Abstract
Advances in genetics have meant that the genetic services are now accessed by increasing numbers of patients. One way of dealing with the pressure on services without jeopardising patient care is the inclusion of nonmedical genetic counsellors and genetic nurses in the genetic services team. However, a cohesive approach to the profession has been lacking in Europe, and an educational programme and registration system for European practitioners is required. The aim of this study was to ascertain the type of work undertaken by genetic nurses and counsellors in Europe and the context in which they practised. We used a cross-sectional survey design to collect data from 213 practitioners, either genetic nurses or genetic counsellors, from 18 European countries. Respondents completed the survey online, and data were analysed using descriptive statistics and cross-tabulations. The majority were involved in undertaking the initial contact with the patient (89.9 %) and explaining the genetic test to the patient (91.5 %), while 74 % ordered tests and 91.4 % obtained informed consent for such tests. Psychological support before and after genetic testing was provided by 80.2 % of respondents, and 82.1 % reported regularly managing cases autonomously. While the genetic counselling profession is barely established in some countries, counsellors are able to contribute substantially to patient care as part of the multi-disciplinary team. Further efforts to establish the profession at the European level through a registration process will enhance the confidence in this new group of allied health professionals.
Keywords: Genetic counsellor, Professional practice, Genetic nurse
Introduction
Medical genetic services have offered care to patients at risk of or affected by genetic condition for decades in Europe (Harper 2007). However, the speed of technological innovation and concurrent advances in scientific knowledge regarding the cause of genetic disease has enabled genetic testing to be available to a wider group of patients. In consequence, there has been an increase in demand on genetic services in Europe (Cassiman 2010; Gregory et al. 2007; Modell et al. 2007; Peshkin et al. 2008), resulting in a need to consider the ways in which this demand can be addressed.
In a recent review of service models for provision of genetic healthcare, Battista et al. (2012) highlighted the effective use of multidisciplinary clinics and services to ensure that patients and families have access to co-ordinated care; however, the authors acknowledge that one of the challenges in doing this is the need to re-organise professional roles. One area for development of multidisciplinary genetic services lies in the utilisation of clinical personnel who are not medically trained but have other relevant clinical skills and expertise. It has been suggested that genetic counsellors or genetic nurses can have a role in delivering genetic counselling services in many health settings, particularly where diagnostic skills are not required because the condition in the family has been identified (Skirton et al. 1997). These include services for families with metabolic disease (O'Shea et al. 2011), cardiac disease (Oliva et al. 2011; Ingles and Semsarian 2007), neurological conditions (Quaid 2011), hereditary cancer (Torrance et al. 2006) and in prenatal counselling (Gagnon et al. 2009). However, the number of genetic counsellors in Europe is relatively small (Cordier et al. 2012) when compared to other health professions and is likely to remain so. Development in each country may therefore be hindered due to the difficulties of establishing a supportive professional infrastructure and educational programme for low numbers of practitioners. For this reason, Sahhar et al. (2005) emphasised the need for international collaboration in the field to share experience and good practice. In this context, development of the profession on a European scale is a practical proposition.
In a recent survey (Cordier et al. 2012) of key informants in 18 European countries, it was stated that in 14 of those countries, genetic nurses and genetic counsellors were working as part of multidisciplinary specialist genetic teams. The professional title of a nonmedical genetic health professional may apply to either genetic nurse or genetic counsellor. In most cases, genetic nurses and genetic counsellors work similarly, but their educational route differs. In some countries, nurses who have been trained in the specialty work alongside medical colleagues. However, more frequently, nonmedical genetic counsellors in this role have one of a wide range of academic backgrounds (e.g. biology, genetics, nursing and psychology) and been further educated via a Masters degree in genetic counselling. In the study by Cordier et al. (2012), genetic counsellors were working in 11 of the countries surveyed, while genetic nurses were working in 8. However, the overall numbers differed greatly, with approximately 122 genetic nurses compared with 500 genetic counsellors in Europe overall. Factors that influenced the development of the role in each country were cited as the degree of support for introduction of such posts by medical colleagues and the need to address the pressure on clinical services. While that survey provided a profile of the profession in Europe, specific data on the work of individual genetic nurses and counsellors were not available, and these were needed to inform a proposed educational programme and registration system for European practitioners. The aim of this study was to ascertain the type of work undertaken by genetic nurses and counsellors in Europe and the context in which they practised.
