Abstract
Background. The mechanism of Plasmodium falciparum resistance to quinine is not known. In vitro quantitative trait loci mapping suggests involvement of a predicted P. falciparum sodium–hydrogen exchanger (pfnhe–1) on chromosome 13.
Methods. We conducted prospective quinine efficacy studies in 2 villages, Kollé and Faladié, Mali. Cases of clinical malaria requiring intravenous therapy were treated with standard doses of quinine and followed for 28 days. Treatment outcomes were classified using modified World Health Organization protocols. Molecular markers of parasite polymorphisms were used to distinguish recrudescent parasites from new infections. The prevalence of pfnhe–1 ms4760–1 among parasites before versus after quinine treatment was determined by direct sequencing.
Results. Overall, 163 patients were enrolled and successfully followed. Without molecular correction, the mean adequate clinical and parasitological response (ACPR) was 50.3% (n = 163). After polymerase chain reaction correction to account for new infections, the corrected ACPR was 100%. The prevalence of ms4760–1 increased significantly, from 26.2% (n = 107) before quinine treatment to 46.3% (n = 54) after therapy (P = .01). In a control sulfadoxine–pyrimethamine study, the prevalence of ms4760–1 was similar before and after treatment.
Conclusions. This study supports a role for pfnhe–1 in decreased susceptibility of P. falciparum to quinine in the field.
Keywords: Malaria, recurrence, antimalarials, Plasmodium falciparum, drug resistance, sodium–hydrogen antiporter, microsatellite, Mali
Control of uncomplicated cases of malaria has been greatly impaired by development of resistance against mainstay antimalarial agents [1, 2]. The first–line antimalarial strategy is presently artemisinin combination therapy. Quinine (QN) is used in many malaria-endemic countries for the management of severe life–threatening malaria and as rescue therapy for parasites resistant to other antimalarial drugs. As a monotherapy, QN is associated with significant recrudescence rates [3]. This may be because QN is a rapidly acting drug with a relatively short elimination half–life [4, 5]. Failure of QN in malaria treatment has been long documented, particularly in South America [6, 7] and Southeast Asia [8]. Although high–level resistance of Plasmodium falciparum to QN is rare, in vivo and in vitro decreases in parasite susceptibility have led to the use of this drug in combination, particularly with the antibiotics tetracycline or doxycycline [9–13].
The mechanisms of decreased P. falciparum susceptibility to QN are not clearly understood. Modulation of in vitro QN sensitivity has been associated with single nucleotide polymorphisms in the pfcrt (chloroquine–resistance transporter) and pfmdr1 (multidrug resistance 1) genes [14, 15]. Involvement of additional genes also seems to be important, because the association of pfcrt and pfmdr1 is not always observed [16]. This reality of a complex phenotype is also supported by the frequent efficacy of QN against chloroquine-resistant parasites [17, 18].
The availability of a laboratory-derived genetic cross between 2 parasites of markedly different in vitro QN responses [19] permitted a quantitative trait loci–based approach that identified genomic regions contributing to the phenotypes [18]. Analysis showed a possible association between reduced P. falciparum susceptibility to QN and a locus on chromosome 13. A pairwise effect was also detected between that chromosome 13 locus and an additional locus on chromosome 9. The set of predicted genes on the chromosome 13 locus included a homologue to the family of Na+/H+ exchanger (NHE) proteins [18]. The P. falciparum–encoded PfNHE–1 is 1920 amino acids long and harbors an open reading frame with a microsatellite polymorphism consisting of variable DNNND repeat units, designated ms4760. The predicted pfnhe–1 sequence was analyzed in the Dd2 × HB3 progeny, as well as in a range of field isolates and laboratory strains with variable susceptibilities to QN. Eight variants of ms4760 were originally discovered. The variant ms4760–1 with 2 copies of DNNND repeat units was significantly associated with reduced in vitro QN sensitivity [18]. These results were later supported by transfection experiments [20]. The aforementioned studies were performed with in vitro cultured laboratory strains. However, these polymorphisms were also present in natural P. falciparum populations [21] and found to be associated with QN sensitivity among field isolates in in vitro assays [22–24].
Here we extend these studies to clinical settings by exploring the in vivo impact of QN therapy on the prevalence of the pfnhe–1 ms4760 and pfcrt polymorphisms in 2 Malian villages.
METHODS
Study Design and Procedures
This QN efficacy study was conducted in Kollé and Faladié, Mali. Kollé (with approximately 2800 inhabitants) is a rural village located 57 km south of Bamako, the capital city of Mali. Faladié (with approximately 3000 inhabitants) is located 80 km northwest of Bamako. Malaria is endemic in both villages, with seasonal transmission occurring between July and December.
Patients presenting with clinical malaria requiring intravenous treatment were eligible for the study. The 28–day World Health Organization (WHO) 2003 protocol for antimalarial drug efficacy was adapted to the QN regimen [25]. Patients aged ≥6 months who presented with P. falciparum malaria at a parasitemia of ≥500 000 trophozoites/μL or who had ≥1 clinical symptom of severe malaria (eg, coma [Blantyre coma scale score of <2], prostration, inability to drink or eat, vomiting, convulsion, obsessing, respiratory distress, icterus, and hematuria associated with the presence of parasites) were included. Informed consent or assent was obtained before any protocol–specific procedure was performed. Pregnant women, patients allergic to QN, and patients whom the physician believed to be too severely ill were excluded from the study. At inclusion, thick and thin blood smears and full clinical examinations were performed for each.
