Abstract
Background
Ethnic minority adolescents and Hispanics in particular, are disproportionately affected by extreme obesity and its associated co-morbidities. Bariatric surgery is one of the few effective treatments for morbid obesity, yet little information about weight outcomes after surgery in this demographic are available. We determined the effectiveness of bariatric surgery in reducing weight and body mass index (BMI) in adolescents, a majority of whom were non-Mexican American Hispanic and originated from Central and/or South America and the Caribbean Basin region.
Methods
Adolescents (16-to-19 years old) who had undergone gastric bypass or adjustable gastric band surgery between 2001 and 2010 and who had complete follow up data available (91%) were included in the analysis. Mean weight and BMI before and 1-year after surgery were compared.
Results
Among 71 adolescents (80% Hispanic, 77% female), Mean BMI and weight, and z-scores and percentile transformations were all significantly lower after surgery for the entire sample (P<0.001). Gastric bypass surgery showed significantly better weight loss outcomes for all anthropometric measures versus adjustable gastric band surgery (P<0.05). The weight loss was similar among Hispanics and non-Hispanics. No perioperative complications were reported. Three patients who stopped taking supplements as prescribed experienced iron-deficiency anemia within the year following surgery.
Conclusions
Our results show that bariatric surgery can markedly reduce weight among a predominantly Hispanic adolescent patient sample, and gastric bypass procedure in particular. These findings indicate that bariatric surgery has the potential to be safe and effective in substantially reducing weight in a group of adolescents who are at particularly high risk for obesity-related health consequences.
Keywords: overweight, treatment, pediatric, metabolic surgery, pre-diabetes, metabolic syndrome, Hispanic, multiethnic, adolescent
INTRODUCTION
The Centers for Disease Control and Prevention (CDC) recently reported that the prevalence of childhood obesity in the United States (US) has stabilized over the past few years, although it remains high among all age, sex, and ethnic groups [1]. However, an estimated 12% of all US children between 2 and 19 years old fall in the category of morbid obesity (a body mass index [BMI] ≥97th percentile for age and sex) [1]. Moreover, significant differences in obesity prevalence by race/ethnicity were noted. In 2009–2010, 21.2 % of Hispanic children and adolescents were obese compared with 14% of non-Hispanic white children and adolescents [1]. The authors also found that there was a significant increase in BMI among adolescent males ages 12 through 19 years from 1999–2000 to 2009–2010 [1].
Childhood-onset obesity has several short- and long-term health-related consequences, including hypertension, insulin resistance, glucose intolerance, dyslipidemia, and hypertension, which comprise the metabolic syndrome [2,3]. In turn, these conditions are risk factors for type 2 diabetes and cardiovascular disease in both childhood and adulthood [4–6]. Childhood overweight has also been associated with orthopedic problems [7], polycystic ovarian syndrome [8], non-alcoholic fatty liver disease [9], as well as anxiety and depression [10]. The majority of these health issues also tend to continue into adulthood [4,5]. Ethnic minorities are disproportionately affected by virtually all of these conditions, and diabetes and cardiovascular disease in particular.
In recent years, weight-loss surgery has become increasingly accepted as an effective method to resolve many of these comorbidities and is considered to be a reasonable option when other methods of weight loss fail [11–13]. Current studies suggest that neither pharmacological nor dietary treatment can maintain long-term weight loss in obese adolescents as effectively as can weight-loss surgery [13–15]. Although bariatric surgery is now accepted for adults as the treatment of choice for recalcitrant morbid obesity, bariatric surgeries in adolescents now account only for approximately 0.73% of the cases performed in the US, although this rate is expected to rise [16–19].
Moreover, studies of bariatric surgery in adolescents have enrolled predominantly non-Hispanic white patients, so there is little outcome data for ethnic minority groups in general and for non-Mexican American Hispanics in particular. Therefore, the aim of this study was to assess the reduction in weight and BMI in a cohort of ethnically diverse, predominantly Hispanic obese adolescents who underwent bariatric surgery.