Materials and methods
Study design
To determine the current practice of genetic counsellors and genetic nurses in European countries, we used a cross-sectional survey design. Ethical approval for the study was obtained from the Plymouth University Ethics Committee.
Sample and recruitment
We aimed to recruit genetic counsellors or genetic nurses working in any European country. It was estimated through a previous study (Cordier et al. 2012) that there were approximately 600 practitioners working in Europe at the time of the study, of which 256 were members of the European Network of Genetic Nurses and Counsellors [http://www.engnc.org/]. This network was set up to expedite communication between practitioners in Europe, and there is no fee to join. We approached all members of the ENGNC via an email that included the Participant Information Sheet for the study and a letter of invitation that included the link to the online survey. All members of the network were asked to forward the information to colleagues who may not have been members, and all received two further reminder emails. We also sent the letter of invitation and Participant Information Sheet by email to the leaders of the five relevant professional organisations in Europe: the Norwegian National Association of Genetic Counsellors, French Association of Genetic Counsellors, Association of Genetic Nurses and Counsellors (UK), Swedish Association of Genetic Counsellors (Svenska föreningen för genetiska vägledare) and the Dutch Society of Genetic Counsellors (Nederlandse Vereniging Genetisch Consulenten). They were asked to circulate the information to their members and all did so.
Data collection
We were unable to find a validated survey tool to suit the purpose, so the survey was constructed by five of the authors. We first identified topics of interest and formulated questions, using an iterative process to refine the wording. The survey questions were uploaded to an online survey tool, Survey MonkeyTM , which we had previously used successfully for a similar study. It was important to use accessible means to ensure that we maximised responses; we therefore decided to use an online method of collecting data. We then asked three colleagues to complete the survey and report back on any areas of difficulty or unclear terminology. All potential participants were sent a link to the survey by email, so that they could then complete the survey in their own time. Information about the study was provided on the first page of the survey, and participants were asked to give their consent to have their data included in the study. They could not proceed to the actual questions unless they confirmed that they gave their consent.
Data analysis
The data were analysed using descriptive statistics and Chi-squared tests.
Results
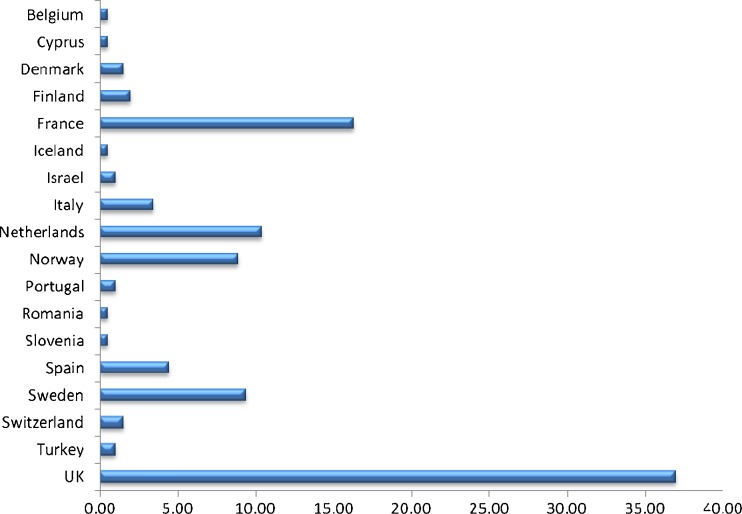
The participants’ demographics are presented in Table 1, along with their professional qualifications and the number of years they had spent in their roles as either genetic nurses or genetic counsellors. A total of 216 practitioners responded to the online survey, although 3 were from outside Europe, so the total number of relevant responses was 213, which we estimate to be approximately a third of those who work in Europe at the present time. The majority of respondents were female (92.5 %), and almost 20 % were within the 26–30 years age category. All but one of the male respondents were aged 40 or less, while two thirds of the male respondents were between 26 and 35 years of age. Whilst 82.9 % of respondents identified themselves as genetic counsellors, only 75.0 % used this as their professional title. The most widely held professional qualification was the Masters degree in genetic counselling (61.8 %). Although 16.6 % had been working as either genetic nurses or genetic counsellors for less than a year, 24.1 % of respondents had been doing so for between 5 and 10 years. Respondents were from 18 countries (see Fig. 1), with the majority working in the United Kingdom (UK) (37 %) or France (16.3 %).
