Abstract
The sickle cell gene in India reaches its highest prevalence among the tribal people, many of whom are marginalized in the Indian society, living in remote rural areas which are often in the hilly regions of the Deccan plateau. Delivery of all services including health care presents special challenges which are addressed in this study by an outreach program and a mobile clinical unit. Another concern among the tribal people, a suspicion of centrally provided services conceived as being imposed from the outside, has been addressed by the concept of the Sickle Cell Swa (self) Suraksha (protection) Abhiyan (movement), which seeks to educate tribal communities in sickle cell (SS) disease so that the request for screening emanates from the community itself. This program has now screened 7,307 subjects in nine villages, finding the sickle cell trait in 23.7 % (range 18.5–30.9 %) and probable SS disease in 112 subjects. The organization of the program is described along with the delivery of results on a laminated card displaying the hemoglobin genotype, advice related to the genotype, blood group information (specifically requested by the villagers), contacts within the village sickle cell committee, and clinical contacts for medical advice. In addition, a local villager has been given basic health care training to regularly visit and monitor cases of SS disease and refer those with significant complications to the hospital coordinating the screening program. It is too early to determine the success of this program, but it represents a village-based model of detection of the sickle cell gene and care for cases with the disease which is accepted by the affected communities and may have broader implications for sickle cell disease in India.
Keywords: Sickle cell disease, India, Tribal populations, Screening for HbS
Introduction
The sickle cell gene is widespread in India, affecting predominantly the tribal peoples of central India (states of Gujarat, Maharastra, Madhya Pradesh, Chhattisgarh, and Orissa) with another focus of the gene in southern India in the north of Tamil Nadu and Kerala. The tribal peoples in these areas are often relatively backward, living in rural areas with limited facilities, and generally marginalized from much of Indian society. Detection of the sickle cell trait and sickle cell disease among these peoples therefore poses particular challenges. There have been many programs designed to advance the tribal peoples in the Indian society, and sickle cell disease has emerged as one of the important public health problems affecting these groups. Several states have initiated sickle cell control programs, Gujarat leading the way in early 2006, Chhattisgarh in 2008, and Maharastra in 2011. These screening programs usually have two objectives: firstly, screening of the susceptible populations, seeking to identify carriers in order to conduct education and counseling to reduce affected births; and secondly, identifying patients with the disease in order to improve clinical management. However, there may be a perception that programs imposed on communities from the outside may be less successful than educating communities wherein they recognize the importance of detecting the carrier state and specifically request such screening for the benefit of their villages. This is a concept advanced by the Vision Medical Foundation for Rural Health & Research in Bardoli, Gujarat State under their Sickle Cell Swa (self) Suraksha (protection) Abhiyan (movement). As other states in India develop their sickle cell control programs, this model of population screening may be of interest, and some preliminary experience is therefore presented.
Material and methods
Initiation of village interest
Initially, there were meetings with village leaders to discuss the provision of screening and to determine the project design according to the wishes of the village communities. Target villages are encouraged to appoint a village sickle cell committee which usually comprises the elected leader (sarpanch), school principal, spiritual leaders, social leaders, political leader from all parties, and educated volunteers. The village leaders then sensitize and motivate the village people.
Village census
The village committee is responsible for providing a streetwise village census, recording the name, age, gender, family structure, employment, income, and any history of sickle cell disease in the family.
Sickle cell camp
In the Indian tradition, screening is conducted in a single session or “camp.” The village sickle cell committee is responsible for sending written invitations to the villagers to attend the camp which takes place on a predesignated day. The format usually includes a formal welcome, opening prayers, entertainment in the form of dances or songs performed by the children, and speeches on the importance and genetics of sickle cell disease followed by blood sampling. Clerical stations are set up to register patients, allocating unique ID numbers and supplying a blood tube; after which, the villagers move to bleeding stations each staffed by a team of two nurses experienced in venipunctures. Using 2-ml syringes and gauge 22 needles, 2 ml of venous blood is drawn from the antecubital vein into tubes prepared with EDTA, marked with the person's name and ID number, and kept in cool storage pending return to the laboratory. Sampling proceeds at the rate of 60 samples per team per hour, allowing the collection of up to 960 samples in a 4-h period. Transportation and lunch are the responsibility of the village committee, and at the end of the day, the samples are returned to the laboratory for analysis.