Patients enrolled during 2005–2007 were treated with 12.5 mg/kg QN twice daily for 5 days. In 2008, the regimen was changed to 8 mg/kg 3 times daily for 7 days, according to established protocols (WHO malaria treatment guideline 2006 [WHO/HTM/MAL/2006.1108]). All patients received full curative doses of QN, which was administered by the study team in an inpatient setting. QN treatment was administered intravenously with 10% hypertonic glucose solution until the patient was able to receive oral treatment.
Follow–up was adapted to the QN treatment schedule. Briefly, active follow–up was performed on days 1–7, 14, 21, and 28. Body weight, height, axillary temperature, splenomegaly prevalence, pulse rate, breathing rate, and other signs of a severe condition were measured and recorded on case report forms. For laboratory assessments at enrollment and at each follow–up visit (days 0, 1, 3, 7, 14, 21, and 28 and during unscheduled visits), thick and thin blood films and blotting of blood onto filter paper samples were performed. Thick and thin blood films were stained with Giemsa stain, and parasite density was determined by dividing the number of asexual parasites by 300 leukocytes and multiplying by 7500 (the estimated mean of leukocytes/microliter of blood) [26].
Treatment outcomes were defined according to the clinical or parasitologic response and were classified as early therapeutic failure (ETF), late clinical failure (LCF), late parasitological failure (LPF), and adequate clinical and parasitologic response (ACPR), according to slight modifications of WHO protocols [25].
Cases of QN treatment failure were treated with artesunate–amodiaquine or artemether–lumefantrine, according to the Malian National Malaria Control Program guidelines. Severe malaria cases that could not be managed in the field clinic were referred to teaching hospitals in Bamako.
As a control, a prospective sulfadoxine-pyrimethamine efficacy study was conducted as described elsewhere in Kollé during 2007 and 2008 [27]. The prevalence of ms4760–1 in baseline and post–sulfadoxine–pyrimethamine infections was measured.
The study was approved by the Ethics Committee of the Faculty of Medicine, Pharmacy, and Odonto–Stomatology, University of Bamako, Mali, and the Ethics Committee of the National Institutes of Allergy and Infectious Diseases, National Institutes of Health, Bethesda.
Molecular Methods
P. falciparum genomic DNA was extracted from blood blotted onto filter paper samples by an established methanol–based method [28].
Molecular markers of parasite polymorphisms pfmsp1, pfmsp2, and CA1 were used to distinguish recrudescent parasites from new infections by nested polymerase chain reaction (PCR), as described elsewhere [29, 30]. A sample was classified as a true failure if it was recrudescent with all 3 markers.
The diversity of ms4760 was determined by direct PCR amplicon sequencing in all samples before QN treatment and in all recurrent parasitemia during the 28–day follow–up. Nested PCR was performed for the first PCR amplification, with the following primers and conditions: F1fw 5′–GACAATTTCGGTAGATGCCCTAT–3′ and R1rev 5′–GGTCTTGCAGTGCAT GGA–3′, using 1 × buffer, 1.5 mM of MgCl2, 200 µm of each dNTP, 1 µm of each primer, and 0.625 U of the Taq DNA polymerase (Invitrogen, San Diego, CA, USA). The product was used to perform the second amplification with the following primers, under the same conditions as the first amplification: F2fw 5′–AGTGGTAGTAATAATGATA–3′ and R5rev 5′–GTACCCTTAGTTGAAATATT–3′. Products of approximately 350 base pairs from the second amplification were treated with ExoSAP–IT enzyme, as recommended by the manufacturer (USB, Cleveland, OH). The obtained product was capillary sequenced using the second amplification primers F2fw and R5rev and fluorescent nucleotides in an ABI 3730XL automatic sequencer (Applied Biosystems, Foster City, CA). The prevalence of ms4760–1 among parasites before versus after QN treatment was determined. Conversely, as a negative control, we measured the prevalence of ms4760–1 at baseline and after sulfadoxine–pyrimethamine treatment. DNA was extracted from blood blotted filter papers that was collected before treatment and for any parasitemia after administration of sulfadoxine–pyrimethamine. Sequencing was performed as described above. The polymorphism of pfnhe–1 ms4760 was determined by alignment. The prevalence of pfnhe–1 ms4760 was compared between the pretreatment and posttreatment infections.
Samples collected before and after QN treatment and for which the results from pfnhe–1 analyses were available were tested for the pfcrt K76T codon, using previously described methods [31].
