Abstract
Health needs assessment (HNA) is a commonly used process for those working in public health. The PHG Foundation has developed a Toolkit to provide users with a stepwise approach for undertaking a HNA on birth defects. We report the findings from using the Toolkit to examine needs in relation to policies and programs, services, and interventions for neural tube defects (NTDs) in Argentina. The trend over the last few decades is one of decline in infant mortality from nutritional and infectious causes, thus further increasing the relative importance of birth defects. The observed prevalence of NTDs is consistent with that reported internationally. Since 2002 folic acid fortification (FAF) has been mandatory by law, and different studies have shown at least a 50 % decrease in the birth prevalence of NTDs after FAF. In Argentina, there is inequity between the public and non-public health sectors. The birth prevalence of NTDs seems lower in the non-public sector, possibly as a result of better nutritional status of women, higher access to folic acid supplementation, and earlier prenatal diagnosis followed by termination of pregnancy (ToP) in non-public hospitals. Although illegal, ToP is believed to be widespread, with better access for people of higher socioeconomic status. Through the process of HNA, we identified several unmet needs regarding registration of cases, public and professional education, legislation, and organization of care pathways. In our experience, the Toolkit brought together people working on the same issue, and it engaged and motivated experts and stakeholders to work together to tackle the problem.
Keywords: Health needs assessment, Argentina, Neural tube defects, Health services, Interventions
Introduction
Birth defects are structural or functional abnormalities present at birth (WHO 1996), although most are detected later in life. The birth prevalence of birth defects is 2 to 3 %, and their relative importance, compared to other causes of morbidity and mortality, has been increasing in recent decades in low- and middle-income countries whilst in high- and high–middle-income countries, they are amongst the leading causes of infant mortality (Christianson et al. 2006; WHO 2010). Neural tube defects (NTDs) are birth defects involving the central nervous system caused by incomplete closure of the neural tube. They include spina bifida (ICD-10 Q05), encephalocoele (e-coele, ICD-10 Q01), and anencephaly (ICD-10 Q00). It has been estimated that approximately 230,000 (live birth prevalence of 1.70/1,000 births) babies with NTDs are born alive in the world every year with a further 75,000 stillborn (0.56/1,000 births) (PHG Foundation 2011). Surviving infants have a range of severities from none to severe cognitive and physical disability, depending on the severity of the initial defect and the impact of postnatal management. These infants also require follow-up and care throughout life to treat complications including infections and possible neurological lesion as well as any associated physical disability or intellectual impairment.
Periconceptional intake of folic acid through supplementation and food fortification can help to reduce the occurrence of NTDs. They are among the most cost-effective public health interventions available regarding birth defects (Yi et al. 2011). In the absence of other interventions, mandatory folic acid fortification (FAF) of foods could reduce the NTD birth prevalence to 0.5–0.9/1,000, with the remaining cases being “folate resistant” (Wyszynski 2006). Other interventions related to NTDs are prenatal screening by maternal serum alpha fetoprotein and prenatal diagnosis by fetal ultrasound scan, followed in the case of spina bifida or encephalocele by planning for the care of the child or by selective termination of pregnancy (ToP) for pregnancies diagnosed with anencephaly. Health care of people with NTDs requires a multidisciplinary approach involving both general and specialist surgeons, treatment of complications, rehabilitation, and social support.
In May 2010, the World Health Assembly passed a resolution that called on member states to “prevent birth defects wherever possible, to implement screening programs, and to provide ongoing support and care to children with birth defects and their families” (World Health Assembly 2010).
In Argentina, NTDs have been recognized as an important cause of both mortality and morbidity, and the birth prevalence can be reduced through effective interventions (López-Camelo et al. 2010). Since 2002, FAF has been mandatory by law. There have also been recent efforts to improve the organization of care pathways, which are generally patchy and concentrated in big centers such as Buenos Aires.
Here, we report the findings from examining needs, services, and interventions in relation to NTDs from our pilot of the PHG Foundation Health Needs Assessment (HNA) Toolkit, an open-access web-based resource that can be downloaded without cost and covers the major categories of birth defects—including NTDs—and the services involved in the treatment, care, and prevention of birth defects (Toolkit website: http://toolkit.bornhealthy.org; Nacul et al. (2012) Submitted to PloS Medicine).
HNA is a commonly used process for those working in public health (Wright et al. 1998; Williams and Wright 1998) and involves epidemiological, qualitative, and comparative methods to describe the health problems of a population, identify inequalities in health and access to services, and determine priorities for the most effective use of resources (Wright et al. 1998). The PHG Foundation has developed this Toolkit to provide users with a stepwise approach for undertaking a HNA on birth defects, which is useful in countries with little experience in this way of analyzing needs and prioritizing service development and interventions. In light of the WHA resolution, we decided to use the Toolkit, because although we already had local information about NTDs, we did not have any way to systematize those data nor other relevant information for the planning of interventions to reduce their burden. The use of the Toolkit also served as a guide for finding local data on NTDs and as a context for contacting local stakeholders. It was also an opportunity to work in parallel with other countries in the region on similar goals and have the support of public health professionals from the PHG Foundation in the use of HNA and their Toolkit.
