Introduction
Over the past few decades, several advances have been made in our knowledge of the genetic basis of diseases, prompting particular attention to the prevention and control of this determinant and to the adequate management of those affected or at risk of developing genetic conditions.
The causes of genetic disease are manifold, and a variety of approaches are thus required for their prevention and to ensure better care of patients and families. In 2000, the World Health Organization (WHO) proposed that interventions for prevention and control of genetic disorders and congenital malformations should be added to the primary health care (PHC) framework (WHO 2000).
The main characteristic of PHC is its status as the first contact to the health system, providing comprehensive, continuous care over time and coordinating the care received by individuals and families at the various points of care throughout the health system. Other defining characteristics of PHC include its family- and community-oriented nature and cultural competence (Starfield 1992).
At the interface between genetics and PHC is the field of community genetics. In 1998, Leo ten Kate defined community genetics as “bringing genetic services to the community as a whole.” (ten Kate 1998) The author later expanded this definition, describing community genetics as “the art and science of the responsible and realistic application of health and disease-related genetics and genomics knowledge and technologies in human populations and communities to the benefit of individuals therein. Community genetics is multi-, inter- and transdisciplinary and aims to maximize benefits while minimizing the risk of harm, respecting the autonomy of individuals and ensuring equity” (ten Kate et al. 2010).
Within this context, several efforts have been made in the direction of integrating basic knowledge of genetics into the framework of PHC. Education is viewed as the key for preparing primary care providers for a reality in which genetics will be present in the daily routine of health care and disease prevention (Khoury 2003). Genetic diseases contribute significantly to the population-wide disease burden, and primary care providers have an important role to play in their prevention and in the identification of patients that could benefit from referral to medical genetics services, as they will remain responsible for the care of these patients throughout the life course (Burke and Emery 2002).
In 2009, the Brazilian government published its national policy for comprehensive clinical genetics care (Brasil 2009). This policy includes both specialty medical genetics care and primary care. In the latter setting, the policy provides for identification and follow-up of families with conditions related to congenital anomalies and genetically determined diseases.
The objective of this study was to ascertain whether implementation of a medical genetics education program produced for primary care providers could contribute to the integration of concepts and attitudes related to the identification, management, and prevention of congenital malformations and genetic diseases into the care provided at primary health care units.
Materials and methods
Setting
The municipality of Porto Alegre, located in Southern Brazil, has a population of approximately 1,400,000 (IBGE 2011). There are 56 Basic Health Care Unities in the municipality, two established genetics services, and a referral center for neonatal screening. Twelve of the Basic Health Care Unities are affiliated with Grupo Hospitalar Conceição (GHC), which has over 30 years’ experience in primary care and served as the model for the current Brazilian Family Health Strategy, which was implemented nationwide from 1994. The Medical Genetics Service at Hospital de Clínicas de Porto Alegre is recognized throughout Latin America as a leading center for the diagnosis and treatment of genetic diseases, and, since 2004, has been a WHO Collaborating Centre for the Development of Medical Genetics Services in Latin America.
Design of the educational program
The content and format of the program were idealized by investigators affiliated to the Medical Genetics Services of Hospital de Clínicas de Porto Alegre (SGM/HCPA). Three meetings were held with the project investigators—as well as other SGM/HCPA staff and students interested in the topic—to define which subjects would be addressed during lectures, the duration of the program, and the assessment method.
Once the topics had been defined, a questionnaire designed to assess their adequacy for a medical genetics educational program for primary care providers was distributed to participants of the 22nd Brazilian Congress on Medical Genetics.
The content chosen for presentation in the program included: basic concepts in medical genetics (lecture 1); familial genetic analysis (lecture 2); teratogens and prevention of birth defects (lecture 3); genetics of mental disability (lecture 4); inborn errors of metabolism (IEM) and neonatal screening (lecture 5); cancer genetics (lecture 6); genetics and common adult chronic diseases (lecture 7); and pre-conception counseling/prenatal diagnosis (PND), and genetic counseling (lecture 8). Ethical aspects of genetics and the use of information resources (such as relevant websites and hotlines) were presented during lectures as appropriate. Due to the advanced content of lectures, the decision was made to limit participation in the program to health care providers with a graduated education level. Each lecture was 60 to 90 min in duration.
The program was presented to leaders of the Grupo Hospitalar Conceição Community Health Service (SSC/GHC) and minor adjustments were made. The program was then presented to the coordinators of all 12 Basic Health Unities affiliated with SSC/GHC to gauge their interest in and availability to take part in the program.
