In many ways, the Dartmouth Atlas has put EOL care “on the map” of health care policy debates. It has proven an invaluable resource to those interested in examining patterns of health care utilization among elderly patients in the last two years of life. Most notably, the Dartmouth Atlas group has spearheaded research that has demonstrated dramatic regional variability1,2,3,4 in the health care provided to patients who have died. We applaud the creation of such a valuable data repository and consider the Dartmouth Atlas to be a remarkable tool for the promotion of an evidence-based evaluation of EOL care. We are also sympathetic with its mission – the reduction of unwarranted non-uniformities and inefficiencies in health care delivery to terminally ill patients. Like the Dartmouth Atlas authors, we share a concern about the growing number of patients who receive aggressive and extremely costly care near death.5,6,7,8,9
Nevertheless, the Dartmouth Atlas alone does not provide a detailed, comprehensive view of the terrain that would be required for a thorough examination of EOL care and the factors that influence it. It describes how medical resources are distributed and consumed across the United States at national, regional, and local levels. It also characterizes the aggressiveness of care provided within hospitals to Medicare patients in their final two years of life.4 Although it is true that there exist large variations in the intensity of EOL care that patients receive, we need to look beyond the regional supply of medical resources (e.g., number of ICU beds) for more complete explanations of why this is the case. Regional variation is part of the explanation, but we find that at least some, and perhaps considerably more, variance in the aggressiveness of EOL care is better attributed to micro-, psychosocial-level, factors than to macro-, regional- or health system-level, factors.
Several recent studies 9, 10,11,12,13,14,15,16,17,18 demonstrate that “demand-side” characteristics (e.g., patient race/ethnicity, age, health status, functional decline, prognostic understanding, treatment preferences, nearby and dependent family members, religious views, spiritual support by religious and medical communities, participation in EOL discussions) are highly significant predictors of aggressiveness of EOL care over and above the effects of the hospital or clinic or regional availability of medical resources in which the care was received. Research has shown that these demand-side characteristics explain more of the variance in geographic and ethnic disparities in the aggressiveness of care than do supply-side characteristics (e.g., hospital bed supply, teaching hospital status, number of medical specialists per capita). If psychosocial factors are powerful predictors of the aggressiveness of EOL care, particularly once health care system factors are taken into account, then greater attention needs to be paid to examining and, ultimately, intervening at the patient, family, and provider levels.
Curiously, in the report “Quality of End-of-Life Cancer Care for Medicare Beneficiaries Regional and Hospital-Specific Analyses”4 released November 16, 2010 on the Dartmouth Atlas website, the authors minimize the impact of patient treatment preferences that they do not actually assess. As stated in the introductory paragraph: “Even among the nation’s leading medical centers, there is no consistent pattern of care or evidence that treatment patterns follow patient preferences.” In the NCI-NIMH-funded prospective cohort “Coping with Cancer” study, we interviewed advanced cancer patients in some of the nation’s leading medical centers. Patient preferences were not only a significant determinant of the intensity of care patients received in the last week of their life, 18 but preferences had a more significant effect on the likelihood of receipt of aggressive EOL care (i.e., cardiopulmonary resuscitation and/or mechanical ventilation in the last week of life followed by death in an Intensive Care Unit) than did the medical center in which the patient received care. In fact, treatment site was not significantly associated with patients’ EOL medical care after adjustment for patients’ preferences, race/ethnicity, communication with physicians, and patients’ terminal illness acknowledgment.
It is true that only seven medical centers participated in the Coping with Cancer study. Still, academic and non-academic, urban, suburban and rural, safety-net hospitals and VA cancer centers in the Northeast and Southwest were represented. We in no way wish to imply that the Coping with Cancer data provide all the answers. They do not and are limited by the need for the inclusion of more geographic regions, hospitals, providers and patients, linkages with large administrative databases that account for medical resources used, as well as repeated assessments of patients and providers along the continuum of care. We are not claiming that Coping with Cancer should be considered the final word in determining the relative influence of patient versus regional/health care intensity factors in explaining the aggressiveness of EOL care a patient receives. What these results do reveal, however, is the need to pay closer attention to how patients and their family members influence medical care received near death – factors that the Dartmouth Atlas data alone do not assess and cannot examine.
