One study showed a small subgroup effect, but in accordance with the authors’ own conclusion, it was classified as not effective [25].
Six studies examined cognitive interventions [21,26–30]. Four focused on mental disorders [21,28–30] and two were general prevention [26,27]. A combination of CBT and problem solving therapy (PST) reduced sickness absence with 46% in employees with depression (n = 139) [21]. Other cognitive interventions [26–30] had no effect on sickness absence.
We concluded that there is limited evidence of effect of CBT combined with PST on sickness absence and no evidence of effect of other cognitive interventions on sickness absence.
There were five educational interventions reported in four articles, all focusing on musculoskeletal complaints [31–34]. None of these showed a significant reduction of sickness absence. There were no effects of information on back pain and handling of workloads [31], education about prevention of upper extremity pain [32], group meetings to increase physical activity and awareness of ergonomic work style [33] or education of baggage handlers in lifting techniques with or without a lumbar support [34].
We concluded that there is moderate evidence that workplace education aiming to prevent musculoskeletal disorders is not effective in reducing sickness absence.
Three articles reported results from five composite interventions [23,25,31], all targeting musculoskeletal complaints. The Sheerbrooke model, a comprehensive intervention including both workplace adjustment and a clinical component, showed a significant effect on sickness absence [23]. There were no effects of screening workplaces for hazards (focusing on lifting) and distributing a brochure about low back pain [31] and ergonomic adjustment, education and fast access to health care in a comprehensive intervention [25]. An effect on sickness absence from upper extremity complaints was explained by attrition bias [25].
We concluded that there is limited evidence for the effect of the Sheerbrooke model on sickness absence and no evidence of effect on sickness absence of other composite interventions.
There were eight interventions from seven articles on physical activity [22,24,26,29,35–37]. Two of these reported significant reductions of sickness absence. Graded activity and back schools had a significant effect on sickness absence and RTW in a population of auto workers with LBP [22], and the intervention and results were later replicated [24]. Workplace physical exercise was examined in five studies, none of which showed effect [26,29,35–37].
We concluded that there is moderate evidence that graded activity reduces sickness absence and moderate evidence that workplace exercise programs do not reduce sickness absence.
We searched clinicaltrials.gov for ongoing studies. We found 10 studies [38–47] that would probably have been included if they had been published. These were trials on physical exercise [38,45], obesity prevention [39,40,42] and education [41,43,46,47].
Discussion
Overall, there is moderate evidence that graded activity reduces sickness absence and limited evidence that the Sheerbrooke model and CBT reduce sickness absence. In addition, the studies included in this review indicate that there is also moderate evidence that workplace physical exercise programmes do not reduce sickness absence. In general, however, there is at best limited evidence that the workplace interventions considered are effective in reducing sickness absence.
The major strengths of the review were the broad inclusion criteria for diagnoses and interventions. Since many reviews focus on narrow groups of diagnosis and interventions, this review provides a supplementary overarching perspective. This is important due to the high frequency of comorbid complaints, both in the general population and in clinical populations [7,9].
There were also some limitations in the review. Blinding of participants and treatment providers is not possible in these interventions, thus motivation and preferences of the participants may influence the results. Some studies have reduced this problem by using register data. Data from sickness absence registers contain errors and limitations, but they are unlikely to be caused by systematic biases between intervention groups [48,49]. While the articles screened for inclusion in full text comprised studies from many countries, only one of the included studies was not Dutch or Nordic [23]. In the Netherlands and the Nordic countries, the employers and the state carry the major part of the sickness absence costs, and this may affect research funding. The Netherlands and Nordic countries are also the largest contributors to research on the related field of RTW, together with the USA [50]. Five of 12 studies excluded for insufficient sickness absence reporting were from the USA [51–55], so a lack of sickness absence data, or differences in the reporting of these data, may be one of many potential reasons why there were no US studies included.
In this review, the interventions were categorized into groups based on our combined understanding of the interventions and their content. This understanding is certainly open for discussion. As interventions grow more comprehensive and multidisciplinary, it becomes increasingly difficult to compare studies.
An evidence hierarchy [20] was used in order to make this review transparent and fair. The evidence hierarchy rules were used together with our understanding of the results. No intervention type was rated as ‘high-quality’ evidence because none of the intervention types showed significant sickness absence reduction in two studies with a low risk of bias. We did not use the latest version of the hierarchy [56] because it was less suited to the narrative approach we used.