Laboratory analysis
The samples are initially screened using a solubility test with reagents produced in our laboratory, and all positive results and a random 5 % sample of negative results were confirmed by hemoglobin electrophoresis on cellulose acetate. Samples suspected to be positive for sickle cell (SS) disease are submitted to a full blood count (Sysmex KX21 analyzer). Blood groups are also determined on all samples (anti-A, anti-B, anti-A,B, monoclonal blood grouping antibodies for slide and tube tests) since this information was requested by the villagers in case of a need for transfusion in which the village may provide an informal “blood bank.”
Statistical analysis
The expected genotype frequencies were derived by applying the Hardy–Weinberg equilibrium test and compared with the observed frequencies using a likelihood ratio chi-squared statistic.
Dissemination of data
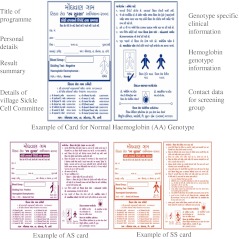
Specially printed cards are produced and laminated for each village since they bear village-specific names and phone numbers of members of the sickle cell committee. These members are given special information and instructions, equipped with additional educational materials, and are able to contact doctors in the event of special problems or the need for additional information. The layout of the cards is similar for the different genotypes but color-coded blue for normal hemoglobin (AA) genotype, purple for sickle cell trait (AS), and red for SS disease with explanations in Gujarati (Fig. 1). After data insertion, the cards for each nuclear family are placed in a family envelope for distribution at a special gram sabha (village meeting) to which all families are invited. This meeting usually has a cultural program arranged by the village, with illustrated video presentations by doctors and sometimes with a “marriage quiz” to be answered by the villagers.
Fig. 1.
Examples of genotype cards
Sickle cell health care worker
The village committee is asked to identify a suitable person for training as a sickle cell health care worker who receives special training on monitoring sickle cell patients. Receiving a part-time salary, they are given a kit containing an electronic thermometer, sphygmomanometer, pulse oximeter, and a calibrated ruler for measuring the spleen size and are requested to visit the SS patients every 3 months, recording their observations.
Results
The program has currently sampled a population of 7,307 among nine villages (Table 1). The proportion of villagers sampled has averaged 54 % (range 12.6–92.1 %) and exceeded 75 % in five of the nine villages.
Table 1.
Survey results from nine villages
| Village | Total population | Sampled | Solubility test | Electrophoresis | Blood group data | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | negative | positive | AS (%) | SS | O+ | O− | A+ | A− | B+ | B− | AB+ | AB− | Total | ||
| 1. Moghvan | 2,376 | 2,018 | 84.9 | 1,541 | 477 | 456 (22.6) | 21 | 741 | 9 | 668 | 10 | 455 | 8 | 126 | 1 | 2,018 |
| 2. Kalaghat and Ghodi ruvali | 1,045 | 533 | 51.0 | 413 | 120 | 114 (21.4) | 6 | 159 | 3 | 154 | 6 | 154 | 1 | 55 | 1 | 533 |
| 3. Maiyali Mota satsila | 796 | 733 | 92.1 | 556 | 177 | 163 (22.2) | 14 | 270 | 2 | 236 | 4 | 158 | 2 | 61 | 0 | 733 |
| 4. Ghodchit | 1,245 | 966 | 77.6 | 651 | 315 | 298 (30.9) | 17 | 321 | 3 | 313 | 3 | 221 | 1 | 98 | 6 | 966 |
| 5. Dumda | 1,125 | 928 | 82.5 | 689 | 239 | 222 (23.9) | 17 | 280 | 2 | 298 | 2 | 267 | 4 | 73 | 2 | 928 |
| 6. Ghuntvel | 815 | 377 | 46.3 | 269 | 108 | 97 (25.8) | 11 | 145 | 3 | 125 | 2 | 80 | 0 | 22 | 0 | 377 |
| 7. Gunkhadi | 1,200 | 601 | 50.1 | 465 | 136 | 128 (21.3) | 8 | 189 | 3 | 197 | 3 | 154 | 2 | 51 | 2 | 601 |
| 8. Uchhal | 4,108 | 518 | 12.6 | 417 | 101 | 96 (18.5) | 5 | 162 | 2 | 148 | 1 | 145 | 0 | 56 | 1 | 515a |
| 9. Borkuva | 833 | 633 | 76.0 | 454 | 179 | 166 (18.6) | 13 | 193 | 2 | 184 | 2 | 199 | 0 | 53 | 0 | 633 |
| Totals | 13,543 | 7,307 | 54.0 | 5,452 | 1,852 | 1,740 (23.7) | 112 | 2,460 | 29 | 2,323 | 33 | 1,833 | 18 | 595 | 13 | 7,304 |
aIn three samples, blood groups could not be determined
Abnormal hemoglobins
The solubility tests were positive in 1,852 subjects of whom 1,740 (23.7 %) were found to have the sickle cell trait, and 112 had an electrophoretic pattern consistent with SS disease. Comparison of the observed and expected genotype frequencies showed no deviation from those expected for villages 2, 3, and 5–9, but deficiencies of the observed cases of SS disease occurred in Moghvan (Obs/Exp = 21/31, p = 0.05) and in Ghodchit (Obs/Exp = 17/29, p = 0.01).