Characteristics of participating Basic Health Care Unities
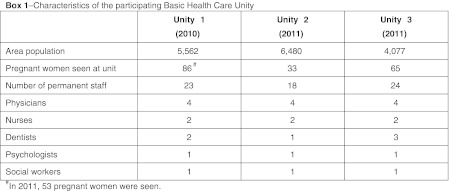
On the basis of availability and interest, three GHC-affiliated Basic Health Care Unities, all located on the Northern region of Porto Alegre, were selected for participation. The characteristics of these facilities are shown in Box 1. In addition to providers trained at a higher education level, PHC teams also comprise health care workers trained at a vocational and technical level, such as community health agents and nurse technicians; together, these primary care providers make up the standard staff of primary health care units. Although residents and interns are not accounted as regular staff, some of them chose to took part in the program.
Program implementation and evaluation
The program was initially carried out at one Basic Health Care Unity, Unity 1, for the pre-pilot stage of the study. During the first meeting, the program was presented, an initial questionnaire was administered and pretesting was performed (pre-1). The first five lectures, held 14 to 30 days apart, were followed by a second meeting for post-testing (post 1). This meeting was followed by the last three lectures of the program, again held 14 to 30 days apart. Furthermore, two separate meetings were held for presentation and discussion of cases selected by Unity 1 staff. Before and after the final lectures, a new round of pre- and post-testing was performed (pre-2 and post-2). During the last meeting, post-testing was followed by a final questionnaire for evaluation of the program. Finally, 6 months after the end of the program, a retention test was administered. Each pre- and post-test consisted of 15 multiple-choice questions, whereas the retention test was a simple compilation of these questions. Overall, 15 meetings were held at Unity 1.
The initial questionnaire was designed to outline a profile of unit staff and provide an instrument for self-assessment of genetics knowledge, genetics knowledge as applied to clinical practice, and confidence in providing genetics-related information to patients and their families. All self-assessment items were graded on a Likert-type scale. The final questionnaire consisted of three self-assessment items and questions on the impact of the program on clinical practice, on use of the information resources presented during the program, and on use of the educational materials provided. After some adjustments to the number of meetings and assessment methods, the program was expanded to Unity 2 and Unity 3. Initial and final meetings were held as in Unity 1, but only one pretest and one post-test were administered. The tests administered at Unity 2 and Unity 3 consisted of 20 questions each. Lectures were held 14 to 30 days apart as in Unity 1 and there were no case discussion meetings, for a total of ten meetings (lectures and sessions) at each Basic Health Care Unity.
All lectures were taught at the Basic Health Care Unity, by the same expert lecturers, except for the first lecture (a general overview of genetics), which was taught by two master’s candidates. Participants were given supporting material (booklets) related to each lecture. All meetings were monitored by the program coordinator. Classes were evaluated on a scale of zero to five in terms of clarity of explanations, mastery of the subject at hand, student interest, and relevance of the topic addressed. Classes were scheduled according to the availability of PHC teams, no less than 14 and no more than 30 days apart.
Development of educational material
After a discussion with SSC/GHC management and Unity 1 staff, two topics were selected for development of educational material geared to the community: teratogens in pregnancy (due to the reportedly high rate of alcohol and drug use in the community) and pre-conception counseling (due to the reportedly high rate of unplanned pregnancies in the community and to the implementation of a pre-conception counseling service in all primary health care units run by SSC/GHC during the study year).
Dissemination of this educational material to the community was planned at a meeting with community health agents. During this meeting, the importance of the selected topics was stressed and agents were asked to distribute the prepared material to the community. The material was also provided to program participants and made available at Basic Health Care Unity consulting rooms and waiting areas. The community health agent meetings were only held at Unity 1 and Unity 2, as Unity 3 had no community health agents on staff during the study period.
A “Handbook of Medical Genetics for Primary Care” was also developed and printed to serve as a user-friendly quick reference on the subjects addressed during the program.
Assessment of prevention measures adopted by GHC
A survey was conducted of all women treated at Unity 1 who had given birth in the year immediately preceding and the year immediately following the program. A questionnaire was used to measure adequacy to interventions already adopted by SSC/GHC for the prevention and control of genetic diseases and birth defects. In this instrument, women were asked about measures that should have been taken during their prenatal visits: inquiry and guidance on smoking, alcohol intake, and illicit drug or medication use; serological screening for rubella, with guidance and referral for immunization as necessary; prescription of folic acid during the optimal window for supplementation or at another point in time; and performance of prenatal ultrasound during the recommended period or at another point in time. Women were also asked about neonatal screening and hearing screening, and as to whether these interventions were performed during the optimal period for screening or at another time. The questionnaire administered to women who gave birth in the year after the program also included items on pre-conception counseling.