Table 1.
Participant demographics
| Demographic | n | % | |
|---|---|---|---|
| Occupation, n = 202 | Genetic nurse | 20 | 10.1 |
| Genetic counsellor | 165 | 82.9 | |
| Other (e.g., psychologist) | 14 | 7.0 | |
| Gender, n = 204 | Male | 15 | 7.5 |
| Female | 186 | 92.5 | |
| Age, n = 204 | 21–25 | 14 | 7.0 |
| 26–30 | 40 | 19.9 | |
| 31–35 | 36 | 17.9 | |
| 36–40 | 16 | 8.0 | |
| 41–45 | 23 | 11.4 | |
| 46–50 | 23 | 11.4 | |
| 51–55 | 25 | 12.4 | |
| 56–60 | 21 | 10.4 | |
| 61–65 | 3 | 1.5 | |
| Over 65 | 0 | 0 | |
| Professional qualifications, n = 202 | Nursing diploma | 24 | 12.1 |
| Nursing degree | 16 | 8.0 | |
| Specialist nursing qualification | 26 | 13.1 | |
| Masters degree in nursing | 10 | 5.0 | |
| Masters degree in genetic nursing | 2 | 1.0 | |
| Masters degree in genetic counselling | 123 | 61.8 | |
| Other Masters degree | 37 | 18.6 | |
| Professional doctorate | 2 | 1.0 | |
| PhD | 30 | 15.1 | |
| Clinical psychologist degree | 4 | 2.0 | |
| Social worker degree | 2 | 1.0 | |
| Other | 47 | 23.6 | |
| Years working as a genetic nurse or genetic counsellor, n = 202 | Less than 1 year | 33 | 16.6 |
| Between 1 and 3 years | 37 | 18.6 | |
| Between 3 and 5 years | 33 | 16.6 | |
| Between 5 and 10 years | 48 | 24.1 | |
| Between 10 and 15 years | 22 | 11.1 | |
| Between 15 and 20 years | 15 | 7.5 | |
| Between 20 and 25 years | 10 | 5.0 | |
| Over 25 years | 1 | 0.5 |
Fig. 1.
Percentage of participants by country in which they were working
The profession in European countries
Of the total participants, 31.5 % stated that there was no law governing the work of genetic counsellors in their country; however, 25.9 % did recognise that there was a law that generally governed the work of health professionals, which included genetic counsellors. Over 17 % of respondents were unaware of any law governing practice as genetic counsellors in their country.
The majority of respondents were aware that an association or society specifically for genetic nurses and/or genetic counsellors existed in their country (85.4 %), with 69.4 % being a member of a general genetic organisation. Although a set programme for education was in place for the genetic counsellors (76.1 %), only 12.1 % of respondents knew of available programmes for genetic nurses in their countries.