Methods
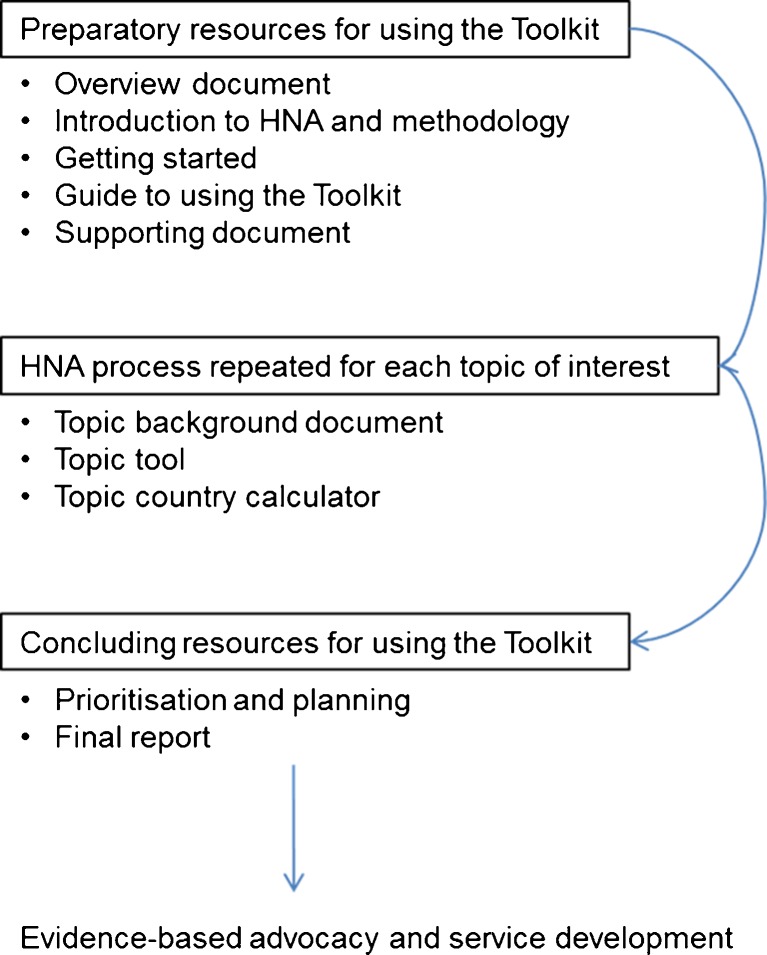
The Toolkit is a step-by-step interactive guide that supports users undertaking HNA in relation to congenital disorders. Additional details on the Toolkit methodology can be found both at the homepage (http://toolkit.bornhealthy.org) and within the guide (http://toolkit.bornhealthy.org/guide.pdf). The process is briefly outlined in Fig. 1. The HNA process starts with a series of documents that introduce the key concepts involved in the HNA before moving to a more structured approach for specific clinical (e.g., NTDs) or service (e.g., preconception care) topics. The NTD package within the Toolkit has a background document developed to enable users with different levels of knowledge to start the process from the same minimum point. This background document contains information and data on the epidemiology of NTDs (including risk factors and the estimated global burden of morbidity and mortality) with an emphasis on public health approaches to control the burden of NTDs at the population level. Some limited information is also provided on the effectiveness and cost-effectiveness of some example interventions, but the list is not intended to be exhaustive, and both the costs and impacts of the intervention vary depending on local circumstances. The NTD HNA tool and calculator is intended to lead users through the process of evaluating existing services and interventions and also allows recording of both qualitative and quantitative epidemiological data specific to NTDs, with the calculator containing prepopulated modeled data specifically for Argentina if local data are unavailable.
Fig. 1.
Brief overview of the Toolkit HNA process
The tool guides users through the collation of the following:
Demographic data on the country or region
Key epidemiological indicators for the burden of disease for a chosen condition or conditions, including comparative data and the potential effects of specific interventions
A structured assessment of existing policies, programs, services, and interventions in terms of their availability, quality, coverage, and effectiveness
A comparison of the current situation (“where are we now?”) with the desired situation (“where do we want to be?”)
Identification of gaps and unmet needs
Qualitative and quantitative assessments of the effectiveness of interventions
Prioritization of action areas and interventions that are relevant and appropriate to the level of socioeconomic development of the country and are sensitive to societal values, culture, and legislation
The HNA process also stresses the importance of involving all major stakeholder groups including, for example, policy makers, government/ministry representatives, public health and clinical professionals from a range of health services, laboratory scientists, representatives from patient support groups and charities, health economists, researchers, and the private health sector (Nacul et al. (2012) Submitted to PloS Medicine).
