Abstract
Background:
Complete rupture of the distal tendon of the biceps brachii is relatively rare and there is little information to guide therapists in rehabilitation after this injury. The purposes of this case report are to review the rehabilitation concepts used for treating such an injury, and discuss how to modify exercises during rehabilitation based on patient progression while adhering to physician recommended guidelines and standard treatment protocols.
Case Presentation:
The patient was an active 38‐year old male experienced in weight‐training. He presented with a surgically repaired right distal biceps tendon following an accident on a trampoline adapted with a bungee suspension harness. The intervention focused on restoring range of motion and strengthening of the supporting muscles of the upper extremity without placing undue stress on the biceps brachii.
Outcomes:
The patient was able to progress from a moderate restriction in ROM to full AROM two weeks ahead of the physician's post‐operative orders and initiate a re‐strengthening protocol by the eighth week of rehabilitation. At the eighth post‐operative week the patient reported no deficits in functional abilities throughout his normal daily activities with his affected upper extremity.
Discussion:
The results of this case report strengthen current knowledge regarding physical therapy treatment for a distal biceps tendon repair while at the same time providing new insights for future protocol considerations in active individuals. Most current protocols do not advocate aggressive stretching, AROM, or strengthening of a surgically repaired biceps tendon early in the rehabilitation process due to the fear of a re‐rupture. In the opinion of the authors, if full AROM can be achieved before the 6th week of rehabilitation, initiating a slow transition into light strengthening of the biceps brachii may be possible.
Level of evidence:
4‐Single Case report
Keywords: Distal biceps tendon surgical repair, rehabilitation guidelines
BACKGROUND AND PURPOSE
Complete rupture of the distal tendon of the biceps brachii is relatively rare and there is little information to guide therapists in rehabilitation after this injury and subsequent surgical repair. A regimented physical rehabilitation program of resistance training and stretching is warranted for patients who sustain a distal biceps tendon rupture and undergo surgical reattachment of the tendon. In the opinion of the authors, such a protocol may be effective in promoting full recovery and return to functional and athletic activities.
Complete rupture of the distal biceps brachii accounts for approximately 3% of all biceps ruptures (the long head ruptures account for 96% and the short head 1%).1 The loss of function from a distal biceps tendon rupture is substantial secondary to the total loss of torque produced by the biceps brachii resulting in decreased strength in elbow flexion and supination, and recovery can be slow.2 Therapists and other exercise professionals need to be aware of the best practices following this injury. The most common mechanism of injury is a single unanticipated load placed on the elbow joint while in a flexed position.2 An audible “pop” is usually heard followed by an visually observable abnormal contour of the upper arm.3 In almost all cases, conservative treatment without surgical reattachment of the distal tendon to the radial tuberosity has been shown to leave patients with markedly decreased muscular strength and endurance of forearm supination and elbow flexion.4,5 Therefore, immediate surgical repair is the recommended course of action. However delayed surgical treatment (3 weeks to 5 months after diagnosis) has been shown to be equally beneficial in long term follow‐up results when compared to patients treated early (within 8 days of initial injury).6
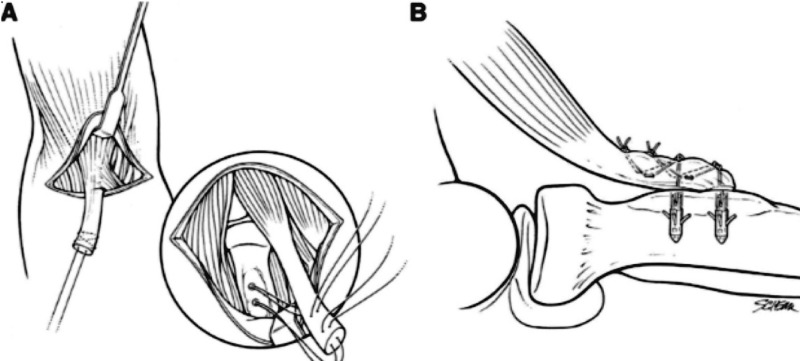
The biceps brachii is the main flexor at the elbow joint and a powerful supinator when the elbow is in a flexed position.7 It also aids with shoulder flexion, stabilization of the humeral head during deltoid contraction, and can assist in abduction and internal rotation of the humerus.7 Proximally, the long head of the biceps originates at the supraglenoid tubercle of the scapula and the short head from the coracoid process of the scapula.7 Distally, the biceps inserts on the radial tuberosity and via the bicipital aponeurosis (Figure 1).12
Figure 1.