With regard to a national registration or accreditation system being in place for genetic counsellors, 49.5 % said this was the case in their country; however, 39.3 % of respondents had no such registration system. A further 9.2 % were unsure, but had no knowledge of a national registration system.
Practice setting
The vast majority of respondents worked in a hospital setting (89.1 %), with 84.5 % working within a genetics department, 15.5 % within an oncology department and 8 % within an obstetrics/gynaecology department. Of the respondents, 41.2 % stated that it was a legal requirement in their country to be employed by, or to work with a medical colleague, while 32.4 % always did so, irrespective of a legal obligation. Many of the remaining respondents were unsure about the legal obligation in this regard. However, there were mixed responses when the data were analysed according to country. Although all counsellors from France knew of the legal requirement to work with a medical colleague, some respondents from other countries, including UK, Spain, Norway, Sweden and Italy, replied that it was not a legal requirement, while others from the same countries stated it was.
Role as a genetic nurse or genetic counsellor
Respondents were asked about their roles as genetic nurses and/or genetic counsellors, with regard to genetic testing. These findings are presented in Table 2. The genetic nurse or genetic counsellor alone would usually undertake the initial contact with the patient (55.3 %); however, they or the medical geneticist (depending on the case) would usually explain the genetic test to the patient (53.7 %), order a genetic test (42.6 %) and obtain informed consent for a genetic test (49.2 %). Discussing test results with the patient was usually done by whoever saw the patient before testing (49.5 %). With regard to drawing a family tree, 39.9 % stated that they alone performed this task, with only 14.9 % doing so with a doctor present. However, for many this depended on the case itself (31.4 %). The post-consultation letter to the patient was frequently written by the genetic nurse or genetic counsellor (20.7 %), although in the majority of cases, it was done by whoever saw the patient in the clinic (52.7 %). Psychological support before and after genetic testing was provided to patients by the genetic nurse or genetic counsellor alone in 39 % of cases, although again, it was frequently done by the person who saw the patient in the clinic (34.2 %), or by the genetic nurses/counsellors in conjunction with a medical colleague (7.0 %), totalling 80.2 % of practitioners who were providing psychological support associated with genetic testing.
Table 2.
Roles undertaken by genetic nurse or genetic counsellor
| Questions | You (genetic nurse or genetic counsellor) | A medical geneticist | Both medical geneticist and genetic nurse/genetic counsellor together | Either, but depends on the case | Other | ||||||
| Total n= | n | % | n | % | n | % | n | % | n | % | |
| Who USUALLY undertakes the first contact with the patient (for example to find out the patient’s background and give information about the genetic service)? | 188 | 104 | 55.3 | 4 | 2.1 | 5 | 2.7 | 60 | 31.9 | 15 | 8.0 |
| Who USUALLY explains the genetic test to the patient? | 188 | 58 | 30.9 | 11 | 5.9 | 13 | 6.9 | 101 | 53.7 | 5 | 2.7 |
| Who USUALLY orders a genetic test for the patient? | 188 | 40 | 21.3 | 46 | 24.5 | 19 | 10.1 | 80 | 42.6 | 3 | 1.6 |
| Who USUALLY obtains informed consent for a genetic test from the patient? | 185 | 61 | 33.0 | 15 | 8.1 | 17 | 9.2 | 91 | 49.2 | 1 | 0.5 |
| Question | You (genetic nurse or genetic counsellor) | A medical geneticist | Both medical geneticist and genetic nurse/genetic counsellor together | Whoever saw the patient before testing | Other | ||||||
| Who USUALLY discusses the genetic test result with the patient? | 184 | 33 | 17.9 | 32 | 17.4 | 22 | 12.0 | 91 | 49.5 | 6 | 3.3 |
When we compared data between respondents from countries where the genetic counsellor profession is well established (France, Netherlands, Norway, Sweden, UK) with those from countries where the profession is relatively new, we found no significant differences between the groups in terms of genetic counsellors making the first contact, explaining a genetic test and providing psychological support. Although there were practitioners from eight countries who responded they would order genetic tests, those from the five countries where the profession is well established were more likely to order genetic tests than those from the other countries represented (Israel, Spain and Turkey) (χ2 = 3.906, 1 df, p < .05).
