Abstract
INTRODUCTION
Osteosarcoma is the most common primary malignant tumour of bone and commonly involved sites are the distal femur, proximal tibia, and humerus. Osteosarcoma of proximal femur usually arises at the metaphysis and articular cartilage acts as a relative barrier to tumour spread, with extension into the hip joint being extremely rare.
PRESENTATION OF CASE
A previously fit and well sixteen-year-old male presented with a 2 month history of right hip pain and a limp. Plain radiographs and magnetic resonance imaging (MRI) showed an expansile lesion in the right femoral neck, extending 16 cm distally from the proximal femoral articular surface through the intertrochanteric region into the upper right femoral shaft. There was also clear evidence of intra-articular extension into the acetabulum.
DISCUSSION
Endoprosthetic replacement following resection is a good treatment option for proximal femoral tumours due to the low complication rate and achievement of good postoperative function. However, treatment of a proximal femoral lesion with intra-articular involvement by prosthetic reconstruction is challenging. We report a patient who presented with osteosarcoma of the proximal femur extending into the hip joint and describe the technique of en-bloc extra-articular resection of the acetabulum and proximal femur with reconstruction using a custom made prosthesis.
CONCLUSION
We conclude that extra-articular resection and endoprosthetic reconstruction using a coned hemi-pelvic implant with fluted stem and a modular femoral implant is a useful treatment option in the management of a proximal femoral lesion involving the hip-joint. It allows adequate tumour clearance and stable reconstruction for rapid post-operative recovery with early mobilisation.
Keywords: Osteosarcoma, Intra-articular extension, Endoprosthesis, Proximal femur
1. Introduction
Osteosarcoma is the most common primary malignant tumour of bone and commonly involved sites are the distal femur, proximal tibia, and humerus.1 Other significant locations are the proximal femur, pelvis, skull, and jaw. Osteosarcoma of the proximal femur usually arises at the metaphysis. Articular cartilage acts as a relative barrier to tumour spread, and extension into the hip joint is extremely rare.2
For tumours confined to the proximal femur, endoprosthetic replacement following tumour resection is a good treatment option due to its low complication rate and good postoperative function.3–5 However, treatment of a proximal femoral lesion with intra-articular involvement by prosthetic reconstruction is challenging. The need for adequate excision margins and the anatomically complex pelvis means that reconstruction procedures are associated with high rates of morbidity and mortality, and poor functional outcome.6
To date, a technique of complete endoprosthetic reconstruction of a proximal femoral osteosarcoma involving the hip joint has not been described. We report a patient who presented with osteosarcoma of the proximal femur extending into the hip joint. We describe the technique of en-bloc extra-articular resection of the acetabulum and proximal femur with reconstruction using a custom made prosthesis.
The authors have obtained the patient's informed written consent for print and electronic publication of this case report.
2. Case report
A previously fit and well sixteen-year-old male presented with a 2 month history of right hip pain and a limp. Plain radiographs of the pelvis, hips and proximal femur showed mixed osteopenic and sclerotic areas in the right proximal femur from the growth plate distally for approximately 11 cm (Fig. 1). Magnetic resonance imaging (MRI) showed an expansile lesion in the right femoral neck, extending 16 cm distally from the proximal femoral articular surface through the intertrochanteric region into the upper right femoral shaft. The lesion was seen to breach the cortex and extend into the soft tissue, infiltrating the quadratus femoris muscle medially and superiorly, and infiltrating the vastus lateralis muscle laterally. There was also clear evidence of intra-articular extension into the acetabulum but no evidence of neurovascular involvement (Fig. 2). Staging computerised tomography (CT) and bone scan confirmed this to be an isolated lesion and CT guided biopsy confirmed an osteosarcoma.
Fig. 1.

Plain radiograph demonstrating the lesion in the proximal femur.
Fig. 2.
