Abstract
We assessed relationships between neighborhood racial residential segregation (RRS), individual-level health declines and mortality using Health and Retirement Study data. We calculated the census-tract level Location Quotient for Racial Residential Segregation (LQRRS), and estimated adjusted relative risks (ARR) of LQRRS for declines in self-reported health or death 1992–2000, controlling for individual-level characteristics.
Of 6,653 adults, 3333 lived in minimal, 2242 in low, 562 in moderate, and 516 in high LQRRS tracts in 1992. Major decline/death rates were: 18.6%, 25.2%, 33.8% and 30.4% in minimal, low, moderate and high tracts, respectively. Adjusting for demographic characteristics, residence in low, moderate and high LQRRS census tracts was associated with greater likelihood of major decline/death compared to minimal LQRRS. Controlling for all variables, only moderate LQRRS predicted major decline/death, ARR=1.31 (95% CI 1.07, 1.59; p<.05).
Keywords: segregation, census tracts, health status, contextual effects, health disparities, geography, United States
INTRODUCTION
Large disparities in health and high levels of racial residential segregation (RRS) are pervasive realities for many African Americans in the United States when compared to non-Hispanic whites (Massey and Denton, 1993; Williams, 1996, 1997, 1999). Several studies demonstrate a potential link between RRS and individual and community level health outcomes that may partially explain the basis for these disparities. For example, areas with higher levels of racial residential segregation are associated with higher rates of infant and adult mortality (LaVeist, 1993; Fang et al., 1998; Geronimus et al., 1996, 1999), cardiovascular disease (Diez Roux et al., 2001; Cooper, 2001), and poorer mental health (Aneshensel and Sucoff, 1996; Schulz et al., 2001), and these associations remain after controlling for individual level characteristics of residents such as socioeconomic status and health behaviors. Additionally, LaVeist found racial segregation to be associated with greater odds of death for African Americans and that older African American adults are more likely than other age groups to live in neighborhoods disadvantaged by racial segregation (LaViest, 2003).
What do we mean by segregation and how does RRS effect health outcomes? In the most general sense, segregation is the geographical separation of people on the basis of ethnicity or race (Kaplan and Holloway, 1998). Measures of RRS may capture exposure to factors deleterious to health, including higher levels of poverty, crime, incivility and social disorganization; poorer educational and occupational opportunities (Williams et al., 2010); poorer housing and the built environment, as well as poor role models for health behaviors. Notwithstanding what we know about the association of RRS and health outcomes, previous empirical work studying this relationship has notable gaps (White and Borrell, 2011). For example, the majority of studies investigating the relationships between segregation and health outcomes have focused on mortality outcomes including adult all-cause and infant mortality (White and Borrell, 2011; Fang, et al., 1998; Geronimus, et al., 1996, 1999). However, explanatory factors may not be uniform in their impact on different health outcomes, and therefore expanding outcomes to include declines in subjective health status may strengthen our understanding of the relationship between segregation and health.
Segregation is a phenomenon that can be meaningful at several geographic levels, such as counties, metropolitan areas, cities or neighborhoods. Traditional operational measures of segregation most prevalent in the health literature are calculated for large geographic areas (e.g., metropolitan areas, cities) and are typically used in the investigation of aggregate outcomes—e.g., rates of mortality and rates of low birth weight (White and Borrell, 2011). However, neighborhood factors have been suggested as particularly important determinants of health for older adults (Yao and Robert, 2007). Hence, these large area measures tell us relatively little about the extent to which individuals are exposed directly to segregation and how local areas or neighborhoods characterized by segregation might affect individual level health outcomes. Lastly, the use of cross sectional analyses limits the ability of many studies to understand the explanatory importance of individual variables influencing health. For example, cross sectional studies cannot discern whether disparities in outcomes have decreased or increased over time (Yao and Robert, 2007).
We designed our study to help address these important gaps. We assess the relationship between racial residential segregation and self-reported major declines in health or death in older adults using a small area measure of segregation, the Location Quotient for Racial Residential Segregation (LQRRS). The LQRRS measure can be considered as examining the hypothesis of relative deprivation (one’s position relative to others in society is a health determinant) as put forth by Robert Merton (1938). He claimed that individual differences could be better studied by examining relative, rather than absolute differences. More recently, Wilkinson and Pickett (2007) have argued that social inequalities (including health status and mortality) are best studied by comparing the degree of relative differences between individuals and groups, rather than simply comparing absolute levels of social indicators. Following Merton (1938) we introduce a segregation measure that accounts for relative differences by comparison of smaller neighborhood units relative to the larger metropolitan area.
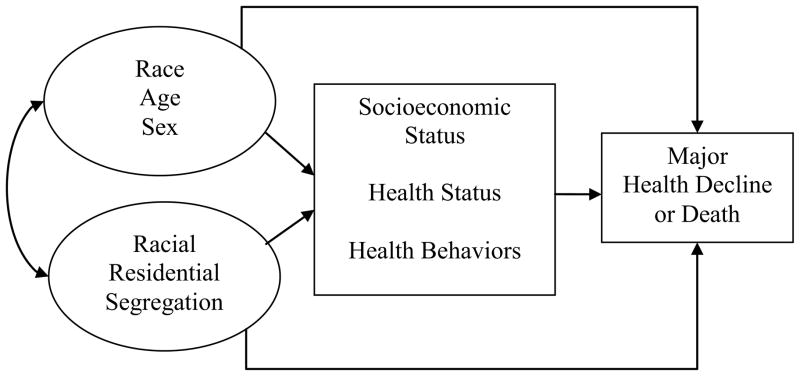
Figure 1 presents the conceptual model guiding this investigation. First, we conceptualize racial residential segregation and the three demographic variables of age, sex and race/ethnicity to be exogenous covariates and their unanalyzed association is indicated by a curved double arrowed connection. This model suggests racial residential segregation and demographics affect health outcomes both directly and indirectly, where the effects are mediated to some degree by individual level factors including socioeconomic status (educational attainment, income, health insurance coverage, net worth), health behaviors (smoking and alcohol consumption patterns), and health status (self-reported overall health, chronic health conditions). These individual factors are more proximate determinants of health declines and death (Link and Phelan, 1995). Our model also suggests that not all of the effects of segregation and demographics are mediated by individual level factors and we allow for direct effects of segregation and demographics on health.
Figure 1.
Conceptual Model of Racial Residential Segregation, Individual Level Factors and Health Outcomes.