Respondents from Cyprus, Denmark, France, Israel, Italy, Netherlands, Norway, Romania, Spain, Sweden and Switzerland reported managing cases alone, without the patient seeing a doctor; 67 % did so frequently, another 15.1 % did so sometimes, 9.2 % rarely and only 8.6 % never managed cases alone. Many of these cases involved risk assessment for familial cancer (76.4 %), risk assessment for autosomal recessive conditions with known diagnosis (68.5 %), risk assessment for autosomal dominant conditions with known diagnosis (68.5 %), presymptomatic testing for familial cancer (67.3 %) and carrier testing for autosomal recessive conditions (66.1 %). Respondents from countries where genetic counselling or genetic nursing was more recently established were much less likely to manage cases alone than those from the five countries with established systems (χ2 = 13.129, 1 df, p < .001).
Discussion
The results of this survey indicate that genetic counsellors and nurses in a number of European countries are working in an autonomous manner within multidisciplinary genetics teams. Within those teams, genetic counsellors and nurses are providing a range of patient care and managing caseloads. We were unable to find other recent literature on this topic, but the types of cases managed by genetic counsellors reported in this study are very similar to those reported by Skirton et al. (1997) in a UK study of genetic nurses and medical geneticists. In that study, it was the opinion of both medical and nonmedical staff that it was appropriate for cases involving recessive conditions, aneuploidy and neural tube defects. However, in that study, medical geneticists were more likely than genetic nurses to state that cancer genetic cases should be handled by those nurses; this may have been because cancer genetics was still a relatively new field. However, as in this survey, there was a consensus that cases requiring diagnostic skills should not be managed by genetic counsellors without medical input. Given the emphasis on psychological support and counselling skills in the core competences for genetic nurses and genetic counsellors (Skirton et al. 2010b), it was surprising that almost a fifth of practitioners did not report providing psychological support to patients before and after genetic testing. However, this may have been because we did not specify the nature of such support, and it may have been interpreted by some respondents as specialist support by a psychologist. In future studies, this needs to be better defined.
It is of relevance that the majority of respondents were working in countries with a national organisation for genetic counsellors. This could, of course, be an artefact of the way we recruited participants (one approach came via the national organisation); however, it is also consistent with the relative numbers of genetic counsellors working in each country (Cordier et al. 2012). Where numbers of genetic counsellors are increasing, they are more likely to form an association, which in turn may foster the growth of the profession. For example, since the survey was conducted, a new association has been formed in Spain (IDEC 2012) by graduates of the first Spanish Masters degree course in genetic counselling. However, in those countries where there are currently few practitioners, the lack of a supportive organisation could hamper the establishment of educational programmes and appropriate standards of practice. The lack of national professional organisations for genetic counsellors and nurses in many countries does therefore appear to indicate that at this moment a European approach is helpful.
In a study of genetic counsellors practising in one state in the USA, Mester et al. (2009) found that only 28 % of respondents were in favour of having genetic counsellors working under the supervision of medical practitioners. We did not ask the question as to whether respondents were in favour of this, but in fact the overwhelming majority were either obliged to work under medical supervision or did so regardless of legal obligation. There did appear to be some confusion about this amongst respondents as some stated there was a legal obligation to work with a medical colleague, while others from the same country indicated there was not. Despite this lack of clarity, in Europe therefore there seems to be an acceptance that genetic counsellors should work in multidisciplinary teams, rather than independently. The fact that in many cases genetic counsellors reported that tasks were undertaken by the person who had seen the patient, rather than allocated to one particular profession, seems to imply that there is flexibility within the team, with a focus on continuity of patient care. In the US study, 82 % of genetic counsellors believed they should be able to order a genetic test without direct medical input, whereas in our study, over 63.9 % of respondents were actually undertaking that role. The authors of the US study state that a system of licensure for genetic counsellors would be helpful in establishing genetic counselling as a genuine health profession and help to protect patient safety. At present, there are few European countries in which a scheme to assess fitness to practice operates, but such schemes have the potential to enhance the confidence and competence of genetic counsellors to perform these roles, as well as enhancing the confidence of colleagues and managers who have an influence on the degree of autonomous practice that is appropriate in the clinical setting.