Quinine Plasma Levels
Plasma QN levels were determined in blood samples collected at 3 time points: before QN administration on day 0, 7 days after the initiation of treatment, and 14 days after the initiation of treatment. Only patients with samples from the 3 time points described above were included in this pharmacokinetic analysis. Fifty microliters of plasma were used for QN quantification. Quinine was measured by liquid chromatography with spectrometric detection after extraction by a dichloromethane isopropanol mixture in the presence of hydroquinidine chlorhydrate as an internal standard. Detection was by excitation at 350 nm and fluorometric emission at 440 nm, using a flow rate of 2 mL/min, with the injection rate set at 30 µL. A 4.6 mm × 25 cm ultrasphere column with octadecylsilane particles (Beckman) was used (the protocol was developed at Laboratoire de Pharmacologie Analytique et Pharmacocinétique, Hôpital Saint–Vincent de Paul, Paris France).
Data Analysis
Patients were included in the analysis only if they received the correct dose of the study drug, attended all follow–up visits, and did not take another antimalarial drug during the follow–up period.
EpiInfo version 6.04 (Centers for Disease Control and Prevention, Atlanta, GA), SPSS 11.0 (The Predictive Analytics; IBM, Chicago, IL), and STATA 9.1 (StataCorp, College Station, TX) were used to generate summary statistics and to compare therapeutic efficacy. The Spearman correlation test was used to assess the relation between ms4760–1 and the pfcrt K76T codon mutation. The prevalence of polymorphisms before versus after QN therapy was compared with the Fisher exact test and 2 × 2 contingency table analysis. Sequencher vs 4.7 (Gene Codes, Ann Arbor, MI) was used to align and compare field sample sequences with the previously described 8 variants of pfnhe–1 ms4760 [18].
RESULTS
In Vivo Quinine Efficacy
Overall, 169 patients were enrolled (83 from Faladié and 86 from Kollé). Six were lost to follow–up, yielding 163 patients for the final in vivo analyses. Without molecular correction, the mean ACPR was 50.3% (Table 1). After PCR correction to account for new infections, the corrected ACPR was 100% (Table 1). Results for the 2 villages were similar. Overall, 81 patients (49.7%) had a patent infection during follow–up. After the 5–day and 7–day QN treatment regimens, 69 of 126 patients (54.8%) and 12 of 37 patients (32.4%), respectively, presented with posttreatment parasitemia (P = .01). The 7–day treatment regimen delayed reinfections by 5 days, from day 14 to day 19 after treatment initiation.
Table 1.
In Vivo Quinine Efficacy Among Subjects From Faladié and Kollé, Before and After Molecular Correction
| Parameter | Faladié, Subjects, % (n = 82) | Kollé, Subjects, % (n = 81) | Overall, Subjects, % (n = 163) |
|---|---|---|---|
| LCF | 12.4 | 23.5 | 17.9 |
| LPF | 39.5 | 23.5 | 31.5 |
| ACPR | 48.2 | 53.1 | 50.3 |
| ACPRc | 100 | 100 | 100 |
Abbreviations: ACPR, adequate clinical and parasitological response; ACPRc, adequate clinical and parasitological response after molecular correction; LCF, late clinical failure; LPF, late parasitological failure.
Most (94%) of the 163 patients cleared parasitemia by day 3 after initiation of QN therapy, while all patients had cleared parasitemia and fever by day 7.
Molecular Analysis
All 163 day 0 samples were available for molecular analysis, while only 73 of 81 posttreatment samples were available. Of the 236 samples amplified by PCR, 22.9% were mixed infections and did not yield usable sequences. PCR and sequencing were successful in 107 of 163 samples (65.6%) obtained before QN therapy and in 54 of 73 (74.0%) obtained after QN therapy. The polymorphism of pfnhe–1 ms4760 was determined by alignment and compared between pretreatment and posttreatment samples.
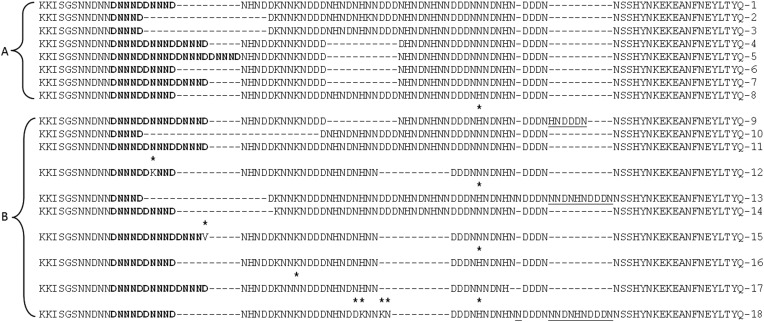
Overall, 6 of the 8 pfnhe–1 microsatellites described by Ferdig et al [18] and 10 other ms4760 variants were found. Alignment of these variants showed new deletions or insertions (Figure 1), of which 5 had been observed in other studies with samples from Africa and India [24, 32–34].
Figure 1.