METHODS
Data sources
For this study we use two data sources. The first includes Wave 1 (1992) and Wave 5 (2000) of the Health and Retirement Study (HRS), a longitudinal, nationally representative, multistage area probability sample of U.S. households. Supported by the National Institute on Aging and conducted by the University of Michigan’s Institute for Social Research, the first wave of data collection targeted non-institutionalized persons in the contiguous U.S. ages 51–61 (born 1931–1941) and their spouses. For the initial interview, in-home, face-to-face interviews were conducted for 7,608 households yielding 12,652 individual respondents (an overall response rate of 82%). Subjects were subsequently interviewed every two years. Blacks, Hispanics, and Florida residents were over sampled. By design, the HRS staff provided sampling and analytical weights only for the targeted “age-eligible” respondents and their “age-eligible” spouses/partners to adjust for over sampling and non-response bias. A more detailed description of the overall study design and sampling methods are provided elsewhere (Heeringa and Connor, 1995). Complete details on the HRS are available online at http://hrsonline.isr.umich.edu. Our second data source is the 1990 U.S. Decennial Census (U.S. Census Bureau, 1990) from which we obtained the necessary population values at the Metropolitan Statistical Area (MSA) and census tract levels in order to compute our focal independent variable LQRRS. The U.S. Census data was then merged with HRS restricted baseline data gathered in 1992 that included subjects’ census tract information.
Subjects
Because of the HRS complex survey design and our desire to produce nationally representative estimates for this age group in our final analysis, we were limited to using those respondents for whom sampling and analysis weights were provided. By design, these were the targeted “age-eligible” respondents and spouses/partners mentioned above, ages 51–61 in 1992, numbering 9,824 individuals of the original 12,652 respondents, the balance of which were spouses of the age eligible respondents outside of the 51–61 age range. Next, 85 (0.9%) respondents had incomplete records for either the 1992 or 2000 interview and were excluded. An additional 1399 (14.2%) were lost to follow-up over the 8-year period. This left us with 8340 respondents initially available who had complete records in both waves of data collection or who had died during the period 1992–2000. Among these 8340 respondents we excluded an additional 1687 persons (17.1%) who were rural (non-MSA) residents. This left 5975 persons who had complete records plus 678 persons who died in the period 1992–2000 for a total study sample of 6653. We used both publicly available HRS data files and a restricted data file containing geographic identifiers for each respondent. Finally, because of the sensitive nature of the geographic identifiers, this study was approved by a local institutional review board and the staff of the Health and Retirement Study.
Major decline/death
Two health status indicators were combined to define our single outcome measure: major decline in self-reported overall health (SROH) between 1992 and 2000, and death (all cause mortality) between 1992 and 2000. Self reported overall health (SROH) or global self-rated health has been used as an important patient-derived outcome variable (Satariano, 1986; Shetterly et al., 1996; Idler and Benyamini, 1997). Previous work also documents that SROH is predictive of mortality in longitudinal studies (Onawola and LaVeist, 1998; Bowling, 1991), predicts medical care services use (Krauss et al., 1999), and is useful in predicting subsequent changes in health, physical functioning, disability, and distress (Farmer and Ferraro, 1997; Ferraro et al., 1997; Idler and Kasl, 1991).
First, death was determined using National Death Index and household contacts by the HRS staff and made available as a public dataset. Second, self reported overall health was assessed with the Excellent/Very Good/Good/Fair/Poor questionnaire response format at each interview. A major decline in SROH was defined as follows: 1) a decline from excellent/very good/good health in 1992 to fair/poor health in 2000; or 2) a decline from fair health in 1992 to poor in 2000 (Baker et al., 2001, 2006; Sudano and Baker, 2006). We also expanded this health status measure (major decline in heath) to include any individuals—regardless of 1992 health status—who died between 1992 and 2000. Thus we call our final outcome measure a major decline or death 1992 – 2000.
An Exposition of LQRRS: A Local (Small Area) Measure of Racial Residential Segregation
Racial residential segregation is typically measured across large areas, reflecting the ambient effects across a region, such as an MSA, county, or city. While traditional large scale measures such as the popular index of dissimilarity (or “D”) are often used when analyzing aggregated rates of outcomes in a region, they fail to characterize the segregation level of the smaller constituent geographic units. Segregation levels across constituent units are not expected to be uniform; the level in each unit is likely to deviate from the aggregate level. Therefore, it is important to recognize that spatial variation among the constituent levels (typically census tracts) imposes different magnitudes of effects for residents in different parts of the region. Measures such as “D”, which describes the overall segregation level of a region, are labeled as global measures, but local measures—with a value assigned to each constituent unit—are needed in order to more accurately depict the conditions experienced by individuals (O’Sullivan and Wong, 2007; Wong, 1996, 2002). Notwithstanding the debate on whether to use a spatial versus social or interactional definition of neighborhood (O’Campo, 2003), using census tracts has been the de facto method for approximating a neighborhood unit in scores of studies (O’Campo, 2003; Saelens et al., 2003) and it is our approach in this study. We therefore use the terms “neighborhood” and “census tract” interchangeably.
We take the theoretical stance that variation in health outcomes can be explained by relative (rather than absolute) differences in the segregation of neighborhoods. In order to depict the segregation experience of individuals within a neighborhood, a conventional solution involves the proportion (or percentage) of minority members in a unit as a marker for the level of segregation (Myers, 2004; Kiel and Zabel, 1996). Even though this indicator is highly correlated with other measures of segregation and its calculation is straightforward, it has important limitations. While some have questioned the conceptual meaning of proportional measures, others have questioned construct validity and interpretation. Massey and Denton (1988) suggested five dimensions of segregation: evenness, isolation, concentration, centralization and clustering, and while the validity and interpretations of these five dimensions are beyond the scope of this article (interested readers can refer to Wong (2008)), simple proportions do not adequately characterize any of these varied dimensions of segregation. Some have suggested that measures of segregation should refer to “differences in the distribution [our emphasis] of social groups” and hence “only dispersion [our emphasis] measures are proper measures of segregation” (James and Taeuber, 1985). The evenness dimension, which is effectively captured by the dissimilarity index D, has been the standard segregation measure. However, this premise is only appropriate when one assesses the aggregated segregation pattern of the region. To properly account for the features of inequality operating on individuals at the neighborhood level, a relative comparison measure is more appropriate to reflect the experience of residents (Wong, 2002).
Rarely used to reflect racial residential segregation, the Location Quotient (LQ) has been commonly used by economic geographers and regional labor economists and is a standard tool to assess the level of specialization of a particular industry or type of economic activity in a subunit within a region (Isserman, 1977). It has also been used by demographers to characterize the distribution of a population with specific characteristics relative to the overall composition of the characteristic across a larger area (see http://www.bls.gov/cew/cewlq.htm for more details and a web tool for calculating various LQ’s). In demography, LQ is regarded as a measure of relative concentration, but demographers use of “concentration” here is not identical to the meaning conveyed by the five dimensional categorization of segregation (James and Taeuber, 1985; Massey et al., 1996). For Massey, concentration refers to a ratio of occupied physical space or density (Massey and Denton, 1988). Our operationalization extends the work of Massey with a ratio that quantifies the relative racial homogeneity of each neighborhood within an MSA.