Aside from asserting that a disconnect exists between patient preferences and the EOL care patients receive, the Dartmouth Atlas 2010 report claims that racial disparities in EOL care are primarily a function of regional variation in the supply of medical resources. The reference for this claim is a study by Barnato et al. in which Medicare beneficiaries were asked in telephone interviews about the care that they would hypothetically want if they were dying. In this report they state: “The observed relationship between respondents’ preferences for avoiding potentially life-shortening palliative drugs and greater spending regions was explained by the confounding effect of race/ethnicity.” 19 These findings contradict the conclusion of Baicker et al. that “Differences in end-of-life care are driven more by residence than by race… [and that] intensive EOL care [is] …driven primarily by the supply of providers.” 20 Again, this runs counter to the evidence derived from our Coping with Cancer study of racial disparities in EOL care.21,22 When we examine aggressive care in the last week of life, we find that the race of the patient is a highly significant predictor of aggressiveness of EOL care even after controlling for the region or hospital in which the patient was treated. Moreover, most of the black patients in Coping with Cancer who received aggressive EOL care did so at Parkland County Hospital – a hospital with a Dartmouth Health Care Intensity score of only 12.2 out of a possible 100. 23
Other studieshave alsofound that race/ethnic status, over and above the effects of regional medical resources, is among the strongest predictors of intensity of EOL care. Kelley et al.15 showed that patient-level factors such as race/ethnicity accounted for 10% of the variance in the intensity of EOL care. Not only did this proportion of variance remain stable after adjusting for geographic region, but geographic region accounted for only an additional 5% of the variance in the intensity of EOL care. Hardy et al. 17 has also reported that substantial ethnic disparities in hospice service use persist in analyses within urban and rural areas as well as within socioeconomic status levels. As a final example, Lackan et al. 24 in a multivariate, multilevel analysis of Californians aged 65 years and older (N = 472,382) demonstrated that race and ethnicity and immigrant status were highly significant predictors of death in a hospital inpatient unit, and these socio-demographic characteristics were at least as influential as hospital service area characteristics (e.g., the number of beds or physicians per 1000 persons). For these reasons, we take issue with the Dartmouth Atlas conclusions that intensity of EOL care is “driven more by residence than by race …[or] by the supply of providers”.20
If we are to identify the most important determinants of the intensity of EOL care, we need to integrate the Dartmouth Atlas data with more refined psychosocial assessments of actual, not hypothetical, terminally ill patients, their family members, and providers. Data from large, nationally representative and institutionally and geographically diverse administrative databases need to be linked to interviews with patients and their formal and informal caregivers, along with their health care providers, designed to assess pertinent psychological and social factors. Only then will we be able to determine both the level and the specific targets within each level, or even between each level (e.g., therapeutic alliance between patients and their providers), where interventions can have the greatest impact.
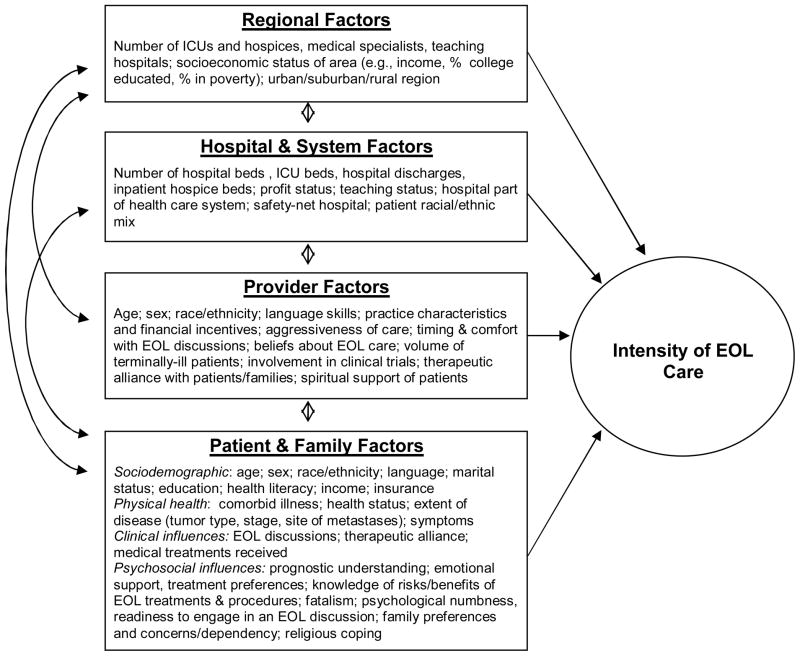
In order to identify non-uniformities, inefficiencies, and inequities in care, and to explain variation in the intensity of EOL care, researchers need to design studies to evaluate elements of the conceptual model we present below in Figure 1. In addition to regional and hospital and health care system factors, studies should assess health care provider, patient and family factors. Specifically, these would include measures of clinical communications, patient and family member treatment preferences, and values, acculturation, religious beliefs and prognostic understanding, knowledge of the pros and cons of treatment options, psychological adjustment, medical decision-making styles and therapeutic alliance of health care providers with patients and their family members.