The most frequent diagnoses linked to sickness absence are musculoskeletal and mental complaints [6]. The studies included in this review reflected this; musculoskeletal complaints and particularly LBP were the most frequent diagnostic groups.
Problems with recruitment of participants were commonly reported in our sample, thus many of the studies reported results from non-representative samples of employees. This reflects a more general problem with workplace interventions: those at high risk for sickness absence may be less likely to participate in the intervention, or may simply not be present at the workplace due to sickness absence [57].
Our results differ somewhat from other reviews of workplace interventions. A recent Cochrane review found moderate evidence for the effectiveness of changes in the work organization or work environment interventions on sickness absence [4]. Our wider definition may be one of the reasons why the results were different. In another review of workplace interventions for LBP, physical exercise and comprehensive multidisciplinary interventions were effective in reducing sickness absence [58]. Studies published after this review was completed and differences in inclusion criteria may explain the discrepancy.
Graded activity interventions led to a significant reduction in sickness absence in two studies [22,24]. However, another study that did not fulfil our workplace inclusion criterion has shown that graded activity had a negative effect on RTW for employees who were still on sickness absence after 8 weeks of participating in the Sheerbrooke model intervention [59]. Employees who do not respond to the Sheerbrooke model may need more treatment than graded activity provides. The primary purpose of graded activity programmes is to demonstrate by starting carefully and then gradually increasing the activity, that activity may be painful, but it is safe. According to Staal et al.: ‘The primary goal of the physical exercises was not to improve aerobic endurance, muscle strength, or any other aspect of physical fitness but to make the disabled worker aware that it was safe to move and to be physically active despite his or her pain’ [24]. This approach is consistent with the theory [60] behind the brief intervention that has been effective in multiple RCTs [61–64].
The Sheerbrooke model [23] is a comprehensive programme with cascading stages and components, including a workplace assessment. The programme focuses on involving all stakeholders around the injured worker. This approach has been identified as effective in previous reviews [5] and may be one of the reasons why the Sheerbrooke model reduced sick leave in this review, but it is not possible to confirm this from the available data. An adapted version of the Sheerbrooke model in the Netherlands also reduced sickness absence significantly [59] but recruited participants from occupational physicians and thus was not included in this review.
CBT is not widely tested in workplace settings. Our review suggests that CBT may reduce sickness absence for high-risk employees [21]. However, more studies are needed before firm conclusions can be drawn.
While the workplace interventions can reach large and diverse groups, those most in need of an intervention may be on sickness absence or feel too sick to participate. Targeting employees already on sickness absence may lead to better results, but preventing further sickness absence after the first long period of sickness absence may be more difficult [22,24,59]. Workplace interventions often do not focus on sickness absence per se, and additionally promoting activity when possible at times when pain and health complaints are present may be a more feasible goal [64].
In view of our findings organizations aiming to reduce sickness absence should not have too high expectations of sickness absence reduction resulting from workplace interventions. New approaches to sickness absence reduction may be necessary. Long-term investment in health and job satisfaction rather than tools for rapid sickness absence reduction may be a more effective approach [57].
Although there are many studies of workplace interventions, there is a need for more high-quality studies. Studies that test single component interventions, or that test individual intervention components separately, are valuable in determining which components (or combination of components) are most effective in reducing sickness absence. Also, a more standardized way of measuring and reporting sickness absence internationally would be helpful for comparing studies and allow meaningful meta-analyses.
In conclusion, the currently available evidence does not support active workplace interventions as being generally effective in reducing sickness absence. However, there is moderate evidence that graded activity reduces sickness absence and limited evidence that the Sheerbrooke model and CBT reduce sickness absence. The studies included in this review provide moderate evidence that physical activity and education do not reduce sickness absence. Reducing sickness absence with active workplace interventions is possible, but the intervention content must be carefully considered.
Key points
Previous reviews on workplace interventions have studied specific diagnoses or interventions. This systematic review is an overarching review of active workplace interventions for all diagnoses.
Active workplace interventions do not seem to be generally effective in reducing sickness absence. However, there is moderate evidence that graded activity reduces sickness absence and limited evidence that the Sheerbrooke model and cognitive behavioural therapy reduce sickness absence.