The LQ can be calculated simply as:
where LQim is the value for the ith unit or tract in a region or MSA for minority group m; xim is the number of individuals from minority group m living in the ith tract; Xi is the total number of residents in the ith tract of the MSA; Xm is the total number of individuals from minority group m in the MSA; and X is the total number of residents in the MSA. Hence the final value consists of a ratio of two proportions in which the numerator is the proportion of minority residents in the tract and the denominator the proportion of minority residents in the larger region or MSA. As an example, a census tract with an LQ index of 5 means that the proportion of group M living in the tract is 5 times the proportion of group M in the larger region or MSA as a whole. The LQ can be calculated for any two groups or any two characteristics so we therefore had to choose which groups to use in our measure of LQRRS. Because Hispanics are relatively under-represented in our sample compared to whites and blacks, we chose to focus this analysis on the relative distribution of non-Hispanic African-Americans compared to all others. Hence our LQRRS is more accurately a measure of Black/other segregation versus Black/White segregation.
Variables
To represent and to control for individual level factors important to health outcomes, we used an approach informed in part by Andersen’s Behavioral Model for Healthcare Utilization (Anderson, 1995) and its subsequent expansion to include health outcomes (Anderson, 2000). In this framework, characteristics of the individual are organized into categories reflecting predisposing (generally demographic variables), enabling (generally socioeconomic variables) and need-related (health status and lifestyle variables) contributing to health care utilization and ultimately health outcomes. Previous work demonstrates that these factors are linked to the use of health care preventive services (Sudano and Baker, 2003), act as barriers to care (Baker et al., 2002), and are associated with declines in health and mortality (Sudano and Baker, 2006). Details on these variables follow below.
Demographics
Respondents’ age in years (continuous) was recorded from the 1992 interview; sex was categorized as female or male (referent group); marital status was categorized as married (referent group), separated/divorced/widowed, or never married; race/ethnicity was categorized as white, black or Hispanic using self-reported data from respondents.
Socioeconomic Status
Educational attainment was measured in number of years of formal schooling completed. We computed an adjusted income measure for each respondent--an income-to-needs ratio (INR)-that incorporates total household income divided by the poverty guideline for a given size household. As an example, an INR of 3.0 is equivalent to an income 300% of the poverty guidelines for a given family size. Net worth as of 1992 was first measured as a continuous variable in units of US dollars. Both INR and net worth were collapsed into variables with 6 and 5 categories, respectively. INR values were <1.00, 1.00–1.49, 1.50–1.99, 2.00–2.99, 3.00–4.99 and 5.00 and greater. Net worth values were actually quintiles of the distribution with dollar amounts of <$20,200; $20,201-$69,000; $69,001-$138,000; $138,001-$286,000 and >$286,000. Both INR and net worth were entered into the equation as pseudo-continuous variables using their respective numerical values of 1–6 and 1–5. Finally, we used a measure of intermittent insurance status, first determining the existence of any kind of health insurance coverage (public or private) in 1992, 1994, and 1996, and then categorizing individuals as a) insured all 3 interviews (referent), b) 1–2 reports of being uninsured, or c) uninsured all 3 interviews.
Health Status
All multivariate models adjusted for 4 health status variables based on self-reports from the 1992 interview. These included self-reported overall health categorized as poor (referent), fair, good, very good and excellent; a count of total number of chronic diseases (hypertension, diabetes, health disease, chronic lung disease, cancer, arthritis, stroke, and visual difficulties) (Verbrugge et al., 1989), and a count of the number of physical limitations. Three sets of questions previously described by HRS investigators assess the number of physical limitations and include 4 items assessing difficulties with mobility (activities requiring large muscle strength), 6 items assessing difficulties with agility (activities required to perform instrumental activities of daily living), and 5 items assessing difficulties with facility (activities required to perform activities of daily living) (Fillenbaum, Burchett and Welsh, 1993; Baker et al., 2001). A report of any difficulty with the activity was coded as 1 and no difficulty coded as 0. The total number of difficulties was summed and entered into the equations as a continuous variable.
Some of the respondents in the HRS reported fair or poor health status at baseline, and therefore were more likely to experience a health decline or death in subsequent waves. Conversely, others reported very good or excellent health, and were thus less likely to have a decline and more likely to survive over the study period. If in fact health status at baseline influences segregation, the estimates of the effect of segregation may be biased because they in some regard are reflections of baseline health status. To control for potential selection bias, in which baseline health status is related to segregation, we included along with the 3 measures detailed above another a measure of health status—self-reported health status trajectory in the past year, categorized as much worse (referent), somewhat worse, the same, somewhat better, and much better.
Health Behaviors
Health behaviors include a smoking behavior measure categorized as never smoked (referent), past and current smoker; past problem drinking measured using the CAGE index dichotomized as none or 1 indicator as referent versus 2 or more indicators (Mayfield et al., 1974); a measure of current drinking pattern based on number of drinks per day categorized as abstainer, moderate (referent), and heavy drinking; and body mass index (BMI) was categorized into quintiles, with the lowest quintile as referent.
Analytic scheme
We used the analytic and survey weights included in the data files to produce nationally representative point estimates and to account for the complex sampling design in the HRS. Nested multivariable logistic regression models estimated unadjusted and adjusted odds ratios of health declines (major decline in self-reported health or death 1992–2000) for categories of LQRRS, controlling for individuals’ demographic characteristics, socioeconomic status, health status and health behaviors. Odds ratios were converted to adjusted relative risks using a published formula from Zhang and Yu (1998). We used STATA versions 9 and 10 (College Station, TX) for all analyses. A p value of 0.05 was used to determine statistical significance. In order to determine the necessity of accounting for clustering of individuals within census tracts, we used the xtlogit procedure in STATA to calculate the intraclass correlation coefficient (ICC) (reported as rho by xtlogit). The ICC was .02 and was not statistically significant. Research suggests that linear regression estimates are sufficient when the ICC < .05 and that there is no benefit to multilevel modeling when the ICC is not different from zero (Goldstein, 2003). We report only the logistic regression results here.
RESULTS
Study subjects lived in 85 MSA’s in a total of 1303 census tracts. Whites resided in 78 MSA’s and 1031 tracts, Blacks in 60 MSA’s and 338 tracts, and Hispanics in 59 MSA’s and 263 tracts. Distributions within tracts range from 1–58 respondents for Whites, 1–18 for Blacks and 1–19 for Hispanics, while means within tracts were similar at approximately 10 for each group.