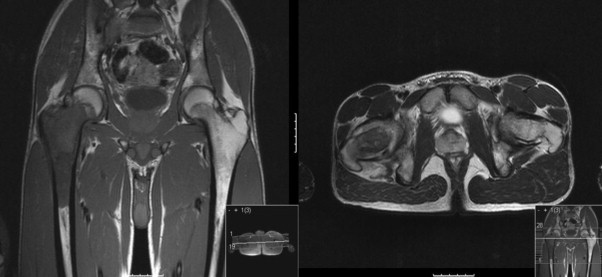
Coronal and sagittal MRI demonstrating the extent of the lesion.
Initial management consisted of 6 cycles of neoadjuvant MAP (Methotrexate, Adriamycin, cisPlatin) chemotherapy as per the Euramos 1 Trial,7 followed by an extra-articular resection of the proximal femur and acetabulum and reconstruction with a coned hemi-pelvic implant and proximal femoral endoprosthesis as described below. Post-operatively the patient was managed in slings and springs, and following muscle control, allowed to mobilise bearing part of his weight on day 3. Follow-up after one year showed satisfactory results with no evidence of tumour recurrence or complications like infection or dislocation. The joint was stable with no limb length discrepancy and the patient able to fully weight bear and routinely perform moderate activities.
3. Surgical technique
With the patient supine a vertical groin incision was made over adductor longus. Deep dissection was performed and the obturator nerve and vessels were identified and protected. An ischial osteotomy was made under fluoroscopic guidance using osteotomes (Fig. 3). The incision was then closed in layers.
Fig. 3.
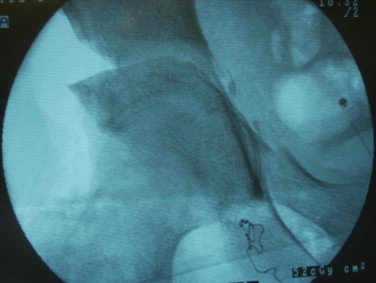
Intraoperative fluoroscopic imaging demonstrating the ‘mobilised’ hip after the iliac and pubic osteotomies.
A Somerville bikini incision was then made over the ilium. The abductor muscles were reflected subperiosteally from iliac bone distally to the capsule of the hip joint. Tensor fascia lata was separated from sartorius inferior to the anterior superior iliac spine. The reflected head of rectus femoris was separated from the acetabulum and capsule. Iliac and pubic rami osteotomies were performed and the hip was mobilised (Fig. 4). The incision was then closed in layers.
Fig. 4.
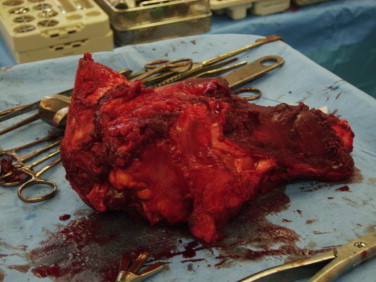
Macroscopic appearance of the tumour after the extra-articular resection.
The patient was then turned to a lateral position. A lateral incision was made and using an anterior and posterior approach, the hip joint was mobilised and the proximal femur transected 18 cm distal from the greater trochanter. An extra-articular resection of the hip joint and proximal femur was therefore performed (Fig. 5).
Fig. 5.

Post-operative radiograph demonstrating the extent of excision and the endoprosthetic reconstruction.
The ilium was prepared using a custom reamer. An uncemented, custom-made coned hemi-pelvic implant with fluted stem (Stanmore Implants Worldwide Ltd., Stanmore, United Kingdom) was inserted into the iliac cavity adjacent to the sacro-iliac joint under fluoroscopic guidance. Two AO cancellous screws were inserted into the ilium to provide a frame for a cement block to be applied around the implant. A polyethylene liner was cemented into the shell. A modular femoral endoprosthetic implant was constructed (Fig. 6). A Trevira tube8 (mesh tube used for re-attachment of soft tissues) was applied to the prosthetic femoral stem and muscles reattached to the tube and incision closed.
Fig. 6.