Active interventions may be ineffective if the goal is short term sickness absence reduction alone. However, these interventions may have other benefits not considered in this review.
Funding
Clinic of Physical Medicine and Rehabilitation, Vestfold Hospital Trust, Stavern, Norway, and Norwegian Research Council.
Conflicts of interest
None declared.
Supplementary Material
Acknowledgements
Many thanks to Lisa M. Aarsheim and Helene Sofie Eriksen, who helped with sourcing articles, maintaining the database and retrieving e-mail addresses of authors. Also thanks to Svenn Sivertsen at medical library of the University of Bergen for assisting in creating the search terms.
References
- 1. Waddel G, Burton AK. Is Work Good for Your Health and Well-Being? London: The Stationery Office, 2006. [Google Scholar]
- 2. Côté P, Baldwin ML, Johnson WG, Frank JW, Butler RJ. Patterns of sick-leave and health outcomes in injured workers with back pain. Eur Spine J 2008; 17: 484–493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kivimäki M, Head J, Ferrie JE, Shipley MJ, Vahtera J, Marmot MG. Sickness absence as a global measure of health: evidence from mortality in the Whitehall II prospective cohort study. Br Med J 2003; 327: 364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. van Oostrom SH, Driessen MT, de Vet HC, et al. Workplace interventions for preventing work disability. Cochrane Database Syst Rev 2009; 2:CD006955 [DOI] [PubMed] [Google Scholar]
- 5. Carroll C, Rick J, Pilgrim H, Cameron J, Hillage J. Workplace involvement improves return to work rates among employees with back pain on long-term sick leave: a systematic review of the effectiveness and cost-effectiveness of interventions. Disabil Rehabil 2010; 32: 607–621 [DOI] [PubMed] [Google Scholar]
- 6. NAV. Sykefraværstilfeller 2 kv 2001–2011. Diagnose og kjønn. Antall - Sykefraværsstatistikk - Sykefraværsstatistikk - NAV http://www.nav.no/Om+NAV/Tall+og+analyse/Jobb+og+helse/Sykefrav%C3%A6rsstatistikk/Sykefrav%C3%A6rsstatistikk/Sykefrav%C3%A6rstilfeller+2+kv+2001–2011.+Diagnose+og+kj%C3%B8nn.+Antall.287520.cms (30 September 2011, date last accessed)
- 7. Hestbaek L, Leboeuf-Yde C, Kyvik KO, et al. Comorbidity with low back pain. Spine 2004; 29: 1483–91 [DOI] [PubMed] [Google Scholar]
- 8. Ihlebaek C, Eriksen HR, Ursin H. Prevalence of subjective health complaints (SHC) in Norway. Scand J Public Health 2002; 30: 20–29 [PubMed] [Google Scholar]
- 9. Ihlebaek C, Brage S, Eriksen HR. Health complaints and sickness absence in Norway, 1996-2003. Occup Med (Lond) 2007; 57: 43–49 [DOI] [PubMed] [Google Scholar]
- 10. Reme SE, Tangen T, Moe T, Eriksen HR. Prevalence of psychiatric disorders in sick listed chronic low back pain patients. Eur J Pain 2011; 15: 1075–1080 [DOI] [PubMed] [Google Scholar]
- 11. Norcross JC, Karpiak CP, Santoro SO. Clinical psychologists across the years: the division of clinical psychology from 1960 to 2003. J Clin Psychol 2005; 61: 1467–1483 [DOI] [PubMed] [Google Scholar]
- 12. Hagen KB, Hilde G, Jamtvedt G, Winnem MF. The Cochrane review of bed rest for acute low back pain and sciatica. Spine 2000; 25: 2932–2939 [DOI] [PubMed] [Google Scholar]
- 13. Schaafsma F, Schonstein E, Ojajärvi A, Verbeek J. Physical conditioning programs for improving work outcomes among workers with back pain. Scand J Work Environ Health 2011; 37: 1–5 [DOI] [PubMed] [Google Scholar]
- 14. de Greef M, van Wijck R, Reynders K, et al. Impact of the Groningen exercise therapy for symphony orchestra musicians program on perceived physical competence and playing-related musculoskeletal disorders of professional musicians Med Probl Perform Art 2003; 18: 156–160 [Google Scholar]