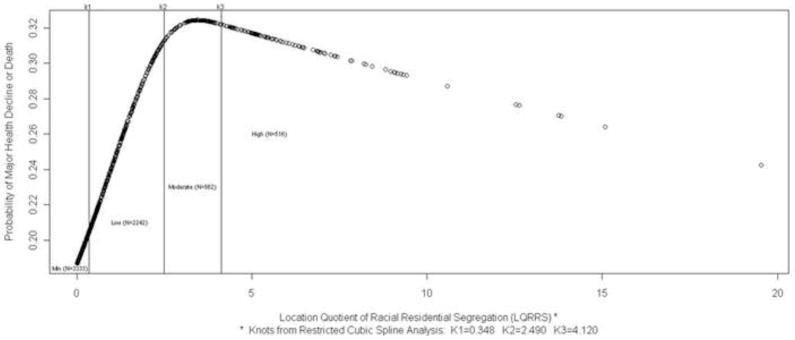
Because the use of LQRRS as operationalized in our study is new (we know of no other study that has used it), there is no consensus on how to incorporate it into multivariable models. Other continuous measures of segregation at the global level are typically categorized in analyses to facilitate interpretation of effects and we follow this practice (Cutler et al., 1999). For example the “D” index has a possible range of 0.0–1.0 and is often categorized as low (>0.3), moderate (0.3–0.6), and high (>0.6) (Massey and Denton, 1993; Williams, 1996). We used methods suggested by Harrell (2006) (i.e., restricted cubic splines) to establish empirically justifiable cut points for the LQRRS/health outcome relationship, and subsequently categorized LQRRS as minimal, low, moderate and high (cut points detailed below).
As mentioned above, the distribution of respondents by LQRRS was skewed, with 3,333 (50.1%) of the study population respondents living in minimally segregated neighborhoods (614 tracts with LQRRS values < 0.34); 2,242 (33.7%) living in low segregation neighborhoods (474 tracts with LQRRS values of 0.34–2.49); 562 (8.4%) living in moderately segregated neighborhoods (104 tracts with LQRRS values of 2.50–4.11); and 516 (7.8%) living in highly segregated neighborhoods (116 tracts with LQRRS values of >4.11) (Table 1).
Table 1.
Study Population Characteristics by LQRRS Category (N=6653)
| LQRRS Census Tract Levels | |||||
|---|---|---|---|---|---|
|
| |||||
| Demographics | Minimal m=610 n=3333 |
Low m=474 n=2242 |
Moderate m=104 n=562 |
High m=116 n=516 |
p |
|
| |||||
| Age, mean years (SD) | 55.9 (3.2) | 55.8 (3.1) | 55.9 (3.1) | 56.1 (3.2) | .263 |
|
| |||||
| Female Sex, % | 51.0 | 51.7 | 60.2 | 56.3 | .003 |
|
| |||||
| Racial/Ethnic Group, % | .000 | ||||
| White | 94.7 | 79.7 | 25.8 | 22.4 | |
| Black | 10.7 | 10.8 | 69.6 | 74.3 | |
| Hispanic | 4.3 | 9.6 | 4.7 | 3.3 | |
|
| |||||
| Marital Status, % | .000 | ||||
| Never Married | 3.1 | 4.9 | 7.7 | 7.7 | |
| Separated, Divorced, Widowed | 17.3 | 23.2 | 37.8 | 37.5 | |
| Married | 79.6 | 71.8 | 54.7 | 54.8 | |
|
| |||||
|
Socioeconomic Status
| |||||
| Education in years, mean (SD) | 12.7 (2.9) | 11.7 (3.6) | 11.7 (3.1) | 11.7 (3.0) | .000 |
|
| |||||
| Income-to needs ratio, mean (SD) | 5.0 (1.4) | 4.5(1.6) | 4.1 (1.8) | 4.0(1.8) | .000 |
|
| |||||
| Net Worth in thousands of $, mean (SD) | 30.8 (59.4) | 18.0 (36.5) | 14.1 (52.7) | 13.6 (43.8) | .000 |
|
| |||||
| Continuously Insured (1992–96) % | 83.8 | 76.4 | 70.8 | 71.6 | .000 |
|
| |||||
|
Health Status
| |||||
| Self-reported Overall Health, % | .000 | ||||
| Poor | 5.6 | 8.4 | 10.6 | 12.7 | |
| Fair | 9.1 | 15.0 | 21.8 | 19.8 | |
| Good | 23.9 | 26.5 | 32.5 | 32.5 | |
| Very Good | 32.6 | 27.0 | 24.4 | 23.0 | |
| Excellent | 28.8 | 23.2 | 10.7 | 12.0 | |
|
| |||||
| Chronic Disease Count, mean (SD) | 1.1 (1.1) | 1.3 (1.3) | 1.4 (1.3) | 1.5 (1.3) | .000 |
|
| |||||
| Physical Limitations Count, mean (SD) | 2.6 (3.0) | 3.3 (3.5) | 3.5 (3.6) | 3.8 (4.0) | .000 |
|
| |||||
| Health Now as Opposed to 1-year Ago, % | .000 | ||||
| Much Worse | 1.7 | 2.6 | 4.2 | 6.9 | |
| Somewhat Worse | 8.7 | 10.8 | 12.0 | 9.7 | |
| The Same | 74.7 | 70.5 | 66.6 | 67.8 | |
| Somewhat Better | 10.0 | 10.0 | 11.8 | 8.7 | |
| Much Better | 4.9 | 6.2 | 5.5 | 7.0 | |
|
| |||||
| Major Decline or Death 1992–2000, % | 18.1 | 23.8 | 33.7 | 30.5 | .000 |
|
| |||||
|
Health Behaviors
| |||||
| Smoking, % | .000 | ||||
| Never | 36.1 | 32.2 | 39.0 | 31.3 | |
| Past smoker | 39.3 | 38.0 | 39.9 | 36.3 | |
| Current smoker | 24.6 | 30.0 | 31.2 | 32.3 | |
|
| |||||
| Baseline Alcohol Use Pattern, % | .000 | ||||
| Abstainer | 29.7 | 39.1 | 43.0 | 40.9 | |
| Moderate | 64.6 | 56.0 | 50.7 | 52.0 | |
| Heavy | 5.7 | 4.9 | 6.3 | 7.1 | |
|
| |||||
| Problem Drinking History (CAGE), % >2 | 12.5 | 15.1 | 20.2 | 17.2 | .000 |
|
| |||||
| BMI Quintiles, % | .000 | ||||
| 1st (14.3–23.0) | 19.5 | 21.6 | 14.3 | 16.4 | |
| 2nd (23.1–25.2) | 12.4 | 19.5 | 18.6 | 16.3 | |
| 3rd (25.3–27.4) | 19.6 | 19.3 | 17.4 | 18.2 | |
| 4th (27.5–30.6) | 20.7 | 20.1 | 22.0 | 21.8 | |
| 5th (30.7–59.1) | 16.8 | 19.4 | 27.7 | 27.4 | |
Notes: Results are from weighted analyses using survey estimation procedures in Stata 9 and 10. m=number of tracts in the LQRRS category; n=number of respondents in the LQRRS category. BMI=Body mass index (kg/m2).