While Sahhar et al. (2005) emphasised the need for communication and collaboration between genetic counsellors from different nations, they stated the intention to develop a set of core competences for those working in the Australian setting, despite the existence of core competences developed in the UK and the USA. This need to establish the norms for practice according to regional setting is important to ensure practice is relevant to the patient group and health service in which clinical care is offered. For this reason, practice standards (Skirton et al. 2010a) and European core competences have been devised (Skirton et al. 2010b) as the basis for further development of a registration system and Masters level curriculum for European genetic counsellors. The recently established European Board of Medical Genetics aims to ensure that the profession is recognised at European level and that practitioners in each European country have a comparable standard of education and a means of demonstrating competence, which will facilitate practice within countries as well as across borders within Europe.
Limitations
This survey was conducted in English, and though it would be expected that health professionals working in advanced practice such as genetic counselling would be able to use English in order to maintain their own professional knowledge, it may be that some practitioners lacked the language skills or confidence to complete the survey in that language.
We used a number of routes to ensure that all potential participants had an invitation to take part, but it may be that some who were not part of either the European network of their national association were not aware of the study. It may be, therefore, that those who participated were the most professionally active practitioners in Europe, and we may not have captured the practice of those who were less involved in professional organisations.
Conclusions
While there are certainly some European countries in which the genetic counselling profession is barely established, the findings of our study indicate that where counsellors are working, they are able to contribute substantially to patient care as part of the multidisciplinary team. Further efforts to establish the profession at the European level through a registration process will enhance the confidence in this new group of allied health professionals.
Acknowledgments
Conflict of interest
The authors declare no conflict of interest.
References
- Battista RN, Blancquaert I, Laberge AM, van Schendel N, Leduc N. Genetics in health care: an overview of current and emerging models. Public Health Genomics. 2012;15(1):34–45. doi: 10.1159/000328846. [DOI] [PubMed] [Google Scholar]
- Cassiman JJ. Quality genetic services for the population, now and in the future. Bull Mem Acad R Med Belg. 2010;165(10–12):475–482. [PubMed] [Google Scholar]
- Cordier C, Lambert D, Voelckel MA, Hosterey-Ugander U, Skirton H. A profile of the genetic counsellor and genetic nurse profession in Europe. J Comm Genet. 2012;3(1):19–24. doi: 10.1007/s12687-011-0073-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gagnon A, Wilson RD, Allen VM, Audibert F, Blight C, Brock J-A, Désilets VA, Johnson J-A, Langlois S, Murphy-Kaulbeck L, Wyatt P. Evaluation of prenatally diagnosed structural congenital anomalies. J Obstet Gynaecol Can. 2009;31(9):875. doi: 10.1016/S1701-2163(16)34307-9. [DOI] [PubMed] [Google Scholar]
- Gregory H, Wordsworth S, Gibbons B, Wilson B, Haites N. Risk estimation for familial breast cancer: improving the system of counselling. Eur J Hum Genet. 2007;15(11):1139–1144. doi: 10.1038/sj.ejhg.5201895. [DOI] [PubMed] [Google Scholar]
