Abstract
INTRODUCTION
Esophageal achalasia is an uncommon, benign, neurodegenerative disease that induces a transit disorder characterized by incomplete lower esophageal sphincter relaxation.
PRESENTATION OF CASE
A 56-year-old woman with dysphagia was admitted to our hospital. An esophagography revealed flask-type achalasia. Endoscopy revealed a dilated esophagus and some resistance at the esophagogastric junction. We used a capped wound protector, common straight forceps, and hook-type electrocautery to perform transumbilical single incision laparoscopic Heller myotomy with Dor fundoplication (SILHD). The left liver lobe and cardia were pulled by a thread. A 6-cm Heller myotomy of the esophagus was performed with an additional 2-cm myotomy of the gastric wall. Dor fundoplication was performed to cover the exposed submucosa. Intraoperative endoscopy confirmed the adequacy of the myotomy and Dor fundoplication. There were no postoperative complications. An esophagography and an endoscopic examination did not reveal stenosis or reflux at 1-year follow-up, and the patient has been satisfactorily symptom free.
DISCUSSION
LHD is the most accepted surgical treatment for achalasia and has low invasiveness and long-term efficacy. SILHD for achalasia is a new approach and may provide improved cosmetics and less invasiveness compared with those by conventional LHD. The 1-year follow-up results in the present case are the longest reported to date. The evaluation of long-term results in a large-scale study is necessary in future.
CONCLUSION
SILHD can be safe, widely accepted, mid-term minimal invasive and cosmetically superior surgical procedure for achalasia.
Keywords: Single incision laparoscopic surgery, Achalasia
1. Introduction
Esophageal achalasia is a comparatively rare, benign, neurodegenerative disease presents a transit disorder characterized by incomplete relaxation of the lower esophageal sphincter. Patients commonly present the dysphagia, regurgitation, retrosternal pain, and weight loss. Chemical administration, endoscopic treatment with botulinum toxin, pneumatic dilatation, and surgery are performed depending on the disease stage.1 Laparoscopic Heller myotomy with Dor fundoplication (LHD) is preferred because of its low invasiveness and long-term efficacy.2 Single incision laparoscopic surgery (SILS) was recently developed to provide improved cosmetics and less invasiveness, compared to those by standard laparoscopic surgery,3,4 and has been introduced for treatment of several abdominal diseases. We report a case in which single incision laparoscopic Heller myotomy with Dor fundoplication (SILHD) using common instruments resulted in an excellent postoperative course.
2. Presentation of case
A 56-year-old woman complained of dysphagia for approximately 10 years. Symptomatic aggravation, including emesis of food remnants during recumbency, was gradually recognized over the last 5 years. At a primary clinic, lower esophageal transit disorder was revealed on esophageal barium examination, and she was referred to our hospital. She had been prescribed a calcium blocker as an initial treatment for achalasia at clinic.
Abdominal radiography revealed the disappearance of a gastric air bubble. Barium esophagography revealed a flask-type dilatation of the esophageal body to a maximum of 6.0 cm transversely. Peristalsis was not observed, and stagnation of barium occurred (Fig. 1). Liquid was pooled within the interior. Esophageal gastroscopy showed that the esophagus was dilated with food remnants. Esophageal diverticula and neoplastic lesions were not observed. Chest computed tomography showed that the lower esophageal wall was thickened and expanded.
Fig. 1.

Barium esophagography revealed a flask-type dilatation to a maximum of 6.0 cm transversely.
During the clinical course, the patient's body weight decreased more than 5 kg (Eckardt score, 2 points); dysphagia occurred with every meal (3 points); retrosternal pain was experienced occasionally (1 point); regurgitation was frequently noted during recumbency (2 points). Her total Eckardt score was 8 points and initial treatment with a calcium blocker was not effective for the management of digestive symptoms. On the basis of these findings, stage III achalasia was diagnosed. Proposed achalasia therapy, including pneumatic dilatation, endoscopic treatment, and surgery, was explained; after obtaining an informed consent, SILHD was performed.