Significance tests for categorical variables are based on the Pearson χ2 statistic corrected for survey design and the test for continuous variables are based on the t statistic. Income-to-needs ratio is based on household income in 1991 divided by the poverty guideline for a given household size. A value of 5.00 for example indicates a household income 5 times (or alternative, 500% of) the poverty guideline for a given household size.
Age was the only characteristic not associated with LQRRS in the bivariate analysis. There were higher percentages of females in moderate and high segregation neighborhoods. A higher percentage of blacks lived in moderate and highly segregated neighborhoods than in minimally segregated neighborhoods, while for whites higher percentages lived in minimally and low segregation neighborhoods, and the highest percentage of Hispanics lived in low segregated neighborhoods.
Living in a minimally segregated neighborhood was associated with higher socioeconomic status. In particular, at the bivariate level, average net worth in minimally segregated neighborhoods was 2.3 times higher than in highly segregated neighborhoods. Those in the most segregated neighborhoods had the lowest levels of income to needs. Respondents living in moderate and highly segregated neighborhoods had higher mean counts of chronic disease and physical limitations. Living in these neighborhoods was also associated with reporting lower self-rated health at baseline and experiencing a major decline or death between 1992 and 2000. The highest level of LQRRS was associated with worsening baseline self-reported health (health as opposed to 1-year ago) but also with improving self-reported health. Highly segregated neighborhoods had the highest percentage of current smokers and heavy drinkers, while moderately segregated neighborhoods had the highest percentage with a history of alcohol abuse and the highest percentage of obese residents.
Predicted probabilities from a logit analysis of the relationship between LQRRS and major health declines or death is displayed in Figure 2. The eight year probability of major decline or death is near zero in the minimal segregation category, increases rapidly in the low segregation category and is highest in the moderate and high segregation categories. Also notable is the slight decline in probability of major decline or death as the continuous LQRRS measure increases.
Figure 2.
LQRRS Cutpoints by Probability of Major Decline or Death 1992–2000 N=6653)
Table 2 presents the results of nested logistic regression analyses for the change in relative risk of major decline or death by LQRRS when adding demographics, socioeconomic status, baseline health status, and health behaviors to the logistic regression model. LQRRS has a strong and statistically significant association with major decline/death at low, moderate and high levels in the unadjusted model, with ARR’s ranging from 1.32–1.86. In Model 2 the magnitude of the ARR’s decreases but the same overall pattern of relationships is maintained.
Table 2.
Nested Logistic Regression Results Showing Changes in Adjusted Relative Risk (ARR) of Major Decline or Death for Low, Moderate and High vs. Minimal LQRRS (N=6653).
| ARR by LQRRS (95% Confidence Intervals) | |||||
|---|---|---|---|---|---|
| Nested Models of Major Decline/Death as of 2000 | Minimal LQRRS Tracts N=3333 | Low LQRRS Tracts n=2242 | Moderate LQRRS Tracts n=562 | High LQRRS Tracts n=516 | |
| 1 | Unadjusted | Referent | 1.32*** (1.16–1.49) | 1.86*** (1.63–2.10) | 1.69*** (1.45–1.95) |
| 2 | Demographicsa | Referent | 1.25*** (1.10–1.42) | 1.57*** (1.31–1.86) | 1.37** (1.12–1.66) |
| 3 | Demographics, SESb | Referent | 1.10 (0.96–1.26) | 1.36** (1.12–1.64) | 1.19 (0.95–1.46) |
| 4 | Demographics, SES, Health Statusc | Referent | 1.08 (0.93–1.25) | 1.31* (1.07–1.59) | 1.11 (0.88–1.37) |
| 5 | Demographics, SES, Health Status, Health Behaviorsd | Referent | 1.07 (0.92–1.23) | 1.31* (1.07–1.59) | 1.08 (0.86–1.36) |
Notes. All statistical tests are compared to the referent group (Minimal LQRRS).
Demographic variables include age, sex, racial/ethnic group.
SES (socioeconomic status) variables include educational attainment, insurance status, income-to-needs ratio (total household income divided by the poverty guideline for a given size household) and net worth in quintiles (see methods section for details) as of the 1992 interview.
Health status variables include: self-rated health (at baseline), self-rated health at baseline (as opposed to prior year), chronic diseases, and functional limitation.
Health behavior variables include the following, as of the respondents’ 1992 interview: smoking status, alcohol consumption pattern, CAGE score, and body mass index.
= p < 0.05;
= p < 0.01;
= p < 0.001
Addition of the socioeconomic status variables in Model 3 severely reduces the effect of segregation on major decline/death for low and high LQRRS census tracts. For moderate LQRRS census tracts the effect of segregation on major health decline/death is also reduced but remains statistically significant. Results from models 4 and 5 indicate that controlling for individual baseline health status and health behaviors does not substantially reduce the effect of segregation on major health decline/death over and above the model that includes SES.
DISCUSSION
This study has overcome key limitations of previous studies of segregation and health, notably the reliance on only large-area measures of segregation, cross-sectional data, aggregate (non-individual) data, the absence of key indicators such as body mass index and substance use/misuse, and coarse measures of health status (White and Borrell, 2011; LaViest, 2003; Robert and Ruel, 2006). In this study of older adults in the United States, the results provide preliminary support for the conceptual model in Figure 1. Socioeconomic status explains much of the association between neighborhood racial segregation and health outcomes. Health status and health behaviors did not explain much of the association between segregation and health after controlling for socioeconomic status, and these individual level factors did not explain all of the effects of LQRRS for residents of moderately segregated neighborhoods.
These findings are consistent with previous research that has demonstrated the effect of RRS on health status to be mediated through individual characteristics. Communities with greater residential segregation can be characterized by lower community socioeconomic status (SES) including higher levels of poverty and unemployment, fewer job opportunities, fewer or restricted social and public services, poorer school systems, and higher proportions of deteriorated or abandoned housing stock (Cohen et al., 2003). Such observations have led many researchers to conclude that RRS is a “fundamental” or basic underlying “social” factor shaping the opportunity structure and life-world of individuals residing in segregated communities—communities with potentially damaging health consequences for many (Williams and Collins, 2001).