Alignment of ms4760 microsatellite sequences from different Plasmodium falciparum lines. A, The 8 sequences described by Ferdig et al [18]. B, The 10 new sequences from the Malian Quinine study. DNNND copies are highlighted in bold. Asterisks indicate base changes to the encoding nucleotide sequence. Insertions are underlined. New sequences found in Mali are classified from ms4760-9 to ms4760-18.
ms4760–1 was present in 26.2% of samples (107) obtained before QN treatment but in 46.3% of samples (54; P = .01) obtained after QN treatment. The odds of recurrent parasitemia after QN therapy among patient presenting with ms4760–1 at day 0 were 2.4 times the odds among patients who did not present with ms4760–1 at day 0 (95% confidence interval, 1.2–4.8). In the control sulfadoxine–pyrimethamine study, the prevalence of ms4760–1 before treatment was not statistically different from the prevalence after treatment (Table 2).
Table 2.
Selection of ms4760-1 by Quinine but Not Sulfadoxine-pyrimethamine in P. falciparum Parasites From Subjects in Kolle and Faladje, Mali
| Treatment | Before Treatment, Samples, % (No.) | After Treatment, Samples, % (No.) | Pa | OR (95% CI) |
|---|---|---|---|---|
| Quinine | 26.2 (107) | 46.3 (54) | .01 | 2.43 (1.2–4.8) |
| SP | 31.8 (44) | 14.3 (21) | .23 | 0.36 (.09–1.4) |
Abbreviations: CI, confidence interval; OR, odds ratio.
a By the χ2 or Fisher exact tests.
There was a trend toward decreased prevalence of ms4760–1 from day 14 (66%; n = 9) to later time points (days 21–28; 42.2%; n = 45). Interestingly, at each of these time points, the prevalence of ms4760–1 remained higher than at baseline (data not shown).
The ms4760-3 marker, in contrast, was significantly more prevalent before treatment (36.4%) than after treatment (14.8%; P = .004). The remaining microsatellites were randomly distributed before and after the QN treatment (Table 3)
Table 3.
ms4760 Diversity Among Parasites in Samples Collected Before (Day 0) and After Quinine Treatment From Subjects in Kollé and Faladié
| Prevalence, % |
|||
|---|---|---|---|
| Variant | Day 0 Parasites (n = 107) | Recurrent Parasites (n = 54) | P |
| ms4760-1 | 26.2 | 46.3 | .01 |
| ms4760-2 | 0 | 0 | NA |
| ms4760-3 | 36.4 | 14.8 | .004 |
| ms4760-4 | 0 | 0 | NA |
| ms4760-5 | 1.9 | 1.85 | .5 |
| ms4760-6 | 3.7 | 1.85 | .8 |
| ms4760-7 | 22.5 | 16.7 | .3 |
| ms4760-8 | 3.7 | 7.4 | .5 |
| ms4760-9 | 0 | 1.85 | NA |
| ms4760-10 | 0 | 1.85 | NA |
| ms4760-11 | 1.9 | 0 | NA |
| ms4760-12 | 0 | 1.85 | NA |
| ms4760-13 | 0 | 1.85 | NA |
| ms4760-14 | 0.9 | 0 | NA |
| ms4760-15 | 1.9 | 0 | NA |
| ms4760-16 | 0 | 1.85 | NA |
| ms4760-17 | 0.9 | 0 | NA |
| ms4760-18 | 0 | 1.85 | NA |
The predominant variants are in bold.
Abbreviation: NA, not applicable.
Among the samples from both villages, pfcrt codon 76 analysis was successful in 74 pre–QN and 28 post-QN treatment samples. Mixed infections with both wild-type and mutant alleles were excluded. The prevalence of the pfcrt 76T codon was similar in the pretreatment samples, compared with the posttreatment samples (Table 4)
Table 4.
pfcrt K76T Profile Distributions Among Parasites Harboring ms4760–1 in Samples Collected Before and After Quinine Treatment From Subjects in Kollé and Faladié
| Profile | Before Treatment, Samples, % (No.) | After Treatment, Samples, % (No.) | P |
|---|---|---|---|
| pfcrt 76T | 69.0 (74) | 64.3 (28) | .6 |
| ms4760–1/pfcrt 76T | 55.6 (18) | 80.0 (10) | .3 |
Pharmacokinetics Analysis
Of 30 patients included in the PK study, a subset of 12 showed interpretable results. Among those 12 patients, the mean plasma level of QN was 25 µg/mL at day 7 (interquartile range, 1.88–3.11) but was below the detection limit of 1 µg/mL at day 14.
DISCUSSION
In this study, QN treatment selected malaria parasites with the pfnhe–1 microsatellite ms4760–1. The observed selection appears to be QN specific, as the treatment with sulfadoxine–pyrimethamine was not associated with such selection of ms4760–1 in posttreatment parasites.
Our data are in agreement with the study by Ferdig et al [18] that found an association between pfnhe–1 and decreased susceptibility to QN. They are also consistent with other studies that assessed the role of pfnhe–1 in P. falciparum resistance to QN in culture–adapted parasites [16, 33], culture–adapted P. falciparum field isolates, or ex vivo experiments [32]. More-recent in vitro studies also point to the involvement of the pfnhe–1 gene in modulation of QN response in vitro in field samples [33], and Nkruma et al [20] provide transfection data that support a role for pfnhe–1 in QN resistance, albeit in a strain–dependent manner. Finally, Ugandan field isolates harboring ms4760–1 showed a modest decrease of in vitro QN sensitivity, but the presence of ms4760–1 did not predict clinical failure during the in vivo study [34]. Our results are, however, at odds with other recent reports suggesting that the pfnhe–1 ms4760 microsatellite was not associated with QN susceptibility in the Republic of Congo, in Asia [23, 35], and in travelers returning to France from various countries [36]. These discordant findings suggest that the role of pfnhe–1 in QN resistance may be dependent on the genetic background of the parasites [20] and/or geographic origin [23].