The surgery was started with the patient in the spine position. General anesthesia was used together with epidural analgesics. Her umbilicus was incised 2.5 cm vertically, and a capped wound protector (WRAPDISK®, Hakko Co. Ltd., Nagano, Japan) was applied. Three 5 mm cannulas were used in the protector. A 5 mm flexible scope, hook-type electrocautery, and common straight forceps were primarily used (Fig. 2). Pneumoperitoneum was maintained by supply of carbon dioxide at 8 mmHg. The left liver lobe was lifted using a silicon drain that was attached by a silk thread to the dermis. Nylon thread was stitched transabdominally at the anterior wall of the cardia to pull the abdominal esophagus. A hook-type electrocautery was used to divide the esophageal sphincter from esophagogastric junction at the anterior wall. Myotomy was performed with an esophagus side of 6 cm and a gastric side of 2 cm (Fig. 3A). After myotomy, endoscopy confirmed that the esophagogastric junction was sufficiently expanded, and the endoscope could be inserted into the stomach without resistance. Leakage of the endoscopic supply of air, which is a sign of mucosal tear, was not identified. Dor fundoplication was subsequently performed. The short gastric vessel was not divided because there was no resistance from the stomach wall. Eight sutures with a polypropylene thread to cover the exposed submucosa ware used to fix the edge of the esophageal sphincter and fundic wrap (Fig. 3B). Finally, endoscopy confirmed the absence of large aperture and stenosis at the junction. The drain was not inserted. The operative time was 248 min and blood loss was minimal.
Fig. 2.
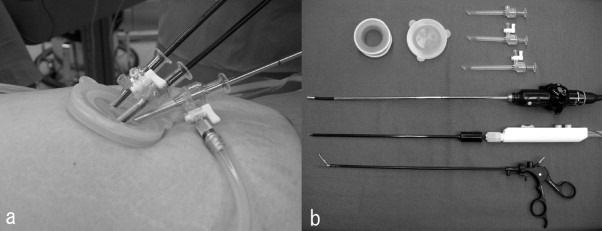
Operative instruments. (a) Capped wound protector at the umbilicus and (b) reusable instruments; wound protector, cap, cannulas, 5 mm flexible scope, electrocautery, and forceps.
Fig. 3.
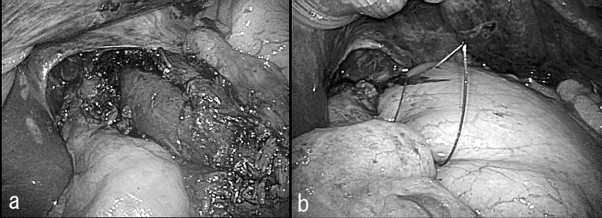
Intraoperative view. (a) Heller myotomy was performed with an esophagus side of 6 cm and a gastric side of 2 cm and (b) subsequently anti-reflux procedure of Dor fundoplication was performed to cover the exposed submucosa.
There were no postoperative complications. Liquid passage was smooth and gastroesophageal reflux was not observed on esophagography on the second postoperative day. Oral intake was started after esophagography. Her subjective symptoms completely disappeared.
At 1-year follow-up, she did not show any symptoms and was satisfied with her postoperative course. Esophagography showed that the barium passage was smooth and there was no esophageal reflux was not seen (Fig. 4). Esophagitis, stenosis, and an excessive aperture were not detected endoscopically (Fig. 5).
Fig. 4.

Postoperative esophagography revealed that liquid passage was smoothly and gastroesophageal reflux was not observed.
Fig. 5.
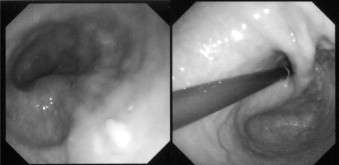
Postoperative endoscopy did not show esophagitis, stenosis, or excessive aperture.
3. Discussion
For esophageal achalasia, the most effective treatments are pneumatic dilatation and LHD. Pneumatic dilatation is generally accepted as a nonsurgical treatment and has achieved 74–90% symptomatic improvement.1 Laparoscopic Heller myotomy, which was reported in 1991, is less invasive than open laparotomy, and LHD with an anti-reflex procedure become the standard surgical treatment. Long-term results of LHD have been excellent, with a 73–100% improvement rate.1,5–8 However, a recent large-scale, randomized, clinical trial in Europe did not show a significant difference in the results between an endoscopic pneumodilatation group and a LHD group within 2 years.9 The long-term efficacy of these treatments for esophageal achalasia remains controversial.
SILS, by definition, involves only one incised wound at the umbilicus in the pursuit of minimal invasiveness. The first SILS for appendectomy was reported in 1992,3 and SILS for cholecystectomy was reported in 1997.4 Over the next decade, the worldwide use of SILS increased and has been applied to many abdominal diseases. Several controlled trials of SILS and conventional laparoscopic surgery have reported superior results with respect to pain, recovery, and cosmetics compared with those obtained by conventional laparoscopic surgery.10,11 In contrast, some studies have concluded that SILS has disadvantages of prolonged operative time and increased complications.12 Longer operative times might result from a difficult learning curve. The operative time of SILS was significantly different in 9–75 experiences.13–15 With respect to the learning curve for SILS, the procedures may be learned more rapidly if surgeons have previous laparoscopic surgical experiences. In our institution, SILHD was performed in the 107th case treated by SILS procedure of appendectomy, splenectomy, colorectal surgery, gastrectomy and transabdominal preperitoneal hernioplasty; therefore, significant previous relevant experience had been gained. In previous literatures, the SILHD operative time has ranged from 117 to 273 min and was longer than that for conventional LDH. 16.7% of the patients who underwent SILHD were required additional ports because of technical difficulty. SILHD might be more technically advanced procedure.
