Abstract
In Schizophrenia, low motivation may play a role in the initiation and frequency of functional behaviors. Several reviews support the efficacy of the Theory of Planned Behavior (TPB) to predict engagement in various behaviors, but little research has utilized the TPB to explain functional behavior in schizophrenia. This study tested the TPB for predicting prospective engagement in functional behaviors in a sample of 64 individuals with schizophrenia. Participants completed questionnaires assessing their attitudes toward, social norms regarding, perceived behavioral control over, and intention to engage in various functional behaviors during the upcoming week. Follow-up questionnaires assessed engagement in functional behaviors. Zero-order correlations indicated that positive attitudes, social norms, and perceived behavioral control were positively correlated with intentions to engage in functional behaviors. In turn, intentions were positively correlated with engagement in functional behaviors. Using path analysis, social norms and control were significantly related to intentions, which in turn predicted greater engagement in functional behaviors. Results suggest that patients with schizophrenia make reasoned decisions for or against engaging in functional behaviors. Skills training interventions that also target components of the TPB may be effective for increasing motivation to engage in learned behaviors.
Keywords: Functioning, Motivation, Reasoned Action, Attitudes, Norms, Self-Efficacy
1. Introduction
Individuals with Schizophrenia are less likely to achieve higher order social milestones such as employment (Anthony and Blanch, 1987; Slade and Salkever, 2001) or independent living (Cohen et al., 2000; Palmer et al., 1999), and they often struggle to adequately perform daily functional tasks that serve as a foundation for higher order accomplishments (Aubin et al., 2009; Bowie et al., 2006; Burns and Patrick, 2007; Twamley et al., 2002). As a result, schizophrenia’s annual cost to society is $62 billion (Wu et al., 2005).
Despite these impairments to daily living skills, a diagnosis of schizophrenia does not resolve an individual to poor functioning. Significant variation in functioning exists across two spectrums, which we will term quality and quantity. By quality we mean the individual’s capacity to perform daily living tasks. Several studies in schizophrenia have documented variation in the quality spectrum (Bowie et al., 2008; Bowie et al., 2006; Mausbach et al., 2008a; Mausbach et al., 2008b). Much of this variance in quality has been attributed to deficits in neurocognition or functional capacity (Fett et al., 2011), with the assumption that individuals fail to perform functional behaviors because they do not have the cognitive ability (Green, 1996, 2006; Green et al., 2000) or they do not know how to perform the necessary action(s) (Mausbach et al., 2009). Although there is still room to improve prediction of functional ability, little doubt remains that these factors, along with clinical factors such as depressive symptoms (Conley, 2009; Conley et al., 2007) or positive and negative symptoms (Leifker et al., 2009) explain a significant amount of variance in who performs these behaviors well.
While potentially related to quality, we refer to quantity as the amount the individual actually performs the behavior. Quantity is influenced by a number of factors, most notably motivation. Thus, separate from an individual’s capacity to perform functional behaviors is their desire to regularly engage in them. Recent research has examined both physiologic and social contextual predictors of motivation. Physiologically, the prefrontal and subcortical mesolimbic dopamine systems appear to play a role in motivation in this population (Barch and Dowd, 2010). From a social contextual viewpoint, Choi, Fiszdon, and Medalia (2010) tested the expectancy-value theory of motivation (Eccles and Wigfield, 2002) and found that perceived self-competence for learning arithmetic was significantly related to the value participants’ placed on arithmetic (i.e., task value) and sustained learning of arithmetic ability three months following arithmetic training. These results provide evidence that cognitive attributions play a potentially crucial role in learning and behavior in schizophrenia.
While self-competence may play an important role in predicting functional behaviors, some individuals with schizophrenia may experience environmental barriers that would prevent them from performing a behavior even if they felt they knew how. In addition, expectations placed on the individuals to perform certain behaviors may enhance or hinder an individual’s motivation to engage in the behavior. Along these lines, the Theory of Planned Behavior (TPB) provides a strong model in which to examine motivation in this population (Ajzen, 1991). The TPB is an extension of the Theory of Reasoned Action (TRA)(Fishbein and Ajzen, 1975) which hypothesizes that the most proximal and direct predictor of human behavior is the individual’s intention to engage in the behavior. Intention, in turn, is directly predicted by two antecedent factors: a) the individual’s attitude toward performing the behavior, and b) the subjective normative expectations of others. In developing the TPB, Ajzen added a third predictor of behavioral intention titled “perceived behavioral control,” which encompassed both self-efficacy and environmental control. Ajzen conceptualized perceived behavioral control as directly predicting behavioral intention as well as the individual’s actual engagement in the behavior.