- Harper PS. A short history of medical genetics. Oxford: Oxford University Press; 2007. [Google Scholar]
- IDEC (2012) The Spanish Genetic Counselling Society is born. Available at: http://www.idec.upf.edu/en/seccions/idec/noticies.php?id=828. Accessed 22 Jun 2012
- Ingles J, Semsarian C. Sudden cardiac death in the young: a clinical genetic approach. Intern Med J. 2007;37(1):32–37. doi: 10.1111/j.1445-5994.2006.01241.x. [DOI] [PubMed] [Google Scholar]
- Mester JL, Trepanier AM, Harper CE, Rozek LS, Yashar BM, Uhlmann WR. Perceptions of licensure: a survey of Michigan genetic counselors. J Genet Couns. 2009;18(4):357–365. doi: 10.1007/s10897-009-9225-0. [DOI] [PubMed] [Google Scholar]
- Modell B, Darlison M, Birgens H, Cario H, Faustino P, Giordano PC, Gulbis B, Hopmeier P, Lena-Russo D, Romao L, Theodorsson E. Epidemiology of haemoglobin disorders in Europe: an overview. Scand J Clin Lab Investig. 2007;67(1):39–69. doi: 10.1080/00365510601046557. [DOI] [PubMed] [Google Scholar]
- Oliva A, Brugada R, D'Aloja E, Boschi I, Partemi S, Brugada J, Pascali VL. State of the art in forensic investigation of sudden cardiac death. Am J Forensic Med Pathol. 2011;32(1):1–16. doi: 10.1097/PAF.0b013e3181c2dc96. [DOI] [PubMed] [Google Scholar]
- O'Shea R, Murphy AM, Treacy E, Lynch SA, Thirlaway K, Lambert D. Communication of genetic information by other health professionals: the role of the genetic counsellor in specialist clinics. J Genet Couns. 2011;20(2):192–203. doi: 10.1007/s10897-010-9337-6. [DOI] [PubMed] [Google Scholar]
- Peshkin BN, Demarco TA, Graves KD, Brown K, Nusbaum RH, Moglia D, Forman A, Valdimarsdottir H, Schwartz MD. Telephone genetic counseling for high-risk women undergoing BRCA1 and BRCA2 testing: rationale and development of a randomized controlled trial. Genet Test. 2008;12(1):37–52. doi: 10.1089/gte.2006.0525. [DOI] [PubMed] [Google Scholar]
- Quaid KA. Genetic counseling for frontotemporal dementias. J Mol Neurosci. 2011;45(3):706–709. doi: 10.1007/s12031-011-9557-8. [DOI] [PubMed] [Google Scholar]
- Sahhar MA, Young MA, Sheffield LJ, Aitken M. Educating genetic counselors in Australia: developing an international perspective. J Genet Couns. 2005;14(4):283–294. doi: 10.1007/s10897-005-0572-1. [DOI] [PubMed] [Google Scholar]
- Skirton H, Barnes C, Curtis G, Walford-Moore J. The role and practice of the genetic nurse. J Med Genet. 1997;34(2):141–147. doi: 10.1136/jmg.34.2.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skirton H, Voelckel MA, Patch C. Using a community of practice to develop standards of practice and education for genetic counsellors in Europe. J Comm Genet. 2010;1:169–173. doi: 10.1007/s12687-010-0024-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skirton H, Lewis C, Kent A, Coviello D. Genetic education and the challenge of genomic medicine: development of core competences to support preparation of health professionals in Europe. Eur J Hum Genet. 2010;18(9):972–977. doi: 10.1038/ejhg.2010.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torrance N, Mollison J, Wordsworth S, Gray J, Miedzybrodzka Z, Haites N, Grant A, Campbell M, Watson MS, Clarke A, Wilson B. Genetic nurse counsellors can be an acceptable and cost-effective alternative to clinical geneticists for breast cancer risk genetic counselling. Evidence from two parallel randomised controlled equivalence trials. Br J Cancer. 2006;95(4):435–444. doi: 10.1038/sj.bjc.6603248. [DOI] [PMC free article] [PubMed] [Google Scholar]