The information was collated using the tool, which guides the user through different types of questions: open questions, quantitative questions with tables for epidemiology, and qualifying questions. The information collation work was undertaken by the authors, members of the coordination of the National Registry of Congenital Anomalies (RENAC) based at the National Center of Medical Genetics (BG, RL, PB), linked to the National Health Ministry of Argentina, with supervision and help of the authors based at the PHG Foundation (CA, SM, LN, GSS). The HNA on NTDs started by reviewing the published literature for NTDs in Argentina archived within MEDLINE (via PubMed) on June 20, 2012, for articles using the search terms as described in “Appendix 1.” We also manually checked the references of included papers and searched Google (www.google.com) for additional Spanish language sources of information not indexed in MEDLINE. Once the literature was reviewed, we contacted experts and stakeholders involved in the topic in the National Ministry of Health (the Maternal and Child National Department, Statistics and Health Information Department, National Genetics Network Program), birth defects registries (Latin-American Collaborative Study of Congenital Malformations—ECLAMC), public hospitals (spina bifida committees formed by health professionals), and nongovernmental organizations (Spina Bifida and Hydrocephalus Parents Association—APEBI). We (BG, RL, PB) met in person with some of the experts and stakeholders and introduced them to the Toolkit. They described, based on their experience, the main problems related to NTDs and what actions they thought should be priorities. After these initial contacts, we continued to keep in touch with stakeholders and experts, and in some cases, we served as a link between them. The information obtained from stakeholders and experts were then combined with the identified literature, and we evaluated the priorities for NTDs in Argentina.
Results
Here, we present the results of the evaluation following the structure of the Toolkit: country profile, epidemiology, interventions, and needs assessment.
Country profile
Argentina has a population of 40,117,096 people in an area of 2,780,400 km2 (INDEC 2010). In 2010, there were 756,176 live births (National Ministry of Health 2011). The government is a federal presidential republic comprising of 24 provinces. Around 65 % of the population is concentrated in the central region provinces, particularly in the province of Buenos Aires and the Autonomous City of Buenos Aires. In Argentina, 90 % of the population live in urban areas. Health care is provided by both a public sector, where 57 % of births occur, and a non-public sector, with 43 % of births. The non-public sector is funded by social insurance (employer and labor union-sponsored plans) and private insurance plans. The public system, which consists of public hospitals and primary health care centers, and works under the coordination of ministries and departments of health of different jurisdictions (national, provincial, or municipal), provides free services at the point of need. Health care is free in the public sector, and the Plan Nacer, under the National Ministry of Health, has improved the quality and quantity of health care in this sector in the last years. This has been achieved through direct payments to health service providers according to medical practices, such as, for example, surgical procedures for congenital heart disease. As Argentina has a federal health care system in which the budget for health service providers comes from the provinces, the Plan Nacer directly funds local health service providers according to activities and results (Plan Nacer 2012).
Epidemiology of birth defects in Argentina
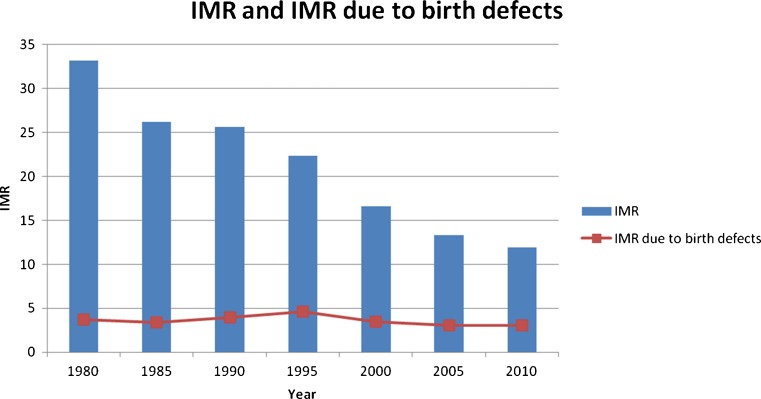
In 2010, the infant mortality rate (IMR) was 11.9/1,000 live births (LB). This decreased from 33.2/1,000 LB in 1980 to 25.6/1,000 in 1990 and further still to 16.6/1,000 LB in 2000. Figure 2 shows there has been an important decrease in IMR, but IMR due to birth defects appears to have remained constant over this same time period. In 2010, birth defects as a whole accounted for 25 % of infant mortality and was the second leading cause of infant mortality after perinatal causes (Fig. 3).
Fig. 2.
Infant mortality rate in the last decades in Argentina. Annual reports of the Department of Health Statistics and Research, Vital Statistics National Ministry of Health, 1981, 1986, 1991, 1996, 2001, 2006 and 2011
Fig. 3.
Causes of infant mortality in Argentina. Annual report of the Department of Health Statistics and Research, Vital Statistics National Ministry of Health, 2011
Epidemiology of NTDs in Argentina
Among birth defects, NTDs are the fourth most prevalent after congenital heart disease, Down's syndrome, and orofacial clefts (National Registry of Congenital Anomalies (RENAC), 2012, Annual report on birth defects prevalence, unpublished). The estimated prevalence by the PHG database of NTDs worldwide was reported in the “Introduction.” According to the RENAC, the live birth prevalence of NTDs in Argentina is 1.27/1,000 births (95 % CI 1.08 to 1.47), the prevalence of spina bifida is 0.63/1,000 births (95 % CI 0.45 to 0.81), anencephaly 0.36/1,000 births (95 % CI 0.22 to 0.49), and encephalocele 0.28/1,000 births (95 % CI 0.16 to 0.40). This is similar to the prevalence of neural tube defects reported by ECLAMC (Castilla 2004, López-Camelo et al. 2010). Among birth defects, anencephaly is the second highest cause of newborn mortality (which does not include fetal deaths) after heart disease (Bronberg et al. 2009).