When markers of parasite polymorphisms were used to distinguish true recrudescent infections from reinfections, we found that all recurrent parasites were different from the original day 0 parasites. Yet, we show clinical evidence for significant selection of ms4760-1 on initiation of QN therapy. Furthermore, given the low serum levels of QN on day 14—consistent with its pharmacokinetic characteristics—the question arises of how this selection of ms4760–1 would have occurred in vivo. One hypothesis might be that the observed selection was merely due to normal biological fluctuations during follow–up. However, in these same villages, when sulfadoxine–pyrimethamine was used to treat patients, there was no selection of ms4760-1, indicating that the selection observed in the QN study was indeed due to an effect of QN.
Most of the selective effect was observed in parasites appearing in the bloodstream at day 14. This peak of selection just 2 weeks after initiation of treatment raises the possibility that these parasites might have been released from the liver, which could have occurred 6–10 days earlier [37] and then could have been selected by residual low-level QN pressure. It is also possible that the parasites that appeared at day 14 were indeed present at day 0, although at levels undetectable even by nested PCR. QN might have cleared the highly susceptible parasites, while parasites with decreased susceptibility or, possibly, those that were metabolically quiescent could have recovered in numbers to become detectable at day 14 or beyond. This is supported by our observation that, when QN was administered for a longer period, the rate of recurrent parasitemia decreased and the time to patent parasitemia increased. We note that no QN was detectable by HPLC at day 14. This is consistent with results of mathematical models [38] and with our previous observations, in which pyrimethamine treatment selected DHFR mutant parasites within weeks, although these parasites were undetectable at day 0 [39], as well as with studies performed in Malawi, where the pfcrt 76T codon was not detected by conventional nested PCR but was detected in 25% of subjects by a heteroduplex tracking assay [40].
The observed efficacy of QN (after molecular correction to distinguish new infections) is consistent with several other reports reviewed by Okombo et al [24]. However, overall, 49.7% of 163 patients had a patent infection during the 28–day follow–up, which is comparable to the failure rate observed in other studies, using a similar treatment dose of 30 mg/day in 3 doses for 5 days [4, 41]. The rate of reinfection on day 14 justified the change of treatment duration from 5 to 7 days, which not only decreased the rate of recurrent parasitemia but also increased the time to patent parasitemia by 5 days. Thus, as previously shown, treatment duration is important in QN's in vivo efficacy [42].
We found that the uncorrected ACPR after QN treatment was 50.3%. These parasites may represent new infections from novel mosquito bites in these settings of intense malaria transmission. As discussed above, these parasites may also be new blood-stage organisms emerging from the liver. In either case, the fact that half of the patients would be sent home with impending parasitemia is of public health concern. This is consistent with several previous reports and supports the current recommendation of intravenous artesunate for the management of severe malaria [43–45]. In areas where intravenous artesunate is not available, QN treatment should be followed with a full course of an artemisinin combination therapy before discharge from the hospital. Alternatively, a drug that kills liver-stage parasites may be a good adjunct to QN therapy.
As shown in several other recent field studies [17, 22, 24, 32, 34, 46], in addition to 6 of the 8 pfnhe–1 microsatellites described by Ferdig et al [18], we discovered 10 novel microsatellites randomly distributed before and after the QN treatment. This confirms the high diversity of P. falciparum in Malian settings. ms4760-3 was the most represented microsatellite in our samples before QN treatment, followed by ms4760-1 and ms4760-7, whereas ms4760-2 and ms4760-4 were not found in this study. Other types, including the new ones, were all in low frequencies. This observation is similar to the East Africa ms4760 profile [18, 24, 34], while the Asian setting harbors mainly ms4760-7 [18, 35]. This diversity in ms4760 in the 2 villages in Mali was not affected by QN treatment. The significance of the counterselection of ms4760–3 by QN treatment was not known.
A few studies [14, 15, 21] have implicated pfcrt and/or an interaction between pfcrt and ms4760–1 in the phenotype of decreased susceptibility of P. falciparum to QN. We found no selection of pfcrt by QN treatment in vivo, although a trend for an increase in the ms4760–1 + pfcrt76T haplotype was noted. This trend did not reach statistical significance. The role of “ms4760–1 + pfcrt 76T” in QN resistance in the field needs further investigation in larger studies.