Ample evidence derived from cross-sectional studies suggests a relationship between RRS and unemployment levels (Cubbin et al., 2001) and proportion of residents living below poverty levels. Likewise, RRS has been linked to social factors such as higher crime levels (Kawachi and Kennedy, 1997), and higher rates of female headed households (Gee, 2002; LeClere et al., 1997, 1998). The physical environment of a community has also been associated with levels of segregation. Specifically, toxic dumps are more frequently located in or near areas of high RRS (Sexton and Anderson, 1993), and areas of high RRS often have extremely poor housing stock, which increase potential exposure to lead or other noxious substances. Each has serious health consequences including increased risks of cancer, cognitive disability, and asthma. Similarly, areas of high RRS are often sites of intense promotion of alcohol and tobacco consumption, fewer grocery stores stocking a full range of nutritious products, and more likely to have unsafe streets and few areas for physical exercise, leading to higher rates of obesity and inactivity. All of these factors may ultimately translate into increased risks for cancer, hypertension, diabetes, and cardiovascular disease. In short, all of this evidence suggests an association between RRS and community characteristics that plausibly leads to downstream effects on residents’ health (Grady and Ramirez, 2008; Kramer and Hogue, 2009).
Based on the descriptive results reported in Table 1, bivariate results in Figure 2 and the multivariate results in Table 2 we conclude that LQRRS is an effective way of operationalizing racial residential segregation. Our findings from a nationally representative panel study in the United States are similar to cross-sectional findings on relative deprivation by socioeconomic status in a European sample (Stafford and Marmot, 2003). By using LQRRS, a measure of the relative concentration of neighborhood racial segregation, our research is more consistent with the realities of geographic variation in inequality than prior studies. We do not assume that a specific proportion of minorities is responsible for health inequalities in all communities in the United States. Instead, our operational definition of LQRRS recognizes the importance of how segregated a person’s neighborhood is as compared with other neighborhoods in a metropolis, recognizing the pervasive nature of localized status hierarchies.
Our research is an extension of prior empirical and theoretical understandings of the complexity of social inequality (Shulz and Mullings, 2006). Being female and having lower socioeconomic status were both associated with living in census tracts characterized by higher levels of segregation. Our multivariate analysis is supportive of a theoretical model in which health disparities are woven together into a race, class and gender triad of neighborhood health disadvantage.
Limitations and Directions for Future Research
This study has several important limitations. First, our results only represent the 1931–1941 age cohort and may not be generalizable to other age groups. Second, our operational definition of LQRRS is based on a comparison of the distribution of African Americans to all others at the census tract level. Future studies could estimate the potential for a non-uniform effect of our Afro-centric LQRRS measure on the health of other racial and ethnic minorities such as Hispanics and could compute separate segregation indices for different racial and ethnic groups. Cultural and ethnic homogeneity in some settings may offer residents with greater access to social capital and informal networks of support that promote health.
Third, to address attrition we compared characteristics of those included in our analyses with those excluded due to attrition and those excluded because of rural residence; no significant differences were found between the three groups in age, sex, net worth, insurance status, and health behaviors (data not shown). There were significant differences however in education (both excluded groups were slightly less educated); race/ethnicity (more rural white exclusions, fewer rural black exclusions, and more Hispanics lost to attrition); income (both excluded groups had between $5,000 to 15,000 less household income in 1992); and health status (rural exclusions more likely to be in poor or fair health status in 1992 compared to both other groups—27% vs. 19%, respectively. Although recent work using the Health and Retirement Study data found little evidence for attrition bias (Kapteyn et al., 2006) this attrition may or may not induce bias under various conditions (e.g., attrition completely at random, outcome dependent attrition, etc.) (Mirowsky and Reynolds, 2000).
Fourth, a healthy survivor effect (observed in past studies of smoking and obesity) is likely to weaken the association between residential racial segregation and health decline in longitudinal analysis (Koster et al., 2007; Ostbye and Taylor, 2004; Ostbye et al., 2002). Fifth, individuals may move over the study period, but they may move to very similar or very dissimilar census tracts. Any analysis that does not account for mobility tacitly assumes that the “exposure”—in an epidemiological sense—to LQRRS is constant throughout the study period. In an ancillary analysis (data not shown) we used an indicator variable for having moved between baseline and wave 5. The effect of moving on major death/decline was statistically significant (OR 2.33, p<0.001; CI 2.05–2.64), but its inclusion did not alter the magnitude or statistical significance of LQRRS.
We further acknowledge that our LQRRS measure is among the category of segregation measures commonly termed “aspatial” and hence is subject to some limitations. Most notably, LQRRS does not adequately characterize segregation levels of adjacent census tracts and cannot address the modifiable areal unit problem (Wong, 1997; Reardon and O’Sullivan, 2004). Hence future work will incorporate spatial measures at the census tract level to directly compare and contrast these alternative formulations of segregation.
Finally, the continued statistically significantly elevated risk for the moderate LQRRS category after all the controls have been included suggests that there are other processes as yet unidentified and unmeasured that may explain this finding. While our research is limited by the availability of individual level concepts in the HRS, other characteristics of neighborhoods, including environmental factors like noise, pollution, dilapidated housing, and neighborhood socioeconomic status indicators could be operationalized in a future study in order to give a more complete depiction of how neighborhood-level measures influence health outcomes.
Notwithstanding these limitations, our study has addressed several limitations identified in a recent review of research on segregation and health (White and Borrell, 2011). Our analysis extends prior work with evidence that LQRRS, a relative concentration segregation measure, has a substantial influence on the health declines and mortality of older adults as they age. Health inequalities are created by larger inequalities in society. The segregation of racial and ethnic minorities into disadvantaged neighborhoods is a persistent and lasting structural cause of health disparities (Williams and Collins, 1995; Williams et al., 2010). The results presented here lend further support to the theory that a person’s relative position in society, including the relative concentration of minority group members in their neighborhood compared to other neighborhoods in a region, can influence health over time for older adults, and can reinforce the multiplicative structure of health and social inequality.
LQRRS is a newly developed aspatial local area measure of racial residential segregation.
We use longitudinal data on older adults from the Health and Retirement Study.
This new measure has a curvilinear association with major declines in health and mortality.
Acknowledgments
This work was supported by grants from the National Institute of Aging (1RO1 AG024206), the National Cancer Institute (R25T-CA111898), and the VA Health Services Research and Development Services (IIR 06-091).