METHODS
We reviewed the medical records of all adolescents ages 16-to-19 years who underwent bariatric surgery at a solo community-based surgical practice in Miami, Florida between 2001 and 2010. Patients were only included in this analysis if they had post-surgery anthropometric data available (71 out of 78 or 91%) to ensure a 100% follow-up rate. A medical complication was defined by the surgical program as any event which required either an intervention, an increase in the hospital stay, a readmission, or an emergency department visit within 30 days. This review included the surgeon’s clinic notes as well as a review of the hospital’s computer system for ER visits and readmission. All surgeries were performed by one surgeon. This study was approved by the University of Miami Institutional Review Board.
Measures
Data were collected on demographic characteristics (sex, race, and ethnicity), pre-surgical height and weight, BMI and peri-operative complications. Follow-up weight data were collected between 9 and 15 months after surgery.
A staff nurse measured height and weight during routine clinical visits. Weight was measured to the nearest 0.045 kilograms using a digital scale (Model 5002 Stand-On Scale; Scale Tronix, Inc., White Plains, New York) with participants wearing light clothing and no shoes. Height was measured to the nearest 0.5 cm using a wall-mounted stadiometer (Ayrton Stadiometer Model S100; Ayrton Corporation, Prior Lake, Minnesota). CDC weight classifications for youth using BMI (defined as weight [kg]/height [m]2) percentiles ranges; underweight (<5th), normal weight (≥5th to <85th), overweight (≥85th to <95th) obese (≥95th), and morbidly obese (≥97th) [1,19]. As in adults, BMI is an imperfect indicator of adiposity in children. However, because BMI is nonlinear in children, BMI percentiles and z-scores are used to evaluate weight and anthropometric change and were thus included in this analysis as the primary outcomes [20].
Surgical Eligibility
All patients were treated at a high-volume multidisciplinary bariatric program overseen by an adult bariatric surgeon (who performs between 250–400 bariatric procedures annually). All selected patients met the National Institutes of Health criteria for bariatric surgery [21–23]. As such, all had either a BMI greater than 35 kg/m2 with at least one co-morbidity (e.g., elevated blood pressure, hypercholesterolemia) or a BMI greater than 40 kg/m2.
The evaluation and preoperative approach was identical in adolescents and adults with only two exceptions; adolescents were (1) referred to a pediatric endocrinologist for a thorough evaluation to rule out any underlying endocrine disorder and (2) had x-rays taken to evaluate bone maturity to ensure the child had achieved adult status. All patients obtained medical clearance for surgery from their primary pediatrician. Follow-up information was conveyed to referring physician on patient-specific post-operative results (e.g. any information on complications, weight loss, co-morbidities, etc). Patients and their parents received group and individual interdisciplinary education about potential surgical and nonsurgical options, possible outcomes, possible complications, and necessary postoperative lifestyle changes. All patients underwent psychological and nutritional evaluations before surgery. Parents were required to attend the nutritional evaluation with their child.
Statistical Methods
Baseline differences in all demographic variables and BMI were compared via chi-square for categorical variables and t-test for continuous variables. To assess longitudinal change in weight and BMI, separate repeated-measures linear mixed models were fit using the MIXED procedure in SAS Version 9.2 (SAS Institute, Inc., Cary, North Carolina). A linear mixed models approach was used because this analysis technique accommodates data with complex covariance structures and randomly missing data. Age, sex, and ethnicity (Hispanic and non-Hispanic whites only because of insufficient numbers of non-Hispanic blacks and those identified as “other”) were the covariates considered for potential inclusion into each model. The interactions between time and ethnicity and time and sex were also assessed.
Statistical tests resulting in a probability of 0.05 or less were considered statistically significant. All data met the assumptions of the tests used to analyze them.
RESULTS
A total of 78 adolescent patients underwent bariatric surgery in the defined timeframe and of these, 71 had available data at the one year interval after surgery. The majority of the sample was Hispanic (80%), female (77%) and underwent gastric bypass surgery (92%) versus adjustable gastric band (8%). Mean (SD) age at surgery was 18.3 (1.04) years (Table 1).