Ethical aspects
The project was approved by the Research Ethics Committees of Hospital de Clínicas de Porto Alegre and Grupo Hospitalar Conceição. All participants provided written informed consent at the beginning of the first study session. All tests and questionnaires (except those designed to outline a profile of participants) were anonymous.
Data analysis
Data were entered into a Microsoft Excel spreadsheet and analyzed in the SPSS 18 (Statistical Program for Social Science). Categorical variables were expressed as absolute and relative frequencies. The Shapiro–Wilk test was used to test for normality of distribution in continuous variables. Normally distributed continuous variables were expressed as means and standard deviations, and the Student t test was used for comparison of means. Asymmetrically distributed variables were expressed as medians and interquartile ranges, with the Mann–Whitney U used for comparisons.
Results
Forty-three professionals across the three selected Basic Health Care Unities took part in the program, and 31 (72.1 %) completed it (defined as attendance of >75 % of lectures and completion of the post-test and final assessment questionnaires). Eight of the providers who did not complete the program were residents or interns, not regular PHC team. A profile of the participants from each Basic Health Care Unity is shown in Table 1. All PHC team trained at a higher education level took part in the program (except for one nurse at Unity 3), as well as residents and interns from a variety of specialties (including two Pharmacology residents at Unity 2). The staff of Unity 1 had been in practice the longest, and this unit also had the highest percentage of professionals who did not take Medical Genetics during their undergraduate studies. The percentage of professionals with a postgraduate qualification (most were board-certified in family health) was similar across all three units.
Table 1.
Sample profile
| Unity 1 | Unity 2 | Unity 3 | ||
|---|---|---|---|---|
| (n = 14) | (n = 15) | (n = 14) | ||
| Degree | Medicine | 4 | 6 | 5 |
| (28.6 %) | (40.0 %) | (35.7 %) | ||
| Nursing | 4 | 3 | 1 | |
| (28.6 %) | (20.0 %) | (7.1 %) | ||
| Psychology | 1 | 2 | 3 | |
| (7.1 %) | (13.3 %) | (21.4 %) | ||
| Dentistry | 4 | 1 | 4 | |
| (28.6 %) | (6.7 %) | (28.6 %) | ||
| Social Services | 1 | 1 | 1 | |
| (7.1 %) | (6.7 %) | (7.1 %) | ||
| Pharmacology | - | 2 | - | |
| (13.3 %) | ||||
| Time since graduation (months)a | 252.0 | 132.0 | 84.0 | |
| (33.0–339.0) | (12.0–300.0) | (21.0–207.0) | ||
| Duration of practice in primary care (months)a | 144.0 | 120.0 | 60.0 | |
| (29.2–231.0) | (7.0–216.0) | (7.5–114.0) | ||
| Took Genetics during undergraduate studies? | Yes 7 | Yes 12 | Yes 10 | |
| (50.0 %) | (80.0 %) | (71.4 %) | ||
| Pursued a postgraduate degree? | Yes 12 | Yes 11 | Yes 11 | |
| (85.7 %) | (73.3 %) | (78.6 %) | ||
aVariables expressed as median (interquartile range)
The median number of correct responses in each test administered at Unity 1 is shown in Table 2. Despite a statistically significant pre-/post-test difference, no significant difference was found in the retention test administered 6 months after the end of the program. The mean number of correct responses in each test administered at Unity 2 and Unity 3 is shown in Table 3.
Table 2.
Results of pretest, post-test, and retention test (Unity 1)
| Unity 1 | |||||||
|---|---|---|---|---|---|---|---|
| Test | Pre 1 | Post 1 | Pre 2 | Post 2 | Retention | ||
| (n = 14) | (n = 11) | (n = 11) | (n = 8) | (n = 8) | |||
| 8.0 | 10.0 | p = 0.017 | 7.0 | 9.0 | p = 0.024 | 8.50a | |
| (6.7–8.2) | (7.0–11.0) | (7.0–8.0) | (6.7–9.7) | (8.1–9.2) | |||
Number of items in each test, 15. Variables expressed as median (interquartile range)
aNo statistically significant difference as compared to Post 1 or Post 2 (p = 0.170 and p = 0.132, respectively)
Table 3.
