Abstract
Post-traumatic pseudoaneurysms are rare in the peripheral arteries and usually occur as a late sequel of trauma. Surgery has traditionally been considered as the gold standard of therapy for traumatic peripheral pseudoaneurysms. We report 2 cases of post traumatic pseudoaneurysms successfully treated by percutaneous cyanoacrylate glue (N-Butyl 2 cyanoacrylate) embolization. This method offers complete exclusion of the pseudoaneurysm, at the same time avoiding the morbidity of open surgery.
Keywords: Pseudoaneurysm, Cyanoacrylate glue, Embolization
Introduction
Surgery has long been considered as gold standard for the treatment of peripheral pseudoaneurysms [1]. However, nonsurgical alternatives such as ultrasound-guided compression, coil embolization, stent placement, and percutaneous thrombin injection are being increasingly used to treat peripheral pseudoaneurysms. Cyanoacrylate glue (N-butyl cyanoacrylate) has been widely used in neurovascular interventions and in endovascular treatment of pseudoaneurysms [2–6]. We report two cases of peripheral pseudoaneurysms treated by percutaneous embolization with cyanoacrylate glue.
Case 1
A 35-year-old lady presented with a swelling over the right shoulder for the last 3 months. She had sustained a midshaft humerus fracture 3 months ago for which she had undergone an open reduction and internal fixation with an intramedullary nail.
On examination, she was found to have a firm 5 × 5 cm swelling over the right shoulder. The swelling was pulsatile. A pseudoaneurysm of the axillary artery was suspected and a digital subtraction angiogram obtained. This revealed a pseudoaneurysm arising from the circumflex humoral branch of the axillary artery.
Selective cannulation of the feeder vessel was unsuccessful. The pseudoaneurysm was percutaneously punctured under US guidance with a 20 G Chiba needle and an angiogram was obtained (Fig. 1a). The feeder artery origin was occluded by a 7 mm × 2.5 cm balloon. Check injection of contrast into the pseudoaneurysm revealed stasis of contrast within the pseudoaneurysm, confirming occlusion of the feeder vessel (Fig. 1b). The pseudoaneurysm was embolized with 1 ml of 33% Histoacryl (B. Braun Melsungen AG, Germany) and Lipiodol (Guerbet, France). Postembolization, right subclavian angiogram revealed nonopacification of the pseudoaneurysm (Fig. 1c). Ultrasound screening revealed complete thrombosis of the pseudoaneurysm cavity.
Fig. 1.
a) DSA showing opacification of pseudoaneurysm with reflux into parent artery b) occlusion of the parent artery with a balloon c) post embolization check angiogram with complete exclusion of the pseudoaneurysm
Case 2
A 55-year-old man sustained a fracture neck of right femur following a fall. He underwent surgical fixation for the same, but developed implant infection. He underwent implant exit followed by a right cemented total hip replacement. Postoperatively, he was found to have a tender swelling over the right thigh, with bleeding from the wound. A femoral pseudoaneurysm was suspected and a duplex ultrasound obtained. This revealed a pseudoaneurysm arising from a muscular branch of the profunda femoris artery.
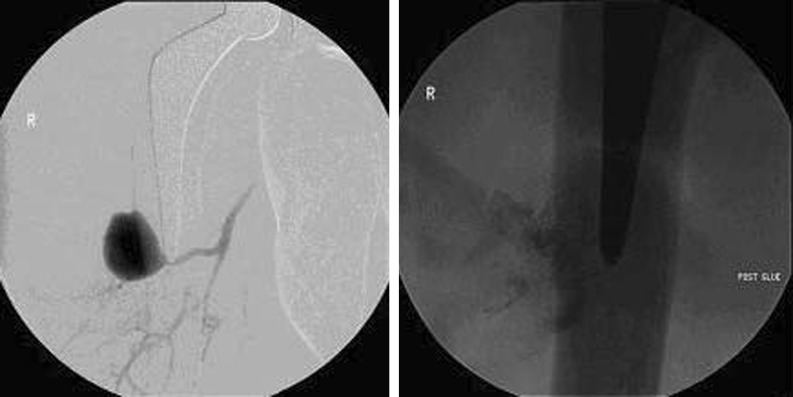
Percutaneous puncture of the pseudoaneurysm was done under ultrasound guidance. Check angiogram revealed a 3 × 2 cm pseudoaneurysm communicating with a branch arising from the profunda femoris artery (Fig. 2a). There was reflux of the contrast into adjacent muscular branches of the profunda femoris artery, but not into the parent vessel. The pseudoaneurysm was embolized with 1.5 ml of 40% Histoacryl (B. Braun Melsungen AG, Germany) and Lipiodol (Guerbet, France). Postprocedure check angiogram revealed complete occlusion of the pseudoaneurysm. Postembolization, ultrasound screening revealed complete thrombosis of the pseudoaneurysm cavity, and a plain radiograph revealed a glue cast within the pseudoaneurysm (Fig. 2b).