Table 1.
Demographic Characteristics of Morbidly Obese Adolescents who Underwent Bariatric Surgery between 2001 and 2010.
| Characteristic | All | Male | Female |
|---|---|---|---|
| Sample size, n (%) | 71 (100) | 16 (23) | 55 (77) |
| Hispanic, n (%) | 57 (80) | 13 (81) | 44 (80) |
| Gastric bypass, n (%) | 65 (92) | 15 (94) | 50 (91) |
| Adjustable gastric band, n (%) | 6 (8) | 1 (6) | 5 (9) |
| Age, mean (SD), years | 18.3 (1.04) | 18.6 (0.93) | 18.3 (1.06) |
| Age range, years | 16.03–19.9 | 16.7–19.9 | 16.0–19.9 |
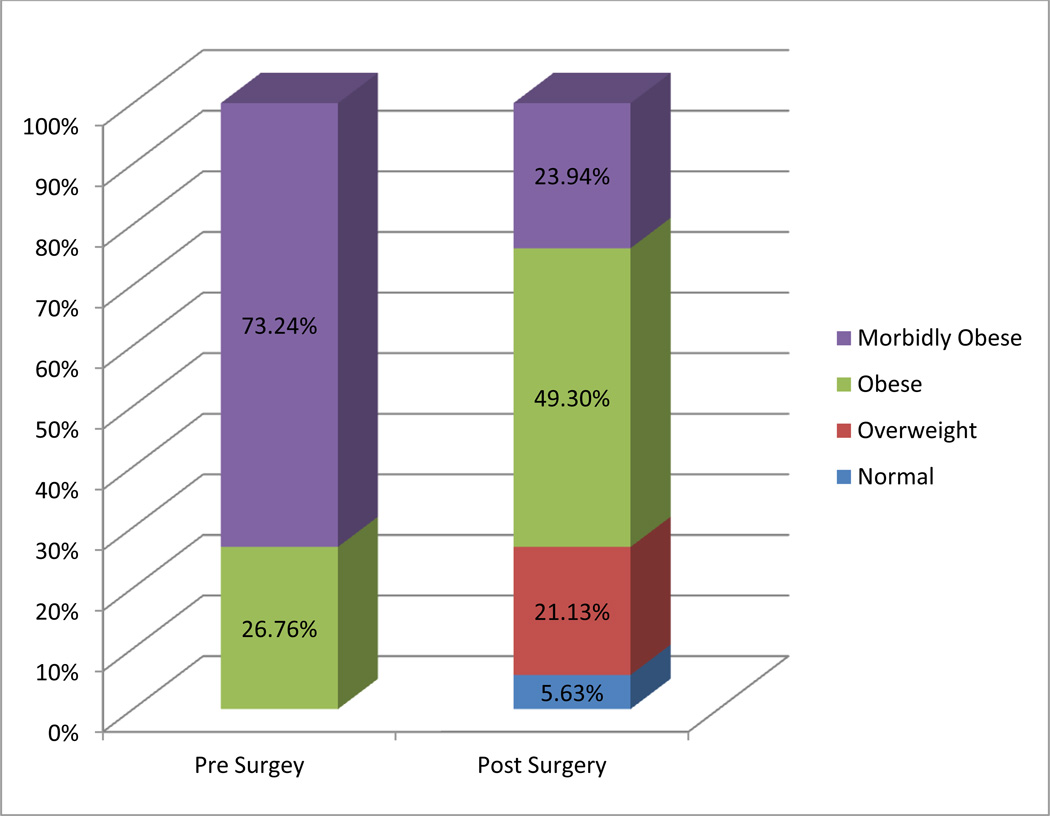
Mean BMI and weight as well as z-scores and percentile transformations were all significantly lower after surgery for the entire sample (P<0.001; Table 2). Whereas none of the children met normal or overweight criteria prior to the surgery, approximated 27% achieved these categories on follow-up. Thirty-five percent did not change weight category in follow-up (Figure 1).