There are national variations in the birth prevalence of NTDs, the rates being higher in public hospitals compared to non-public hospitals. Also, hospitals in the central region provinces have a higher frequency of spina bifida (Campaña et al. 2010a).
According to the Burden of Disease Study (Borruel et al. 2010), congenital anomalies in Argentina in 2005 were the cause of 86,400 life years lost from premature death and 104,919 DALYs.
According to the First National Survey of People with Disabilities (INDEC 2003), a total of 2,176,123 persons live with disabilities in Argentina, with 12.8 % (278,482) having the disability from birth. Also, 38.4 % of disabled patients did not have social or private insurance plans, further increasing the burden of their condition.
Interventions
Folic acid fortification
Fortification of wheat flour and its derivatives is mandatory (National law number 25630, http://www.infojus.gov.ar/index.php?kk_seccion=documento®istro=LEYNAC&docid=LEY%2520C%2520025630%25202002%252007%252031). The fortification includes folic acid, iron, thiamine, riboflavin, and niacin. The amount of folic acid added to flour is 2.2 mg/kg. This addition was based on an estimated consumption of 160 g of bread per day, yielding a mean intake of 0.35 mg of folic acid per day.
The law on fortification was enacted in 2002, and the population began to be exposed to fortified food at the end of 2003. By the last quarter of 2004, the first children prenatally exposed to fortification were born, and by 2005, it is believed that most infants would have been exposed prenatally to FAF. So far, the observed effect of the FAF is a decrease in the birth prevalence of NTDs with prevalence rate ratios of 0.41 for anencephaly, 0.41 for spina bifida, and 0.17 for encephalocele (López-Camelo et al. 2010). Another study showed a decrease in mortality rate by 56 % for anencephaly and 67 % for spina bifida when comparing the period 2000–2003 to 2005–2006. A decrease in hospital records for discharges was also observed. These were 53.8 % for anencephaly, 33.4 % for encephalocele, and 45.4 % for spina bifida when comparing the year 2000 with the year 2005 (Calvo and Biglieri 2008).
Bread samples obtained at random in the Cuyo region showed levels of folic acid consistent with fortification, although in 27 %, these were slightly below values established in the regulations. However, the average folic acid intake in the women studied in that region reached the recommendation, with 77.8 % of folic acid coming from derivatives of wheat flour (Zabala et al. 2008).
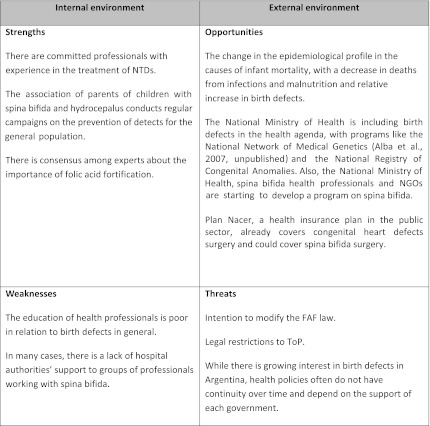
Whilst undertaking the strengths, weaknesses, opportunities, and threats (SWOT) analysis as part of the HNA, we observed some threats to folic acid fortification: lack of public information on FAF and NTDs. There has been a proposal to modify law 25630 approved by one chamber of the congress in 2008. This proposal is that fortification should only be applied to wheat flour and bread and not for wheat flour packaged derivatives such as fresh pasta and cookies. This proposal was defended by the manufacturers of the products, due to alleged effects of iron fortification on organoleptic properties, i.e., change in color or flavor, which might make them less attractive to consumers (Silverino Bavio 2009). Because of the pressure applied from stakeholders like the Argentinian Pediatric Association (SAP 2008), so far, this amendment to the law has not been made.
Folic acid supplementation
A survey performed in two regions of Argentina showed that around 25 % of pregnant women use periconceptional folic acid supplements during pregnancy. Pregnant women with higher levels of education and receiving care in a non-public hospital are more likely to use folic acid supplements (Zabala et al. 2008). An explanation for the relatively low usage of supplements is that in Argentina, at least 50 % of pregnancies are unplanned (Gadow et al. 1998), and there are gaps in knowledge of both the general population and health professionals on the prevention of NTDs (Barbero et al. 2003a).
Prenatal care
The gestational age at detection of a malformation occurs on average 3 weeks earlier in the non-public sector and the first prenatal visit and first prenatal scan, 4 and 5 weeks earlier, respectively in the non-public sector. Also the numbers of prenatal visits and prenatal scans are higher in this sector (Campaña et al. 2010a, b).
Acceptance of a routine scan is high in both the public and non-public sectors (SIP 2006). A study including 13 hospitals from Argentina (public and non-public) from the ECLAMC network showed that the detection rate of spina bifida and anencephaly by prenatal ultrasound is high (93.9 % for spina bifida and 87.5 % for anencephaly) (Campaña et al. 2010a, b). The detailed fetal anomaly scan and invasive prenatal diagnosis are performed by genetic services. Access is higher in the non-public sector and in the central region provinces (Liascovich et al. 2006). However, there was no quality assurance for any genetic services that we could identify. Alpha fetoprotein blood testing to screen for NTDs is not routinely performed but is available in the non-public sector and can be found in a few hospitals in the public sector too.