Anatomy of the biceps brachii. Note the distal attachment to the radial head via the biciptial aponeurosis. Used with permission from The Journal of Hand Surgery.
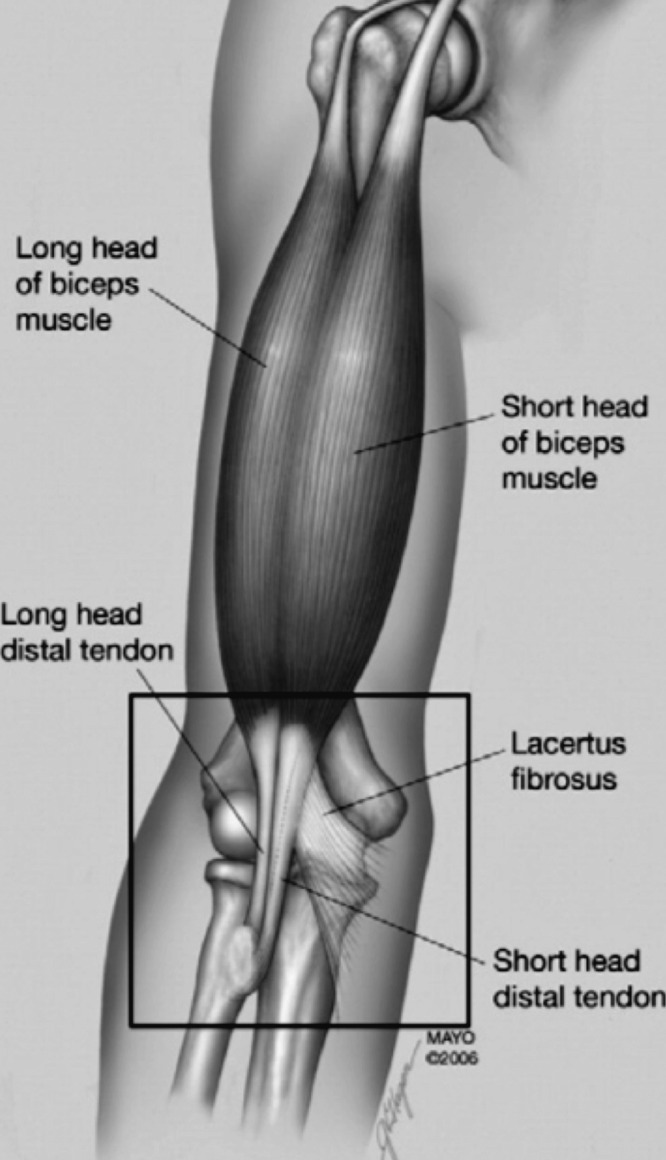
The two types of surgical procedures commonly used are the single‐incision technique and the double‐incision technique (Figures 2 and 3).8,9 Numerous studies have been performed examining the different methods of surgical repair of the distal biceps brachii tendon tear as well as long term results of operative vs. non‐operative treatments in terms of strength and range of motion (ROM) recovery.2,9,10 Younger patients with higher activity levels demonstrate improved recovery of ROM as compared to similar injuries sustained by those in an elderly population, yet there is limited information available to guide therapists and other exercise professionals with regard to strengthening of the muscle post‐surgery.5,6 In early rehabilitation, strengthening exercises (which stress the suture anchor) have commonly been prohibited due to fear of re‐rupturing the tendon. Although new surgical techniques are being developed that have demonstrated the ability for surgically repaired tendons to withstand higher loads prior to failure, recommendations for the introduction of strengthening exercises post‐surgery have not been modified to reflect these surgical advances.11 For example, Heinzelmann et al recently found that repair of a distal biceps tendon rupture with use of a soft tissue button and interference screw technique through a limited anterior incision can allow for a greater repair strength, thus allowing for earlier aggressive rehabilitation such as a progression to light pain‐free strengthening at only 2 weeks postoperative.12
Figure 2.
Single‐incision technique for distal biceps tendon repair. Used with permission from The Journal of Shoulder and Elbow Surgery.
Figure 3.