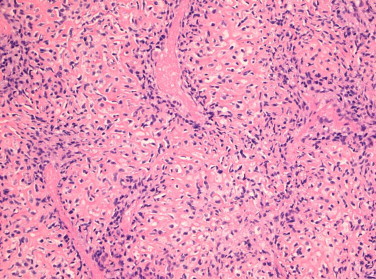
Histological photo of the tumour showing severely atypical osteoblasts embedded within lace-like osteoid matrix (H&E stain, 4× magnification).
4. Discussion
Articular cartilage provides a structural barrier to tumour invasion and hip joint involvement by lesions of the proximal femur is uncommon.1,2 Endoprosthetic replacement of a lesion confined to the proximal femur is a good option for reconstruction after tumour resection due to its low complication rate and good postoperative function.3–5
However, surgical resection of a malignant lesion involving the acetabulum is challenging and controversial. Aiming for adequate excision margins via an extra-articular approach, and an adequate reconstruction is usually associated with significant morbidity and mortality, and variable functional outcome.
A number of peri-acetabular reconstruction procedures exist. Arthrodesis and arthrosis have lower rates of morbidity but are frequently associated with a shortened limb and poor function.6,9 Anatomic reconstruction with biological techniques such as allografts or re-implantation of the excised bone after autoclaving or irradiation have high rates of infection, non-union, tumour recurrence, fracture and dislocation.10,11
Peri-acetabular resection and endoprosthetic reconstruction for tumours of the acetabulum is well established12 but associated with high morbidity. The saddle prosthesis, originally developed for revision of failed total hip arthroplasty, has been used in recent years as a reconstruction device for large bone defects following resection of peri-acetabular malignant tumours.13–15 The implant transmits load between iliac bone and bare polish chrome-cobalt. Early clinical and radiological results indicate that a useful and stable articulation can be achieved. However, commonly encountered complications are deep infection, dislocation and peripheral nerve palsy.16,17
Jaiswal et al. reported a series on 98 patients with peri-acetabular tumours treated by resection and reconstruction with custom-made saddle prosthesis and found this procedure to be associated with significant morbidity and advised that patients be carefully selected and informed of the high complication rates pre-operatively.12
Falkinstein et al. reported a retrospective study of 21 patients who underwent limb salvage following type II pelvic resection and endoprosthetic reconstruction. The prosthesis was designed to use the remaining part of the ilium to support a horizontally placed acetabular component secured with internal fixation and bone cement. The most common complications encountered were deep infection, superficial wound infections, and dislocation.18
To date there has been no report on the technique of extra-articular resection and complete endoprosthetic reconstruction of a proximal femoral osteosarcoma involving the hip joint. Nakamura describes the use of an extra-articular resection of a proximal femoral tumour involving the hip joint in 1 case of Ewing's sarcoma and 2 cases of osteosarcoma. Proximal resection was achieved via a triple osteotomy. The cartilage was shaved off the pelvic aspect of lesion, and the bone soaked in cisPlatin, and reimplanted with reconstruction plates to fix it to the pelvis.19 His results showed that between 24 and 37 months postoperatively all three cases experienced hip dislocations and two cases experienced infection and average functional evaluation score using ISOLS (International Symposium on Limb Salvage) criteria was 71% (range: 50–83%).
With the intention of complete endoprosthetic replacement, the major challenge and goal, in this case, was to achieve biomechanical stability of the construct and minimise the risk of infection and dislocation.
Following the excision of large tumours and the resultant loss of bone stock, achieving mechanical stability of the prosthesis is difficult. A potential solution is to use a conical fluted stem. The design of the conical fluted stem allows it to flex and load the proximal body with complete distal fixation and exceptional rotational stability. The successful use of conical fluted stems use in primary and revision total hip replacement with significant bone loss has been well described.20–22 Bruns et al. have recently reported on the outcome of 25 patients in whom a MUTARS (modular tumour and revision system) mega prosthesis with a conical fluted stem was used in the treatment of bone tumours. After a mean follow-up period of 2.5 years they showed no radiological evidence of stem loosening or subsidence with low rates of dislocation and support the use of a fluted stem implant on a background of precise pre-operative planning.23
Further benefits of this technique include not requiring allograft reconstruction or re-implantation of an excised segment which is associated with significant infection rates10,13 and it allows the use of the Trevira tube as described by Gosheger et al.,8 which allows soft tissue reattachment without increasing the risk of infection.
