Abstract
The population of India is extremely diverse comprising of more than 3,000 ethnic groups who still follow endogamy. Haemoglobinopathies are the commonest hereditary disorders in India and pose a major health problem. The data on the prevalence of β-thalassemias and other haemoglobinopathies in different caste/ethnic groups of India is scarce. Therefore the present multicentre study was undertaken in six cities of six states of India (Maharashtra, Gujarat, West Bengal, Assam, Karnataka and Punjab) to determine the prevalence of haemoglobinopathies in different caste/ethnic groups using uniform methodology. Fifty-six thousand seven hundred eighty individuals (college students and pregnant women) from different caste/ethnic groups were screened. RBC indices were measured on an automated haematology counter while the percentage of HbA2, HbF and other abnormal Hb variants were estimated by HPLC on the Variant Hemoglobin Testing System. The overall prevalence of β-thalassemia trait was 2.78 % and varied from 1.48 to 3.64 % in different states, while the prevalence of β-thalassemia trait in 59 ethnic groups varied from 0 to 9.3 %. HbE trait was mainly seen in Dibrugarh in Assam (23.9 %) and Kolkata in West Bengal (3.92 %). In six ethnic groups from Assam, the prevalence of HbE trait varied from 41.1 to 66.7 %. Few subjects with δβ-thalassemia, HPFH, HbS trait, HbD trait, HbE homozygous and HbE β-thalassemia as well as HbS homozygous and HbS-β-thalassemia (<1 %) were also identified. This is the first large multicentre study covering cities from different regions of the country for screening for β-thalassemia carriers and other haemoglobinopathies where uniform protocols and methodology was followed and quality control ensured by the co-ordinating centre. This study also shows that establishment of centres for screening for β-thalassemia and other haemoglobinopathies is possible in medical colleges. Creating awareness, screening and counselling can be done at these centres. This experience will help to formulate a national thalassemia control programme in India.
Keywords: β-Thalassemia, Other haemoglobinopathies, Caste/ethnic goups, India, Multicentre study
Introduction
The inherited disorders of haemoglobin, particularly the β-thalassemias and their interaction with haemoglobin E (HbE) and haemoglobin S (HbS) are a considerable health problem in India and contribute significantly to morbidity and mortality. Earlier studies have shown that the overall prevalence of β-thalassemia is 3–4 % with an estimate of around 8,000 to 10,000 new births with major disease each year (Madan et al. 2010; Balgir 1996). Most of these children have a severe clinical presentation but are managed sub-optimally due to lack of financial resources in majority of the families. Thus preventing the birth of affected children is the best option for India. A prerequisite for this is the knowledge of the prevalence of β-thalassemia and other haemoglobinopathies in different regions of the country and in particular in different ethnic groups. A few studies done earlier have shown that certain communities like the Sindhis, Kutchhi Bhanushalis and Punjabis from Western and Northern India have a high prevalence of β-thalassemia (5–15 %; Sukumaran 1975; Mehta et al. 1972; Balgir 2005) and some population groups from the north eastern regions have a high prevalence of HbE (5–50 %; Das et al. 1980, 1991; Piplani 2000). However, there is not much information on the distribution of β-thalassemia in Karnataka in the south and in the north eastern region.
Realising this, the Indian Council of Medical Research undertook an extensive multicentre study to create awareness in the population and to determine the prevalence of β-thalassemia and other haemoglobinopathies in six states from different regions in India covering a large number of ethnic groups in the country.
Materials and methods
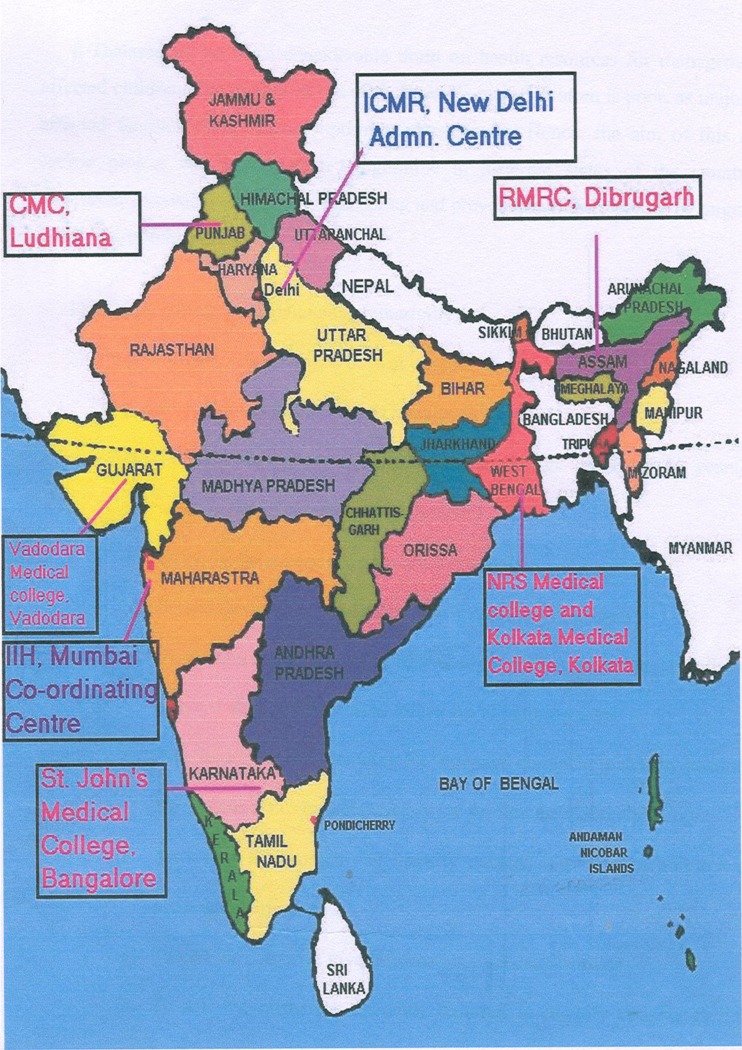
This study was conducted between the years 2000 and 2005 under the “Jai Vigyan Programme” of the former Prime Minister of India. Six centres at Mumbai in Maharashtra and Vadodara in Gujarat in the west, Bangalore in Karnataka in the south, Kolkata in West Bengal in the east, Dibrugarh in Assam in the north east and Ludhiana in Punjab in the north were selected for the study (Fig. 1). National Institute of Immunohaematology in Mumbai was the technical co-ordinating centre.