Blood groups
Of the ABO blood group system, group O accounted for 34 %, group A for 32 %, group B for 25 %, and group AB for 8 %.
Discussion
Sickle cell disease is recognized to be a major health problem among the tribal people living on the Deccan plateau. Substantial funding has been made available for the development of sickle cell services in these populations by both the Indian Council of Medical Research and the National Rural Health Commission. The state governments have also recognized the need for improving sickle cell services, and sickle cell control programs have been initiated in Gujarat in 2006, Chhattisgarh in 2008, and Maharastra in 2011. These programs are directed towards population screening and have used different logistical approaches towards detecting sickle cell disease, educating populations on the significance of the sickle cell trait, and avoiding births with sickle cell disease. One such program in Chhattisgarh used the solubility test for preliminary screening in the village, followed by venipunctures of subjects with positive tests which were then studied further by hemoglobin electrophoresis in the central laboratory. This project targeted children aged 3–15 years and analyzed 359,823 subjects in 2 years and 9 months (Patra et al. 2011), finding a sickle cell trait rate of 9.3 % and 747 subjects with an electrophoretic pattern compatible with SS disease. In the present study in Gujarat, a higher trait frequency occurred, consistent with previous observations (Vyas et al. 1962), and 112 cases consistent with SS disease were detected. Comparison of the observed and expected frequencies of the SS genotype found a close agreement in seven of the nine villages, the two other villages showing deficiencies of borderline or greater significance. A similar deficiency was noted in a study in Chhattisgarh, the most likely explanation being a failure of SS patients to enter the sampled population either from early death or absence from school.
The two approaches illustrated in Chhattisgarh and Gujarat allow comparison of different models of care: the first which is generously funded by the state government and the second which utilizes a different philosophy whereby the request for screening came from the village sickle cell committee. It was believed that in the latter model, there will be greater interest and respect for the findings than in government-funded programs which may appear to be imposed from the outside, but this remains to be shown by follow-up of the populations in the two models. Both generate personal laminated genotype cards, and both attempt to provide clinical care for detected SS patients; once again, the models are fertile areas for social research to determine the effectiveness of the sickle cell worker employed in the Gujarat model.
The objectives of the screening program were twofold: the detection of persons with SS disease who could then be offered clinical care and the detection of the carrier state followed by counseling on the significance of the sickle cell trait and, depending on their choice of partner, the potential risks of having a child with sickle cell disease. Such counseling must clearly be nondirective, explaining not only the lack of symptoms in persons with the sickle cell trait, but also the genetics of sickle cell disease. The counseled individuals are then empowered to make informed decisions. We realize that this approach may be deemed as eugenic by some observers, but most workers in the detection of sickle cell disease are convinced that individuals with the sickle cell trait should be given this information, allowing informed choices and prevention of disease where possible. Such genetic knowledge has influenced decisions on arranged marriages in Bahrain (Al Arrayed 2005) and in Saudi Arabia (Memish and Saeed 2011), and the ethical and other implications of compulsory premarital testing in these societies have been discussed (Alswaidi and O'Brien 2009; Alswaidi et al. 2012). In the current Gujarat program, it is believed that the voluntary participation and the nondirective nature of counseling avoid some negative aspects associated with an approach which may be considered by some as eugenic.
