Abstract
INTRODUCTION
Acquired bladder diverticula (BD) in men over the age of 60 are usually due to bladder outlet obstruction (BOO) secondary to prostatic enlargement. In cases of clinical significant BD with persistent symptoms or complications surgical excision should be considered. In the treatment of BD it is important to address the BOO with a bladder outlet procedure either simultaneously or in a staged fashion.
PRESENTATION OF CASE
We present to the best of our knowledge, the first case of sequential robotic-assisted bladder diverticulectomy (RABD) combined with robotic-assisted radical prostatectomy (RARP) in a patient with large diverticula and malignant prostate enlargement as the cause of BOO.
DISCUSSION
Concomitant open radical prostatectomy and bladder diverticulectomy series have been described, while minimal invasive procedures combining BD excision with relive of BOO especially due to benign prostatic enlargement have been reported to be safe and effective.
CONCLUSION
Concomitant RABD with RARP is a safe and effective procedure with excellent oncological and functional results.
Keywords: Bladder diverticula, Robotic diverticulectomy
1. Introduction
Bladder diverticula (BD) represent a herniation of the bladder urothelium through a defect of the bladder wall. Due to the fact that BD contain only scattered muscle fibers, they fail to empty their content efficiently during bladder emptying leading to high residual urine with characteristic findings in cystoscopic and imaging evaluation. BD are typically asymptomatic and are found during investigation of associated lower urinary tract symptoms (LUTS). Although, if a diverticulectomy procedure is decided, it should be performed in relation to an outlet procedure, which can be done as a staged procedure or concurrently in the same session.1,2 We report, to the best of our knowledge, the first case of robotic-assisted bladder diverticulectomy (RABD) combined with robotic-assisted radical prostatectomy (RARP) in a patient with large diverticula and malignant prostate enlargement as the cause of bladder outlet obstruction (BOO).
2. Presentation of case
A 59-year-old healthy male with a 5-year history of LUTS under treatment with an a-blocker presented to our clinic with exacerbation of his symptoms during the last year. Furthermore, he had documented recurrent urinary tract infections for a period of 6 months. His IPSS score was 21 and he complained for incomplete bladder emptying, lower abdominal fullness and double voiding. No unusual findings were noted during digital rectal examination. On uroflowmetry, maximum flow rate (Qmax) was 8 mL/s. Ultrasound showed a thick bladder wall with two large BD expanding from either lateral side of the bladder. The maximum diameter was 5 cm and 4 cm for the left and right BD respectively. No dilatation of the upper urinary tract was noted, while the prostate was estimated to be 90 cm3 and the post void residual urine was 100 mL. Serum creatinine was normal, but the PSA was significantly elevated from 4.2 ng/mL two years ago to 7.4 ng/mL. The patient underwent transrectal ultrasound guided 12-core biopsy and the pathology report revealed adenocarcinoma on 4 cores taken from the base in both lobes of the prostate with a Gleason score 7 (3 + 4). Computed tomography (CT) of the abdomen and pelvis was done for staging purposes and to further determine the location of the BD as well as their relationship to the adjacent structures especially the ureters. Flexible cystoscopy was performed to identify the ureteral orifice and to exclude any malignancy of the urothelium inside the BD.
After consulting with the patient RARP was planed in the same setting with RABD. We used a transperitoneal approach similar to that used in RARP as described previously by Nilsson et al. with the addition of the fourth robotic arm placed at the left lateral iliac fossa.3 Initially the sigmoid colon was mobilized. The peritoneum was incised lateral to the left medial umbilical ligament just under the vas deferens. To determine the exact position of the BD we relied on the preoperative imaging and cystoscopy. Using as landmarks the external iliac artery (lateral) the medial umbilical ligament (medial), the vas deferens (above) and the ureter (below) our dissection continued lateral to the bladder. Since the BD was adjacent to the ureteric orifice, our first concern was to identify the left ureter and dissect it free from its attachments to avoid any iatrogenic injury. Visualization of the BD was achieved by retrograde filling and emptying of the bladder. This step was repeated whenever in doubt of the boundaries of the BD. Sharp and blunt dissection was used as needed to dissect free the BD from the overlying tissues. The fourth robotic arm was used to manipulate the BD to all directions and with the additional counter traction from the assistant the plane of dissection was facilitated. The BD was transected at its neck and the bladder wall opening was approximated by 2-zero Biosyin on a CV-25 needle (Covidien, Inc.) in a two layer running fashion (Fig. 1). The same steps were followed for the second BD on the right side (Fig. 2). To verify any leakage from the suture line the bladder was filled once more up to 120 cm3. Furthermore, RARP was conducted in a standard fashion. Preservation of both neurovascular bundles was achieved in a cautery free manner and a watertight anastomosis was completed (Fig. 2). A drain was placed and all specimens were retrieved through an extension of the camera port incision.