Fig. 2.
a) DSA through a percutaneous Chiba needle into the pseudoaneurysm with feeder artery from right profunda femoris artery b) Plain radiograph, post glue injection demonstrating a glue cast within the pseudoaneurysm
Discussion
A pseudoaneurysm forms when blood escapes from the lumen of an artery through a defect in one or more layers of the arterial wall and forms a localized pocket of flow in the surrounding tissues [7]. Penetrating trauma is the most common cause of noniatrogenic traumatic pseudoaneurysms [1]. If untreated, these can result in pain, swelling, compression of adjacent structures, rupture, and bleeding [8, 9].The diagnosis is often suspected clinically and confirmed by a color flow duplex ultrasound or a digital subtraction angiogram [1].
Small (<1 cm) asymptomatic pseudoaneurysms can be observed because many will thrombose spontaneously [10]. However, larger (>1 cm) and symptomatic pseudoaneurysms require treatment.
Treatment options include ultrasound-guided compression, covered stent placement, coil embolization, percutaneous embolization, and open surgical repair.
Ultrasound-guided compression is mainly used for treatment of iatrogenic pseudoaneurysms at the groin. Major drawbacks include high failure rates, operator fatigue, and patient intolerance [8, 9].
Covered stents bridge the rent in the vessel wall, and thus exclude the pseudoaneurysm from circulation. Currently their use is limited to pseudoaneurysms that have a difficult percutaneous access or when surgery is associated with major morbidity and mortality [11]. These are also not ideal for deployment across joints [1].
Coil embolization is used to treat pseudoaneurysms that are difficult to access percutaneously [1].
Direct percutaneous embolization with thrombin causes rapid obliteration of the pseudoaneurysm cavity and is highly effective [9], even in patients on anticoagulation or antiplatelet agents [12]. Drawbacks include the risk of anaphylactic reaction, distal embolization, and its nonavailability in many places.
Open surgical repair of pseudoaneurysms is usually reserved for patients with groin hematoma and skin necrosis, distal limb ischemia, infection, or abscess [1, 8].
In our cases, the use of covered stent was not considered due to the high cost of the stent and money constraints. Selective cannulation of the feeder artery was attempted for coil embolization, but was however not successful, and hence coiling could not be done. Although percutaneous ultrasound-guided thrombin injection can be used to treat these pseudoaneurysms, this was not used because of nonavailability of thrombin.
Cyanoacrylate glue (N-butyl 2 cyanoacrylate) is widely used as a visceral arterial embolic agent for endovascular treatment of vascular malformations of the brain as well as many other visceral pseudoaneurysms. There have been various reports of its use in splenic [2], pancreatic [3], common hepatic [4], renal [5], and celiac trunk [6] pseudoaneurysms.
Polymerization of monomers of cyanoacrylate and formation of a glue cast form the basis of use of this agent. This occurs instantaneously when the glue comes in contact with ions and free radicals present in the body fluids [5, 13].
It also has minimal tissue toxicity and induces very little inflammation [14]. Other advantages of cyanoacrylate glue include its radio-opaque nature, when mixed with an iodized oil such as Lipiodol, which helps in visualization with fluoroscopy [4] and its low viscosity, which helps in easy injection through a needle [13].
The main drawback of the use of cyanoacrylate glue is the possibility of reflux of the glue in the parent vessel [15]. This can lead to ischemia of the normal structures. There are reports of small bowel stricture due to glue spillover following treatment of visceral pseudoaneurysms [15]. In our second case, although there was some spillover of glue, it was only into small muscular branches, and not into the main vessel, and was thus asymptomatic. Balloon protection of the parent artery [15] (as was done in case 1) as well as ultrasound compression of the neck [13] help to reduce the risk of spillover of glue.
Contraindications to use of cyanoacrylate glue include large pulsatile groin hematomas, presence of an abscess, skin necrosis, and distal ischemia. Open surgical intervention is indicated in these cases.
Conclusion
Arterial pseudoaneurysms are increasingly being managed nonoperatively. Percutaneous cyanoacrylate glue injection under fluoroscopic guidance is a safe and inexpensive alternative to open surgery for peripheral pseudoaneurysms. It has the dual advantage of being minimally invasive as well as having a low failure rate.