Fig. 1.
Locations of the co-ordinating centre and the co-investigating centres
Target population
A total of 56,780 individuals were tested. Each centre screened on average 5,000 college or university students (age 17–26 years) and 5,000 pregnant women (age 17–37 years) except the centre at Dibrugarh where only 1,920 pregnant women could be screened. Colleges and antenatal clinics were selected to cover a cross-section of the different cities and individuals from different caste/ethnic groups. The study populations included an undifferentiated mixture of urban and rural people.
Educational talks and audiovisual presentations were given and posters displayed for awareness generation before taking an informed consent for testing. Parental consent was also taken for the college students.
A well-designed proforma was used to get information on the caste/ethnic group, linguistic group and religion, consanguinity in the family, any family history of blood disorders as well as to record all the laboratory findings.
A 5-ml intravenous blood sample was collected in EDTA. RBC indices were measured on a haematology counter (Abacus 2.1). HbA2, HbF and other haemoglobin variants were quantitated by HPLC using the Variant Hemoglobin Testing System (Bio-Rad Laboratories, Hercules CA,USA). HbA2 level of >4.0 % was used as a cutoff for diagnosis of β-thalassemia carriers. Hb electrophoresis on cellulose acetate at pH 8.9 was also done in all the cases (Wild and Bain 2001).
Statistical analysis
The 95 % confidence interval was calculated. The chi-square test was used to compare the distribution of various alleles causing haemoglobinopathies in six cities of India. Gene frequencies of these alleles were calculated by using the Maximum Likelihood method.
Results
The age of the college students ranged from 17 to 26 years and included both males and females in the ratio of 1: 1.2. The antenatal women were in the age group of 17 to 37 years. Table 1 shows the distribution of β-thalassemia and other haemoglobinopathies detected at the six centres. In all, 56,780 individuals were screened and the overall prevalence of β-thalassemia carriers was 2.78 % (95 % CI 2.66–2.94). Ludhiana and Kolkata had the highest prevalence 3.96 % (95 % CI 3.62–4.38) and 3.64 % (95 % CI 3.23–3.97), respectively, while Dibrugarh showed the lowest prevalence, 1.48 % (95 % CI 1.21–1.79). Sporadic cases of δβ-thalassemia trait—0.06 % (95 % CI 0.01–0.11) and HPFH trait were more commonly encountered in the western region in Vadodara—2.94 % (95 % CI 2.57–3.23) and in Mumbai—0.53 % (95 % CI 0.39–0.67) while HbD trait was mainly seen in the northern region in Ludhiana (1.09 %). HbE trait was highly prevalent in Dibrugarh—23.9 % (95 % CI 22.99–25.01) and was also more common in Kolkata—3.92 % (95 % CI 3.52–4.28) while few cases were also seen in the other regions. The prevalence of homozygous HbE disease was 5.33 % in Dibrugarh (95 % CI 4.77–5.83) and of HbE–β-thalassemia was 1.44 % (95 % CI 1.12–1.68). Few individuals with sickle cell disease, sickle–β-thalassemia, HbD homozygous, HbD–β-thalassemia, HbD Iran trait, HbQ India trait and Hb Lepore trait were also encountered at the different centres.
Table 1.
Prevalence of β-thalassemia and other haemoglobinopathies in six cities of India
| Sr no | Name of the city | Number screened | β-Thal trait, no. (%) | δβ Thal trait, no. (%) | HPFH trait, no. (%) | HbS trait, no. (%) | HbD trait, no. (%) | HbE trait, no. (%) | HbS homozygous, no. (%) | HbE homozygous, no. (%) | HbE-β-Thal, no. (%) | HbS-β-Thal, no. (%) | Other haemoglobino pathies |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Bangalore | 9,981 (95%CI) | 216 (2.16 %) | 13 (0.13 %) | 39(0.39 %) | 20 (0.20 %) | 19 (0.19 %) | 13 (0.13 %) | 7 (0.07 %) | 3 (0.03 %) | 1 (0.01 %) | 6 (0.06 %) | HbD-homozygous, 2; othersa, 1 |
| (1.87–2.45) | (0.06–0.2) | (0.27–0.51) | (0.11–0.29) | (0.1–0.28) | (0.06–0.2) | (0.02–0.12) | (0–0.06) | (−0.01–0.03) | (0.01–0.14) | ||||
| 2 | Kolkata | 9,990 (95%CI) | 364 (3.64 %) | 2 (0.02 %) | 13 (0.13 %) | 14 (0.14 %) | 20 (0.2 %) | 392 (3.92 %) | 1 (0.01 %) | 12 (0.12 %) | 9(0.09 %) | – | HbD-β-thal, 1; HbD-homozygous, 1; othersa, 14 |