Results of pretest, post-test, and retention test (Unity 2 and Unity 3)
| Unity 2 | Unity 3 | |||||
|---|---|---|---|---|---|---|
| Test | Pre | Post | Pre | Post | ||
| (n = 15) | (n = 12) | (n = 14) | (n = 11) | |||
| 13.8 | 14.2 | p = 0.578 | 12.4 | 13.0 | p = 0.026 | |
| (12.1–15.5) | (12.4–16.0) | (10.8–13.9) | (11.1–14.9) | |||
Number of items in each test, 20. Variables expressed as mean (±SD)
Responses for the self-assessment questionnaire are shown in Table 4. Regarding the influence of the program on primary care practices, 85.7 % of professionals at all participating Basic Health Care Unities (24 out of 28) reported changes after the program, particularly in relation to their awareness of potentially genetic causes of diseases, a better approach to obtaining and using the family history, and the prevention of birth defects through care of pregnant patients and pre-conception counseling. Furthermore, 64.3 % of providers (18 out of 28) claimed they had used the information resources presented during the program, and 57.1 % (16 out of 28) reported use of the educational material provided during the program in their daily clinical practice.
Table 4.
Results of questionnaire for self-assessment of genetics knowledge
| Topic | Self-assessment | Unity 1 | Unity 2 | Unity 3 | |||
|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | Pre | Post | ||
| (n = 14) | (n = 8) | (n = 15) | (n = 9a) | (n = 14) | (n = 11) | ||
| Knowledge of medical genetics | Very good | – | – | 1 | – | – | 1 |
| (6.7 %) | (9.1 %) | ||||||
| Good | 1 | 2 | 1 | 1 | – | 1 | |
| (7.1 %) | (25.0 %) | (6.7 %) | (11.1 %) | (9.1 %) | |||
| Fair | 7 | 4 | 9 | 7 | 7 | 7 | |
| (50.0 %) | (50.0 %) | (60.0 %) | (77.9 %) | (50.0 %) | (63.6 %) | ||
| Poor | 6 | 2 | 3 | 1 | 5 | 2 | |
| (42.9 %) | (50.0 %) | (20.0 %) | (11.1 %) | (35.7 %) | (18.2 %) | ||
| Very poor | – | – | 1 | – | 2 | – | |
| (6.7 %) | (14.3 %) | ||||||
| Sufficiency of knowledge of genetics for current practice | Sufficient | – | 1 | 3 | 3 | 2 | 2 |
| (12.5 %) | (20.0 %) | (33.3 %) | (14.3 %) | (18.2 %) | |||
| Intermediate | 7 | 4 | 6 | 5 | 6 | 7 | |
| (50.0 %) | (50.0 %) | (40.0 %) | (55.5 %) | (42.9 %) | (63.6 %) | ||
| Insufficient | 7 | 3 | 6 | 1 | 6 | 2 | |
| (50.0 %) | (37.5 %) | (40.0 %) | (11.1 %) | (42.9 %) | (18.2 %) | ||
| Confidence in ability to provide information on genetics to patients and their families | Completely confident | – | – | 1 | – | – | – |
| (6.7 %) | |||||||
| Very confident | – | 1 | – | – | – | – | |
| (12.5 %) | |||||||
| Confident | 4 | 3 | 5 | 4 | 2 | 7 | |
| (28.6 %) | (37.5 %) | (33.3 %) | (44.4 %) | (14.3 %) | (63.6 %) | ||
| Somewhat confident | 9 | 3 | 6 | 4 | 9 | 4 | |
| (64.3 %) | (37.5 %) | (40.0 %) | (44.4 %) | (64.3 %) | (36.4 %) | ||
| Not at all confident | 1 | 1 | 3 | 1 | 3 | – | |
| (7.1 %) | (12.5 %) | (20.0 %) | (11.1 %) | (21.4 %) | |||
aThree professionals did not complete the questionnaire
Considering all participating Unities, the lectures that had the best reviews in terms of clarity, interest, and mastery and relevance of the topic were the lectures on cancer genetics (lecture 6), teratogens (lecture 3), mental disability (lecture 5), and PND and pre-conception counseling (lecture 8), all of which had a score of >4.75 (corresponding to >95 % satisfaction). All other lectures were assigned a score of ≥4 (corresponding to ≥80 %).
Concerning assessment of the adequacy of program content by participants of the 22nd Brazilian Congress on Medical Genetics, 85 genetics experts with different backgrounds completed the questionnaire distributed during the Congress. The topics evaluated by over 90 % of participants as being very relevant or relevant were: basic concepts of medical genetics (lecture 1); teratogens (lecture 3); IEM and neonatal screening (lecture 5); and cancer genetics (lecture 8). All other topics were evaluated by 80 % to 90 % of participants as being very relevant or relevant. Some topics that were not included separately in the program were listed and evaluated by over 90 % of participants as being very relevant or relevant: use of information resources; ethical aspects of genetics; and assessment of neurological and psychomotor development. Use of information resources and ethical aspects of genetics were presented in lectures whenever applicable. The third topic was ultimately not included in the program, as the program was designed to be broader and more comprehensive in scope rather than limited to genetic diseases presenting in childhood.