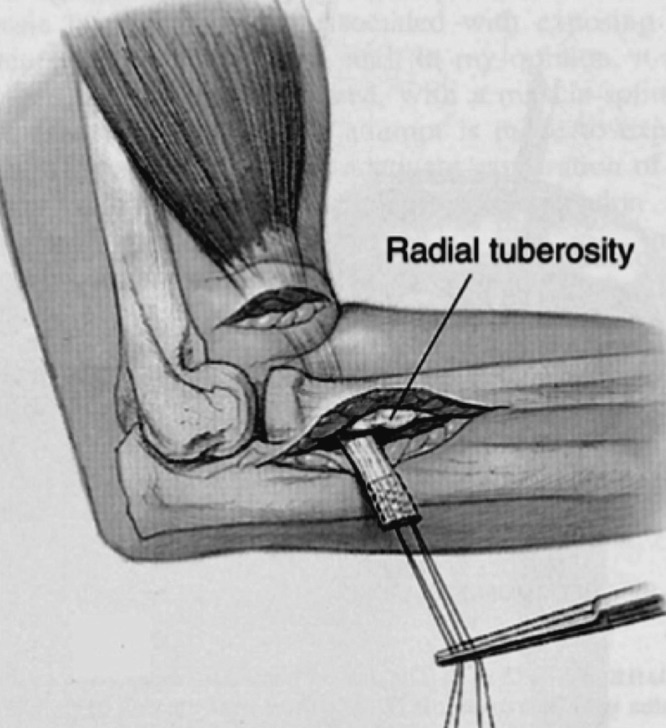
Double‐incision technique for distal biceps tendon repair. Used with permission from The Elbow and Its Disorders. Copyright Elsevier (2000).
Rehabilitation of a surgically repaired distal biceps tendon typically follows two phases: first immobilization, either with a cast or hinged brace, in order to limit full motion for the first 6 postoperative weeks, and a second phase that focuses on strengthening the atrophied muscles and eventual return to functional activities.3 In a retrospective review of 113 patients who underwent therapy for distal biceps repairs, Cheung et al reported that by increasing ROM through the use of a hinged brace with an extension restriction originally set at 60° of flexion and decreasing 20° every two weeks, full extension was achieved by week six, with strengthening of the biceps starting during the eighth week.13 More conservative treatment protocols have documented placing the injured extremity in a cast for six weeks, with restrictions on active stretching even at the 12th post‐operative week, and a strengthening phase initiated only at the 16th post‐operative week.3 There is little information on more aggressive rehabilitation protocols for this type of surgery. The descriptions of the treatments described in this case report may help guide physical therapists in the rehabilitation of a patient with a ruptured distal biceps brachii tendon that has been surgically repaired.
The purposes of this case report are to: 1) present the rehabilitation protocol used with an individual with a surgically repaired ruptured distal biceps tendon, 2) review the rehabilitation concepts used for developing the protocol for treating such an injury, and 3) discuss how to modify exercises during the rehabilitation process based on patient progression while still adhering to the physician recommended guidelines.
Case Description: Patient History
The patient was an active, 38‐year old male who participated regularly in resistance training. He underwent surgical repair of the right distal biceps tendon following an accident on a trampoline adapted with a bungee suspension harness. While in the ascending phase of his jump, the patient held on too tightly to the trampoline bungee cords attached to the harness causing his right upper extremity to forcibly abduct resulting in an extension torque at his elbow joint against the elbow being held in flexion. This mechanism of injury resulted in a eccentric overload on the distal biceps muscle tendon causing it to tear away from the insertion at the radial tuberosity. The patient described hearing a “popping” sound followed by sudden sharp and severe pain. Magnetic resonance imaging (MRI) of the upper extremity revealed complete rupture of the distal biceps brachii. Surgery was performed 15 days after the initial injury using a single‐incision technique. Informed consent was given by the patient to be presented in this publication
Clinical Impression #1
Prior to the injury the patient was highly active, participating in resistance training exercise 4‐5 times a week. Following the injury, his goal was to return to his previous exercise schedule. Based on his history, mechanism of injury, and the level of invasiveness with the surgical procedure to reattach the biceps tendon, the authors anticipated that he might ‐demonstrate severe limitations in elbow joint ROM accompanied with high levels of pain. Based on subsequent observations, the initial plan for examination included assessment of ROM and pain levels with a verbal numeric rating scale (NRS) and no manual muscle testing (MMT) per physician orders.