Table 2.
Pre-1 Year Post Bariatric Surgery Differences in Anthropometric Measures by Sex, Ethnicity, and Surgery Type.
| Body Mass Index (kg/m2) |
Body Mass Index z-score |
Body Mass Index percentile |
Weight (kg) |
Weight z-score |
Weight percentile |
Estimated kg Lost |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Measure | Pre Mean(SE) (N = 71) |
Post Mean(SE) (N = 71) |
Pre Mean(SE) (N = 71) |
Post Mean(SE) (N = 71) |
Pre Mean(SE) (N = 71) |
Post Mean(SE) (N = 71) |
Pre Mean(SE) (N = 71) |
Post Mean(SE) (N = 71) |
Pre Mean(SE) (N = 71) |
Post Mean(SE) (N = 71) |
Pre Mean(SE) (N = 71) |
Post Mean(SE) (N = 71) |
Post Mean(SE) (N = 71) |
|
| Total* | 46.1(0.6) | 35.4(0.9) | 2.6(0.1) | 1.9(0.1) | 99.3(0.1) | 94.4(1.2) | 128.4(2.1) | 99.14(2.70) | 2.7(0.0) | 2.0(0.1) | 99.4(0.1) | 93.0(1.7) | 29.2(1.8) | |
| Male† | 49.7(1.7) | 39.2(2.4) | 3.1(0.8) | 2.3(0.2) | 99.9(0.1) | 94.8(3.5) | 155.1(5.3) | 121.56(7.17) | 3.4(0.1) | 2.4(0.3) | 99.9(0.1) | 93.1(4.4) | 32.5(4.5) | |
| Female† | 45.1(0.7) | 34.4(0.9) | 2.4(0.1) | 1.8(0.1) | 99.1(0.1) | 94.3(1.2) | 120.67(2.31) | 92.7(2.8) | 2.5(0.1) | 1.8(0.1) | 99.3(0.1) | 93.0(1.7) | 27.9(2.0) | |
| Hispanic†† | 45.8(0.7) | 35.5(0.9) | 2.6(0.1) | 1.9(0.1) | 99.3(0.1) | 94.3(1.5) | 127.01(2.43) | 98.3(3.0) | 2.7(0.1) | 2.0(0.1) | 99.4(0.1) | 92.7(1.9) | 28.6(2.0) | |
| Non-Hispanic†† | 47.3(1.5) | 35.2(2.1) | 2.6(0.1) | 1.9(0.1) | 99.4(0.1) | 95.1(1.5) | 132.64(3.51) | 101.3(5.9) | 2.8(0.1) | 2.1(0.2) | 99.6(0.1) | 94.2(3.4) | 31.0(4.7) | |
| Gastric Bypass‖ | 46.2(0.6) | 34.9(0.8) | 2.6(0.1) | 1.9(0.1) | 99.3(0.1) | 94.1(1.3) | 128.57(2.06) | 97.7(2.6) | 2.7(0.1) | 1.9(0.1) | 99.4(0.1) | 92.6(1.8) | 30.8(1.8) | |
| Lap Band‖ | 45.3(3.1) | 41.4(3.8) | 2.5(0.1) | 2.2(0.2) | 99.3(0.2) | 97.8(1.0) | 126.22(9.99) | 115.2(12.1) | 2.7(0.2) | 2.4(0.3) | 99.5(0.1) | 98.1(1.1) | 11.8(2.7) | |
All pre-post differences were statistically significant (P<0.001). Means adjusted by age and sex.
All differences between before and after surgery were statistically significant (P<0.01), except body mass index and weight percentile for male; no significant differences by sex were found. Means were adjusted by age.
All differences between before and after surgery were statistically significant (P<0.01), except weight percentile for non-Hispanic; but no significant differences by ethnicity were found. Means were adjusted by age and sex. The non-Hispanic group consisted of 9 non-Hispanic whites, 3 non-Hispanic blacks and 2 who identified as “other.”