Regarding our survey of pregnant women treated at the participating Basic Health Care Unities, 25 out of 86 (29.1 %) women seen in 2010 and 23 out of 53 (43.4 %) women seen in 2011 completed the questionnaire. The results of these surveys are presented in Table 5 and show few changes in practices already established as part of the prenatal care provided by SSC/GHC. Only one respondent in the 2011 survey claimed to have received pre-conception counseling.
Table 5.
Results of questionnaire on measures for prevention and control of congenital disorders and birth defects adopted at GHC-run primary health care units, as administered to pregnant women seen at the participating units
| Pre (n = 25) | Post (n = 23) | |
|---|---|---|
| Asked about smoking? | 23 Yes (92.0 %)/1NR | 23 Yes (100.0 %) |
| Given guidance on smoking? | 19 Yes (16.0 %) | 17 Yes (73.9 %) |
| Asked about alcohol intake? | 22 Yes (88.0 %) | 21 Yes (91.3 %) |
| Given guidance on alcohol intake? | 19 Yes (76.0 %) | 18 Yes (78.3 %) |
| Asked about drug use? | 20 Yes (80.0 %) | 19 Yes (82.6 %)/1 NR |
| Given guidance on drug use? | 19 Yes (76.0 %) | 16 Yes (69.6 %)/1 NR |
| Asked about medication use? | 19 Yes (76.0 %) | 18 Yes (78.3 %)/1 NR |
| Given guidance on medication use? | 18 Yes (72.0 %) | 19 Yes (82.6 %)/1 NR |
| Rubella serological testing performed? | 11 Yes (44.0 %)/5 NR | 4 Yes (17.4 %)/13 NR |
| If not immune: given guidance? | 8 Yes (72.7 %)/14 NA | 1 Yes (25.0 %)/2 NR/19 NA |
| If not immune: given vaccine? | 3 Yes (27.3 %)/14 NA | 2 Yes (50.0 %)/2 NR/19 NA |
| Took folic acid 90–30 days before conception? | 0 Yes (0.0 %) | 0 Yes (0.0 %)/1 NR |
| Took folic acid at another point in time? | 12 Yesa (48.0 %)/1 NR | 5 Yesb (21.7 %)/2 NR |
| Ultrasound performed on 3rd month of pregnancy? | 18 Yes (72.0 %) | 14 Yes (60.9 %) |
| Ultrasound performed at another point in time? | 4 Yesc (16.0 %) | 3 Yesd (13.0 %)/1NR |
| Neonatal hearing screening performed during 1st week of life? | 17 Yes (68.0 %) | 23 Yes (100.0 %) |
| Neonatal hearing screening performed at another point in time? | 8 Yese (32.0 %) | NA |
| Audiological screening performed during 1st month of life? | 21 Yes (84.0 %) | 19 Yes (82.6 %) |
| Audiological screening performed at another point in time? | 3 Yesf (12.0 %) | 1 Yesg (4.3 %) |
NR no recollection, NA not applicable
aFrom diagnosis of pregnancy through delivery
bFrom diagnosis of pregnancy through end of the first trimester
cBetween the fifth and sixth months of pregnancy
dOn the fifth month of pregnancy
eBetween the 10th and 15th day of life
fBetween the second and fifth month of life
gBetween the first and second month of life
Discussion
Although most health professionals have studied genetics during undergraduate courses, it is well known that the genetics content presented in the curriculum of undergraduate and professional degree programs is limited and not oriented to clinical practice (Greendale and Pyeritz 2001; Williams 2001; Suther and Goodson 2003). Penchaszadeh et al. (1999) maintain that the curricula of undergraduate health degree programs should be modernized and the practical aspects of medical genetics included. Furthermore, the authors note, “for those professionals already in practice, continuing education programs to familiarize them with the modern concepts of clinical genetics are essential.”