Funding
Nil
References
- 1.Mansour MA, Gorsuch JM. Diagnosis and management of pseudoaneurysms. Perspect Vasc Surg Endovasc Ther. 2007;19(1):58–64. doi: 10.1177/1531003506298074. [DOI] [PubMed] [Google Scholar]
- 2.Kim BS, Do HM, Razavi M. N-butyl cyanoacrylate glue embolization of splenic artery aneurysms. J Vasc Interv Radiol. 2004;15(1 Pt 1):91–94. doi: 10.1097/01.RVI.0000099537.29957.13. [DOI] [PubMed] [Google Scholar]
- 3.Montgomery ML, Harisinghani MG, Norbash AM, Gervais DA, Kaufman JA, Mueller PR. CT and fluoroscopically guided percutaneous embolization treatment of a pseudoaneurysm associated with pancreatitis. J Vasc Interv Radiol. 2005;16(3):411–415. doi: 10.1097/01.RVI.0000147072.12096.3D. [DOI] [PubMed] [Google Scholar]
- 4.Garg A, Banait S, Babhad S, Kanchankar N, Nimade P, Panchal C. Endovascular treatment of pseudoaneurysm of the common hepatic artery with intra-aneurysmal glue (N-butyl 2-cyanoacrylate) embolization. Cardiovasc Intervent Radiol. 2007;30(5):999–1002. doi: 10.1007/s00270-007-9104-8. [DOI] [PubMed] [Google Scholar]
- 5.Lal A, Kumar A, Prakash M, Singhal M, Agarwal MM, Sarkar D, et al. Percutaneous cyanoacrylate glue injection into the renal pseudoaneurysm to control intractable hematuria after percutaneous nephrolithotomy. Cardiovasc Intervent Radiol. 2009;32(4):767–771. doi: 10.1007/s00270-009-9522-x. [DOI] [PubMed] [Google Scholar]
- 6.Schoder M, Cejna M, Langle F, Hittmaier K, Lammer J. Glue embolization of a ruptured celiac trunk pseudoaneurysm via the gastroduodenal artery. Eur Radiol. 2000;10(8):1335–1337. doi: 10.1007/s003309900227. [DOI] [PubMed] [Google Scholar]
- 7.Tisi PV, Callam MJ (2009) Treatment for femoral pseudoaneurysms. Cochrane Database Syst Rev (2):CD004981 [DOI] [PubMed]
- 8.Morgan R, Belli AM. Current treatment methods for postcatheterization pseudoaneurysms. J Vasc Interv Radiol. 2003;14(6):697–710. doi: 10.1097/01.RVI.0000071089.76348.6A. [DOI] [PubMed] [Google Scholar]
- 9.Kang SS, Labropoulos N, Mansour MA, Michelini M, Filliung D, Baubly MP, et al. Expanded indications for ultrasound-guided thrombin injection of pseudoaneurysms. J Vasc Surg. 2000;31(2):289–298. doi: 10.1016/S0741-5214(00)90160-5. [DOI] [PubMed] [Google Scholar]
- 10.Kresowik TF, Khoury MD, Miller BV, Winniford MD, Shamma AR, Sharp WJ, et al (1991) A prospective study of the incidence and natural history of femoral vascular complications after percutaneous transluminal coronary angioplasty. J Vasc Surg 13(2):328–333; discussion 33–35 [PubMed]
- 11.Criado E, Marston WA, Ligush J, Mauro MA, Keagy BA. Endovascular repair of peripheral aneurysms, pseudoaneurysms, and arteriovenous fistulas. Ann Vasc Surg. 1997;11(3):256–263. doi: 10.1007/s100169900043. [DOI] [PubMed] [Google Scholar]
- 12.Brophy DP, Sheiman RG, Amatulle P, Akbari CM. Iatrogenic femoral pseudoaneurysms: thrombin injection after failed US-guided compression. Radiology. 2000;214(1):278–282. doi: 10.1148/radiology.214.1.r00ja10278. [DOI] [PubMed] [Google Scholar]
- 13.Aytekin C, Firat A, Yildirim E, Kirbas I, Boyvat F. Ultrasound-guided glue injection as alternative treatment of femoral pseudoaneurysms. Cardiovasc Intervent Radiol. 2004;27(6):612–615. doi: 10.1007/s00270-004-0197-z. [DOI] [PubMed] [Google Scholar]
- 14.Toriumi DM, Raslan WF, Friedman M, Tardy ME., Jr Variable histotoxicity of histoacryl when used in a subcutaneous site: an experimental study. Laryngoscope. 1991;101(4 Pt 1):339–343. doi: 10.1002/lary.1991.101.4.339. [DOI] [PubMed] [Google Scholar]
- 15.Gulati GS, Gulati MS, Makharia G, Hatimota P, Saikia N, Paul SB, et al. Percutaneous glue embolization of a visceral artery pseudoaneurysm in a case of sickle cell anemia. Cardiovasc Intervent Radiol. 2006;29(4):665–668. doi: 10.1007/s00270-004-0204-4. [DOI] [PubMed] [Google Scholar]