Termination of pregnancy
According to the Argentinian criminal code, ToP was illegal except for in two situations:
If the pregnancy is a threat to the woman's health or life
When the pregnancy is the consequence of a rape of a woman with mental retardation
In 2012, the Supreme Court of Argentina extended the exception in 2 to pregnancies as the consequence of rape, regardless of the mental status of the woman. The Supreme Court stated that there is no need for the doctors to take the case to courts to get permission to perform the ToP. It is only necessary for the affidavit of the woman to state that she was raped (Centro de Informacion Judicial 2012).
In the city of Buenos Aires, it is legal to induce labor after 24 weeks of gestational age in case of anencephaly and other lethal conditions (Law Number 1044 of the Autonomous City of Buenos Aires, Legislatura de la Ciudad Autónoma de Buenos Aires 2003).
Since termination of pregnancy is illegal in Argentina, there are no official records about it. However, the estimated number of terminations of pregnancy in Argentina based on hospital discharges was in the range of 485,974 to 522,216 in the year 2000 (CENEP 2007), which represents around 41 % of pregnancies. If prenatal diagnosis by ultrasound were widespread, by using the detection rates by ultrasound for anencephaly and spina bifida as described in the “Prenatal care” section and proportion of ToP for NTDs of 41 %, we could achieve a 38 % decrease in the prevalence of spina bifida and a 36 % decrease for anencephaly.
According to a survey, for women of low socioeconomic status, 10 % of abortions are provided by physicians and 30 % by people who are not physicians, and 60 % are self-induced. In the middle and upper socioeconomic classes, 60 % of abortions are provided by physicians, 10 % by non-medical people, and 30 % are self-induced (Mario and Pantelides 2009). Misoprostol, a teratogenic agent, is the most frequently used drug in self-induced abortions. Unsafe abortion is the leading cause of maternal mortality in Argentina (Barbero et al. 2011).
The effect of differential access to ToP in the public and non-public sector has been illustrated by Barbero et al. (2003a, b), showing a relative risk estimation of 7.10 (95 % CI 3.03 to 16.63) for anencephaly in public hospitals compared to non-public ones. For spina bifida, the relative risk was 5.75 (95 % CI 3.27 to 10.11) when comparing data from 4 years of live births (totaling 60,116 births) (Table 1).
Table 1.
Rates of anencephaly and spina bifida in a public and a non-public hospital in Argentina
| Number of anencephaly (/1,000) | Number of spina bifida (/1,000) | Total live births | |
|---|---|---|---|
| Public hospital | 45 (1.45) | 85 (2.74) | 31,071 |
| Non-public hospital | 6 (0.2) | 14 (0.48) | 29,045 |
Postnatal care
Ninety-nine percent of births in Argentina occur in hospitals and are attended by physicians or midwives (National Ministry of Health 2011). Newborn physical examination is regularly performed for NTDs and other external birth defects.
Acute care of spina bifida involves the work of pediatricians, neurosurgeons, and their team and is usually optimal. Long-term care of patients with spina bifida is performed by health professionals who work in hospitals, but without an organized national or regional system for the treatment and care of those with NTDs. These groups have a variable composition and can include surgeons, urologists, neurosurgeons, neurologists, orthopedic surgeons, pediatricians, ophthalmologists, physiotherapists, psychologists, and social workers. Chronic care is deficient due to the lack of specialists in nephrology and urology and the lack of hospital authorities' support.
There is a national law for disabled persons, which states that the disabled must have free access to treatment, rehabilitation, and social and economic support, as well as free access to public transportation and exemptions from paying taxes (National law no. 22.431/81 (1981)). Recently, spina bifida health professionals and nongovernmental organizations, under the name of the Myelomeningocele Argentina Group, with support of the National Ministry of Health, began the development of a national program to coordinate the care of affected children. Since the initial contact with this group, author BG was invited to join the group meetings and serve as consultant on epidemiology issues related to spina bifida.
The strengths, weaknesses, opportunities, and threats identified from the work with stakeholders are summarized in Table 2.
Table 2.
SWOT analysis for the work of the stakeholders
Identified needs
Through the process of HNA, we identified several unmet needs on the topic:
Increase of coverage of the National Registry of Congenital Anomalies to obtain more accurate data on NTD birth prevalence
Improvement of professional education through courses and publications
Support to and raising the profile of the ongoing integration of hospital committees on spina bifida across the country by the Myelomeningocele Argentina Group
Inclusion of free NTD surgery as part of the Plan Nacer, a health insurance plan in the public sector
Implementation of universal and free prenatal screening of alpha fetoprotein levels
ToP decriminalization in cases of major birth defects, such as NTDs
Public education: creation of information sheets for parents of children with birth defects and awareness raising on the importance of folic acid for NTD prevention
Actions (already) taken
We listed the priorities indicated from discussions with different stakeholders and the evaluation of the feasibility and sustainability of each action proposed to address priority areas and minimize gaps. After performing the prioritization process, we started developing information sheets for parents of children with NTDs and actions to increase the coverage of the National Registry for Congenital Anomalies, and started working with the Myelomeningocele Argentina Group.