The correct answer rate during the pretest, which was <70 % at all three Basic Health Care Unities, shows that primary care providers have insufficient knowledge of genetics. Although Unity 1 and Unity 3 staff had a statistically significant difference in their pretest and post-test grades, this difference was minor in light of the percentage of correct answers, which did not reach 70 % in either unit. Staff at Unity 2 had a higher correct response rate during the pretest, which reflects higher baseline knowledge. Although this was the only unit whose staff had a >70 % correct answer rate during post-testing, there was no significant difference between pre-/post-test scores. It is well documented that most primary care providers have limited knowledge of genetics (Emery et al. 1999; Suther and Goodson 2003; Nippert et al. 2010). This limitation reflects both the rapid progress in genetics and the deficiency in genetics education during undergraduate study, as well as the deficient approach to teaching of medical genetics during residency or specialization programs and the lack of continuing medical education programs for primary care providers. Surveys of these professionals have also revealed deficient ability to obtain and assess a family history, limited self-confidence regarding their knowledge of genetics, wasted opportunities to diagnose genetic disorders, and few referrals to medical genetics services (Burke and Emery 2002; Suther and Goodson 2003).
Analysis of the response rate of the self-assessment questionnaire revealed that the program achieved its expected results, namely, to increase overall knowledge of medical genetics (particularly as applied to primary care) and increase provider confidence in giving genetic information to patients and their families. There were some contradictory findings among the staff of Unity 1 and Unity 2, suggesting that knowledge of genetics actually decreased after lectures and that some providers actually became less confident after the program. These findings may suggest that the program made providers realize that they need to learn more about medical genetics before they can incorporate its concepts into their practice of primary care. Indeed, this concern was reported by several participants.
A systematic review carried out by Suther and Goodson (2003) noted four main barriers to provision of genetics services by primary care physicians: inadequate knowledge of genetics, lack of detailed or updated family histories, lack of confidence, and lack of referral guidelines. Our results show that, after the program, primary care providers reported an improved knowledge of genetics (as confirmed by statistical testing at two Unities) and increased confidence to provide genetic information to patients and their families. A survey conducted in four European countries found that only 19.3 % of health care professionals feel very confident or confident with respect to their genetics-related knowledge, skills, and (Nippert et al. 2010). Carroll et al. (2009), in their study of an educational intervention (workshop), found that most participants reported increased confidence in addressing genetics-related issues after the intervention.
Kolb et al. (1999) believe that most of the underuse of genetics interventions in clinical practice by primary care providers is due to the lack of adequate information and knowledge on the subject. The authors found significant improvement in knowledge about genetic conditions and attitudes of primary care professionals toward provision of genetics services during prenatal and pediatric care after a basic, 8-h genetics education program, the content of which was more restricted than that presented in our intervention.
In the present study, the gap between classes was determined by the availability of professionals, as participation in the program was an activity that deviated from their routine. We believe the widely spaced schedule (which led to over 6 months of contact between teams and teachers) and the fact that all classes were taught in Basic Health Care Unities helped bring the genetics professionals closer to the reality of primary care. This is beneficial to both groups, as geneticists can benefit from a greater understanding of the perspective of primary care while primary care providers learn more about the contributions of genetics to disease states and about the many ways in which information on the genetic basis of diseases can benefit patients (Burke and Emery 2002).
Several methods are available that can facilitate the partnership between primary care and medical genetics. Joint educational initiatives are valid methods and can be implemented in a variety of configurations. These initiatives should present genetics as relevant to the practice of primary care, framing it within the context of highly prevalent health conditions (such as screening and prevention of common chronic diseases) and with the objective of developing competences for shared decision making, evidence-based practice, and risk and uncertainty management (Burke and Emery 2002).
In the present study, most professionals reported a change in attitude during daily clinical practice after the program. A similar finding was reported by Carroll et al. (2009), where participants reported improvement in their ability to obtain a family history and improvement in their knowledge of genetics aspects relevant to clinical practice. Primary care providers should view genetics as an integral part of their daily practice, not a field confined to the identification and management of complicated monogenic diseases. Furthermore, these professionals require systematic education to improve their knowledge, skills, and attitudes, which will help them, recognize the importance of early identification of potentially heterozygous individuals, assessment of reproductive risk, and interpretation of family histories (Qureshi et al. 2004; Nippert et al. 2010).
Although program content was selected by medical genetics experts, all classes were well-reviewed by participants and considered relevant to their primary care practice. Educational strategies geared to primary care providers tend to be more successful if they are based on a careful analysis of the aspects of genetics most relevant to their practice and of how genetics can be integrated into their existing competences and knowledge. Prior experiences with this type of educational strategy suggest that primary care providers and medical geneticists have much to learn from one another, and that programs such as this provide an opportunity to foster dialogue and encourage a greater appreciation of the distinct perspectives of these two fields (Burke and Emery 2002; Guttmacher et al. 2007). Burke et al. (2009) identified the following as key topics for a medical genetics in primary care curriculum: identifying patients with, or at risk of, a genetic condition; clinical management of genetic conditions; and communicating genetic information. We believe the content presented during our study intervention covered these themes.