Figure 1.
Conceptual model for examining influences on intensity of EOL care
Note: Figure 1 presents a conceptual framework for investigating influences on EOL outcomes such as intensity of EOL care. Hierarchical models are recommended to capture the associations of the factors on the left with EOL care; in general, the hierarchical structure has patient/families nested within physicians, nested within institutions and health systems, nested within regions. In addition to the factors on the left influencing EOL care and outcomes, they are related to each other as well. For example, patient and family factors influence the physicians seen, hospitals used, and the areas where one lives. Similarly, physicians often chose to work in certain hospitals or health systems and in certain areas. We do not consider this an exhaustive list of influences on EOL outcomes, but rather a conceptual model of the levels and relationships between these levels that should be factored into analyses.
As part of this agenda, we also recommend longitudinal, prospective cohort studies to determine outcomes/effectiveness of aggressive interventions in seriously ill patients. This would overcome one of the major limitations of the current Dartmouth Atlas Project data, which samples on the condition of death and thereby only allows investigators to perform retrospective examinations of the care of decedents. Patients who benefit from aggressive interventions and survive are not included in the Dartmouth Atlas data. A less biased sampling of terminally ill patients followed prospectively would permit a fairer test of the potential benefits of aggressive care.
In conclusion, the Dartmouth Atlas project has enabled giant strides forward in understanding the patterns of care received by deceased patients. Not only has it put EOL care on the health care policy map, but it has also placed burdensome, futile and costly EOL care at center stage in the health care reform debate. Nevertheless, without the inclusion of powerful psychosocial factors, the picture, and understanding, of determinants of intensity of EOL care will remain incomplete and the analysis superficial. The Dartmouth Atlas project has provided many of the broad strokes necessary to sketch the outlines of EOL care. We now need to “zoom in” and add psychosocial data to fill in missing details and enhance the resolution of the overall EOL care picture. Such data will support analyses that have more depth, precision, and completeness, and solidify the evidence-base from which informed policy to improve the quality of EOL care can be constructed.
References
- 1.Wennberg JE, Cooper MM, editors. The Dartmouth atlas of health care 1999. Chicago, IL: American Hospital Association Press; 1999. The quality of medical care in the United States: a report on the Medicare program. [PubMed] [Google Scholar]
- 2.Wennberg JE, Fisher ES, Stukel TA, Skinner JS, Sharp SM, Bronner KK. Use of hospitals, physician visits, and hospice care during the last six months of life among cohorts loyal to highly respected hospitals in the United States. BMJ. 2004;328:607. doi: 10.1136/bmj.328.7440.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fisher ES, Wennberg DE, Stukel DA, Gottlieb D, Lucas FL, Pinder E. The implications of regional variations in Medicare spending: part 1, utilization of services and the quality of care. Ann Intern Med. 2003;138:273–87. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- 4.Quality of End-of-Life Cancer Care for Medicare Beneficiaries Regional and Hospital-Specific Analyses. http://www.dartmouthatlas.org/downloads/reports/Cancer_report_11_16_10.pdf. [PubMed]
- 5.Earle CC, Neville BA, Landrum MB, et al. Trends in the aggressiveness of cancer care near the end of life. J Clin Oncol. 2004;22:315–21. doi: 10.1200/JCO.2004.08.136. [DOI] [PubMed] [Google Scholar]
- 6.Earle CC, Landrum MB, Souza JM, et al. Aggressiveness of cancer care near the end of life: is it a quality-of-care issue? J Clin Oncol. 2008;26:3860–3866. doi: 10.1200/JCO.2007.15.8253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Emanuel EJ, Young-Xu Y, Levinsky NG, et al. Chemotherapy use among Medicare beneficiaries at the end of life. Ann Intern Med. 2003;138:639–43. doi: 10.7326/0003-4819-138-8-200304150-00011. [DOI] [PubMed] [Google Scholar]
- 8.Temel JS, McCanon J, Greer JA, et al. Aggressiveness of care in a prospective cohort of patients with advanced NSCLC. Cancer. 2008;113:826–33. doi: 10.1002/cncr.23620. [DOI] [PubMed] [Google Scholar]