Although QN treatment selected pfnhe–1 ms4760–1, one might ask whether this microsatellite could be used as a molecular marker for QN resistance. We found that patients who presented with ms4760–1 at day 0 were nearly 2–fold more likely to have a recurring parasitemia after QN treatment, but the confidence interval was too wide for the association to reach statistical significance, probably because of the relatively small sample size. This comparatively small scale of the study was due to the logistic difficulties associated to the performance of these types of in vivo field studies. First, QN is only indicated for severe malaria, which is an unusual event [45]. Second, because of the need for multiple samples, for ethical reasons we could only include patients who were ill enough to warrant QN treatment but not too severely ill to undergo the study procedures. These difficulties are reflected in the fact that it took approximately 4 years to include 169 suitable cases in this study. Finally, to avoid alterations of the parasite population by culture adaptation, we performed direct sequencing of PCR products from blood samples collected directly from the patients, and nearly 23% of the 236 samples indicated mixed infections and did not yield usable sequences. Apart from the obvious difficulties, our study warrants the future conduct of similar but larger studies. Such studies are necessary for confirming the present observation and allow the pooling of data (eg, in the context of the WWARN initiative) for the full assessment of the role suggested here of ms4760–1 as a molecular marker of QN resistance.
In conclusion, our study is the first to demonstrate the selection of pfnhe–1 ms4760–1 by QN treatment in vivo and supports an important role for this locus in QN resistance in the field.
Notes
Acknowledgments. We thank the villages of Kollé and Faladié, Mali; the Laboratoire de Pharmacologie Analytique et Pharmacocinétique, Hôpital Saint–Vincent de Paul, Paris France, for assistance with the QN pharmacokinetics analyses; and NIAID intramural editor Brenda Rae Marshall, for assistance.
Financial support. This work was supported by the Howard Hughes Medical Institute International Scholarship (grant 55005502 to A. A. D.), by the Intramural Research Program of the Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Institutes of Health, and by European and Developing Countries Clinical Trials Partnership (EDCTP IP_07_31060_002).
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Peters W. Plasmodium: resistance to antimalarial drugs. Ann Parasitol Hum Comp. 1990;65(Suppl 1):103–6. doi: 10.1051/parasite/1990651103. [DOI] [PubMed] [Google Scholar]
- 2.Baird JK. Effectiveness of antimalarial drugs. N Engl J Med. 2005;352:1565–77. doi: 10.1056/NEJMra043207. [DOI] [PubMed] [Google Scholar]
- 3.Wongsrichanalai C, Pickard AL, Wernsdorfer WH, Meshnick SR. Epidemiology of drug–resistant malaria. Lancet Infect Dis. 2002;2:209–18. doi: 10.1016/s1473-3099(02)00239-6. [DOI] [PubMed] [Google Scholar]
- 4.Sabchareon A, Chongsuphajaisiddhi T, Attanath P. Serum quinine concentrations following the initial dose in children with falciparum malaria. SE Asian J Trop Med Public Health. 1982;13:556–62. [PubMed] [Google Scholar]
- 5.Shann F, Stace J, Edstein M. Pharmacokinetics of quinine in children. J Pediatr. 1985;106:506–10. doi: 10.1016/s0022-3476(85)80692-2. [DOI] [PubMed] [Google Scholar]
- 6.Neiva A. Development of malaria hematozoa resistant to quinine [in Portuguese, 1910] R Mem Inst Oswaldo Cruz. 1987;82:303–9. [PubMed] [Google Scholar]
- 7.Nocht BaWH. Beobachtungen über relative chininresistenz bei malaria aus Brasilien. Deutsch MedWschr. 1910;36:1557–60. [Google Scholar]
- 8.Bjorkman A, Phillips–Howard PA. The epidemiology of drug–resistant malaria. Trans R Soc Trop Med Hyg. 1990;84:177–80. doi: 10.1016/0035-9203(90)90246-b. [DOI] [PubMed] [Google Scholar]
- 9.Peters W. How to prevent malaria. Trop Doct. 1987;17:1–3. doi: 10.1177/004947558701700101. [DOI] [PubMed] [Google Scholar]
- 10.Giboda M, Denis MB. Response of Kampuchean strains of Plasmodium falciparum to antimalarials: in–vivo assessment of quinine and quinine plus tetracycline; multiple drug resistance in vitro. J Trop Med Hyg. 1988;91:205–11. [PubMed] [Google Scholar]
- 11.Pukrittayakamee S, Supanaranond W, Looareesuwan S, Vanijanonta S, White NJ. Quinine in severe falciparum malaria: evidence of declining efficacy in Thailand. Trans R Soc Trop Med Hyg. 1994;88:324–7. doi: 10.1016/0035-9203(94)90102-3. [DOI] [PubMed] [Google Scholar]