Examination
The patient presented with the right upper extremity in a brace, locked at 90° of elbow flexion (Figure 4).14 Physician orders at the time called for no active flexion of the elbow or supination at the forearm. Review of the patient's history indicated no previous musculoskeletal injuries to the upper extremities and no major cardiopulmonary, integumentary, neuromuscular, or other medical issues that might impede recovery or participation in rehabilitation. Physical examination of the injured region revealed a visible and palpable deformity of the biceps brachii muscle belly, primarily in the distal region, with a small scar in the right antecubital fossa where the biceps tendon had been surgically reattached. The scar was approximately three cm in length and was healing well without any signs of infection.
Figure 4.

Immobilization hinged brace for the elbow joint. Specific brace shown is a Mackie Elbow Brace. Photograph used with permission from Ortho Innovations.
Active range of motion (AROM) was assessed bilaterally with a standard (universal) goniometer.15 AROM of the right (involved) elbow joint into flexion and extension revealed dramatic decreases when compared to the contralateral side, with pain of 3/10 reported using the NRS that occurred at the end of his range of motion (Table 1).16,17 At the time of the initial evaluation, no MMT's were performed due to physician prescribed precautions. Elbow joint mobility presented with major restrictions. A restricted end‐feel was found with arthrokinematic assessment in the humeroulnar, humeroradial, superior radioulnar and inferior radioulnar motions.
Table 1.
Initial evaluation measurements. Note all measurements are active range
| Motion | Right Upper Extremity | Left Upper Extremity |
|---|---|---|
| Flexion | 130 deg | 150 deg |
| Extension | 35 deg flexion | Odeg |
| Supination | 85 deg | 90 deg |
| Pronation | 50 deg | 90 deg |
deg= degrees of active range of motion
Clinical Impression #2
Based on the physical examination, pervious level of functioning and past literature evidence it was evident hypothesized that if full AROM could be regained the patient would have minimal difficulties in returning to his previous level of activity including heavy resistance training. Per physician orders, exercises that actively contracted the biceps muscle were prohibited until the eighth week of rehabilitation.
Intervention
Initially interventions were focused on restoring range of motion using PROM, stretching, and grades three and four joint mobilizations, along with devising exercises to strengthen supporting scapular stabilizing muscles of the upper extremity without placing undue stress on the biceps brachii. (Figure 5) Range of motion was assessed actively and passively every one to two weeks.
Figure 5.
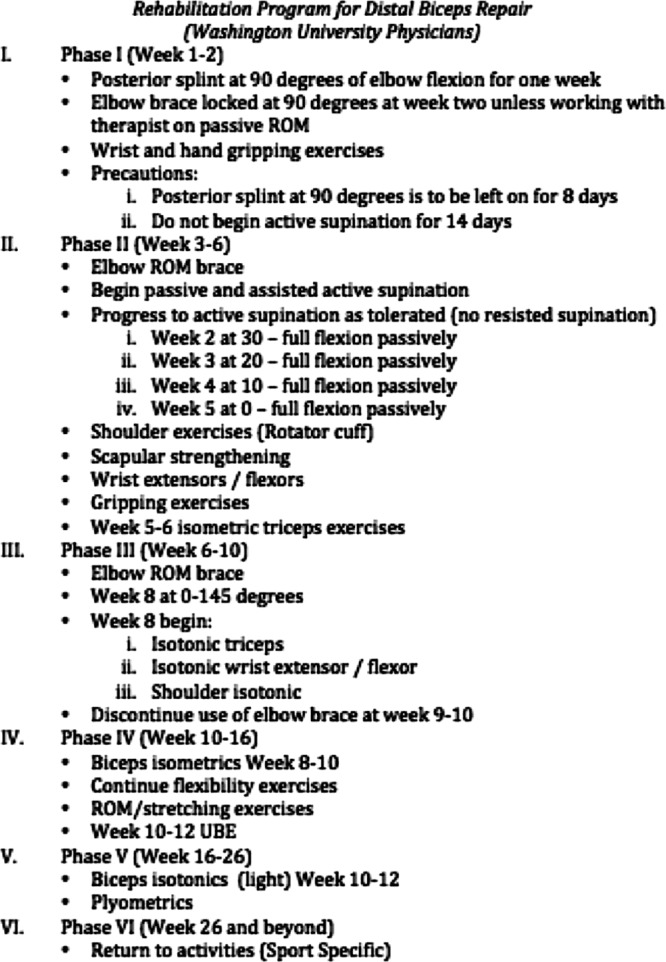
Suggested rehabilitation program protocol for distal biceps repair. Note the protocol includes specific phases of rehabilitation starting from the acute post‐surgery phase, extending to the return‐to‐play period.