| (3.23–3.97) | (−0.01–0.05) | (0.06–0.2) | (0.07–0.21) | (0.11–0.29) | (3.52–4.28) | (−0.01–0.03) | (0.5–0.19) | (0.03–0.15) | |||||
| 3 | Dibrugarh | 6,816 (95%CI) | 101 (1.48 %) | 5 (0.73 %) | 12 (0.18 %) | 9 (0.13 %) | 1 (0.02 %) | 1,629 (23.9 %) | 0 | 363 (5.33 %) | 98 (1.44 %) | 3 (0.04 %) | – |
| (1.21–1.79) | (0.53–0.93) | (0.08–0.28) | (0.04–0.22) | (−0.01–0.05) | (22.99–25.01) | (4.77–5.83) | (1.12–1.68) | (−0.01–0.09) | |||||
| 4 | Ludhiana | 9,991 (95%CI) | 375 (3.96 %) | 2 (0.02 %) | 0 | 6 (0.06 %) | 109 (1.09 %) | 4 (0.04 %) | 0 | 1 | 0 | 0 | HbD-β-thal, 2; HbD- homozygous, 3; othersa, 25 |
| (3.62–4.38) | (−0.01–0.05) | (0.01 −0.11) | (0.9–1.3) | (0–0.08) | |||||||||
| 5 | Mumbai | 10,011 (95%CI) | 255 (2.55 %) | 7 (0.07 %) | 20 (0.2 %) | 53 (0.53 %) | 21 (0.21 %) | 13 (0.13 %) | 0 | 0 | 0 | 0 | Othersa, 9 |
| (2.29–2.91) | (0.02–0.12) | (0.11–0.29) | (0.39–0.67) | (0.12–0.3) | (0.06–0.2) | ||||||||
| 6 | Vadodara | 9,991 (95%CI) | 268 (2.68 %) | 6 (0.06 %) | 9 (0.09 %) | 294 (2.94 %) | 34 (0.34 %) | 12 (0.12 %) | 14 (0.14 %) | 0 | 1 | 0 | HbD-β-thal, 2; HbD-homozygous, 3; othersa, 9 |
| (2.38–3.02) | (0.01–0.11) | (0.03–0.15) | (2.57–3.23) | (0.23–0.45) | (0.05–0.19) | (0.07–0.21) | |||||||
| Total | 56,780 (95%CI) | 1,579 (2.78 %) | 35 (0.06 %) | 93 (0.16 %) | 396 (0.70 %) | 204 (0.36 %) | 2,063 (3.63 %) | 22 (0.04 %) | 379 (0.67 %) | 108 (0.19 %) | 9 (0.02 %) | HbD–homozygous, 7; HbD-β–thal, 4; othersa, 58 | |
| (2.66–2.94) | (0.04–0.08) | (0.13–0.19) | (0.63–0.77) | (0.26–0.34) | (3.45–3.75) | (0.02–0.06) | (0.6–0.74) | (0.15–0.23) | (0.01–0.03) |
aOthers—HbD—Iran, HbQ—India and Hb—Lepore trait
Table 2 shows the prevalence of β-thalassemia heterozygotes analysed according to the caste/ethnic groups of the individuals at the different centres. There were 100 different ethnic groups representing the ethnic diversity of the population. In 38 of these groups, the number of individuals screened was less than 50 and they were thus grouped together as “Others”. This group also included individuals who did not mention their caste/ethnic groups but only mentioned their religion on the proforma. The tea garden workers mainly seen in Dibrugarh who were migrants from Bihar, Orissa and West Bengal were also put under this group. The specific groups under the scheduled castes and scheduled tribes were only mentioned at one centre (Dibrugarh), hence this division could not be given for the other centres. Among the remaining caste/ethnic groups, the prevalence of β-thalassemia carriers was high (5–10 %) among the Rajputs, Jains, Sunnis, Shiyas and Pathans in Bangalore, Mandals in Kolkata, Brahmins in Dibrugarh, Aroras and Ravidasis in Ludhiana, Rajputs and Vellalas in Mumbai, Kshatriyas and Lohanas in Vadodara.
Table 2.
Prevalence of β-thalassemia heterozygotes among various caste/ethnic groups screened at different centres
| β-Thal trait no./total (%) | CI (95 %) | |
|---|---|---|
| Bangalore | ||
| Brahmin | 10/662 (1.5 %) | 0.57–2.42 |
| Kshatriya | 12/426 (2.8 %) | 1.23–4.37 |
| Naidu | 6/366 (1.6 %) | 0.31–2.89 |
| Reddy | 4/222 (1.8 %) | 0.05–3.55 |
| Mudiar | 4/211 (1.9 %) | 0.06–3.74 |
| Baidya | 1/104 (1.0 %) | −0.91–2.91 |
| Rajput | 4/64 (6.3 %) | 0.35–12.25 |
| Shetty | 1/53 (1.9 %) | −1.78–5.58 |
| Vokaliga | 36/1,691 (2.1 %) | 1.42–2.78 |
| Jain | 12/125 (9.6 %) | 4.44–14.76 |
| Sunni | 15/259 (5.8 %) | 2.95–8.65 |
| Shiya | 4/63 (6.3 %) | 0.3–12.3 |
| Pathan | 8/163 (4.9 %) | 1.59–8.21 |
| Shaikh | 5/459 (1.1 %) | 0.15–2.05 |
| Roman Catholic | 3/303 (1.0 %) | −0.12–2.12 |
| Protestant | 1/91 (1.1 %) | −1.04–3.24 |
| Artisana | 20/1,096 (1.8 %) | 1.01–2.59 |
| Scheduled caste | 26/1,567 (1.7 %) | 1.06–2.34 |
| Scheduled tribe | 2/218 (1.4 %) | −0.16–2.96 |
| Othersb | 29/1,242 (2.3 %) | 1.47–3.13 |
| Total | 204/9,385 (2.2 %) | 1.9–2.5 |
| Kolkata | ||
| Brahmin | 42/1,111 (3.8 %) | 2.68–4.92 |
| Kayasta | 40/2,263 (1.8 %) | 1.25–2.35 |
| Mandal | 12/140 (8.6 %) | 3.96–13.24 |
| Baidyas | 11/343 (3.2 %) | 1.34–5.06 |
| Rajput | 2/82 (2.4 %) | −0.91–5.71 |
| Sunni | 5/211 (2.4 %) | 0.33–4.47 |
| Shiya | 3/101 (3.0 %) | −0.33–6.33 |
| Shaikh | 5/209 (2.4 %) | 0.33–4.47 |
| Momin | 0/75 (0) | – |
| Artisana | 48/1,302 (3.7 %) | 2.67–4.73 |
| Scheduled caste | 84/2,199 (3.8 %) | 3–4.6 |
| Scheduled tribe | 3/70 (4.3 %) | −0.45–9.05 |