In single incision laparoscopic surgery, we usually use standard reusable instruments that are same in conventional laparoscopic surgery. In the past reports, the retractors that was required other incision were used.16,17 Moreover specialized instruments like several access port, bending or articulating forceps, and disposable retraction tool are produced for single incision laparoscopic surgery. However these things have not been popular because they are costly and are required to learn the manipulation. We think it is simple, widely acceptable, economical, technically feasible, and less stressful for surgeons to perform operation with familial tools.
Two processes are involved in SILHD. One is the division of the abdominal esophagus and the precise myotomy of the esophageal sphincter. In this procedure, it is important to maintain a good operative view of the right upper abdomen. We lifted the left liver lobe atraumatically by a thread with a silicon drain and pulled the abdominal esophagus using a thread fixed to the cardia. Our organ-lifting method is the same as that used in conventional laparoscopic surgery. Heller myotomy, which was involves incision of the internal sphincter using a hook-type electrocautery, must be performed very carefully to prevent esophageal mucosa tear. In addition, intraoperative endoscopy is very useful for confirming relief of achalasia and mucosal damage. The second process is Dor fundoplication. If there is strong resistance from the stomach wall, small gastric vessels should be divided. This area is at a long distance and very deep from the umbilicus in both the horizontal and vertical planes; however, we think that division of small vessels is not very difficult from our experiences with single incision laparoscopic splenectomy. Suturing in SILS provides experience for peritoneal closure in single incision laparoscopic hernioplasty. Suturing in Dor fundoplication was comparatively easy because the rotation axis while handling the needle was parallel with the esophagus. Surgeons sufficiently experienced in laparoscopic surgery and SILS might perform SILHD. A potential problem is that SILS may be more difficult to perform in heavier or taller patients because it is difficult for common instruments to reach the operative area from the umbilicus.
In previous reports, the procedure-specific complications in SILHD were not increased in the short-term, however, there are no mentions about the mid-term result after operation.16–19 It is necessary to evaluate postoperative course because SILHD is new approach. We confirmed there were no esophagitis, gastroesophageal reflux, stenosis and recurrence of achalasia by endoscopy and esophagography after SILHD. The 1-year follow up results in our case are the longest reported to date. Our report will support many surgeons to consider SILHD for achalasia. Future studies should evaluate long-term results for feasibility, safety, and effectiveness in a large-scale study.
4. Conclusion
SILHD can be safe, widely accepted, mid-term minimal invasive and cosmetically superior surgical procedure for achalasia.
Conflict of interest statement
None.
Funding
None.
Ethical approval
A written informed consent was obtained by the patient for publication of this report and accompanying images.
Author contributions
Hidehisa Yamada, M.D. contributed to the conception and design, gathering of data, review of patient chart, drafting the case, critical revisions, and final approval of the version to be published. Tomoyuki Yano, M.D. contributed to the conception and design, critical revisions, final approval of the version to be published.
References
- 1.Richter J.E., Boeckxstaens G.E. Management of achalasia: surgery or pneumatic dilation. Gut. 2011;60:869–876. doi: 10.1136/gut.2010.212423. [DOI] [PubMed] [Google Scholar]
- 2.Shimi S., Nathanson L.K., Cuschieri A. Laparoscopic cardiomyotomy for achalasia. Journal of the Royal College of Surgeons of Edinburgh. 1991;36:152–154. [PubMed] [Google Scholar]
- 3.Pelosi M.A., Pelosi M.A., 3rd Laparoscopic appendectomy using a single umbilical puncture (minilaparoscopy) Journal of Reproductive Medicine. 1992;37:588–594. [PubMed] [Google Scholar]
- 4.Navarra G., Pozza E., Occhionorelli S., Carcoforo P., Donini I. One-wound laparoscopic cholecystectomy. British Journal of Surgery. 1997;84:695. [PubMed] [Google Scholar]