The results of the retention test administered at Unity 1 6 months after the conclusion of the study intervention suggest that learning was not sustained over time. Thus, there is a need for continuing genetics education strategies for primary care providers. Continuing education should prepare these professionals to provide some basic genetics services independently, by improving their knowledge, skills, and attitudes (Nippert et al. 2010). One viable option for continuing education is access to free websites and hotlines that provide up-to-date information on genetics topics. Such websites can include a mix of basic educational material and clinical practice guidelines, including recommendations for referral to specialist medical genetics services when appropriate (Guttmacher et al. 2007; Carroll et al. 2009).
Our survey of pregnant women treated at the participating Basic Health Care Unity revealed little change in prenatal management. Notably, after the program, all newborns underwent neonatal screening during the optimal timeframe for this intervention. Penchaszadeh et al. (1999) note that education of the public about genetic disorders and birth defects should be attuned to the cultures, beliefs, and values of the population. These education efforts should be community-oriented and address important issues such as alcohol intake during pregnancy, immunizations, self-medication, and the importance of learning about one’s family history so as to enable adequate genetic counseling.
Limitations
The main limitations of this project are as follows: (1) the educational program was designed by genetics specialists, rather than based on unmet needs reported by primary care providers; (2) due to the anonymous nature of questionnaire responses, we were unable to conduct a paired comparison of pre- and post-test results; (3) expansion of the program in its current format to all Basic Health Care Unity in the municipality of Porto Alegre would not be feasible, particularly due to cost constraints and the limited availability of human resources; and, (4) as the program was tied to a research project, the duration of the intervention and outcome assessment periods was quite short, which precluded assessment of long-term attitude changes in PHC team and in the community as a whole.
Conclusion
In spite of its limitations, this program was the first fully developed, comprehensive attempt at integrating medical genetics into PHC in Brazil. The inclusion of genetics in primary care has been the object of international debate for years, and despite the publication of a nationwide Brazilian policy for comprehensive medical genetics care in January 2009, little has been done go far in practical terms to implement its proposals.
According to Penchaszadeh et al. (1999), there is a need to recognize the burden imposed by birth defects and genetic disorders. This, in turn, requires political will and commitment to the development of prevention and management programs for genetic disorders and the organization of genetics services in a manner that is integrated into the primary care framework. The addition of basic knowledge of genetics to the practice of primary care is absolutely essential to the success of these programs.
The intervention tested in this study managed to bring medical genetics closer to primary care, which proved beneficial to both sides. Primary care providers were given the opportunity to learn new concepts, bring their knowledge up to date, and consider genetics as a discipline applicable to their daily practice, thus enabling them to provide better care to patients and their families. Genetics professionals got to know the practice routine of community-oriented primary care, which may led them to rethink the applications of medical genetics, which should not be seen merely as a specialty whose scope is confined to tertiary care, but as a tool for the prevention of a variety of prevalent diseases and conditions that affect communities. However, continuing education strategies, such as online-based programs, appear to be a more appropriate option for inclusion of genetics into the daily practice of PHC than isolated training interventions.
The integration of these two specialties should be strengthened. This requires effort from geneticists and primary care providers, so that community genetics can be truly put into practice. However, concrete integration will only be possible once public policies are in place to ensure the viability of comprehensive genetics care.
Acknowledgments
We would like to thank the March of Dimes Foundation (Global Network for Mother and Infant Health-GNMIH), Instituto Genética para Todos, INAGEMP, and CAPES for their financial support.
The authors wish to express their sincere gratitude to Andressa Federhen, Antonette El Husny, Camila Bittar, Carolina Souza, Fernanda Vianna, Flávia Ferreira, Ida Schwartz, Louise Pinto, Maria Teresa Sanseverino, Tatiele Nalin, and all the others who contributed to this project.
Conflict of interest
The authors have no conflicts of interest to declare.