Several empirical reviews have demonstrated the TPB predicts engagement in various behaviors (Ajzen, 1991; Armitage and Conner, 2001; McEachan et al., 2011; Sheeran, 2002). However, there is a paucity of literature testing the TPB in schizophrenia. One study of Hispanic patients diagnosed with schizophrenia found that medication compliance was predicted by patients’ intention to comply, social norms, and perceived behavioral control (Kopelowicz et al., 2007). This study laid a foundation for using TPB for predicting other outcomes in this population.
The primary aim of this study was to examine the usefulness of the TPB for predicting everyday functional behaviors of individuals with schizophrenia. The particular behaviors we studied revolved around household tasks such as cleaning, doing laundry, and cooking meals, as well as social tasks such as planning activities and socializing with others. We tested the following hypotheses:
More positive attitudes, norms, and perceived control would be significantly related to greater intentions to engage in these behaviors.
Greater intentions to engage in these behaviors would be significantly related to greater engagement in these behaviors.
Greater perceived behavioral control would be significantly related to greater engagement in these behaviors.
2. Methods
2.1. Participants
A total of 64 patients with schizophrenia were enrolled in a randomized trial examining the efficacy of two psychosocial, skills-training interventions for improving functioning in schizophrenia. Participants were required to be at least 40 years of age, have a physician-determined diagnosis of either schizophrenia or schizoaffective disorder that was verified by reviewing medical records for consistency of this diagnosis, and to be psychiatrically stable (e.g., taking antipsychotic medications and not an inpatient at baseline). Participants were primarily recruited from local day treatment or board-and-care (B&C) facilities via presentation of the project by research staff. The protocol was approved by the UCSD Institutional Review Board (IRB) and all participants provided informed consent prior to enrolling in the study.
The 64 participants were primarily middle-aged (mean age = 52.4 years, SD = 6.6), male (60.9%), and resided in a Board and Care setting (85.9%). A majority of participants was White (60.9%), 21.9% were Black, and 9.4% were Hispanic. On average, participants had completed 12 years of education and were experiencing mild clinical symptoms (see Table 1 for sample characteristics).
Table 1.
Characteristics of the sample (N = 64)
| Variable | Sample Range | |
|---|---|---|
| Age, M (SD) | 52.4 (6.4) | 39-56 |
| Male, n (%) | 39 (60.9) | |
| Race/Ethnicity, n (%) | ||
| White | 39 (60.9) | |
| Black | 14 (21.9) | |
| Hispanic | 6 (9.4) | |
| American Indian | 4 (6.2) | |
| Other | 1 (1.6) | |
| Years of education, M (SD) | 12.2 (2.4) | 6-17 |
| PANSS Positive, M (SD) | 14.7 (5.4) | 7-27 |
| PANSS Negative, M (SD) | 17.3 (5.6) | 8-33 |
| PANSS Total, M (SD) | 66.9 (16.1) | 38-103 |
| UPSA Total, M (SD) | 69.9 (14.0) | 27-91 |
| CDSS Total, M (SD) | 4.4 (4.3) | 0-16 |
| Current Living Situation, n (%) | ||
| Board and Care | 55 (85.9) | |
| Private house or apartment | 9 (14.1) | |
| Engagement in Functional Behaviors | ||
| Taking Medications, M (SD) | 2.6 (2.91) | 0-6 |
| Doing Laundry, M (SD) | 0.81 (0.99) | 0-6 |
| Cooking Meals, M (SD) | 0.63 (1.59) | 0-6 |
| Cleaning Room, M (SD) | 2.89 (2.46) | 0-6 |
| Planning Activity, M (SD) | 1.89 (1.98) | 0-6 |
| Socializing, M (SD) | 4.48 (2.09) | 0-6 |
| TPB Constructs | ||
| Attitudes, M (SD) [range = -54 - 541 | 29.59 (13.55) | -10 to 54 |
| Social Norms, M (SD) [range = -12 - 121 | 4.59 (4.52) | -12 to 12 |
| Perceived Behavioral Control, M (SD) | 25.52 (22.98) | -42 to 72 |
| Intentions, M (SD) | 3.66 (5.03) | -8 to 12 |
Note. PANSS = Positive and Negative Syndromes Scale. UPSA = UCSD Performance-based Skills Assessment. CDSS = Calgary Depression Scale for Schizophrenia. TPB = Theory of Planned Behavior.
2.2. Measures
For the current study, six functional behaviors were selected based on feedback from family caregivers, B&C staff, and clinical professionals who described these tasks as indicative of good everyday functioning if performed on a regular basis. The six behaviors were: a) Taking your own medications without any help, b) doing your laundry by yourself without any help, c) cooking a meal by yourself without any help, d) cleaning your room/house without any help, e) planning a fun activity without any help, and f) socializing with someone for at least 15 minutes.