- 5.Campos G.M., Vittinghoff E., Rabl C., Takata M., Gadenstätter M., Lin F. Endoscopic and surgical treatments for achalasia: a systematic review and meta-analysis. Annals of Surgery. 2009;249:45–57. doi: 10.1097/SLA.0b013e31818e43ab. [DOI] [PubMed] [Google Scholar]
- 6.Zaninotto G., Costantini M., Rizzetto C., Zanatta L., Guirroli E., Portale G. Four hundred laparoscopic myotomies for esophageal achalasia: a single centre experience. Annals of Surgery. 2008;248:986–993. doi: 10.1097/SLA.0b013e3181907bdd. [DOI] [PubMed] [Google Scholar]
- 7.Kilic A., Schuchert M.J., Pennathur A., Gilbert S., Landreneau R.J., Luketich J.D. Long-term outcomes of laparoscopic Heller myotomy for achalasia. Surgery. 2009;146:826–833. doi: 10.1016/j.surg.2009.06.049. [DOI] [PubMed] [Google Scholar]
- 8.Chen Z., Bessell J.R., Chew A., Watson D.I. Laparoscopic cardiomyotomy for achalasia: clinical outcomes beyond 5 years. Journal of Gastrointestinal Surgery. 2010;14:594–600. doi: 10.1007/s11605-010-1158-2. [DOI] [PubMed] [Google Scholar]
- 9.Boeckxstaens G.E., Annese V., des Varannes S.B., Chaussade S., Costantini M., Cuttitta A. European Achalasia Trial Investigators. Pneumatic dilation versus laparoscopic Heller's myotomy for idiopathic achalasia. New England Journal of Medicine. 2011;364:1807–1816. doi: 10.1056/NEJMoa1010502. [DOI] [PubMed] [Google Scholar]
- 10.Champagne B.J., Papaconstantinou H.T., Parmar S.S., Nagle D.A., Young-Fadok T.M., Lee E.C. Single-incision versus standard multiport laparoscopic colectomy: a multicenter, case-controlled comparison. Annals of Surgery. 2012;255:66–69. doi: 10.1097/SLA.0b013e3182378442. [DOI] [PubMed] [Google Scholar]
- 11.Lee S.W., Milsom J.W., Nash G.M. Single-incision versus multiport laparoscopic right and hand-assisted left colectomy: a case-matched comparison. Diseases of the Colon and Rectum. 2011;54:1355–1361. doi: 10.1097/DCR.0b013e31822c8d41. [DOI] [PubMed] [Google Scholar]
- 12.Ma J., Cassera M.A., Spaun G.O., Hammill C.W., Hansen P.D., Aliabadi-Wahle S. Randomized controlled trial comparing single-port laparoscopic cholecystectomy and four-port laparoscopic cholecystectomy. Annals of Surgery. 2011;254:22–27. doi: 10.1097/SLA.0b013e3182192f89. [DOI] [PubMed] [Google Scholar]
- 13.Gawart M., Dupitron S., Lutfi R. Laparoendoscopic single-site gastric bands versus standard multiport gastric bands: a comparison of technical learning curve measured by surgical time. American Journal of Surgery. 2012;203:327–330. doi: 10.1016/j.amjsurg.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 14.Hernandez J., Ross S., Morton C., McFarlin K., Dahal S., Golkar F. The learning curve of laparoendoscopic single-site (LESS) cholecystectomy: definable, short, and safe. Journal of the American College of Surgeons. 2010;211:652–657. doi: 10.1016/j.jamcollsurg.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 15.Solomon D., Bell R.L., Duffy A.J., Roberts K.E. Single-port cholecystectomy: small scar, short learning curve. Surgical Endoscopy. 2010;24:2954–2957. doi: 10.1007/s00464-010-1070-6. [DOI] [PubMed] [Google Scholar]
- 16.Barry L., Ross S., Dahal S., Morton C., Okpaleke C., Rosas M. Laparoendoscopic single-site Heller myotomy with anterior fundoplication for achalasia. Surgical Endoscopy. 2011;25:1766–1774. doi: 10.1007/s00464-010-1454-7. [DOI] [PubMed] [Google Scholar]
- 17.Nakajima J., Sasaki A., Obuchi T., Baba S., Umemura A., Wakabayashi G. Single-incision laparoscopic Heller myotomy and Dor fundoplication for achalasia: report of a case. Surgery Today. 2011;41:1543–1547. doi: 10.1007/s00595-010-4533-4. [DOI] [PubMed] [Google Scholar]
- 18.Kobayashi M., Mizuno M., Sasaki A., Arisue A., Akiyama S., Wakabayashi G. Single-port laparoscopic Heller myotomy and Dor fundoplication: initial experience with a new approach for the treatment of pediatric achalasia. Journal of Pediatric Surgery. 2011;46:2200–2203. doi: 10.1016/j.jpedsurg.2011.07.027. [DOI] [PubMed] [Google Scholar]
- 19.Yano F., Omura N., Tsuboi K., Hoshino M., Yamamoto S.R., Kashiwagi H. Single-incision laparoscopic Heller myotomy and Dor fundoplication for achalasia: report of a case. Surgery Today. 2012;42:299–302. doi: 10.1007/s00595-011-0089-1. [DOI] [PubMed] [Google Scholar]