| Othersb | 35/778 (4.5 %) | 3.04–5.96 |
| Total | 280/8,884 (3.2 %) | 2.83–3.57 |
| Dibrugarh | ||
| Brahmin | 22/368 (6.0 %) | 3.57–8.43 |
| Kolita | 15/1,216 (1.2 %) | 0.59–1.81 |
| Koch | 2/360 (0.6 %) | −0.2–1.4 |
| Meistes | 0/99 (0) | – |
| Keot | 0/51 (0) | – |
| Muttak | 0/124(0) | – |
| Jain | 5/123 (4.1 %) | 0.6–7.6 |
| Sunni | 1/52 (1.9 %) | −1.81–5.61 |
| Ahom | 8/915 (0.9 %) | 0.29–1.51 |
| Chutia | 0/74 (0) | – |
| Shut | 0/52 (0) | – |
| Nath | 0/68 (0) | – |
| Kaiberta | 8/335 (2.4) | 0.76–4.04 |
| Bodo | 0/166 (0) | – |
| Kachari | 2/305 (0.7 %) | −0.24–1.64 |
| Deori | 0/51 (0) | – |
| Mishing | 0/229 (0) | – |
| Othersb | 49/2,226 (2.2 %) | 1.59–2.81 |
| Total | 112/6,814 (1.6 %) | 1.3–1.9 |
| Ludhiana | ||
| Brahmin | 22/813 (2.7 %) | 1.59–3.81 |
| Jat Sikh | 45/1,638 (2.7 %) | 1.92–3.48 |
| Khatri | 81/1,743 (4.6 %) | 3.62–5.58 |
| Arora | 90/923 (9.8 %) | 7.88–11.72 |
| Rajput | 17/502 (3.4 %) | 1.81–4.99 |
| Ram Gariah Sikh | 10/220 (4.5 %) | 1.76–7.24 |
| Ramdasi Sikh | 0/98 (0) | – |
| Ravidasi | 6/111 (5.4 %) | 1.2–9.6 |
| Saini | 2/75 (2.7 %) | −0.97–6.37 |
| Jain | 10/238 (4.2 %) | 1.65–6.75 |
| Baniya | 25/600 (4.2 %) | 2.59–5.81 |
| Sunni | 1/79 (1.3 %) | −1.2–3.8 |
| Protestant | 2/146 (1.4 %) | −0.51–3.31 |
| Pentacoste | 5/261 (1.9 %) | 0.24–3.56 |
| Artisana | 24/631 (3.8 %) | 2.31–5.29 |
| Scheduled caste | 21/1,092 (1.9 %) | 1.09–2.71 |
| Othersb | 9/592 (1.5 %) | 0.52–2.48 |
| Total | 370/9,762 (3.8 %) | 3.42–4.18 |
| Mumbai | ||
| Brahmin | 13/495 (2.6 %) | 1.2–4.0 |
| Maratha | 14/883 (1.6 %) | 0.77–2.43 |
| Baidyas | 11/369 (3.0 %) | 1.26–4.74 |
| Baidevi | 2/115 (1.7 %) | −0.66–4.06 |
| Bhandari | 3/104 (2.9 %) | −0.33–6.13 |
| Jaiswal | 1/101 (1.0 %) | −0.94–2.94 |
| Rajput | 6/101 (5.9 %) | 1.3–10.5 |
| Khatri | 2/70 (2.9 %) | −1.03–6.83 |
| Kaller | 1/59 (1.7 %) | −1.6–5.0 |
| Shetty | 7/252 (2.8 %) | 0.76–4.84 |
| Vellala | 8/76 (10.5 %) | 3.61–17.39 |
| Baniya | 1/92 (1.1 %) | −1.03–3.23 |
| Patel | 0/54 (0) | – |
| Jain | 5/136 (3.7 %) | 0.53–6.87 |
| Kunbi | 1/134 (0.7 %) | −0.71–2.11 |
| Sunni | 3/152 (2.0 %) | −0.23–4.23 |
| Shiya | 8/264 (3.0 %) | 0.94–5.06 |
| Shaikh | 13/484 (2.7 %) | 1.26–4.14 |
| Ansari | 0/79 (0) | − |
| Sayeed | 3/99 (3.0 %) | −0.36–6.36 |
| Protestant | 2/88 (2.3 %) | −0.83–5.43 |
| Artisana | 30/1,121 (2.7 %) | 1.75–3.65 |
| Scheduled caste | 45/1,228 (3.7 %) | 2.64–4.76 |
| Scheduled tribe | 3/138 (2.2 %) | −0.25–4.65 |
| Othersb | 34/1,473 (2.3 %) | 1.53–3.07 |
| Total | 216/8,167 (2.6 %) | 2.25–2.95 |
| Vadodara | ||
| Brahmin | 18/960 (1.9 %) | 1.04–2.76 |
| Kshatriya | 5/93 (5.4 %) | 0.81–9.99 |
| Patel | 31/1,117 (2.8 %) | 1.83–3.77 |
| Parmar | 6/173 (3.5 %) | 0.76–6.24 |
| Jain | 21/697 (3.01 %) | 1.74–4.28 |
| Baniya | 8/197 (4.1 %) | 1.33–6.87 |
| Lohana | 7/95 (7.4 %) | 2.14–12.66 |
| Prajapati | 3/191 (1.57 %) | −0.19–3.33 |
| Rajput | 17/718 (2.4 %) | 1.28–3.52 |
| Maratha | 13/410 (3.2 %) | 1.5–4.9 |
| Sindhi | 2/98 (2.0 %) | −0.77–4.77 |
| Sunni | 10/349 (2.9 %) | 1.14–4.66 |
| Shaikh | 4/100 (4 %) | 0.16–7.84 |
| Bohra | 1/74 (1.4 %) | −1.28–4.08 |
| Pathan | 3/80 (3.8 %) | −0.39–7.99 |
| Protestant | 3/81 (3.70 %) | −0.41–7.81 |
| Artisana | 39/1,661 (2.4 %) | 1.66–3.14 |
| Scheduled caste | 30/1,070 (2.8 %) | 1.81–3.79 |
| Scheduled tribe | 5/597 (0.8 %) | 0.09–1.51 |
| Othersb | 15/763 (2.0 %) | 1.01–2.99 |
| Total | 241/9,524 (2.5 %) | 2.19–2.81 |
aArtisans—this includes a pool of different occupational castes like Chammars (Coblers), Lohars (Blacksmith), Sonar (Goldsmith)
bOthers—all the caste/ethnic groups where the total sample size were less than 50, those groups where the caste/ethnic groups were not mentioned and the Tea Garden workers in Assam were pooled together under this group
The prevalence of HbE heterozygotes were also analysed in different caste/ethnic groups for two centres (Kolkata and Dibrugarh) where the prevalence of HbE was high (Table 3). A high prevalence of HbE heterozygotes was seen among the Mandals, Sunnis and Shiyas in Kolkata (5–6.2 %) and almost all the castes/ethnic groups in Dibrugarh (9.5–66.7 %). The prevalence of HbE trait at the other centres was very low (0.04–0.13 %) and is therefore not presented in different caste groups.