- 15. Bethge M, Herbold D, Trowitzsch L, Jacobi C. Work status and health-related quality of life following multimodal work hardening: a cluster randomised trial. J Back Musculoskelet Rehabil 2011; 24: 161–172 [DOI] [PubMed] [Google Scholar]
- 16. Rosenfeld O, Tenenbaum G, Ruskin H, et al. Behavioural modifications following a physical activity programme in the Israeli pharmaceutical industry Aust J Sci Med Sport 1990; 22: 93–96 [Google Scholar]
- 17. Doctor RS, Curtis D, Isaacs G. Psychiatric morbidity in policemen and the effect of brief psychotherapeutic intervention—a pilot study Stress Med 1994; 10: 151–157 [Google Scholar]
- 18. Thomas J, Brunton J. EPPI-Reviewer 3.0: Analysis and Management of Data for Research Synthesis. London: EPPI-Centre Software, Social Science Research Unit, Institute of Education, 2009. [Google Scholar]
- 19. Higgins JT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Chichester, West Sussex: Wiley Online Library, 2008. [Google Scholar]
- 20. van Tulder M, Furlan A, Bombardier C, Bouter L. Editorial Board of the Cochrane Collaboration Back Review Group Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine 2003; 28: 1290–1299 [DOI] [PubMed] [Google Scholar]
- 21. Lexis MA, Jansen NW, Huibers MJ, et al. Prevention of long-term sickness absence and major depression in high-risk employees: a randomised controlled trial. Occup Environ Med 2011; 68: 400–407 [DOI] [PubMed] [Google Scholar]
- 22. Lindström I, Ohlund C, Eek C, et al. The effect of graded activity on patients with subacute low back pain: a ran domized prospective clinical study with an operant-con ditioning behavioral approach. Phys Ther 1992; 72: 279–90 [DOI] [PubMed] [Google Scholar]
- 23. Loisel P, Abenhaim L, Durand P, et al. A population-based, randomized clinical trial on back pain management. Spine 1997; 22: 2911–2918 [DOI] [PubMed] [Google Scholar]
- 24. Staal JB, Hlobil H, Twisk JW, Smid T, Köke AJ, van Mechelen W. Graded activity for low back pain in occupational health care: a randomized, controlled trial. Ann Intern Med 2004; 140: 77–84 [DOI] [PubMed] [Google Scholar]
- 25. IJzelenberg H, Meerding WJ, Burdorf A. Effectiveness of a back pain prevention program: a cluster random ized controlled trial in an occupational setting. Spine 2007; 32: 711–719 [DOI] [PubMed] [Google Scholar]
- 26. Eriksen HR, Ihlebaek C, Mikkelsen A, Grønningsaeter H, Sandal GM, Ursin H. Improving subjective health at the worksite: a randomized controlled trial of stress management training, physical exercise and an integrated health programme. Occup Med (Lond) 2002; 52: 383–391 [DOI] [PubMed] [Google Scholar]
- 27. Proper KI, van der Beek AJ, Hildebrandt VH, Twisk JW, van Mechelen W. Worksite health promotion using individual counselling and the effectiveness on sick leave; results of a randomised controlled trial. Occup Environ Med 2004; 61: 275–279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. van Oostrom SH, van Mechelen W, Terluin B, de Vet HC, Knol DL, Anema JR. A workplace intervention for sick-listed employees with distress: results of a randomised controlled trial. Occup Environ Med 2010; 67: 596–602 [DOI] [PubMed] [Google Scholar]
- 29. van Rhenen W, Blonk RW, Schaufeli WB, van Dijk FJ. Can sickness absence be reduced by stress reduction programs: on the effectiveness of two approaches. Int Arch Occup Environ Health 2007; 80: 505–515 [DOI] [PubMed] [Google Scholar]
- 30. Rebergen DS, Bruinvels DJ, Bezemer PD, van der Beek AJ, van Mechelen W. Guideline-based care of common mental disorders by occupational physicians (CO-OP study): a randomized controlled trial. J Occup Environ Med 2009; 51: 305–312 [DOI] [PubMed] [Google Scholar]
- 31. Frost P, Haahr JP, Andersen JH. Reduction of pain-related disability in working populations: a randomized intervention study of the effects of an educational booklet addressing psychosocial risk factors and screening workplaces for physical health hazards. Spine 2007; 32: 1949–1954 [DOI] [PubMed] [Google Scholar]