Appraisal of the use of the Toolkit in Argentina
Regarding the online accessibility to the Toolkit, the website is user friendly, and the Toolkit files are easy to download. Given the high availability and reliability of the Internet in Argentina, we concluded that in our country and in others with a similar access to reliable internet connections, online access would not be a limitation for people interested in using the Toolkit.
As for language, the Toolkit is currently only available in English. The authors based in Argentina, who do not have English as a mother tongue, could easily understand the language used in the Toolkit. However, this may be a limitation for people who are not used to reading English.
With regard to the stakeholders, the Toolkit served as a context for contacting them. They showed interest in the Toolkit, and it was well received. This was due mainly to the fact that the stakeholders, health professionals, and nongovernmental organizations were already motivated to work on the problem. Therefore, we consider it a key to success that people who coordinate the HNA are in the position to contact stakeholders and work with them.
In our experience, health situation analysis in many cases remains limited to the collection of data and is not primarily action oriented. One of the key aspects of HNA is that from the beginning, it stimulates people conducting the HNA to work together with relevant stakeholders, and this was a key strength of using the PHG HNA Toolkit. Through this joint effort with the stakeholders, the authors were able to push forward the HNA. Also, work with stakeholders has not ended with the end of the HNA, but continues today, as in the case of collaboration with the Myelomeningocele Argentina Group.
There are some sections of the Toolkit that require more quantitative information, such as the Country profile and Epidemiology section. When we started the HNA, we encountered difficulties in completing some of these sections. For example, with our data sources, it was impossible to estimate the prevalence and mortality by age group beyond birth and the number of cases by level of disability or to perform a cost-effectiveness analysis of the interventions. However, through several conversations with the authors based at the PHG Foundation and pilots from other countries performing the HNA, we realized that the lack of data does not limit the progress of the HNA and subsequent actions.
Although HNA is a common practice for those working in the field of public health in many countries, in Argentina, it is not commonly used. The main utility of using the Toolkit was that it provided those unfamiliar with the HNA process a means of systematically collecting the various data and information required to conduct a HNA. However, the HNA process can also be undertaken without the use of the Toolkit.
We also found the Toolkit to be very flexible and able to adapt to the situation of our country, since it takes into account the existing differences in regions within the country and between the public and non-public health sectors. When working with the Toolkit calculator, we used our own local data, but for those countries that do not have good-quality sources available locally, it would be a good option to start by using the prepopulated data already entered in the calculator.
Parallel work in Uruguay and Brazil with the HNA Toolkit on the same topic allowed the formation of a regional community of interest working on the problem with similar goals. This allowed comparison of interventions in different countries (for example, about the various policies of folic acid fortification and legal status of the termination of pregnancy in each country).
Regarding the time required to perform the HNA pilot on NTDs, it took 4 months of part-time work of authors BG, RL, and PB with support from the PHG Foundation staff. The amount of hours dedicated per day for the HNA was variable, and we estimate that it took 3 months of one person's full-time equivalent work. This workload was added to their routine work. We think that the time required is highly variable as it depends on the contacts with stakeholders of the people performing the HNA and their skills in managing epidemiological information.
Discussion
Birth defects are a relevant public health problem in Argentina. The trend over the last few decades is one of decline in infant mortality from nutritional and infectious causes, thus further increasing the relative importance of birth defects (following the so-called epidemiological transition). The prevalence of NTDs observed in Argentina is consistent with that reported internationally. The impact is high for the health system, which faces long-term treatment costs for surviving patients.
There are some effective interventions already being performed like mandatory FAF; however, other interventions are less developed, i.e., there is a lack of organized pathways for the care of those affected. Given the high number of unplanned pregnancies, FAF is the best way to ensure adequate folic acid intake because it is an intervention that favors equity, since wheat flour and its derivatives are widely consumed in Argentina among different social sectors, unlike folic acid supplements which have greater uptake in women with higher educational levels and socioeconomic status. FAF has been shown to be effective in the reduction of the birth prevalence of NTDs in Argentina.
In Argentina, there is inequity between the public and non-public health sectors. The birth prevalence of NTDs seems lower in the non-public sector, possibly as a result of higher access to better nutrition, folic acid supplementation, and earlier prenatal diagnosis followed by ToP in non-public hospitals (Barbero et al. 2003a, b).
Although illegal, studies suggest that termination of pregnancy is widespread, with better access for people of higher socioeconomic status. Universal access to prenatal diagnosis and decriminalization of ToP could be additional safe and effective measures to reduce the prevalence of NTDs and inequities in the burden caused by these conditions. Inequity is also observed when comparing different regions of the country. Prenatal and postnatal care for NTDs is more widespread in the central region provinces. Also, hospitals in this region report a higher frequency of spina bifida, probably because cases detected prenatally are referred there for care (Campaña et al. 2010a, b).
Conclusions
The HNA Toolkit is a systematic approach to assessing needs and then prioritizing actions to tackle the problems associated with birth defects. In our experience, it brought together people working on the same issue, and it engaged and motivated experts and stakeholders in working to tackle the problem. Also, it allowed collaborative work to be undertaken with people located in Brazil and Uruguay simultaneously on similar goals, providing users of the Toolkit with the unique opportunity to also learn from each other. One of the key aspects of the HNA Toolkit is that it is not a data-collecting exercise. It is oriented to getting benefits from interventions.