After the first two weeks of physical therapy the patient reported no increase in soreness. Appendix 1 presents the rehabilitation protocol used with this patient. He also was compliant with a home exercise program (HEP) of AROM exercises of the elbow, shoulder, and forearm similar to those performed in the clinic. Exercises were to be performed at home in all planes of movement for three sets of twenty repetitions to end range of motion, three times daily. Currently available rehabilitation protocols limit active contraction of the biceps brachii muscle until weeks 8‐10 (Figure 5).4 In order to strengthen other muscles, such as the scapular and glenohumeral stabilizers (rhomboids, latissimus dorsi, middle trapezius, etc), an exercise was developed in which the patient bilaterally actively retracted his scapulae and extended his shoulders at the gleno‐humeral joint against elastic resistance (Figure 6). This exercise strengthens the scapular stabilizers without placing additional stress on the biceps brachii muscle. Low biceps activity during performance of this exercise was confirmed by manual palpation. Recent evidence has shown that biceps brachii electromyographic activity during scapular retraction has been measured to be less than 10% of maximal voluntary contraction.18 The patient was also placed seated on an exercise ball during the exercise in order to help increase abdominal and trunk muscle recruitment.
Figure 6.

Double thera‐band scapular retraction and shoulder extension. Note that the biceps brachii contraction is insignificant in this position allowing for strengthening of the scapular and gleno‐humeral stabilizers while still adhering to the specific physician protocol limiting active biceps strengthening until week 8 of rehabilitation.
At the end of week two, ROM was reassessed and demonstrated improvement when compared to baseline (Table 2). In addition, the patient's recovery of ROM was considered ahead of schedule, as the last measurement taken (5 degrees of flexion, or lacking 5 degrees from full extension) surpassed what the physician protocol had suggested by the beginning of week three (20 degrees of flexion) and week four (10 degrees of flexion). At week four, range of motion was assessed a third time. At this time, the patient had regained full passive extension without pain. Although the patient was still minimally limited in passive flexion, he was making a more rapid recovery than is typically observed.3,12,13
Table 2.
Patient active range of motion in extension. Note how the patients range of motion differed than that of the physician recommendations.
| Initial Examination | 2 Weeks | 4 Weeks | |
|---|---|---|---|
| Patient presentation | 35 deg of flexion | 5 deg of flexion | 0 |
| Physician Recommendations | X | 30 deg of flexion | 10 deg of flexion |
At post‐operative week 3 the patient began phase II of rehabilitation (weeks 3‐6), consisting of exercises that focused on strengthening supporting musculature including scapular stabilizers, shoulder rotator cuff, and forearm. The intensity of exercises already in the treatment protocol (Appendix 1) was gradually increased to progress toward complete recovery. At no time during the rehabilitation process did the patient experience any adverse reactions or increase in pain with any of the ROM or strengthening exercises.
After full AROM was achieved by week four, the authors determined that the patient was ready to initiate joint strengthening of the biceps muscle, however, physician orders prohibited this until the 8th week of rehabilitation (Figure 5). It was during weeks 8‐10 that exercises were added to strengthen the biceps brachii specifically using single joint exercises such as bicep curls or multi‐joint exercises such as the latissimus dorsi pull‐down. At the 8th week, the patient reported that he had full function with his extremity and had no deficits with any activities of daily living (ADL).
Outcomes and Discussion
Patients who sustain a distal biceps tendon rupture and who undergo surgical intervention for reattachment fully recover and return to both functional and athletic activities without limitations.3,15,19,20,21,22 In this case, the patient was able to fully recover AROM within 4 weeks and eventually return to strengthening exercises without limitations by the 8th week of rehabilitation (Appendix 1). The rate at which the patient's ROM normalized was faster than generally expected, and led the authors to implement newly devised exercises that enabled the patient to advance strengthening of supporting musculature of the upper back and shoulder girdle while limiting any contraindicated exercise or activity that involved the biceps. It could be that the patient was able to progress towards full extension ROM at a faster rate than previous protocols because of his history of advanced levels of physical activity and a high degree of motivation both of which are well known predictors for successful rehabilitation.3,4 Degree of physical activity level prior to injury has been shown to have a positive effect on rehabilitation potential and the level of post‐injury motion and strength potential should be considered when managing the treatment process.2 These, along with the patient's relatively young age may also have contributed to achieving rehabilitation outcomes ahead of schedule. Overall, this article is just a case report, and generalizations to other/all patients who have undergone distal biceps repairs cannot be made.