- 32. Speklé EM, Hoozemans MJ, Blatter BM, et al. Effectiveness of a questionnaire based intervention programme on the prevalence of arm, shoulder and neck symptoms, risk factors and sick leave in computer workers: a cluster randomised controlled trial in an occupational setting. BMC Musculoskelet Disord 2010; 11: 99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bernaards CM, Bosmans JE, Hildebrandt VH, van Tulder MW, Heymans MW. The cost-effectiveness of a lifestyle physical activity intervention in addition to a work style intervention on recovery from neck and upper limb symptoms and pain reduction in computer workers. Occup Environ Med 2011; 68: 265–272 [DOI] [PubMed] [Google Scholar]
- 34. van Poppel MN, Koes BW, van der Ploeg T, Smid T, Bouter LM. Lumbar supports and education for the prevention of low back pain in industry: a randomized controlled trial. J Am Med Assoc 1998; 279: 1789–1794 [DOI] [PubMed] [Google Scholar]
- 35. Brox JI, Frøystein O. Health-related quality of life and sickness absence in community nursing home employees: randomized controlled trial of physical exercise. Occup Med (Lond) 2005; 55: 558–563 [DOI] [PubMed] [Google Scholar]
- 36. Nurminen E, Malmivaara A, Ilmarinen J, et al. Effectiveness of a worksite exercise program with respect to perceived work ability and sick leaves among women with physical work. Scand J Work Environ Health 2002; 28: 85–93 [DOI] [PubMed] [Google Scholar]
- 37. Tveito TH, Eriksen HR. Integrated health programme: a workplace randomized controlled trial. J Adv Nurs 2009; 65: 110–119 [DOI] [PubMed] [Google Scholar]
- 38. University of Southern Denmark. Work Place Health Promotion: A Change Project http://www.clinicaltrials.gov/show/NCT01366950 (6 March 2012, date last accessed)
- 39. University of North Carolina, Chapel Hill. Comparison of Two Workplace-Sponsored Obesity Prevention Programs http://www.clinicaltrials.gov/ct2/show/NCT00481715 (6 March 2012, date last accessed)
- 40. University of North Carolina, Chapel Hill. Interventions to Control Obesity in Community Colleges (CDC WAY to Health) http://www.clinicaltrials.gov/ct2/show/NCT01282775 (6 March 2012, date last accessed)
- 41. University of Illinois. Cost Effective Health Promotion for Older Adults http://www.clinicaltrials.gov/show/NCT00953030 (6 March 2012, date last accessed)
- 42. University of Aarhus. Physical Exercise, Dietary Counseling and Cognitive Behavioral Training as a Combined Intervention to Reduce Weight and Increase Workability in Health Care Workers http://www.clinicaltrials.gov/show/NCT01015716 (6 March 2012, date last accessed)
- 43. Uni Research (previously Unifob A/S). Ibedrift – A Trial Comparing a New Approach to Musculoskeletal Pain Consisting of Education and Peer Involvement to Treatment as Usual http://www.clinicaltrials.gov/show/NCT00741650 (6 March 2012, date last accessed)
- 44. The Washington Center for Clinical Research. Multicenter Worksite Nutrition Study http://www.clinicaltrials.gov/show/NCT01224548 (6 March 2012, date last accessed)
- 45. Hospices Civils de Lyon. An Educational and Exercise Program as Secondary Prevention of Recurrent Lower Back Pain in Healthcare Workers http://www.clinicaltrials.gov/show/NCT00782925 (6 March 2012, date last accessed)
- 46. Centers for Disease Control and Prevention. Computerized Risk Assessment in an Employee Population http://www.clinicaltrials.gov/show/NCT00153335 (6 March 2012, date last accessed)
- 47. Boston Medical Center. Automated Assessment of Mental Health in the Workplace http://www.clinicaltrials.gov/show/NCT00134576 (6 March 2012, date last accessed)