We conclude that extra-articular resection and endoprosthetic reconstruction using a coned hemi-pelvic implant with fluted stem and a modular femoral implant is a useful treatment option in the management of a proximal femoral lesion involving the hip-joint. It allows adequate tumour clearance and stable reconstruction for rapid post-operative recovery with early mobilisation.
Conflict of interest statement
None.
Funding
None.
Ethical approval
Obtained.
Author's contributions
Mr. Emeka Oragui MA MRCS involved in study design, data collection and writing. Mr. Madhusudhan Raj Nannaparaju MBBS MRCSEd helped in data analysis and writing. Mr. Kesavan Sri-Ram FRCS and Mr. Wasim Khan FRCS contributed in data collection and analysis. Mr. Hashemi Nejad FRCS involved in guidance on writing and supervision and Mr. John Skinner FRCS contributed to the guidance on writing and supervision.
Contributor Information
E. Oragui, Email: emekaoragui@hotmail.com.
M. Nannaparaju, Email: nmsraj@gmail.com.
References
- 1.Moser R.P., Jr. Springer; Berlin/Heidelberg: 2002. Skeletal radiology. ISSN: 0364-2348 (Print), ISSN: 1432-2161 (Online) [Google Scholar]
- 2.Quan G.M.Y. Resistance of epiphyseal cartilage to invasion by osteosarcoma is likely to be due to expression of antiangiogenic factors. Pathobiology. 2002/2003;70:361–367. doi: 10.1159/000071277. [DOI] [PubMed] [Google Scholar]
- 3.Kabukcuoglu Y., Grimer R.J., Tillman R.M., Carter S.R. Endoprosthetic replacement for primary malignant tumors of the proximal femur. Clinical Orthopaedics and Related Research. 1999;358:8–14. [PubMed] [Google Scholar]
- 4.Bickels J., Malawer M.M., Meller I., Kollender Y., Rubert K.M., Henshaw R.M. Proximal and total femur resections with endoprosthetic reconstruction. Surgical technique and prosthetic survivorship: analysis of 64 patients. Presented at the 10th international symposium of the international society of limb salvage (ISOLS); Cairns, Australia, 11–14 April; 1999. [Google Scholar]
- 5.Dobbs H.S., Scales J.T., Wilson J.N. Endoprosthetic replacement of the proximal femur and acetabulum. Journal of Bone and Joint Surgery. 1981;63B:219–224. doi: 10.1302/0301-620X.63B2.7217145. [DOI] [PubMed] [Google Scholar]
- 6.Malawer M.M. Musculoskeletal cancer surgery. Periacetabular Resections. 2001 [Chapter 28] [Google Scholar]
- 7.EURAMOS 1: a randomized trial of the European and American Osteosarcoma Study Group to optimize treatment strategies for resectable osteosarcoma based on histological response to pre-operative chemotherapy (ISRCTN67613327).