Fig. 1.
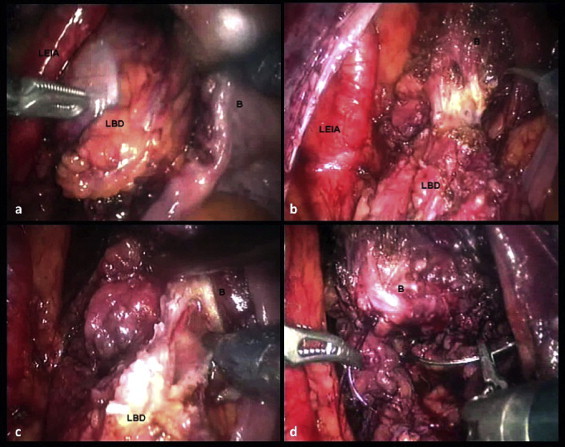
(a) Visualization of the left BD after retrograde filling of the bladder. (b) Dissection and (c) transection of the BD neck. (d) Suturing the bladder opening. LEIA, left external iliac artery; LBD, left bladder diverticulum; B, bladder.
Fig. 2.
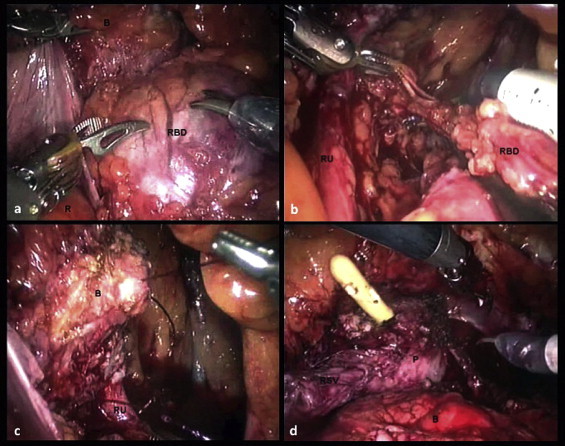
(a) Visualization of the right BD after retrograde filling of the bladder. (b) Transection of the BD neck. (c) Suturing the bladder opening. (d) Dissection the right neurovascular bundle during RARP. B, bladder; RBD, right bladder diverticulum; R, rectum; RU, right ureter; P, prostate; RSV, right seminal vesicle.
Console time was 262 min and the blood loss was minimal. Convalescence was uneventful. The first postoperative day the drain was removed, the patient was mobilized and oral intake was initiated, while the next day the patient was discharged. The catheter was removed 14 days after surgery with previous cystogram. The pathology report confirmed stage pT2c (2009 TNM) adenocarcinoma of the prostate with Gleason score 7 (3 + 4) with negative surgical margins, while the mucosa of both BD revealed squamus transformation of the urothelium with no malignant transformation.
3. Discussion
The first open bladder diverticulectomy was performed by Czerny et al. in 1897, while the laparoscopic counterpart was initially reported by Parra et al. in 1992.2,4 With the advent of the robotic platform, RABD was initially described by Berger et al. in 2006.5 Since then, it has gained popularity among the urologists for procedures requiring complex reconstructive maneuvers, such as BD excision, mainly due to the stereoscopic vision and wristed instrumentation.6,7
Sequential procedures combining BD excision with relive of BOO due to BPH in a minimal invasive approach have been reported in the literature to be safe and effective with comparable results to their open counterparts.8 Furthermore simultaneous interventional treatment for BD in a patient undergoing RARP poses some advantages. In the event of persisting LUTS after RARP, the patients will need a secondary operation and dissection in the previous operated area may be laborious. Secondly, interpretation of urodynamic study in case of incontinence will be misleading due to retrograde filling of the BD. In fact there is no reason to delay surgery for the BD in patients undergoing RARP since experience with RARP will facilitate suturing and reconstruction. The aforementioned advantages have already been recognized in concomitant open radical prostatectomy and bladder diverticulectomy series, while excellent oncological and functional results were remarked.9
Before engaging in a RABD some technical surgical aspects need to be considered.10 To aid BD identification some have proposed endoscopic placement of an additional catheter inside the BD through the urethra.7,11,12 We believe that it is time consuming due to different setup and repositioning of the patient. Since the BD wall is consisted only of bladder mucosa with less stretch resistance than the rest of the bladder wall, retrograde filling makes the BD more prominent than the rest of the bladder. Furthermore, the usually narrow BD neck causes a delayed emptying of the BD during emptying of the bladder, which contributes to better visualization. Hence, the combination of filling and emptying the bladder will be adequate for visualization. Most of the BD are located anterolaterally to the ispilateral ureteric orifice. This makes the ureter prone to iatrogenic injury. Placement of a ureteric stent in advance may simplify identification of the ureter intraoperatively and aid healing in case of inadvertent laceration. Moreover we recommend stenting as a safety measure, meticulous dissection and identification of the ureter beforehand will suffice in most circumstances. It is worth emphasizing that the Retzius space was not dissected and the bladder was not dropped down during the diverticulectomy phase of the procedure. We believe that aided in the identification of the BD especially during the retrograde filling of the bladder. Finally, the fourth arm is of paramount importance, giving the surgeon the control of traction to the BD.