All pre-post differences were statistically significant (P<0.01), except for BMI and weight z-score and percentiles for adjustable gastric band procedure. Estimated kg (weight) loss was the only variable significantly different by type of surgery (P<0.0001). All changes over time were significantly different by type of surgery (gastric bypass resulted in superior weight loss versus adjustable gastric band procedure). Means were adjusted by age and sex.
Figure 1.
Before and After Surgery Changes in Body Mass Index Percentile Categories among a Sample of Adolescents Who Underwent Bariatric Surgery.
Overall, female and male BMI loss were very similar 1 year after surgery (10.5 kg/m2 and 10.7 kg/m2, respectively); BMI was reduced from 49.7 kg/m2 to 39.2 kg/m2 among males and from 45.1 kg/m2 to 34 4 kg/m2 among females. Similarly, when the sample was stratified by ethnicity (Hispanic versus non-Hispanic) BMI among Hispanics was reduced from 45.8 kg/m2 to 35.5 kg/m2 and among non-Hispanic whites from 47.3 kg/m2 to 35.2 kg/m2. (Table 2)
When pre-post anthropometric measures were compared by type of surgery, gastric bypass surgery showed significantly better weight loss outcomes for all anthropometric measures versus adjustable gastric band surgery (P<0.05). The mean BMI loss among those who underwent gastric bypass surgery was almost 3 times that of those who underwent adjustable gastric band procedure (11.3 kg/m2 versus 3.9 kg/m2). (Table 2)
No perioperative complications were reported. There were two minor post-operative complications (nausea and vomiting) that resolved with medical management. Three patients developed iron deficiency anemia due to poor compliance with supplements. (data not shown on tables)
DISCUSSION
Bariatric surgery provides significant weight loss with minimum complications among multiethnic obese adolescents, and Hispanics in particular. Gastric bypass surgery shows significantly greater weight loss outcomes 1 year after surgery versus the adjustable gastric band procedure. Overall, 1-year after surgery, the mean BMI among Hispanic patients who underwent gastric bypass was no longer in the obese range according to their age- and sex-adjusted percentiles. Non-Hispanics had a similar positive response to surgery compared to Hispanics. Complications were few and manageable; a very important finding given that this is one of the biggest concerns of performing bariatric surgery in this specific population of patients. These findings indicate that bariatric surgery has the potential to be safe and effective in substantially reducing weight in multiethnic adolescents, a group that is at particularly high risk for obesity-related health consequences, such as diabetes and cardiovascular disease [1,2].
National prevalence estimates of morbid obesity (a BMI of ≥40 kg/m2) among US youth continue to increase [1]. Studies have shown that nearly one million adolescents in the US ages 12-to-19 years old, or about 4% of the population in this age range, have signs and symptoms of metabolic syndrome, the precursor to type 2 diabetes [2,24,25]. Among overweight adolescents, the prevalence is nearly 30% [24–27]. Even among children as young as 8-years old, national prevalence estimates of having at least one risk factor for metabolic syndrome range from 2% to 9%, using either of two age-, sex-, and ethnicity-adjusted definitions, and this prevalence was closely associated with obesity [24].
Currently, there is no standardized clinical protocol to treat metabolic syndrome in youth, yet the above studies clearly document that our nation may be facing a new and younger generation of type 2 diabetics and those with cardiovascular disease as a result of the increasing proportion of obese children and adolescents. Hispanics are at particularly high risk for type 2 diabetes and its complications. Specifically, after adjusting for population age differences, 2004-to-2006 national survey data for people 20 years or older indicate that 10.4% of Hispanics had a diagnosis of diabetes [28].
One unique characteristic of our Hispanic patient sample is that they are not only predominantly Hispanic, but are all non-Mexican American Hispanic. Instead, most originate from Cuba, Puerto Rico, or countries in Central and South America. Non-Mexican American Hispanics are at high risk for obesity and subsequent metabolic syndrome in other local studies [29] but there is little published information on their bariatric surgery outcomes. Overall, our results are consistent with others that have reported bariatric surgery outcomes among predominantly non-Hispanic whites, and to a lesser extent, non-Hispanic black adolescents that show significant weight loss after surgery [11,12].