- 8.Gosheger G., Hillmann A., Lindner N., Rodl R., Hoffmann C., Burger H. Soft tissue reconstruction of mega prostheses using a trevira tube. Clinical Orthopaedics and Related Research. 2001;393:264–271. doi: 10.1097/00003086-200112000-00030. [DOI] [PubMed] [Google Scholar]
- 9.Tait R.J., Selmer K., Neff J.R. Pelvic resection: oncologic and functional outcome. In: Tan S.K., editor. Limb salvage: current trends. Proceedings of the international symposium ISOLS Singapore; 1993. pp. 299–304. [Google Scholar]
- 10.Harrington K.D. The use of hemipelvic allografts or autoclaved grafts for reconstruction after wide resections of malignant tumors of the pelvis. Journal of Bone and Joint Surgery-American Volume. 1992;74(3):331–341. [PubMed] [Google Scholar]
- 11.Kim H.S., Kim K.J., Han I., Oh J.H., Lee S.H. The use of pasteurized autologous grafts for periacetabular reconstruction. Clinical Orthopaedics and Related Research. 2007;464(November):217–223. doi: 10.1097/BLO.0b013e3181583ae4. [DOI] [PubMed] [Google Scholar]
- 12.Jaiswal Peri-acetabular resection and endoprosthetic reconstruction for tumours of the acetabulum. Journal of Bone and Joint Surgery. 2008;90-B(9):1222–1227. doi: 10.1302/0301-620X.90B9.20758. [DOI] [PubMed] [Google Scholar]
- 13.Nieder E., Flson R.A., Engelbrecht E., Kasselt M.R., Keller A., Steinbrink K. The saddle prosthesis for salvage of the destroyed acetabulum. Journal of Bone and Joint Surgery. British Volume. 1990;72:1014–1022. doi: 10.1302/0301-620X.72B6.2246283. [DOI] [PubMed] [Google Scholar]
- 14.Kitagawa Y. Pelvic reconstruction using saddle prosthesis following limb salvage operation for periacetabular tumour. Journal of Orthopaedic Surgery. 2006;14(2):155–162. doi: 10.1177/230949900601400210. [DOI] [PubMed] [Google Scholar]
- 15.Aboulafia A.J., Buch R., Matthews J., Li W., Malawer M.M. Reconstruction using the saddle prosthesis following excision of primary and metastatic periacetabular tumours. Clinical Orthopaedics and Related Research. 1995;314:203–213. [PubMed] [Google Scholar]
- 16.Cottias P., Jeanrot C., Vinh T.S., Tomeno B., Anract P. Complications and functional evaluation of 17 saddle prostheses for resection of periacetabular tumours. Journal of Surgical Oncology. 2001;78:90–100. doi: 10.1002/jso.1127. [DOI] [PubMed] [Google Scholar]
- 17.Renard A.J., Veth R.P., Schreuder H.W. The saddle prosthesis in pelvic primary and secondary musculoskeletal tumours: functional results at several postoperative intervals. Archives of Orthopaedic and Trauma Surgery. 2000;120:188–194. doi: 10.1007/s004020050041. [DOI] [PubMed] [Google Scholar]
- 18.Falkinstein Y. Reconstruction of type II pelvic resection with a new peri-acetabular reconstruction endoprosthesis. Journal of Bone and Joint Surgery. British Volume. 2008;90(3):371–376. doi: 10.1302/0301-620X.90B3.20144. [DOI] [PubMed] [Google Scholar]
- 19.Nakamura S., Kusuzaki K., Murata H., Takeshita H., Hirata M., Hashiguchi S., Hirasawa Y. Orthopedics. 2001;24(5):445–447. doi: 10.3928/0147-7447-20010501-11. [DOI] [PubMed] [Google Scholar]
- 20.McInnis D.P., Horne G., Devane P.A. Femoral revision with a fluted, tapered, modular stem. Journal of Arthroplasty. 2006;21(3):372–380. doi: 10.1016/j.arth.2005.08.022. [DOI] [PubMed] [Google Scholar]
- 21.Park Y.S. Revision total hip arthroplasty using a fluted and tapered modular distal fixation stem with and without extended trochanteric osteotomy. Journal of Arthroplasty. 2007;22(7):993–999. doi: 10.1016/j.arth.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 22.Wagner H., Wagner M. Konische Schaftverankerung zementfreier Hüftprothes Primärimplantation und Prothesenwechsel. In: Morscher E.W., editor. Endoprothetik. Springer; Berlin, Heidelberg: 1995. pp. 278–288. [Google Scholar]
- 23.Bruns J. Cementless fixation of megaprostheses using a conical fluted stem in the treatment of bone tumours. Journal of Bone and Joint Surgery. British Volume. 2007;89(8):1084–1087. doi: 10.1302/0301-620X.89B8.19236. [DOI] [PubMed] [Google Scholar]