4. Conclusion
Concomitant RABD with RARP is a safe and effective procedure with excellent oncological and functional results. Simultaneous treatment of the two pathologies does not add the complexity of the operation, since skills gained from experience with RARP can easily be implemented to the RABD part of the operation with minor increase of intraoperative time. If further sequela due to recurring LUTS after RARP in patients with BD is to be avoided, this combined surgery should be considered.
Conflict of interest
None.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authors’ contributions
Achilles Ploumidis and Andreas Skolarikos helped in writing the manuscript. Odisseas Sopilidis and Dimitrios Chalikopoulos contributed in data collection. Gerasimos Alivizatos and Peter Wiklund contributed to study design and data analysis.
References
- 1.Rovner E.S. Bladder and urethral diverticula. In: Wein A.J.K.L., Novick A.C., Partin A.W., Peters C.A., editors. Campbell–Walsh urology. 9th ed. Saunders Elsevier; Philadelphia: 2007. pp. 2361–2390. [Google Scholar]
- 2.Fox M., Power R.F., Bruce A.W. Diverticulum of the bladder – presentation and evaluation of treatment of 115 cases. British Journal of Urology. 1962;34(September):286–298. doi: 10.1111/j.1464-410x.1962.tb09459.x. [DOI] [PubMed] [Google Scholar]
- 3.Nilsson A.E., Carlsson S., Laven B.A., Wiklund N.P. Karolinska prostatectomy: a robot-assisted laparoscopic radical prostatectomy technique. Scandinavian Journal of Urology and Nephrology. 2006;40(6):453–458. doi: 10.1080/00365590600911357. [DOI] [PubMed] [Google Scholar]
- 4.Parra R.O., Boullier J.A. Endocavitary (laparoscopic) bladder surgery. Seminars in Urology. 1992;10(November (4)):213–221. [PubMed] [Google Scholar]
- 5.Berger A.D.S.M. Robotic bladder diverticulectomy: initial experience. Journal of Urology Supplements. 2006;75:162. [Google Scholar]
- 6.Altunrende F., Autorino R., Patel N.S., White M.A., Khanna R., Laydner H. Robotic bladder diverticulectomy: technique and surgical outcomes. International Journal of Urology. 2011;8(February) doi: 10.1111/j.1442-2042.2010.02716.x. [DOI] [PubMed] [Google Scholar]
- 7.Myer E.G., Wagner J.R. Robotic assisted laparoscopic bladder diverticulectomy. Journal of Urology. 2007;178(December (6)):2406–2410. doi: 10.1016/j.juro.2007.08.012. discussion 10. [DOI] [PubMed] [Google Scholar]
- 8.Porpiglia F., Tarabuzzi R., Cossu M., Vacca F., Terrone C., Fiori C. Is laparoscopic bladder diverticulectomy after transurethral resection of the prostate safe and effective? Comparison with open surgery. Journal of Endourology. 2004;18(February (1)):73–76. doi: 10.1089/089277904322836721. [DOI] [PubMed] [Google Scholar]
- 9.Skolarikos A., Alivizatos V.I., Chalikopoulos G., Papachristou D., Deliveliotis C.C. Concomitant radical prostatectomy and bladder diverticulectomy: functional and oncological outcome. European Urology Supplements. 2007;6(2):152. [Google Scholar]
- 10.Thiel D.D., Young P.R., Wehle M.J., Broderick G.A., Petrou S.P., Igel T.C. Robotic-assisted bladder diverticulectomy: tips and tricks. Urology. 2011;77(May (5)):1238–1242. doi: 10.1016/j.urology.2010.07.542. [DOI] [PubMed] [Google Scholar]
- 11.Kural A.R., Atug F., Akpinar H., Tufek I. Robot-assisted laparoscopic bladder diverticulectomy combined with photoselective vaporization of prostate: a case report and review of literature. Journal of Endourology. 2009;23(August (8)):1281–1285. doi: 10.1089/end.2008.0674. [DOI] [PubMed] [Google Scholar]
- 12.Shah H.N., Shah R.H., Hegde S.S., Shah J.N., Bansal M.B. Sequential holmium laser enucleation of the prostate and laparoscopic extraperitoneal bladder diverticulectomy: initial experience and review of literature. Journal of Endourology. 2006;20(May (5)):346–350. doi: 10.1089/end.2006.20.346. [DOI] [PubMed] [Google Scholar]