References
- Brasil. Ministério da Saúde (2009) Política nacional de atenção integral em genética clínica, Portaria nº 81/GM, de 20 de janeiro de 2009. Avaliable at http://dtr2001.saude.gov.br/sas/PORTARIAS/Port2009/GM/GM-81.htm. Accessed on 2nd April, 2010
- Burke W, Emery J. Genetics education for primary care providers. Nat Rev Genet. 2002;3(7):561–566. doi: 10.1038/nrg845. [DOI] [PubMed] [Google Scholar]
- Burke S, Martyn M, Stone A, Bennet C, Thomas H, Farndon P. Developing a curriculum statement based on clinical practice: genetics in primary care. Br J Gen Pract. 2009;59(559):99–103. doi: 10.3399/bjgp09X395094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll JC, Rideout AL, Wilson BJ, Allanson J, Blaine SM, Esplen MJ, Farrell SA, Grahan GE, ManKenzie J, Meschino W, Miller F, Prakash P, Shuman C, Summers A, Taylor S. Genetic education for primary care providers—improving attitudes, knowledge and confidence. Can Fam Physician. 2009;55:e92–e99. [PMC free article] [PubMed] [Google Scholar]
- Emery J, Watson E, Peter R, Andermann A. A systematic review of the literature exploring the role of primary care in genetic services. Fam Pract. 1999;16(4):426–445. doi: 10.1093/fampra/16.4.426. [DOI] [PubMed] [Google Scholar]
- Greendale K, Pyeritz RE. Empowering primary care health professionals in medical genetics: how soon? How fast? How far? Am J Med Genet. 2001;106:223–232. doi: 10.1002/ajmg.10010. [DOI] [PubMed] [Google Scholar]
- Guttmacher AE, Porteus ME, McInerney JD. Educating health-care professionals about genetics and genomics. Nat Rev Genet. 2007;8(2):151–157. doi: 10.1038/nrg2007. [DOI] [PubMed] [Google Scholar]
- IBGE. Instituto Brasileiro de Geografia e Estatística (2011) Sinopse do censo demográfico 2010. Avaliable at http://www.ibge.gov.br/home/estatistica/populacao/censo2010/sinopse.pdf. Accessed on 15th July, 2011
- Khoury MJ. Genetics and genomics in practice: the continuum from genetic disease to genetic information in health and disease. Genet Med. 2003;5(4):261–268. doi: 10.1097/01.GIM.0000076977.90682.A5. [DOI] [PubMed] [Google Scholar]
- Kolb SE, Aguilar MC, Dinenberg M, Kaye CI. Genetics education for primary care providers in community health settings. J Commun Health. 1999;24(1):45–59. doi: 10.1023/A:1018765215470. [DOI] [PubMed] [Google Scholar]
- Nippert I, Harris HJ, Julian-Reynier C, Kristoffersson U, ten Kate LP, Anionwu E, Benjamin C, Challen K, Schmidtke J, Nippert PR, Harris R (2010) Confidence of primary care physicians in their ability to carry out basic medical genetic tasks—a European survey in five countries—Part 1. J Commun Genet. doi:10.1007/s12687-010-0030-0 [DOI] [PMC free article] [PubMed]
- Penchaszadeh VB, Christianson AL, Giugliani R, Boulyjenovok V, Katz M. Services for the prevention and management of genetic disorders and birth defects in developing countries. Commun Genet. 1999;2:196–201. doi: 10.1159/000016212. [DOI] [PubMed] [Google Scholar]
- Qureshi N, Modell B, Modell M. Raising the profile of genetics in primary care. Nat Rev Genet. 2004;5(10):783–790. doi: 10.1038/nrg1453. [DOI] [PubMed] [Google Scholar]
- Starfield B. Primary care: concept, evaluation, and policy. New York: Oxford University Press; 1992. [Google Scholar]
- Suther S, Goodson P. Barriers to the provision of genetics services by primary care physicians: a systematic review of the literature. Genet Med. 2003;5:70–76. doi: 10.1097/01.GIM.0000055201.16487.61. [DOI] [PubMed] [Google Scholar]
- Ten Kate LP. Editorial. Commun Genet. 1998;1:1–2. doi: 10.1159/000016137. [DOI] [Google Scholar]
- Ten Kate LP, Al-Gazali L, Anand S, Bittles A, Cassiman JJ, Christianson A, Cornel MC, Hamamy H, Kääriäinen H, Kristoffersson U, Marais D, Penchaszadeh VB, Rahman P, Schmidtke J (2010) Community genetics. Its definition 2010. J Commun Genet. doi 10.1007/s12687-010-0007-z [DOI] [PMC free article] [PubMed]
- Primary health care approaches for prevention and control of congenital and genetic disorders. Geneva: Human Genetics Programme; 2000. [Google Scholar]
- Williams MS. Genetics and managed care: policy statement of American College of Medical Genetics. Genet Med. 2001;3:430–435. doi: 10.1097/00125817-200111000-00010. [DOI] [PubMed] [Google Scholar]