Footnotes
Note: The views expressed in this article are those of the authors and do not necessarily represent the views of the NIA, NCI or the Department of Veterans Affairs. None of these entities had any involvement in the design of this study; the collection, analysis and interpretation of the data; writing this report; or submitting this manuscript for publication.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? Journal of Health & Social Behavior. 1995;36:1–10. [PubMed] [Google Scholar]
- Andersen R. The behavioral model of health services access and utilization. Proceedings of the Academy of Health Services Researcher and Health Policy Annual Meeting; June 25, 2000; Los Angeles, CA. 2000. [Google Scholar]
- Aneshensel CS, Sucoff CA. The neighborhood context of adolescent mental health. Journal of Health & Social Behavior. 1996;37:293–31. [PubMed] [Google Scholar]
- Baker DW, Sudano JJ, Albert JM, Borawski EA, Dor A. Lack of health insurance and decline in overall health in late middle age. New England Journal of Medicine. 2001;345:1106–1112. doi: 10.1056/NEJMsa002887. [DOI] [PubMed] [Google Scholar]
- Baker DW, Sudano JJ, Albert JM, Borawski EA, Dor A. Loss of health insurance and the risk for a decline in self-reported health and physical functioning. Medical Care. 2002;40:1126–1131. doi: 10.1097/00005650-200211000-00013. [DOI] [PubMed] [Google Scholar]
- Baker DW, Sudano JJ, Durazo-Arvizu R, Feinglass J, Witt WP, Thompson J. Health insurance coverage and the risk of decline in overall health and death among the near elderly, 1992–2002. Medical Care. 2006;44:277–282. doi: 10.1097/01.mlr.0000199696.41480.45. [DOI] [PubMed] [Google Scholar]
- Bowling A. Measuring Health: A Review of Quality of Life Measurement Scales. Open University Press; Bristol, PA: 1991. [Google Scholar]
- Cohen DA, Mason K, Bedimo A, Scribner R, Basolo V, Farley TA. Neighborhood physical conditions and health. American Journal of Public Health. 2003;93:467–471. doi: 10.2105/ajph.93.3.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper RS. Social inequality, ethnicity and cardiovascular disease. International Journal of Epidemiology. 2001;30:S48–S52. [Google Scholar]
- Cubbin C, Hadden WC, Winkleby MA. Neighborhood context and cardiovascular disease risk factors: the contribution of material deprivation. Ethnicity & Disease. 2001;11:687–700. [PubMed] [Google Scholar]
- Cutler DM, Glaeser EL, Vigdor JL. The rise and decline of the American ghetto. Journal of Political Economy. 1999;107:455–506. [Google Scholar]
- Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. New England Journal of Medicine. 2001;345:99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- Fang J, Madhavan S, Bosworth W, Alderman MH. Residential segregation and mortality in New York City. Social Science & Medicine. 1998;47:469–476. doi: 10.1016/s0277-9536(98)00128-2. [DOI] [PubMed] [Google Scholar]
- Farmer MM, Ferraro KF. Distress and perceived health: mechanisms of health decline. Journal of Health & Social Behavior. 1997;38:298–311. [PubMed] [Google Scholar]
- Ferraro KF, Farmer MM, Wybraniec JA. Health trajectories: long-term dynamics among black and white adults. Journal of Health & Social Behavior. 1997;38:38–54. [PubMed] [Google Scholar]
- Fillenbaum GG, Burchett BM, Welsh KA. AHEAD/HRS Report No. 94–005. Ann Arbor: University of Michigan; 1993. The 20-Item Word List Test as a measure of cognitive ability in the Health and Retirement Study. [Google Scholar]
- Geronimus AT, Bound J, Waidmann TA, Hillemeier MM, Burns PB. Excess mortality among blacks and whites in the United States. New England Journal of Medicine. 1996;335:1552–1558. doi: 10.1056/NEJM199611213352102. [DOI] [PubMed] [Google Scholar]
- Geronimus AT, Bound J, Waidmann TA. Poverty, time, and place: variation in excess mortality across selected US populations, 1980–1990. Journal of Epidemiology & Community Health. 1999;53:325–334. doi: 10.1136/jech.53.6.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell FE., Jr . Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis. Springer-Verlag; New York: 2006. [Google Scholar]
- Heeringa SG, Connor J. HRS/AHEAD Documentation Report. Ann Arbor, MI: 1995. Technical description of the health and retirement study sample design. [Google Scholar]
- Goldstein H. Multilevel Statistical Models. 3. Edward Arnold; London: 2003. [Google Scholar]
- Gee GC. A multilevel analysis of the relationship between institutional and individual racial discrimination and health status. American Journal of Public Health. 2002;92:615–623. doi: 10.2105/ajph.92.4.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grady SC, Ramirez IJ. Mediating medical risk factors in the residential segregation and low birthweight relationship by race in New York City. Health Place. 2008;14:661–677. doi: 10.1016/j.healthplace.2007.10.011. [DOI] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. Journal of Health & Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Idler EL, Kasl S. Health perceptions and survival: do global evaluations of health status really predict mortality? Journals of Gerontology. 1991;46:S55–S65. doi: 10.1093/geronj/46.2.s55. [DOI] [PubMed] [Google Scholar]
- Isserman AM. The location quotient approach for estimating regional economic impacts. Journal of the American Planning Association. 1977;43:33–41. [Google Scholar]
- James DR, Taeuber KE. Measures of segregation. Sociol Methodol. 1985;15:1–32. [Google Scholar]
- Kapteyn A, Michaud PC, Smith J, van Soest A. Effects of attrition and non-response in the health and retirement study. IZA Discussion Paper. 2006:2246. Available at: ftp://repec.iza.org/RePEc/Discussionpaper/dp2246.pdf.