The choice of diagnostic method in screening programs for hemoglobinopathies is influenced by many factors including the financial resources available and the genetic complexity of the population to be screened. Sickle hemoglobin is relatively simple to detect by a cheap initial screening test before resorting to the more expensive options of hemoglobin electrophoresis on cellulose acetate or by high-pressure liquid chromatography. With the large numbers of subjects and limited resources of the Indian environment, initial screening was performed using the solubility test, performed prior to selected venipuncture in the Chhattisgarh program but after routine venipuncture in Gujarat, the difference in Gujarat being the village request for blood group information. Abnormal hemoglobins such as HbC in populations of West African origin or Punjab in northwest India interact with HbS to form clinically significant sickle cell disease, and these will be missed in screening with the solubility or slide sickle test. Although HbC is unlikely to occur in India except in persons of West African origin, HbD Punjab occurs in up to 2 % of the subjects in northwest India and would be a potential confounder in Gujarat. Furthermore, these screening programs are also limited by their ability to detect the beta thalassemia trait. In India, the most common beta thalassemia gene is the IVS1-5 G → C mutation which is relatively severe, and in combination with HbS, it produces a form of sickle cell beta+ thalassemia characterized by 3–5 % of HbA and a severe clinical course. The prevalence of these genes is unknown among the Gujarat tribal population, but in Chhattisgarh, studies in adjacent tribal areas suggest a trait frequency of 6–7 % (Balgir 2005) or almost as high as the HbS trait frequency. Since without specific diagnostic tests, this beta thalassemia trait will resemble an AA phenotype on hemoglobin electrophoresis, relationships between a subject with the sickle cell trait and an apparent AA phenotype may still result in a child with clinically significant sickle cell disease. More information is therefore required on the prevalence of beta thalassemia genes among the tribal peoples and for simple diagnostic tests capable of their detection. Until more information is available, screening for the purposes of genetic counseling requires the most accurate methods including hematological indices, hemoglobin electrophoresis, quantification of HbA2, and occasional identification of the beta thalassemia mutation by DNA structural analyses.
The addition of blood group data in the Gujarat model may be criticized for the additional expenditure and the fact that blood groups would always have to be repeated at the time of cross-matching, but the blood group determination was a specific request of the villagers who felt that this knowledge would allow the village to maintain a “bank” of similarly matched donors in the event of emergencies.
References
- Al Arrayed S. Campaign to control genetic blood diseases in Bahrain. Community Genet. 2005;8:52–55. doi: 10.1159/000083340. [DOI] [PubMed] [Google Scholar]
- Alswaidi FM, O'Brien SJ. Premarital screening programmes for haemoglobinopathies, HIV and hepatitis viruses: review and factors affecting their success. J Med Screen. 2009;16:22–28. doi: 10.1258/jms.2008.008029. [DOI] [PubMed] [Google Scholar]
- Alswaidi FM, Memish ZA, O'Brien SJ, Al-Hamdan NA, Al-Enzy FM, Alhayani OA, Al-Wadey AM. At-risk marriages after compulsory premarital testing and counseling for β-thalassemia and sickle cell disease in Saudi Arabia, 2005–2006. J Genet Counsel. 2012;21:243–255. doi: 10.1007/s10897-011-9395-4. [DOI] [PubMed] [Google Scholar]
- Balgir RS. The spectrum of haemoglobin variants in two scheduled tribes of Sundergarh district in north-western Orissa, India. Ann Hum Biol. 2005;32:560–573. doi: 10.1080/03014460500228741. [DOI] [PubMed] [Google Scholar]
- Patra PK, Chauhan VS, Khodiar PK, Dalla AR, Serjeant GR. Screening for the sickle cell gene in Chhattisgarh state, India: an approach to a major public health problem. J Community Genet. 2011;2:147–151. doi: 10.1007/s12687-011-0050-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vyas GN, Bhatia HM, Sukumaran PK, Balakrishnan V, Sanghni LD. Study of blood groups, abnormal haemoglobins and other genetical characters in some tribes of Gujarath. Am J Phys Anthrop. 1962;20:255–265. doi: 10.1002/ajpa.1330200310. [DOI] [PubMed] [Google Scholar]