Table 3.
Prevalence of HbE Trait among various caste/ethnic groups screened at Kolkata and Dibrugarh
| HbE trait no/total (%) | CI (95 %) | |
|---|---|---|
| Kolkata | ||
| Brahmin | 21/1,111 (1.9 %) | 1.1–2.7 |
| Kayastha | 99/2,263 (4.4 %) | 3.55–5.25 |
| Mandal | 8/140 (5.7 %) | 1.86–9.54 |
| Baidyas | 8/343 (2.3 %) | 0.71–3.89 |
| Rajput | 1/82 (1.2 %) | −1.16–3.56 |
| Sunni | 13/211 (6.2 %) | 2.95–9.45 |
| Shiya | 5/101 (5.0 %) | 0.75–9.25 |
| Shaikh | 7/209 (3.3 %) | 0.88–5.72 |
| Momin | 1/75 (1.3 %) | −1.26–3.86 |
| Artisana | 50/1,302 (3.8 %) | 2.76–4.84 |
| Scheduled caste | 105/2,199 (4.8 %) | 3.91–5.69 |
| Scheduled tribe | 3/70 (4.3 %) | −0.45–9.05 |
| Othersb | 23/778 (3.0 %) | 1.8–4.2 |
| Total | 344/8,884 (3.9 %) | 3.5–4.3 |
| Dibrugarh | ||
| Brahmin | 35/368 (9.5 %) | 6.5–12.5 |
| Kolita | 279/1,216 (22.9 %) | 20.54–25.26 |
| Koch | 127/360 (35.3 %) | 30.36–40.24 |
| Meistes | 10/99 (10.1 %) | 4.16–16.04 |
| Keot | 14/51 (27.5 %) | 15.25–39.75 |
| Muttak | 51/124 (41.1 %) | 32.44–49.76 |
| Jain | 0/123 (0) | – |
| Sunni | 9/52 (17.3 %) | 7.02–27.58 |
| Ahom | 402/915 (43.9 %) | 40.68–47.12 |
| Chutia | 21/74 (28.4 %) | 18.3–38.67 |
| Shut | 6/52 (11.5 %) | 2.83–20.17 |
| Meth | 23/68 (33.8 %) | 22.56–45.04 |
| Kaiberta | 80/335 (23.9 %) | 19.33–28.47 |
| Bodo | 72/166 (43.4 %) | 35.86–50.94 |
| Kachari | 146/305 (47.9 %) | 42.29–53.51 |
| Deori | 34/51 (66.7 %) | 53.77–79.63 |
| Mishing | 108/229 (47.2 %) | 40.73–53.67 |
| Othersb | 212/2,226 (9.5 %) | 8.28–10.72 |
| Total | 1,629/6,814 (23.9 %) | 22.89–24.91 |
Artisansa—This includes a pool of different occupational castes like Chammars (Coblers), Lohars (Blacksmith), Sonar (Goldsmith)
Othersb—All the caste/ethnic groups where the total sample size were less than 50, those groups where the caste/ethnic groups were not mentioned and the Tea Garden workers in Assam were pooled together under this group
Majority of the individuals screened belonged to the Hindu religion (78.2 %) while 9 % were Muslims, 6.4 % were Sikhs, 3.2 % were Christians, 2.1 % were Jains and 1 % were Buddhists.
The prevalence of β-thalassemia, HbS, HbD and HbE trait in different religious groups from the six cities is shown in Table 4. Jains from Bangalore had the highest prevalence of β-thalassemia trait (9.6 %) followed by Buddhists who were seen only in Mumbai (5.9 %) and Sikhs from Ludhiana (3.7 %). The prevalence of β-thalassemia trait among the same religious group in different cities was quite variable. HbS trait was also more common among the Buddhists in Mumbai (1.7 %) while HbD trait was more common among the Sikhs (1.4 %). The prevalence of HbE trait was the highest among the Hindus in Dibrugarh (25.2) followed by the Christian (21.4 %) and the Muslims from the same centre (13.6 %).
Table 4.
Prevalence of haemoglobinopathies in different religious groups in the six cities
| No. of individuals | β-Thal trait | HbS trait | HbD trait | HbE trait | |
|---|---|---|---|---|---|
| Hindu | |||||
| Bangalore CI (95 %) | 7,896 | 1.97 % (1.66–2.28) | 0.19 % (0.09–0.29) | 0.2 % (0.1–0.3) | 0.06 % (0.01–0.11) |
| Kolkata CI (95 %) | 8,803 | 3.77 % (3.37–4.17) | 0.11 % (0.04–0.18) | 0.19 % (0.19–0.28) | 3.94 % (3.53–4.35) |
| Dibrugarh CI (95 %) | 5,927 | 1.55 % (1.24–1.86) | 0.15 % (0.05–0.25) | 0.01 % (–0.02–0.04) | 25.20 % (24.09–26.31) |
| Ludhiana CI (95 %) | 5,441 | 4.17 % (3.64–4.7) | 0.05 % (−0.01–0.11) | 0.99 % (0.73–1.25) | 0.01 % (−0.02–0.04) |
| Mumbai CI (95 %) | 6,523 | 2.36 % (1.99–2.73) | 0.55 % (0.37–0.73) | 0.21 % (0.1–0.32) | 0.10 % (0.02–0.18) |
| Vadodara CI (95 %) | 8,133 | 2.59 % (2.24–2.94) | 3.08 % (2.7–3.46) | 0.33 % (0.21–0.45) | 0.11 % (0.04–0.18) |
| Muslim | |||||
| Bangalore CI (95 %) | 1,296 | 2.95 % (2.03–3.87) | 0.15 % (−0.06–0.36) | 0.07 % (−0.07–0.21) | 0.55 % (0.15–0.95) |
| Kolkata CI (95 %) | 1,116 | 2.68 % (1.73–3.63) | 0.26 % (−0.04–0.56) | 0.17 % (−0.07–0.41) | 3.85 % (2.72–4.98) |
| Dibrugarh CI (95 %) | 667 | 0.74 % (0.09–1.39) | 0 | 0 | 13.64 % (11.04–16.24) |
| Ludhiana CI (95 %) | 182 | 1.64 % (−0.21–3.49) | 0 | 0 | 0.54 % (−0.52–1.6) |
| Mumbai CI (95 %) | 1,649 | 2.44 % (1.7–3.18) | 0.41 % (0.1–0.72) | 0.22 % (−0.01–0.45) | 0.27 % (0.02–0.52) |
| Vadodara CI (95 %) | 971 | 3.29 % (2.17–4.41) | 1.85 % (1–2.7) | 0.30 % (−0.04–0.64) | 0.20 % (−0.08–0.48) |
| Buddhist | |||||
| Mumbai CI (95 %) | 560 | 5.89 % (3.94–7.84) | 1.7 % (0.63–2.77) | 0 | 0 |
| Jain | |||||
| Bangalore CI (95 %) | 125 | 9.67 % (4.49–14.85) | 0 | 0 | 0 |
| Ludhiana CI (95 %) | 238 | 4.23 % (1.67–6.79) | 0 | 0 | 0.4 % (−0.4–1.2) |