- 12.Adam I, Idris HM, Mohamed–Ali AA, Aelbasit IA, Elbashir MI. Comparison of intramuscular artemether and intravenous quinine in the treatment of Sudanese children with severe falciparum malaria. East Afr Med J. 2002;79:621–5. doi: 10.4314/eamj.v79i12.8668. [DOI] [PubMed] [Google Scholar]
- 13.Adam I, Ali DM, Noureldien W, Elbashir MI. Quinine for the treatment of chloroquine–resistant Plasmodium falciparum malaria in pregnant and non–pregnant Sudanese women. Ann Trop Med Parasitol. 2005;99:427–9. doi: 10.1179/136485905X36217. [DOI] [PubMed] [Google Scholar]
- 14.Cooper RA, Ferdig MT, Su XZ, et al. Alternative mutations at position 76 of the vacuolar transmembrane protein PfCRT are associated with chloroquine resistance and unique stereospecific quinine and quinidine responses in Plasmodium falciparum. Mol Pharmacol. 2002;61:35–42. doi: 10.1124/mol.61.1.35. [DOI] [PubMed] [Google Scholar]
- 15.Mu J, Ferdig MT, Feng X, et al. Multiple transporters associated with malaria parasite responses to chloroquine and quinine. Mol Microbiol. 2003;49:977–89. doi: 10.1046/j.1365-2958.2003.03627.x. [DOI] [PubMed] [Google Scholar]
- 16.Henry M, Briolant S, Zettor A, et al. Plasmodium falciparum Na+/H+ exchanger 1 transporter is involved in reduced susceptibility to quinine. Antimicrob Agents Chemother. 2009;53:1926–30. doi: 10.1128/AAC.01243-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bennett TN, Patel J, Ferdig MT, Roepe PD. Plasmodium falciparum Na+/H+ exchanger activity and quinine resistance. Mol Biochem Parasitol. 2007;153:48–58. doi: 10.1016/j.molbiopara.2007.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ferdig MT, Cooper RA, Mu J, et al. Dissecting the loci of low–level quinine resistance in malaria parasites. Mol Microbiol. 2004;52:985–97. doi: 10.1111/j.1365-2958.2004.04035.x. [DOI] [PubMed] [Google Scholar]
- 19.Wellems TE, Panton LJ, Gluzman IY, et al. Chloroquine resistance not linked to mdr–like genes in a Plasmodium falciparum cross. Nature. 1990;345:253–5. doi: 10.1038/345253a0. [DOI] [PubMed] [Google Scholar]
- 20.Nkrumah LJ, Riegelhaupt PM, Moura P, et al. Probing the multifactorial basis of Plasmodium falciparum quinine resistance: evidence for a strain–specific contribution of the sodium–proton exchanger PfNHE. Mol Biochem Parasitol. 2009;J165:122–31. doi: 10.1016/j.molbiopara.2009.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ursing J, Zakeri S, Gil JP, Bjorkman A. Quinoline resistance associated polymorphisms in the pfcrt, pfmdr1 and pfmrp genes of Plasmodium falciparum in Iran. Acta Trop. 2006;97:352–6. doi: 10.1016/j.actatropica.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 22.Sinou V, Quang LH, Pelleau S, et al. Polymorphism of Plasmodium falciparum Na+/H+ exchanger is indicative of a low in vitro quinine susceptibility in isolates from Viet Nam. Malar J. 2011;10:164. doi: 10.1186/1475-2875-10-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Briolant S, Pelleau S, Bogreau H, et al. In vitro susceptibility to quinine and microsatellite variations of the Plasmodium falciparum Na+/H+ exchanger (Pfnhe–1) gene: the absence of association in clinical isolates from the Republic of Congo. Malar J. 2011;10:37. doi: 10.1186/1475-2875-10-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Okombo J, Kiara SM, Rono J, et al. In vitro activities of quinine and other antimalarials and pfnhe polymorphisms in Plasmodium isolates from Kenya. Antimicrob Agents Chemother. 2010;54:3302–7. doi: 10.1128/AAC.00325-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.World Health Organization. Assessment of therapeutic efficacy of antimalarial drugs for uncomplicated falciparum malaria. Geneva: World Health Organization 2003; WHO/HTM/ RBM/2003.50. [Google Scholar]
- 26.Plowe CV, Doumbo OK, Djimde A, et al. Chloroquine treatment of uncomplicated Plasmodium falciparum malaria in Mali: parasitologic resistance versus therapeutic efficacy. Am J Trop Med Hyg. 2001;64:242–6. doi: 10.4269/ajtmh.2001.64.242. [DOI] [PubMed] [Google Scholar]
- 27.Tekete M, Djimde AA, Beavogui AH, et al. Efficacy of chloroquine, amodiaquine and sulphadoxine–pyrimethamine for the treatment of uncomplicated falciparum malaria: revisiting molecular markers in an area of emerging AQ and SP resistance in Mali. Malar J. 2009;8:34. doi: 10.1186/1475-2875-8-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Long GW, Fries L, Watt GH, Hoffman SL. Polymerase chain reaction amplification from Plasmodium falciparum on dried blood spots. Am J Trop Med Hyg. 1995;52:344–6. doi: 10.4269/ajtmh.1995.52.344. [DOI] [PubMed] [Google Scholar]