Unfortunately, systematic reviews of lifestyle programs addressing changes in diet, exercise, and behavior to promote weight loss have found mostly poor results [10,30]. A recent meta-analysis that included 17 randomized controlled trials of lifestyle programs showed that adolescents experienced modest weight reduction for up to 12-months but weight gain afterward [10]. Furthermore, results from behavioral weight management programs, usually targeting those adolescents who are either overweight or obese, have reported poor rates of attendance and suboptimal weight reduction for youth with extreme obesity [10,31]. For extremely obese adolescents, even after 1 year in a well-designed weight management program, only modest BMI reductions were achieved, and these reductions were particularly less among ethnic minorities.
Our results reaffirm those of other studies [12,32] showing bariatric surgery to be a safe and effective method to reduce weight and consequent cardiometabolic risk for at least 1 year if other lifestyle-change interventions are not successful. It will be particularly important to examine outcomes beyond 1 year after surgery to determine whether positive changes can be maintained.
Finally, our results showing that gastric bypass surgery results in much greater weight loss outcomes versus the adjustable gastric band procedure parallels findings from larger, national cohort reports. [33] Specifically, nationally-representative data of 890 adolescents ages 11–19 years who underwent bariatric surgery from 2004–2010 showed the overall 1 year mean weight loss for those who underwent gastric bypass surgery was more than twice that of those who underwent adjustable gastric band surgery (48.6 kg versus 20 kg). Similar results were found for all other anthropometric changes and comparisons over one year between surgery types, as is reported here.
Limitations and Strengths of the Study
The main limitation of our study was not having adequate cardiometabolic clinical data to analyze in conjunction with the anthropometric outcome variables. Additionally, the process of reporting post-operative complications may potentially miss patients who were admitted to other hospitals and failed to report this upon follow up visits to the surgeon.
The major strength of this study was the reporting of a weight loss method among a predominantly Hispanic, non-Mexican American patient population, which has remained elusive in the literature, yet this group continues to be disproportionately affected by the current childhood obesity epidemic as well as type 2 diabetes and cardiovascular disease.
Conclusion
On the basis of our results, we believe the data support the following conclusions; (1) bariatric surgery can reduce weight and BMI irrespective of ethnicity and among Hispanics in particular; (2) Complications were few and manageable; a very important finding given that this is one of the biggest concerns of performing bariatric surgery in this specific population of patients; and (3) in a private-practice, high volume adult bariatric program, laparoscopic bariatric surgery can be safely performed in older adolescents with results similar to those in adults.
Acknowledgements
We would like to thank Kush Shaw for his help with data collection. We would like to thank all of the adolescent patients who participated in this study.
Funding Source: National Institutes of Health grant K01 DA 026993 (SEM)
Footnotes
Conflict of Interest Statements. Dr. de la Cruz-Munoz is a consultant and proctor for Ethicon EndoSurgery, which manufactures equipment for performing bariatric surgery. No conflicts of interest to report for Drs. Arheart, Miller, Lipshultz and Messiah and Ms. Lopez-Mitnik.