| Mumbai CI (95 %) | 136 | 3.7 % (0.53–6.87) | 0 | 0 | 0 |
| Vadodara CI (95 %) | 697 | 3.0 % (1.73–4.27) | 0 | 0 | 0 |
| Sikh | |||||
| Ludhiana CI (95 %) | 3,485 | 3.67 % (3.05–4.29) | 0.02 % (−0.03–0.07) | 1.43 % (1.04–1.82) | 0.02 % (−0.03–0.07) |
| Christian | |||||
| Bangalore CI (95 %) | 493 | 0.87 % (0.05–1.69) | 0.43 % (−0.15–1.01) | 0.21 % (−0.19–0.61) | 0.21 % (−0.19–0.61) |
| Dibrugarh CI (95 %) | 131 | 0.76 % (−0.73–2.25) | 0 | 0 | 21.37 % (14.29–28.31) |
| Ludhiana CI (95 %) | 672 | 1.04 % (0.27–1.81) | 0.29 % (−0.12–0.7) | 0.74 % (0.09–1.39) | 0 |
| Mumbai CI (95 %) | 317 | 2.20 % (0.59–3.81) | 0 | 0.63 % (−0.24–1.5) | 0 |
| Vadodara CI (95 %) | 168 | 3.19 % (0.53–5.85) | 2.12 % (−0.06–4.3) | 1.06 % (−0.49–2.61) | 0 |
Gene frequencies of various alleles causing haemoglobinopathies in the six cities are shown in Table 5. β-thalassemia (0.0112–0.0189) δβ-thalassemia (0.0000–0.0004) and HPFH (0.0000–0.0020) show more or less even distribution in the six cities. However the abnormal haemoglobins showed an uneven distribution. The gene frequency of HbS was the highest in Vadodara (0.0161) while that of HbE (0.1799) and HbD (0.0059) was the highest in Dibrugarh and Ludhiana, respectively.
Table 5.
Gene frequencies of various alleles causing haemoglobinopathies in six cities from India
| β-Thal allele | δβThal allele | HPFH allele | HbS allele | HbD allele | HbE allele | |
|---|---|---|---|---|---|---|
| Bangalore | 0.0112 | 0.001 | 0.0020 | 0.0020 | 0.0012 | 0.0010 |
| Kolkata | 0.0187 | 0.0000 | 0.0007 | 0.0008 | 0.0012 | 0.0213 |
| Dibrugarh | 0.0148 | 0.0004 | 0.0009 | 0.0009 | 0.0000 | 0.1799 |
| Ludhiana | 0.0189 | 0.0001 | 0.0000 | 0.0003 | 0.0059 | 0.0003 |
| Mumbai | 0.0127 | 0.0004 | 0.0010 | 0.0026 | 0.0010 | 0.0007 |
| Vadodara | 0.0136 | 0.0003 | 0.0005 | 0.0161 | 0.0021 | 0.0007 |
Chi-square test revealed no significant differences in the distribution of β-thalassemia between Bangalore and Mumbai (3.19), Kolkata and Ludhiana (0.16) and Mumbai and Vadodara (0.36) while significant differences were observed between Bangalore and Kolkata (38.75), Bangalore and Dibrugarh (10.18), Bangalore and Ludhiana (43.92), Bangalore and Vadodara (5.67), Kolkata and Dibrugarh (70.38), Kolkata and Mumbai (20.04), Kolkata and Vadodara (15.07), Dibrugarh and Ludhiana (75.97), Dibrugah and Mumbai (22.22), Dibrugarh and Vadodara (27.20) and Ludhiana and Mumbai (23.85). The values in the brackets are χ2 values for 1° of freedom. Due to the small sample size, δβ-thalassemia and HPFH were combined under one category (high HbF determinants) for analysis. Fifty percent of the combinations revealed non-significant values at 1 d.f. (Kolkata × Dibrugarh 2.10, Kolkata × Mumbai 3.41, Kolkata × Vadodara 0, Dibrugarh × Mumbai 0.06, Dibrugarh × Vadodara 2.10 and Mumbai × Vadodara 3.41)
Discussion
India has a population of 1.21 billion according to the Census in 2011. There are 4,693 endogamous communities which includes 427 tribal groups. Although β-thalassemia and other haemoglobinopathies are seen in all the states, the prevalence is quite variable.
There have been several previous studies on screening different communities for β-thalassemia and other abnormal haemoglobins but the number of individuals studied have been few, some of the studies were hospital based and the methodology used has not been uniform (Balgir 1996, 2005; Sukumaran 1975; Mehta et al. 1972; Chhotray et al. 2004; Munshi et al. 2009).
The first multicentre study was done by the Indian Council of Medical Research in the mid 1980s where high school children from Mumbai in the West, Delhi in the North and Kolkata in the East were studied. In this study the prevalence of β-thalassemia trait was 2.7 % in Mumbai, 5.5 % in Delhi and 10.2 % in Kolkata (Madan et al. 2010). However, a follow-up of heterozygotes done about 20 years after screening in Mumbai found that counselling children at the school going age did not have the desired impact (Colah et al. 2007).
The present study included university students and pregnant women. This is the first large community-based study done systematically in six states of India using uniform protocols and methodology as well as quality control exercised by the co-ordinating centre in Mumbai which has a long experience in screening for haemoglobinopathies. This study has shown that it is feasible to establish centres for education, screening and counselling in medical colleges and other institutions where these facilities were not available and will help in formulating a National Thalassemia Control Programme in the country.