With regard to its limitations, the Toolkit is currently available in English only. The HNA is a time-consuming task, and it is preferable that it is performed by someone already working on the problem. The costs of performing the HNA are the costs of the human resources involved. Therefore, these costs could come from ministries of health and other potential funders through grants and scholarships. In addition, the HNA should involve stakeholders working in the field of public health and birth defects. Conversely, by bringing stakeholders together, the workload can be shared, and action can result from stakeholders working to shared agendas that are agreed through a rational and transparent process rather than individuals working in isolation.
Acknowledgments
The authors would like to thank the participants of the stakeholder meeting: Fernanda de Castro and Liliana Campmani, Garrahan Hospital, Myelomeningocele Argentina Group.
Appendix 1
We searched for articles written in English and Spanish using the following terms:
(“Neural tube defects” or “NTDs” or “spina bifida” or “encephalocele” or “anencephaly” or “myelomeningocele”) and (“Argentina” or “Latin America” or “South America”)
(“Defectos del tubo neural” or “DTNs” or “espina bífida” or “encefalocele” or “anencefalia” or “mielomeningocele”) and (“Argentina” or “América Latina” or “Sudamérica”)
References
- Barbero P, Liascovich R, Rozental S, Botto R, Gramajo S, Haefliger C. Conocimientos de tocoginecólogos y pediatras acerca de la etiología y los factores de riesgo de los defectos congénitos (Gynecologists and pediatricians knowledge about the etiology and risk factors of birth defects) Arch argent pediatr. 2003a;101(3):184–192. [Google Scholar]
- Barbero P, Liascovich R, Rittler M, Colantonio G, Alazraqui M, Pedraza A, Prudent L, Fuksman R. (2003b) Frecuencias de anencefalia y espina bifida en dos maternidades con poblaciones de diferente nivel socioeconómico (Frequency of anencephaly and spina bifida in two maternity hospitals with populations of different socioeconomic level). Dissertation, 32nd Genetics Argentinian Congress, Córdoba.
- Barbero P, Liascovich R, Valdez R, Moresco A. Efecto teratogénico del misoprostol: un estudio prospectivo en Argentina (Misoprostol teratogenicity: a prospective study in Argentina) Arch Argent Pediatr. 2011;109(3):226–231. doi: 10.1590/S0325-00752011000300007. [DOI] [PubMed] [Google Scholar]
- Borruel M, Mas P, Borruel G (2010) Estudio de Carga de enfermedad (Burden of diseases study). National Ministry of Health Website www.msal.gov.ar/fesp/descargas_home/Estudio_de_carga_FESP_Imprenta.pdf. Accessed 20 June 2012
- Bronberg R, Alfaro E, Chaves E, Dipierri J. Mortalidad infantil por malformaciones congénitas en Argentina: análisis del quinquenio 2002–2006 (Analysis of infant mortality from congenital malformations in Argentina during the 2002–2006 period) Arch Argent Pediatr. 2009;107(3):203–211. doi: 10.1590/S0325-00752009000300007. [DOI] [PubMed] [Google Scholar]
- Calvo E, Biglieri A. Impacto de la fortificación con ácido fólico sobre el estado nutricional en mujeres y la prevalencia de defectos del tubo neural (Impact of folic acid fortification on women's nutritional status and on the prevalence of neural tube defects) Arch argent pediatr. 2008;106(6):492–498. doi: 10.1590/S0325-00752008000600004. [DOI] [PubMed] [Google Scholar]
- Campaña H, Pawluk MS, López Camelo JS. Grupo de Estudio del ECLAMC, Prevalencia al nacimiento de 27 anomalías congénitas seleccionadas, en 7 regiones geográficas de la Argentina (Births prevalence of 27 selected congenital anomalies in 7 geographic regions of Argentina) Arch Argent Pediatr. 2010;108(5):409–417. doi: 10.1590/S0325-00752010000500006. [DOI] [PubMed] [Google Scholar]
- Campaña H, Ermini M, Aiello HA, Krupitzki H, Castilla EE, López-Camelo JS, Latin American Collaborative Study of Congenital Malformations Study Group Prenatal sonographic detection of birth defects in 18 hospitals from South America. J Ultrasound Med. 2010b;29(2):203–212. doi: 10.7863/jum.2010.29.2.203. [DOI] [PubMed] [Google Scholar]
- Castilla EE, Orioli IM (2004) ECLAMC: the Latin-American collaborative study of congenital malformations. Community Genet. 7(2-3):76–94. [DOI] [PubMed]
- CENEP (2007). Morbilidad materna severa en la Argentina. Estimación de la magnitud del aborto inducido. (Severe maternal morbidity in Argentina. Estimation of the magnitude of induced abortion.) www.despenalizacion.org.ar/pdf/Evidencia/Estudios/Estimacion_aborto_inducido.pdf Accessed 20 June 2012
- Christianson A, Howson CP, Modell B. Global report on birth defects. The hidden toll of dying and disabled children. White Plains: March of Dimes Birth Defects Foundation; 2006. [Google Scholar]
- PHG Foundation (2011) Health needs assessment Toolkit, background information on neural tube defects and the impact of interventions. Born Healthy website. http://toolkit.bornhealthy.org/ntd-background.pdf. Last accessed 20 June 2012
- Gadow EC, Paz JE, López-Camelo JS, Dutra MG, Queenan JT, Simpson JL, Jennings VH, Castilla EE. Unintended pregnancies in women delivering at 18 South American hospitals. NFP-ECLAMC Group. Latin American Collaborative Study of Congenital Malformations. Hum Reprod. 1998;13(7):1991–1995. doi: 10.1093/humrep/13.7.1991. [DOI] [PubMed] [Google Scholar]
- INDEC (2010). National Institute for Statistics and Census. www.indec.gov.ar. Accessed 20 June 2012.