The authors believe that the results of this case report add to the current knowledge regarding physical therapy treatment for a distal biceps tendon repair while at the same time provide insights for future protocol considerations in active individuals. Most current protocols do not advocate aggressive stretching, AROM, or strengthening of a surgically repaired distal biceps tendon early in the rehabilitation process due to the fear of a re‐rupture. At this time the most information on aggressive early rehabilitation of the distal biceps repair has been provided by Cheung et al. They detail a progressive PROM protocol starting immediately and reaching full ROM by the sixth week.4 The patient in this case study, however, started AROM during week 1 and isotonic joint strengthening of the biceps at the start of week 8. The strengthening protocol described in the present report was consistent with the timeline of Cheung et al, but was more advanced than the physician orders prescribed (which indicated only isometric strengthening through weeks 8‐10 before the advancement to isotonic exercises).4 Conversely, both of these protocols are more aggressive than the highly conservative procedures detailed by Thompson in which the injured extremity was placed in a cast for six weeks, with no active stretching until the 12th week, and no strengthening until the 16th week post‐surgery.3
One factor that would have strengthened this case report would have been to document the return of strength in the patient's biceps brachii during the strengthening phase of the rehabilitation protocol as compared to his uninjured extremity. It would also have been beneficial to be able to detail the exact amount of HEP ROM exercises the patient actually performed, which most likely aided in his early recovery.
One concept that has not been investigated in the literature is the effect of strengthening exercises of the biceps (isometric or isotonic) early in the rehabilitation process, as soon as the patient can achieve full active ROM. Presently all published protocols for this particular surgery prohibit any strengthening until well into the eighth week or after. It is likely that these same protocols were not developed with the expectation that patients could recover full ROM by the end of the sixth week. In the opinion of the authors' if full AROM can be achieved before the sixth week of rehabilitation, initiating a slow transition into light strengthening of the biceps brachii may be safe for the patient and worth investigating. Future studies should evaluate the initiation of strengthening exercises when full AROM has been achieved in more patients.
CONCLUSION
The distal biceps brachii tendon rupture is a relatively rare injury and there is currently limited evidence available on rehabilitation techniques and guidelines for proper progression. In this case report, the rate at which the patient's ROM progressed during rehabilitation was faster than generally expected, and led the authors to implement newly devised exercises that enabled the patient to advance strengthening of supporting musculature of the upper back and shoulder girdle while limiting any contraindicated exercise or activity that involved the biceps. While the overall treatment plan did not differ significantly from the requested physician protocol, it is the authors' opinion that full AROM may be achieved before the sixth week of rehabilitation, and therefore, initiating a slow transition into light strengthening of the biceps brachii may be safe for patients and worth investigating with future research with larger numbers of subjects.