- 29.Cheng Q, Lawrence G, Reed C, et al. Measurement of Plasmodium falciparum growth rates in vivo: a test of malaria vaccines. Am J Trop Med Hyg. 1997;57:495–500. doi: 10.4269/ajtmh.1997.57.495. [DOI] [PubMed] [Google Scholar]
- 30.Su X, Wellems TE. Toward a high–resolution Plasmodium falciparum linkage map: polymorphic markers from hundreds of simple sequence repeats. Genomics. 1996;33:430–44. doi: 10.1006/geno.1996.0218. [DOI] [PubMed] [Google Scholar]
- 31.Djimde A, Doumbo OK, Cortese JF, et al. A molecular marker for chloroquine–resistant falciparum malaria. N Engl J Med. 2001;344:257–63. doi: 10.1056/NEJM200101253440403. [DOI] [PubMed] [Google Scholar]
- 32.Andriantsoanirina V, Menard D, Rabearimanana S, et al. Association of microsatellite variations of Plasmodium falciparum Na+/H+ exchanger (Pfnhe–1) gene with reduced in vitro susceptibility to quinine: lack of confirmation in clinical isolates from Africa. Am J Trop Med Hyg. 2010;82:782–7. doi: 10.4269/ajtmh.2010.09-0327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pelleau S, Bertaux L, Briolant S, et al. Differential association of Plasmodium falciparum Na+/H+ exchanger polymorphism and quinine responses in field– and culture–adapted isolates of Plasmodium falciparum. Antimicrob Agents Chemother. 2011;55:5834–41. doi: 10.1128/AAC.00477-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Baliraine FN, Nsobya SL, Achan J, et al. Limited ability of Plasmodium falciparum pfcrt, pfmdr1, and pfnhe1 polymorphisms to predict quinine in vitro sensitivity or clinical effectiveness in Uganda. Antimicrob Agents Chemother. 2011;55:615–22. doi: 10.1128/AAC.00954-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Poyomtip T, Suwandittakul N, Sitthichot N, Khositnithikul R, Tan–Ariya P, Mungthin M. Polymorphisms of the pfmdr1 but not the pfnhe–1 gene is associated with in vitro quinine sensitivity in Thai isolates of Plasmodium falciparum. Malar J. 2012;11:7. doi: 10.1186/1475-2875-11-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pradines B, Bertaux L, Pomares C, Delaunay P, Marty P. Reduced in vitro susceptibility to artemisinin derivatives associated with multi–resistance in a traveller returning from South–East Asia. Malar J. 2011;10:268. doi: 10.1186/1475-2875-10-268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hastings IM, Ward SA. Coartem (artemether–lumefantrine) in Africa: the beginning of the end? J Infect Dis. 2005;192:1303–4. doi: 10.1086/432554. [DOI] [PubMed] [Google Scholar]
- 38.Stepniewska K, Chotivanich K, Brockman A, Day NP, White NJ. Overestimating resistance in field testing of malaria parasites: simple methods for estimating high EC50 values using a Bayesian approach. Malar J. 2007;6:4. doi: 10.1186/1475-2875-6-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Plowe CV, Djimde A, Wellems TE, Diop S, Kouriba B, Doumbo OK. Community pyrimethamine–sulfadoxine use and prevalence of resistant Plasmodium falciparum genotypes in Mali: a model for deterring resistance. Am J Trop Med Hyg. 1996;55:467–71. doi: 10.4269/ajtmh.1996.55.467. [DOI] [PubMed] [Google Scholar]
- 40.Juliano JJ, Kwiek JJ, Cappell K, Mwapasa V, Meshnick SR. Minority–variant pfcrt K76T mutations and chloroquine resistance, Malawi. Emerg Infect Dis. 2007;13:872–7. doi: 10.3201/eid1306.061182. [DOI] [PubMed] [Google Scholar]
- 41.Achidi EA, Ajua A, Kimbi HK, Sinju CM. In vivo efficacy study of quinine sulphate in the treatment of uncomplicated P. falciparum malaria in patients from Southwestern Cameroon. East Afr Med J. 2005;82:181–5. doi: 10.4314/eamj.v82i4.9278. [DOI] [PubMed] [Google Scholar]
- 42.Clain J, Peytavin G, Gachot B, Vachon F, Le BJ. Optimum quinine therapy in falciparum malaria attacks contracted in Africa. Bull Soc Pathol Exot. 1997;90:260–2. [PubMed] [Google Scholar]
- 43.Kremsner PG, Taylor T, Issifou S, et al. A simplified intravenous artesunate regimen for severe malaria. J Infect Dis. 2012;205:312–9. doi: 10.1093/infdis/jir724. [DOI] [PubMed] [Google Scholar]
- 44.Krudsood S, Wilairatana P, Vannaphan S, et al. Clinical experience with intravenous quinine, intramuscular artemether and intravenous artesunate for the treatment of severe malaria in Thailand. SE Asian J Trop Med Public Health. 2003;34:54–61. [PMC free article] [PubMed] [Google Scholar]
- 45.Marsh K. Malaria—a neglected disease? Parasitology. 1992;104(Suppl):S53–S69. doi: 10.1017/s0031182000075247. [DOI] [PubMed] [Google Scholar]
- 46.Vinayak S, Alam MT, Upadhyay M, et al. Extensive genetic diversity in the Plasmodium falciparum Na+/H+ exchanger 1 transporter protein implicated in quinine resistance. Antimicrob Agents Chemother. 2007;51:4508–11. doi: 10.1128/AAC.00317-07. [DOI] [PMC free article] [PubMed] [Google Scholar]