- INDEC, National Institute for Statistics and Census (2003) National survey on disabled people. www.indec.mecon.ar/principal.asp?id_tema=166. Accessed 20 June 2012.
- Legislatura de la Ciudad Autónoma de Buenos Aires (2003) Law number 1044 of the Autonomous City of Buenos Aires www.cedom.gov.ar/es/legislacion/normas/leyes/ley1044.html Accessed 20 June 2012
- Liascovich R, Rozental S, Barbero P, Alba L, Ortiz Z. Censo de servicios de genética médica en Argentina (A census of medical genetics services in Argentina) Rev Panam Salud Publica. 2006;19(2):104–111. doi: 10.1590/S1020-49892006000200005. [DOI] [PubMed] [Google Scholar]
- López-Camelo JS, Castilla EE, Orioli IM. Folic acid flour fortification: impact on the frequencies of 52 congenital anomaly types in three South American countries. Am J Med Genet A. 2010;152A(10):2444–2458. doi: 10.1002/ajmg.a.33479. [DOI] [PubMed] [Google Scholar]
- Mario S, Pantelides EA (2009). Estimación de la magnitud del aborto inducido en la Argentina (Estimation of the magnitude of induced abortion in Argentina). www.eclac.cl/publicaciones/xml/1/36501/lcg2405-P_4.pdf. Accessed 20 June 2012
- National law no. 22.431/81. (1981) Comprehensive protection system for the disabled. infoleg.mecon.gov.ar/infolegInternet/anexos/20000-24999/20620/texact.htm Accessed 20 June 2012
- National Ministry of Health, Department of Health Statistics and Research, Vital Statistics (2011) www.deis.gov.ar/Publicaciones/Archivos/Serie5Nro54.pdf. Accessed 20 June 2012.
- Plan Nacer, National Ministry of Health (2012) www.plannacer.msal.gov.ar. Accessed 20 June 2012.
- SAP (2008) Letter to the Congress about Law 25630 flour fortification. www.sap.org.ar/prof-c-2008-21.php. Accessed 20 June 2012
- Silverino Bavio P (2009), “¿Vale más prevenir que lamentar? Comentario a propósito del proyecto de ley que modifica la ley de prevención de defectos congénitos en Argentina”. (Better to be safe than sorry? Comments concerning amendment of the law for prevention of birth defects in Argentina). http://www.revistapersona.com.ar/Persona82/82Bavio.htm. Accessed 20 June 2012 [PubMed]
- SIP (2006) Sistema Informático Perinatal de la República Argentina. Anuario 2006 www.bvspediatria.org.ar/anuario2006.pdf. Accessed 20 June 2012.
- Centro de Informacion Judicial (2012) Supreme Court of Justice ruling. www.cij.gov.ar/nota-8754-La-Corte-Suprema-preciso-el-alcance-del-aborto-no-punible-y-dijo-que-estos-casos-no-deben-ser-judicializados.html. Accessed 20 June 2012
- Williams R, Wright J. Epidemiological issues in health needs assessment. BMJ. 1998;316(7141):1379–1382. doi: 10.1136/bmj.316.7141.1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Assembly (May 2010) Sixty-third world health assembly: birth defects. WHO website http://apps.who.int/gb/ebwha/pdf_files/WHA63/A63_R17-en.pdf. Accessed 20 June 2012
- Community genetic services. Report of a WHO consultation on community genetics in low- and middle-income countries. Switzerland: Geneve; 2010. [Google Scholar]
- World Health Organization (1996) Control of hereditary diseases. Report of a WHO Scientific Group. WHO Technical Report Series 865. [PubMed]
- Wright J, Williams R, Wilkinson JR. Development and importance of health needs assessment. BMJ. 1998;316(7140):1310–1313. doi: 10.1136/bmj.316.7140.1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyszynski D, editor. Neural tube defects: from origin to treatment. New York: Oxford University Press; 2006. [Google Scholar]
- Yi Y, Lindemann M, Colligs A, Snowball C. Economic burden of neural tube defects and impact of prevention with folic acid: a literature review. Eur J Pediatr. 2011;170(11):1391–1400. doi: 10.1007/s00431-011-1492-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zabala R, Waisman I, Corelli M, Tobler B. Ácido fólico para prevenir defectos del tubo neural: consumo e información en mujeres en edad fértil de la Región Centro Cuyo (Folic acid for neural tube defects prevention: consumption and information in fertil-age women in Centro Cuyo Region) Arch argent pediatr. 2008;106(4):295–301. doi: 10.1590/S0325-00752008000400004. [DOI] [PubMed] [Google Scholar]