- Kawachi I, Kennedy BP. Health and social cohesion: why care about income inequality? British Medical Journal. 1997;314:1037–1040. doi: 10.1136/bmj.314.7086.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiel KA, Zabel JE. Housing price differentials in U.S. cities: household and neighborhood racial effects. Journal of Housing Economics. 1996;5:143–165. [Google Scholar]
- Koster A, Penninx BWJH, Newman AB, et al. Lifestyle factors and incident mobility limitation in obese and non-obese older adults. Obesity. 2007;15:3122–3132. doi: 10.1038/oby.2007.372. [DOI] [PubMed] [Google Scholar]
- Krauss N, Machlin S, Kass B. MEPS Research Findings No. 7. AHCPR Pub. No. 99–0018. Agency for Health Care Policy and Research; Rockville, MD: 1999. Use of health care services, 1996. [Google Scholar]
- LaVeist TA. Segregation, poverty, and empowerment: health consequences for African Americans. Milbank Quarterly. 1993;71:41–64. [PubMed] [Google Scholar]
- LaViest T. Racial segregation and longevity among African Americans: an individual-level analysis. Health Services Research. 2003;38:1719–1734. doi: 10.1111/j.1475-6773.2003.00199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeClere FB, Rogers RG, Peters KD. Ethnicity and mortality in the United States: individual and community correlates. Population and Development Review. 1997;76:169–198. [Google Scholar]
- LeClere FB, Rogers RG, Peters K. Neighborhood social context and racial differences in women’s heart disease mortality. Journal of Health & Social Behavior. 1998;39:91–107. [PubMed] [Google Scholar]
- Link BG, Phelan J. Social conditions as fundamental causes of disease. Journal of Health & Social Behavior. 1995:80–94. [PubMed] [Google Scholar]
- Massey DS, Denton NA. The dimensions of residential segregation. Population and Development Review. 1988;67:281–315s. [Google Scholar]
- Massey DS, Denton NA. American Apartheid: Segregation and the Making of the Underclass. Harvard University Press; Cambridge, MA: 1993. [Google Scholar]
- Massey DS, White MJ, Phua V. The dimensions of segregation revisited. Sociologic Methods & Research. 1996;25:172–206. [Google Scholar]
- Mayfield D, McLeod G, Hall P. The CAGE questionnaire: validation of a new alcoholism screening instrument. American Journal of Psychiatry. 1974;131:1121–1123. doi: 10.1176/ajp.131.10.1121. [DOI] [PubMed] [Google Scholar]
- Merton RK. Social structure and anomie. American Sociological Review. 1938;3:672–82. [Google Scholar]
- Mirowsky J, Reynolds J. Age, depression, and attrition in the national survey of families and households. Sociologic Methods & Research. 2000;28:476. [Google Scholar]
- Myers CK. Discrimination and neighborhood effects: understanding racial differentials in US housing prices. Journal of Urban Economics. 2004;56:279–302. [Google Scholar]
- O’Campo P. Invited commentary: advancing theory and methods for multilevel models of residential neighborhoods and health. American Journal of Epidemiology. 2003;157:9–13. doi: 10.1093/aje/kwf171. [DOI] [PubMed] [Google Scholar]
- O’Sullivan D, Wong DWS. A surface-based approach to measuring spatial segregation. Geographical Analysis. 2007;39:147–168. [Google Scholar]
- Onawola RS, LaVeist TA. Subjective health status as a determinant of mortality among African-American elders. Journal of the National Medical Association. 1998;90:754–758. [PMC free article] [PubMed] [Google Scholar]
- Ostbye T, Taylor DH. The effect of smoking on years of healthy life (YHL) lost among middle-aged and older Americans. Health Services Research. 2004;39:531–552. doi: 10.1111/j.1475-6773.2004.00243.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostbye T, Taylor DH, Jung SH. A longitudinal study of the effects of tobacco smoking and other modifiable risk factors on ill health in middle-aged and old Americans: results from the health and retirement study and asset and health dynamics among the oldest old survey. Preventive Medicine. 2002;34:334–345. doi: 10.1006/pmed.2001.0991. [DOI] [PubMed] [Google Scholar]
- Robert S, Ruel E. Racial segregation and health disparities between black and white older adults. Journals of Gerontology. 2006;61B:S203–S211. doi: 10.1093/geronb/61.4.s203. [DOI] [PubMed] [Google Scholar]
- Saelens BE, Sallis JF, Black J, Chen D. Neighborhood-based differences in physical activity: an environment scale evaluation. American Journal of Public Health. 2003;93:1552–1558. doi: 10.2105/ajph.93.9.1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satariano WA. Race, socioeconomic status, and health: a study of age differences in a depressed area. American Journal of Preventive Medicine. 1986;2:1–5. [PubMed] [Google Scholar]
- Schulz A, Parker E, Israel DB, Fisher DT. Social context, stressors, and disparities in women’s health. Journal of the American Medical Women’s Association. 2001;56:143–149. [PubMed] [Google Scholar]
- Schulz AJ, Mullings L, editors. Gender, Race, Class, and Health: Intersectional Approaches. Jossey-Bass; San Francisco, CA: 2006. [Google Scholar]
- Sexton K, Anderson Y, editors. Equity in environmental health: research issues and needs. Toxicology & Industrial Health. 1993;9:679–959. doi: 10.1177/074823379300900503. [DOI] [PubMed] [Google Scholar]
- Shetterly SM, Baxter J, Mason LD, Hamman RF. Self-rated health among Hispanic vs. non-Hispanic white adults: the San Luis Valley Health and Aging Study. American Journal of Public Health. 1996;86:1798–1801. doi: 10.2105/ajph.86.12.1798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stafford M, Marmot M. Neighbourhood deprivation and health: does it affect us all equally? International Journal of Epidemiology. 2003;32:357–366. doi: 10.1093/ije/dyg084. [DOI] [PubMed] [Google Scholar]
- Sudano JJ, Jr, Baker DW. Intermittent lack of health insurance coverage and use of preventive services. American Journal of Public Health. 2003;93:130–137. doi: 10.2105/ajph.93.1.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sudano JJ, Baker DW. Explaining US racial/ethnic disparities in health declines and mortality in late middle age: the roles of socioeconomic status, health behaviors, and health insurance. Social Science & Medicine. 2006;62:909–922. doi: 10.1016/j.socscimed.2005.06.041. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. Summary tape file 1 – 100 percent data. Washington, D.C: 1990. [Google Scholar]
- Verbrugge LM, Lepkowski JM, Imanaka Y. Comorbidity and its impact on disability. Milbank Quarterly. 1989;67:450–484. [PubMed] [Google Scholar]
- Wilkinson RG, Pickett KE. The problems of relative deprivation: why some societies do better than others. Social Science & Medicine. 2007;5:1965–1978. doi: 10.1016/j.socscimed.2007.05.041. [DOI] [PubMed] [Google Scholar]
- Williams DR. Racism and health: a research agenda. Ethnicity and Disease. 1996;6:1–8. [PubMed] [Google Scholar]
- Williams DR. Race and health: basic questions, emerging directions. Annals of Epidemiology. 1997;7:322–333. doi: 10.1016/s1047-2797(97)00051-3. [DOI] [PubMed] [Google Scholar]
- Williams DR. Race, socioeconomic status, and health. The added effects of racism and discrimination. Annals of the New York Academy of Sciences. 1999;896:173–188. doi: 10.1111/j.1749-6632.1999.tb08114.x. [DOI] [PubMed] [Google Scholar]
- Williams DR, Collins C. US socioeconomic and racial differences in health: patterns and explanations. Annual Review of Sociology. 1995;21:349–386. [Google Scholar]
- Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Reports. 2001;116:404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA, Leavell J, Collins C. Race, socioeconomic status, and health: complexities, ongoing challenges, and research opportunities. Annals of the New York Academy of Sciences. 2010;1186:69–101. doi: 10.1111/j.1749-6632.2009.05339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong DWS. Enhancing segregation studies using GIS. Computers, Environment & Urban Systems. 1996;20:99–109. [Google Scholar]
- Wong DWS. Modeling local segregation: a spatial interaction approach. Geographical and Environmental Modelling. 2002;6:81–97. [Google Scholar]
- Wong DWS. A local multidimensional approach to evaluate changes in segregation. Urban Geography. 2008;29:455–472. [Google Scholar]
- Zhang J, Yu KF. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. Journal of the American Medical Association. 1998;280:1690–1691. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]