- 9.Zhang B, Wright AA, Huskamp HA, Nilsson ME, Maciejewski ML, Earle CC, Block SD, Maciejewski PK, Prigerson HG. Health care costs in the last week of life: associations with end-of-life conversations. Arch Intern Med. 2009;169:480–8. doi: 10.1001/archinternmed.2008.587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maciejewski PK, Phelps AC, Kacel EL, Balboni TA, Balboni M, Wright AA, Pirl W, Prigerson HG. Religious coping and behavioral disengagement: opposing influences on advance care planning and receipt of intensive care near death. Psychooncology. 2011 Mar 29; doi: 10.1002/pon.1967. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Balboni TA, Paulk ME, Balboni MJ, Phelps AC, Loggers ET, Wright AA, Block SD, Lewis EF, Peteet JR, Prigerson HG. Provision of spiritual care to patients with advanced cancer: associations with medical care and quality of life near death. J Clin Oncol. 2010;28:445–52. doi: 10.1200/JCO.2009.24.8005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wright AA, Zhang B, Ray A, Mack JW, Trice E, Balboni T, Mitchell SL, Jackson VA, Block SD, Maciejewski PK, Prigerson HG. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300:1665–73. doi: 10.1001/jama.300.14.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Parr JD, Zhang B, Nilsson ME, Wright A, Balboni T, Duthie E, Paulk E, Prigerson HG. The influence of age on the likelihood of receiving end-of-life care consistent with patient treatment preferences. J Palliat Med. 2010;13:719–26. doi: 10.1089/jpm.2009.0337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nilsson ME, Maciejewski PK, Zhang B, Wright AA, Trice ED, Muriel AC, Friedlander RJ, Fasciano KM, Block SD, Prigerson HG. Mental health, treatment preferences, advance care planning, location, and quality of death in advanced cancer patients with dependent children. Cancer. 2009;115:399–409. doi: 10.1002/cncr.24002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kelley AS, Ettner SL, Morrison RS, Du Q, Wenger NS, Sarkisian CA. Determinants of medical expenditures in the last 6 months of life. Ann Intern Med. 2011;154:235–42. doi: 10.7326/0003-4819-154-4-201102150-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zuckerman S, Waidmann T, Berenson R, Hadley J. Clarifying sources of geographic differences in Medicare spending. N Engl J Med. 2010;363:54–62. doi: 10.1056/NEJMsa0909253. [DOI] [PubMed] [Google Scholar]
- 17.Hardy D, Chan W, Liu CC, Cormier JN, Xia R, Bruera E, Du XL. Racial disparities in the use of hospice services according to geographic residence and socioeconomic status in an elderly cohort with nonsmall cell lung cancer. Cancer. 2011 Apr 1;117(7):1506–15. doi: 10.1002/cncr.25669. Epub 2010 Nov 8. [DOI] [PubMed] [Google Scholar]
- 18.Wright AA, Mack JW, Kritek PA, Balboni TA, Massaro AF, Matulonis UA, Block SD, Prigerson HG. Influence of patients’ preferences and treatment site on cancer patients’ end-of-life care. Cancer. 2010;116:4656–63. doi: 10.1002/cncr.25217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barnato AE, Herndon MB, Anthony DL, Gallagher PM, Skinner JS, Bynum JP, Fisher ES. Are regional variations in end-of-life care intensity explained by patient preferences?: A Study of the US Medicare Population. Med Care. 2007;45:386–93. doi: 10.1097/01.mlr.0000255248.79308.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baicker K, Chandra A, Skinner JS, Wennberg JE. Who you are and where you live: how race and geography affect the treatment of Medicare beneficiaries. Health Aff (Millwood) 2004:VAR33–44. doi: 10.1377/hlthaff.var.33. Suppl Web Exclusives. [DOI] [PubMed] [Google Scholar]
- 21.Loggers ET, Maciejewski PK, Paulk E, DeSanto-Madeya S, Nilsson M, Viswanath K, Wright AA, Balboni TA, Temel J, Stieglitz H, Block S, Prigerson HG. Racial differences in predictors of intensive end-of-life care in patients with advanced cancer. J Clin Oncol. 2009 Nov 20;27(33):5559–64. doi: 10.1200/JCO.2009.22.4733. Epub 2009 Oct 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mack JW, Paulk ME, Viswanath K, Prigerson HG. Racial disparities in the outcomes of communication on medical care received near death. Arch Intern Med. 2010;170:1533–40. doi: 10.1001/archinternmed.2010.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.http://www.dartmouthatlas.org/tools/care.aspx?step=3&loc=116
- 24.Lackan NA, Eschbach K, Stimpson JP, Freeman JL, Goodwin JS. Ethnic differences in inhospital place of death among older adults in California: effects of individual and contextual characteristics and medical resource supply. Med Care. 2009;47:138–45. doi: 10.1097/MLR.0b013e3181844dba. [DOI] [PMC free article] [PubMed] [Google Scholar]