Due to sociocultural practices, marriages in India are usually among individuals of the same caste or ethnic group and this makes it important to know the prevalence of β-thalassemia and also HbE in different ethnic groups.
The prevalence of β-thalassemia varied from 0 to 10.5 % among the different caste/ethnic groups in this study and the prevalence of HbE trait varied from 0 to 66.6 % in the two eastern and north eastern cities. A large study done among the Sindhis of Nagpur in Maharashtra had shown the prevalence of β-thalassemia trait to be 16.81 % (Mulchandani et al. 2008). However the prevalence was found to be extremely variable among the subcastes of Sindhis, Larkhana Sindhis showed the highest prevalence (17 %) while Dadu Sindhis showed the lowest prevalence (8 %) of β-thalassemia (Jawahirani et al. 2007). Considerable differences in the prevalence of β-thalassemia have been shown earlier in different districts of Maharashtra (1–6 %) and Gujarat (0–9.5 %) in western India (Colah et al. 2010). A recent large study on screening for haemoglobinopathies among non-tribal and tribal populations from different cities in Gujarat showed an overall prevalence of β-thalassemia trait of 1.95 % and HbS trait of 6.5 %. A high prevalence of β-thalassemia trait was seen among the Bhanushalis (8.1 %), Bhakta (7.9 %) and Lohanas (6.5 %; Patel et al. 2012) Tribal groups in Maharashtra have shown a prevalence of β-thalassemia trait of 1.6 to 5.6 % (Rao and Gorakshakar 1990) while the prevalence of β-thalassemia trait has also been high (6.3 to 8.5 %) among some tribal groups in Orissa (Balgir 2005, 2006) and in the non-tribal populations of Madhya Pradesh in Central India (9.59 %; Chatterjee et al. 2010). Thus β-thalassemia is not uncommon among many non-tribal and tribal populations in India. Earlier studies on HbE have shown that the prevalence is very variable with some population groups like the Mizos from Mizoram in the north east having a prevalence of HbE trait of 1.5 % (Dash et al. 2005) while among the different tribal groups is Tripura and among the Mishings of Upper Assam and Phayengs and Khurkhvels of Manipur the prevalence of HbE ranged from 16.2 to 47.3 % (Das et al. 1991; Das and Sengupta 2008; Singh and Singh 2008). The Bodo-Kacharis were shown earlier to have one of the highest reported prevalence of HbE trait (64 %; Deka et al. 1988). Our studies are in agreement with some of these earlier reports. A recent report on screening 35,413 individuals from rural areas in West Bengal showed that the prevalence of HbE carriers was 4.3 % while β-thalaseemia carriers was 10.38 % and HbS and HbD carriers was 1.12 % and 0.37 %, respectively (Dolai et al. 2012).
We have also shown that the prevalence of HbE–β-thalassemia in Dibrugarh is 1.44 %. This finding is important as an earlier report has stated that there are only seven cases of HbE β-thalassemia from north eastern India in the literature as opposed to 67,332 predicted cases (Krishnamurti 2000). Subsequently, some reports on HbE-β-thalassemia have been published form North India as well as North East India (Chhotray et al. 2003; Panigrahi et al. 2005; Kakkar 2005; Patne and Shukla 2009).
This is also the first large study to show the prevalence of δβ-thalassemia and HPFH in the Indian population. Interaction of δβ-thalassemia with β-thalassemia can result in a severe disorder and identifying these conditions is important for genetic counselling.
The success of prevention programmes for the control of thalassemias in countries like Cyprus, Italy and Greece have shown that education and screening forms the most important part of these programme (Angastiniotis et al. 1995; Cao et al. 2002; Loukopoulos 2011). It has also been emphasised that there is remarkable diversity in the frequency of the β-thalassemias and carriers of other haemoglobin variants even within small geographic regions in different countries and hence accurate micromapping is important to estimate the disease burden (Weatherall 2011). Our study is therefore important to pave the way for a National Thalassemia Control Programme.
Acknowledgment
We are grateful to the Indian Council of Medical Research, New Delhi for financial support. We thank all the staff appointed on this project at the different centres for their technical support.
References
- Angastiniotis M, Modell B, Englezos P, Boulyjenkov V. Prevention and control of hemoglobinopathies. Bull World Health Organ. 1995;73:375–386. [PMC free article] [PubMed] [Google Scholar]
- Balgir RS. Genetic epidemiology of the three abnormal hemoglobins in India. J Assoc Physicians India. 1996;44:25–28. [PubMed] [Google Scholar]
- Balgir RS. Spectrum of hemoglobinopathies in the state of Orissa, India: a ten years cohort study. JAPI. 2005;53:1021–1026. [PubMed] [Google Scholar]
- Balgir RS. Genetic heterogeneity of population structure in 15 major scheduled tribes in central & eastern India: a study of immuno-hematological disorders. Indian J Hum Genet. 2006;12:86–92. doi: 10.4103/0971-6866.27792. [DOI] [Google Scholar]
- Cao A, Rosatelli MC, Monni G, Galanello R. Screening for thalassemias: a model of success. Obstet Gynaecol Clin N Am. 2002;29:305–328. doi: 10.1016/S0889-8545(01)00006-7. [DOI] [PubMed] [Google Scholar]
- Chatterjee N, Mishra A, Soni R, Kulkarni H, Mantani M, Shrivastava M. Bayesian estimates of the prevalence of β-thalassemia trait in voluntary blood donors of central India: a survey. Hemoglobin. 2010;34:548–560. doi: 10.3109/03630269.2010.526488. [DOI] [PubMed] [Google Scholar]