REFERENCES
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. J Am Med Assoc. 2012 Jan 17; doi: 10.1001/jama.2012.40. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ford ES, Chaoyang L. Defining the MS in children and adolescents: will the real definition please stand up? J Pediatr. 2008;152:160–164. doi: 10.1016/j.jpeds.2007.07.056. [DOI] [PubMed] [Google Scholar]
- 3.National Institutes of Health. Bethesda, MD: National Institutes of Health; 2001. The Third Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) NIH Publication 01-3670. [Google Scholar]
- 4.Sun SS, Liang R, Huang TT, et al. Childhood obesity predicts adult metabolic syndrome: the Fels Longitudinal Study. J Pediatr. 2008;152:191–200. doi: 10.1016/j.jpeds.2007.07.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morrison JA, Friedman LA, Wang P, Glueck CJ. Metabolic syndrome in childhood predicts adult MS and type 2 diabetes mellitus 25 to 30 years later. J Pediatr. 2008;152:201–206. doi: 10.1016/j.jpeds.2007.09.010. [DOI] [PubMed] [Google Scholar]
- 6.Must A, Anderson SE. Effects of obesity on morbidity in children and adolescent. Nutr Clin Care. 2003;6:4–12. [PubMed] [Google Scholar]
- 7.Sugerman HJ, DeMaria EJ, Kellum JM, et al. Effects of bariatric surgery in older patients. Ann Surg. 2004;240:243–247. doi: 10.1097/01.sla.0000133361.68436.da. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wild RA, Carmina E, Diamanti-Kandarakis E, et al. Assessment of cardiovascular risk and prevention of cardiovascular disease in women with the polycystic ovary syndrome: a position statement by the Androgen Excess and Polycystic Ovary Syndrome (AE-PCOS) Society. J Clin Endocrinol Metab. 2010;95:2038–2049. doi: 10.1210/jc.2009-2724. [DOI] [PubMed] [Google Scholar]
- 9.Patton HM, Yates K, Unalp-Arida A, et al. Association between metabolic syndrome and liver histology among children with nonalcoholic fatty liver disease. Am J Gastroenterol. 2010;105:2093–2102. doi: 10.1038/ajg.2010.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Davin SA, Taylor NM. Comprehensive review of obesity and psychological considerations for treatment. Psychol Health Med. 2009;14:716–725. doi: 10.1080/13548500903431501. [DOI] [PubMed] [Google Scholar]
- 11.Inge TH, Jenkins TM, Zeller M, et al. Baseline BMI is a strong predictor of nadir BMI after adolescent gastric bypass. J Pediatr. 2010;156 doi: 10.1016/j.jpeds.2009.07.028. 103-8.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Treadwell JR, Sun F, Schoelles K. Systematic review and meta-analysis of bariatric surgery for pediatric obesity. Ann Surg. 2008;248:763–776. doi: 10.1097/SLA.0b013e31818702f4. [DOI] [PubMed] [Google Scholar]
- 13.Allen SR, Lawson L, Garcia V, Inge TH. Attitudes of bariatric surgeons concerning adolescent bariatric surgery (ABS) Obes Surg. 2005;15:1192–1195. doi: 10.1381/0960892055002176. [DOI] [PubMed] [Google Scholar]
- 14.Yermilov I, McGory ML, Shekelle PW, Ko CY, Maggard MA. Appropriateness criteria for bariatric surgery: beyond the NIH guidelines. Obesity. 2009;17:1521–1527. doi: 10.1038/oby.2009.78. [DOI] [PubMed] [Google Scholar]
- 15.Hollenbeak CS, Rogers AM, Barrus B, Wadiwala I, Cooney RN. Surgical volume impacts bariatric surgery mortality: a case for centers of excellence. Surgery. 2008;144:736–743. doi: 10.1016/j.surg.2008.05.013. [DOI] [PubMed] [Google Scholar]
- 16.Daniels SR, Jacobson MS, McCrindle BW, Eckel RH, Sanner BM. American Heart Association Childhood Obesity Research Summit: executive summary. Circulation. 2009;119:2114–2123. doi: 10.1161/CIRCULATIONAHA.109.192215. [DOI] [PubMed] [Google Scholar]
- 17.Xanthakos SA, Daniels SR, Inge TH. Bariatric surgery in adolescents: an update. Adolesc Med Clin. 2006;17:589–612. doi: 10.1016/j.admecli.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 18.IPEG Standard and Safety Committee. IPEG guidelines for surgical treatment of extremely obese adolescents. J Laparoendosc Adv Surg Tech A. 2009;19:xiv–xvi. doi: 10.1089/lap.2009.9997. [DOI] [PubMed] [Google Scholar]
- 19.Collins J, Mattar S, Qureshi F, et al. Initial outcomes of laparoscopic Roux-en-Y gastric bypass in morbidly obese adolescents. Surg Obes Relat Dis. 2007;3:147–152. doi: 10.1016/j.soard.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. BMI - Body Mass Index: BMI for Children and Teens: 2011. [Accessed November 22, 2011]; Available at: http://www.cdc.gov/nccdphp/dnpa/bmi/bmi-for-age.htm.