- 48. van Poppel MN, de Vet HC, Koes BW, Smid T, Bouter LM. Measuring sick leave: a comparison of self-reported data on sick leave and data from company records. Occup Med (Lond) 2002; 52: 485–490 [DOI] [PubMed] [Google Scholar]
- 49. Øyeflaten I, Lie SA, Ihlebaek C, et al. Comparison of self-reported and register data on sickness absence among Norwegian patients participating in an occupational rehabilitation program Nor Epidemiol 2009; 19: 161–167 [Google Scholar]
- 50. Rollin L, Gehanno JF. Research on return to work in European Union countries. Occup Med (Lond) 2012; 62: 210–215 [DOI] [PubMed] [Google Scholar]
- 51. Rahe RH, Taylor CB, Tolles RL, Newhall LM, Veach TL, Bryson S. A novel stress and coping workplace program reduces illness and healthcare utilization. Psychosom Med 2002; 64: 278–286 [DOI] [PubMed] [Google Scholar]
- 52. Reddell CR, Congleton JJ, Dale Huchingson R, Montgomery JF. An evaluation of a weightlifting belt and back injury prevention training class for airline baggage handlers. Appl Ergon 1992; 23: 319–329 [DOI] [PubMed] [Google Scholar]
- 53. Daltroy LH, Iversen MD, Larson MG, et al. A controlled trial of an educational program to prevent low back injuries. N Engl J Med 1997; 337: 322–328 [DOI] [PubMed] [Google Scholar]
- 54. Jeffery RW, Forster JL, Dunn BV, French SA, McGovern PG, Lando HA. Effects of work-site health promotion on illness-related absenteeism. Occup Med (Lond) 1993; 35: 1142–1146 [DOI] [PubMed] [Google Scholar]
- 55. Feuerstein M, Huang GD, Ortiz JM, Shaw WS, Miller VI, Wood PM. Integrated case management for work-related upper-extremity disorders: impact of patient satisfaction on health and work status. J Occup Environ Med 2003; 45: 803–812 [DOI] [PubMed] [Google Scholar]
- 56. Furlan AD, Pennick V, Bombardier C, van Tulder M. Editorial Board, Cochrane Back Review Group 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine 2009; 34: 1929–1941 [DOI] [PubMed] [Google Scholar]
- 57. Tveito TH, Halvorsen A, Lauvaalien JV, et al. Room for everyone in working life? 10% of the employees—82% of the sickness leave Nor Epidemiol 2002; 12: 63–68 [Google Scholar]
- 58. Tveito TH, Hysing M, Eriksen HR. Low back pain interventions at the workplace: a systematic literature review. Occup Med (Lond) 2004; 54: 3–13 [DOI] [PubMed] [Google Scholar]
- 59. Anema JR, Steenstra IA, Bongers PM, et al. Multidisciplinary rehabilitation for subacute low back pain: graded activity or workplace intervention or both? A randomized controlled trial. Spine 2007; 32: 291–298 [DOI] [PubMed] [Google Scholar]
- 60. Eriksen HR, Murison R, Pensgaard AM, Ursin H. Cognitive activation theory of stress (CATS): from fish brains to the Olympics. Psychoneuroendocrinology 2005; 30: 933–938 [DOI] [PubMed] [Google Scholar]
- 61. Indahl A, Haldorsen EH, Holm S, Reikerås O, Ursin H. Five-year follow-up study of a controlled clinical trial using light mobilization and an informative approach to low back pain. Spine 1998; 23: 2625–2630 [DOI] [PubMed] [Google Scholar]
- 62. Hagen EM, Eriksen HR, Ursin H. Does early intervention with a light mobilization program reduce long-term sick leave for low back pain? Spine 2000; 25: 1973–1976 [DOI] [PubMed] [Google Scholar]
- 63. Brox JI, Sørensen R, Friis A, et al. Randomized clinical trial of lumbar instrumented fusion and cognitive intervention and exercises in patients with chronic low back pain and disc degeneration. Spine 2003; 28: 1913–1921 [DOI] [PubMed] [Google Scholar]
- 64. Sorensen PH, Bendix T, Manniche C, Korsholm L, Lemvigh D, Indahl A. An educational approach based on a non-injury model compared with individual symptom-based physical training in chronic LBP. A pragmatic, randomised trial with a one-year follow-up. BMC Musculoskelet Disord 2010; 11: 212 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.