APPENDIX 1: INTERVENTION PROTOCOL USED WITH THE SUBJECT OF THE CASE REPORT
| Week 1 | Week 2 | Week 3 | Week 4 | Week 5‐6 | Week 8‐10 | |
|---|---|---|---|---|---|---|
| Elbow | AROM Ext: 2x10 (0 lbs) | AROM Ext: 2x10 (0 lbs) | AROM Ext: 2x10 (0 lbs) | AROM Ext: 2x10 (0 lbs) | AROM Ext: 2x10 (0 lbs) | AROM Ext: 2x10 (0 lbs) |
| Joint mobilizations as needed | PROM stretching ext/flex: 5x30 sec | PROM stretching ext/flex: 5x30 sec | PROM stretching ext/flex: 5x30 sec | PROM stretching ext/flex: 5x30 sec | PROM stretching ext/flex: 5x30 sec | |
| Joint mobiliza¬tions as needed | BOSU ‐ Push Up | |||||
| Bicep Curl ‐ 2x10 (4 lbs) | ||||||
| Tricep Extension ‐ 2x10 (10 lbs) | ||||||
| Forearm | Ext/Flex: 3x10 each direction (0 lbs) | Ext/Flex: 3x10 each direction (1 lbs) | Ext/Flex: 3x10 each direction (2 lbs) | Ext/Flex: 3x10 each direction (4 lbs) | Ext/Flex: 3x10 each direction (5 lbs) | Ext/Flex: 3x10 each direction (5 lbs) |
| Hammer radial/ulnar deviation: 3x10 each direction (0 lbs) | Hammer radial/ulnar deviation: 3x10 each direction (1 lbs) | Hammer radial/ulnar deviation: 3x10 each direction (2 lbs) | Hammer radial/ulnar deviation: 3x10 each direction (4 lbs) | Hammer radial/ulnar deviation: 3x10 each direction (5 lbs) | Hammer radial/ulnar deviation: 3x10 each direction (5 lbs) | |
| Shoulder | AROM flexion: 3x10 (Cane) | AROM flexion: 3x10 (1 lbs) | AROM flexion: 3x10 (1 lbs‐3 lbs) | AROM flexion: 3x10 (5 lbs) | AROM flexion: 3x10 (5 lbs) | AROM flexion: 3x10 (5 lbs) |
| Shoulder stretching in all directions (Flex, Abd, ER, IR): 5x30 seconds | Shoulder stretching in all directions (Flex, Abd, ER, IR): 5x30 seconds | Shoulder stretching in all directions (Flex, Abd, ER, IR): 5x30 seconds | Shoulder stretching in all directions (Flex, Abd, ER, IR): 5x30 seconds | Shoulder stretching in all directions (Flex, Abd, ER, IR): 5x30 seconds | Shoulder stretching in all directions (Flex, Abd, ER, IR): 5x30 seconds | |
| T‐Band Ext: x30 reps (Green Band) | T‐Band Ext: x30 reps (Green Band) | T‐Band Ext: x30 reps (Green Band) | ||||
| Shrugs: x30 reps (5 lbs) | Shrugs: x30 reps (8 lbs) | Shrugs: x30 reps (8 lbs) | ||||
| Prone Horiz. Abd: x30 reps (1 lbs) | Prone I‐T‐Y: x30 reps each direction (1 lbs) | |||||
| Prone Horiz. Abd: x30 reps (1 lbs) | Prone I‐T‐Y: x30 reps each direction (1 lbs) | |||||
| Standing Row: 5 lb bar | ||||||
| Lat Pulldown Machine: 3x10 (40 lbs) | ||||||
| Scapular Stabilizers | Scapular retraction double T‐Band on ball: 3x10 (Blue T‐Band resistance) | Scapular retrac¬tion double T‐Band on ball: 3x10 (Black T‐Band resistance) | Scapular retraction double T‐Band on ball: 3x10 (Silver T‐Band resistance) | Scapular retraction double T‐Band on ball: 3x10 (Silver T‐Band resistance) | Scapular retraction double T‐Band on ball: 3x10 (Silver T‐Band resistance) | Scapular retraction double T‐Band on ball: 3x10 (Silver T‐Band resistance) |
| Scapular retrac¬tion into exercise ball: 2x10 | Scapular retraction into exercise ball: 2x10 | Scapular retraction into exercise ball: 2x10 | Scapular retraction into exercise ball: 2x10 | Scapular retraction into exercise ball: 2x10 | ||
| Serratus punches in supine: x30 reps (2 lb weight) | Serratus punches in supine: x30 reps (4 lb weight) | Serratus punches in supine: x30 reps (5 lb weight) | Serratus punches in supine: x30 reps (5 lb weight) | Serratus punches in supine: x30 reps (5 lb weight) |
AROM = Active range of motion, PROM = Passive range of motion,lbs = pounds, Ext = Extension, Flex = Flexion, Abd = Abduction, ER = External IR = Internal rotation, T‐Band = Thera‐Band ®
REFERENCES
- 1.Gilcreest EL. (1933). Rupture of muscle and tendons, particularly subcutaneous rupture of the biceps flexor cubiti. JAMA. 84:1819‐1822 [Google Scholar]
- 2.Lintner S, Fischer T. (1996). Repair of the distal biceps tendon using suture anchors and an anterior approach. Clinical Orthopedics and Related Research. 322: 116‐119 [PubMed] [Google Scholar]