- 21.Gastrointestinal surgery for severe obesity. NIH consensus development conference, March 25–7, 1991. Nutrition. 1996;12:397–404. [PubMed] [Google Scholar]
- 22.Inge TH, Krebs NF, Garcia VF, et al. Bariatric surgery for severely overweight adolescents: concerns and recommendations. Pediatrics. 2004;114:217–223. doi: 10.1542/peds.114.1.217. [DOI] [PubMed] [Google Scholar]
- 23.Al-Qahtani AR. Laparoscopic adjustable gastric banding in adolescent: safety and efficacy. J Pediatr Surg. 2007;42:894–897. doi: 10.1016/j.jpedsurg.2006.12.057. [DOI] [PubMed] [Google Scholar]
- 24.Messiah SE, Arheart KA, Lipshultz SE, Miller TL. Relationship between body mass index and metabolic syndrome risk factors among US 8- to 14-year-olds, 1999–2002. J Pediatr. 2008;153:215–221. doi: 10.1016/j.jpeds.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 25.Cook S, Auinger P, Li C, Ford ES. Metabolic syndrome rates in United States adolescents, from the National Health and Nutrition Examination Survey, 1999–2002. J Pediatr. 2008;152:165–170. doi: 10.1016/j.jpeds.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 26.Weiss R, Dziura J, Burgert TS, et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004;350:2362–2374. doi: 10.1056/NEJMoa031049. [DOI] [PubMed] [Google Scholar]
- 27.Messiah SE, Carrillo-Iregui A, Garibay-Nieto G, Cossio S, Arheart KL. Inter- and intra-ethnic group comparison of metabolic syndrome components among morbidly obese adolescents. J Clin Hyperten. 2010;12:645–652. doi: 10.1111/j.1751-7176.2010.00337.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Centers for Disease Control and Prevention. National Diabetes Fact Sheet: General Information and National Estimates on Diabetes in the United States, 2007. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2008. [Google Scholar]
- 29.Messiah SE, Carrillo-Iregui A, Garibay-Nieto, et al. The prevalence of the metabolic syndrome in US-born latin and afro-caribbean obese adolescents. J Immigr Minor Health. 2008;11:366–371. doi: 10.1007/s10903-008-9219-2. [DOI] [PubMed] [Google Scholar]
- 30.Zeller M, Kirk S, Claytor R, et al. Predictors of attrition from a pediatric weight management program. J Pediatr. 2004;144:466–470. doi: 10.1016/j.jpeds.2003.12.031. [DOI] [PubMed] [Google Scholar]
- 31.Levine MD, Ringham RM, Kalarchian MA, Wisniewski L, Marcus MD. Is family-based behavioral weight control appropriate for severe pediatric obesity? Int J Eat Disord. 2001;30:318–328. doi: 10.1002/eat.1091. [DOI] [PubMed] [Google Scholar]
- 32.Ippisch HM, Inge TH, Daniels SR, et al. Reversibility of cardiac abnormalities in morbidly obese adolescents. J Am Coll Cardiol. 2008;51:1342–1348. doi: 10.1016/j.jacc.2007.12.029. [DOI] [PubMed] [Google Scholar]
- 33.Messiah SE, Lopez-Mitnik G, Winegar D, Sharif B, Arheart K, Reichard K, Michalsky M, Lipshultz SE, Miller TL, Livingston A, De La Cruz Munoz N. Changes in Weight and Comorbidities among Morbidly Obese Adolescents Undergoing Bariatric Surgery: 1-Year Results from the Bariatric Outcomes Longitudinal Database (BOLD) Surgery for Obesity and Related Disorders. 2012 doi: 10.1016/j.soard.2012.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]