- Chhotray GP, Dash BP, Ranjit MR, Colah RB, Mohanty D. Hemoglobin E/beta thalassemia—an experience in the eastern Indian state of Orissa. Acta Hematol. 2003;109:214–216. doi: 10.1159/000070976. [DOI] [PubMed] [Google Scholar]
- Chhotray GP, Dash BP, Ranjit M. Spectrum of hemoglobinopathies in Orissa, India. Hemoglobin. 2004;28:117–122. doi: 10.1081/HEM-120034244. [DOI] [PubMed] [Google Scholar]
- Colah R, Thomas M, Mayekar P. Assessing the impact of screening & counseling high school children for beta thalassemia in India. J Med Screen. 2007;14:158. doi: 10.1258/096914107782066202. [DOI] [PubMed] [Google Scholar]
- Colah R, Gorakshakar A, Phansagaonkar S, D'Souza E, Nadkarni A, Surve R, Sawant P, Master D, Patel R, Ghosh K, Mohanty D. Epidemiology of β-thalassemia is western India: mapping the frequencies and mutation in sub-regions of Maharashtra and Gujarat. Br J Haematol. 2010;149:739–747. doi: 10.1111/j.1365-2141.2010.08131.x. [DOI] [PubMed] [Google Scholar]
- Das B, Sengupta S. HbE genotypes and fertility: a study on a Tibeto–Burmese population in Upper Assam, India. Ann Hum Biol. 2008;35:422–431. doi: 10.1080/03014460802221121. [DOI] [PubMed] [Google Scholar]
- Das BM, Deka R, Das R. Hemoglobin E in six populations of Assam. J Indian Anthropol Soc. 1980;15:153–156. [Google Scholar]
- Das MK, Dey B, Roy M, Mukherjee BM. High prevalence of HbE in 3 populations of the Malda district, West Bengal, India. Hum Hered. 1991;41:84–88. doi: 10.1159/000153983. [DOI] [PubMed] [Google Scholar]
- Dash S, Chhanchimi L, Chhakchhuek L, Zomawaia E. Screening for hemoglobinopathies and G6PD deficiency among the Mizos of Mizoram: a preliminary study. Indian J Pathol Microbiol. 2005;48:17–18. [PubMed] [Google Scholar]
- Deka R, Reddy AP, Mukherjee BM, Das BM, Banerjee S, Roy M, et al. Hemoglobin E distribution in ten endogamous population groups of Assam, India. Hum Hered. 1988;38:261–266. doi: 10.1159/000153796. [DOI] [PubMed] [Google Scholar]
- Dolai TK, Dutta S, Bhattacharyya M, Ghosh MK. Prevalence of hemoglobinopathies in rural Bengal, India. Hemoglobin. 2012;36:57–63. doi: 10.3109/03630269.2011.621007. [DOI] [PubMed] [Google Scholar]
- Jawahirani A, Mamtani M, Das K, Rughwani V, Kulkarni H. Prevalence of beta thalassemia in subcastes of Indian Sindhis: results from a two phase survey. Public Health. 2007;121:193–198. doi: 10.1016/j.puhe.2006.10.017. [DOI] [PubMed] [Google Scholar]
- Kakkar N. Hemoglobin E–thalassemia in a Sikh child: a case report. Indian J Pathol Microbiol. 2005;48:408–410. [PubMed] [Google Scholar]
- Krishnamurti L. Few case of HbE –β thalassemias in Northeast India. Under diagnosis or complete exclusion of β thalassemias by HbE. Pediatr Hematol Oncol. 2000;22:558–563. doi: 10.1097/00043426-200011000-00023. [DOI] [PubMed] [Google Scholar]
- Loukopoulos D. Hemoglobinopathies in Greece: prevention programme over the last 35 years. Indian J Med Res. 2011;134(5):72–76. [PMC free article] [PubMed] [Google Scholar]
- Madan N, Sharma S, Sood SK, Colah R, Bhatia HM. Frequency of β-thalassemia trait and other hemoglobinopathies in northern and western India. Indian J Hum Genet. 2010;16(1):16–25. doi: 10.4103/0971-6866.64941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta BC, Dave VB, Joshi SR, Baxi AJ, Bhatia HM, Patel JC. Study of hematological & genetical characteristics of Cutchi Bhanushali community. Indian J Med Res. 1972;60:305–311. [PubMed] [Google Scholar]
- Mulchandani DV, Fulare MB, Zodpey SP, Vasudeo ND. Prevalence and some epidemiological factors of beta thalassemia trait in Sindhi community of Nagpur city, India. Indian J Public Health. 2008;52:11–15. [PubMed] [Google Scholar]
- Munshi A, Anandraj MP, Joseph J, Shafi G, Anila AN, Jyothy A. Inherited hemoglobin disorders in Andhra Pradesh. India: a population study. Clin Chim Acta. 2009;400:117–119. doi: 10.1016/j.cca.2008.10.025. [DOI] [PubMed] [Google Scholar]
- Panigrahi I, Agarwal S, Gupta T, Singhal P, Pradhan M. Hemoglobin E—beta thalassemia: factors affecting phenotype. Indian Pediatr. 2005;42:357–362. [PubMed] [Google Scholar]
- Patel A, Naik P, Shah M, Sharma N, Narmadeshwar P, Parmar P. Prevalence of common hemoglobinopathies in Gujarat: an analysis of a large population screening programme. Nat J Commun Med. 2012;3:112–116. [Google Scholar]
- Patne SC, Shukla J. Hemgolobin E disorders in Eastern Uttar Pradesh. Indian J Pathol Microbiol. 2009;52:110–112. doi: 10.4103/0377-4929.44991. [DOI] [PubMed] [Google Scholar]
- Piplani S. Hemoglobin E disorders in North East India. J Assoc Physicians India. 2000;48:1082–1084. [PubMed] [Google Scholar]
- Rao VR, Gorakshakar AC. Sickle cell hemoglobin, β-thalassemia and G6PD deficiency in tribes of Maharashtra, India. Gene Geogr. 1990;4:131–134. [PubMed] [Google Scholar]
- Singh MR, Singh TS. Genetic polymorphism at three loci in two populations of Manipur, India. Anthropol Anz. 2008;66:191–198. [PubMed] [Google Scholar]
- Sukumaran PK. Abnormal hemoglobins in India. In: Sen NN, Basu AK, editors. Trends in hematology. Calcutta: Saraswati Press; 1975. pp. 225–236. [Google Scholar]
- Weatherall DJ. The challenge of hemoglobinopathies in resource poor countries. Br J Haematol. 2011;154:736–744. doi: 10.1111/j.1365-2141.2011.08742.x. [DOI] [PubMed] [Google Scholar]
- Wild BJ, Bain BJ. Investigation of abnormal hemoglobin and thalassemia. In: Lewis SM, Bain BJ, Bates I, editors. Practical hematology. 9. London: Churchill Living Stone; 2001. pp. 231–268. [Google Scholar]