- 3.Thompson K, (1998). Rupture of the distal biceps tendon in a collegiate football player: A case report. Journal of Athletic Training. 33:62‐64 [PMC free article] [PubMed] [Google Scholar]
- 4.Athwal GS, Steinmann SP, Rispoli DM. (2007). The distal biceps tendon: footprint and relevant clinical anatomy. The Journal of Hand Surgery. 32A(8). [DOI] [PubMed] [Google Scholar]
- 5.Morrey B.F, Askew LJ, An KN, Dobyns JH. (1985). Rupture of the distal biceps brachii tendon. A biomechanical study. J Bone Joint Surg Am. 67: 418‐421 [PubMed] [Google Scholar]
- 6.Rantanen J, Orava S. (1999). Rupture of the distal biceps tendon. A report of 19 patients treated with anatomic reinsertion, and a meta‐analysis of 147 cases found in the literature. Am J Sports Med. 27:2:128‐132 [DOI] [PubMed] [Google Scholar]
- 7.Gilroy AM, MacPherson BR, Ross LM, (2008). Atlas of Anatomy. New York: Thieme Medical Publishers [Google Scholar]
- 8.Morrey BF. (2000). Injury of the flexors of the elbow: biceps in tendon injury. The elbow and its disorders. 3rd ed. Philadelphia, Pa: Saunders, 468‐478 [Google Scholar]
- 9.John CK, Field LD, Weiss KS, Savoie FH. (2007). Single‐incision repair of aute distal biceps ruptures by use of suture anchors. Journal of Shoulder and Elbow Surgery. 16(1). [DOI] [PubMed] [Google Scholar]
- 10.Hurov JR. (1996). Controlled active mobilization following surgical repair of the avulsed radial attachment of the biceps brachii muscle: A case report. JOSPT. 23 (6): 382‐387 [DOI] [PubMed] [Google Scholar]
- 11.Kettler M, Lunger J, Kuhn V, et al. (2007). Failure strengths in distal biceps tendon repair. Am J Sports Med. 35:1544‐1548 [DOI] [PubMed] [Google Scholar]
- 12.Heinzelmann AD, Savoie FH, Ramsey JR, et al. (2009). A combined technique for distal biceps repair using a soft tissue button and biotenodesis interference screw. Am J Sports Med 37:989. [DOI] [PubMed] [Google Scholar]
- 13.Cheung EV, Lazarus M, Taranta M. (2005). Immediate range of motion after the distal biceps tendon repair. J. Shoulder Elbow Surg. 14:516‐8 [DOI] [PubMed] [Google Scholar]
- 14.OrthoInnovations Mackie Elbow Brace. Available at http://www.orthoinnovations.com/mackieElbow.html Accessed on October 16th, 2011
- 15.Sethi PM, Tibone JE. (2008). Distal biceps repair using cortical button fixation. Sports Med Arthrosc Rev. 16: 130‐135 [DOI] [PubMed] [Google Scholar]
- 16.Li L, Liu X, Herr K. (2007). Postoperative pain intensity assessment: a comparison of four scales in Chinese adults. Pain Med. 8(3):223‐34 [DOI] [PubMed] [Google Scholar]
- 17.Stratford PW, Spadoni GF. (2001). The reliability, consistency, and clinical application of a numeric pain rating scale. Physiotherapy Canada, 51(2), 88‐91 [Google Scholar]
- 18.Smith J, Dahm DL, Kaufman KR, et al. (2006). Electromyographic activity in the immobilized shoulder girdle musculature during scapulothoracic exercises. Arch Phys Med Rehabil, 87:923‐7 [DOI] [PubMed] [Google Scholar]
- 19.Baker BD, Bierwagen D. (1985). Rupture of the distal biceps brachii; operative versus nonoperative treatment. J Bone Joint Sug Am. 67:414‐417 [PubMed] [Google Scholar]
- 20.D'Alessandro DR, Shields CL, Tibone JE, et al. (1993). Repair of distal biceps tendon repair in athletes. American Journal of Sports Medicine. 21:1: 114‐119 [DOI] [PubMed] [Google Scholar]
- 21.Lois DS, Hankin FM, Eckenrode JF, et al. (1986). Distal biceps brachii tendon avulsion. A simplified method of operative repair. The American Journal of Sports Medicine. 14:3. [DOI] [PubMed] [Google Scholar]
- 22.Rantanen J, Orava S. (1999). Rupture of the distal biceps tendon. A report of 19 patients treated with anatomic reinsertion, and a meta‐analysis of 147 cases found in the literature. Am J Sports Med. 27:2:128‐132 [DOI] [PubMed] [Google Scholar]