For these six behaviors we developed a total of four questionnaires based on the guidelines provided by Francis et al. (2004) to assess each of the components of the TPB. Our scales were similar to TPB questionnaires found in the literature that examined behavioral outcomes in non-schizophrenia populations (Ajzen, 1991, 2002). Each of the four questionnaires is described in more detail below.
2.2.1. Attitudes
Participants were read each behavior and asked, “In your opinion, _____ over the next week would be”, with response options ranging from 3 = “extremely good” to -3 = “extremely bad” (e.g., “In your opinion, doing your laundry by yourself without any help during the next week would be”). Next, participants were again read each behavior and asked, “In your view, _____ over the next week is”, with response options ranging from 3 = “Extremely important” to -3 = “Extremely unimportant,” with 0 = “neither important nor unimportant” being the midpoint. Thus, responses were on a 7-point bipolar continuum as recommended by Azjen (1991). Finally, for each behavior participants were asked, “In your view, _____ over the next week is”, with response options ranging from 3 = “Extremely useful” to -3 = “Extremely useless.” Scores from these 18 items were summed to create an overall attitudes score (= 0.89). In addition, 6-months after the original assessment we re-administered the questionnaire to 17 of the 64 individuals to determine test-retest reliability, which was 0.63 for this scale.
2.2.2. Social Norms
Participants were asked to respond to 6 items (1 for each behavior) based on the following stem, “Most people who are important to you think you should ____” (e.g., “Most people who are important to you think you should clean your room/house without any help during the next week”). Response options ranged on a 5-point scale from 2 = “strongly agree” and -2 = “strongly disagree”, with 0 = “neither agree nor disagree” as the midpoint of the scale. The six items were summed to create an overall score (= 0.77), and 6-month test-retest reliability was 0.65.
2.2.3. Perceived Behavioral Control
Participants were first asked to rate how easy or difficult each task was for them, with responses ranging on a 7-point scale from 3 = “extremely easy” to -3 = “extremely difficult” (e.g., “Cooking a meal by yourself is _____”), with 0 “neither easy nor difficult’ as the midpoint. Participants then responded how true or false it was that there were things that would prevent them from performing each behavior, with response options ranging on a 7-point scale from 3 = “extremely false” to -3 = “extremely true” (e.g., There are things that would prevent you from planning a fun activity without any help over the next week”). Next, participants indicated how true or false it was that they a) had control over their ability to perform the behavior, and b) would easily be able to perform the behavior. Response options ranged from 3 = “extremely true” and -3 = “extremely false.” Responses to these 24 items were summed to create an overall score (= 0.91), and 6-month test-retest was 0.77.
2.2.4. Intentions
Participants were asked to report their intent to perform each of these 6 behaviors “over the next week” (e.g., “You intend to take your own medications without any help over the next week”), with response options ranging from 2 = “strongly agree” to -2 = “strongly disagree,” with 0 = ‘neither agree nor disagree’. A total intentions score was created by summing the 6 items (= 0.77), and 6-month test-retest was 0.69.
2.2.5. Performance of Functional Behaviors
After completing the questionnaire, participants were contacted approximately 1 week later and asked to report the total number of times they performed each behavior over the past week on a 7-point scale. Response options were: 0 = None, 1 = 1 time, 2 = 2 times, 3 = 3 times, 4 = 4 times, 5 = 5 times, 6 = 6 or more times. To reflect the fact that some functional behaviors could occur more frequently than others (e.g., socializing can occur more frequently than doing the laundry), we converted responses for each behavior to standardized z-scores so that all behaviors were measured on the same metric. Following this conversion, z-scores for the 6 behaviors were summed to reflect the overall frequency with which participants engaged in these functional behaviors.
2.2.6. Clinical Symptoms
Participants were interviewed using the Positive and Negative Syndrome Scale (PANSS)(Kay et al., 1987). A research associate assigned a score from 1-7 for each of the 30 items, with higher scores reflecting higher pathology. Items for each subscale were summed to subscale scores, with a PANSS total computed by summing all 30 items (range = 30-210).
Depressive symptoms were assessed using the Calgary Depression Scale for Schizophrenia (CDSS)(Addington and Addington, 1990). The CDSS was designed specifically for use in schizophrenia to assess depressive symptoms independent of symptoms of psychopathology typically evident in patients with schizophrenia, particularly negative symptoms. Total scores are created by summing scores for each of the 9 items (range = 0-27). In our study, a single research assistant conducted all ratings of clinical symptoms (both PANSS scores and depressive symptoms). Thus, we did not evaluate Intraclass Correlation Coefficients (ICCs) for these scales.
2.2.7. Functional Capacity
Each participant was also administered the UCSD Performance-based Skills Assessment (UPSA)(Patterson et al., 2001) as an indicator of functional capacity. The UPSA consists of 5 subtests each requiring participants to role-play functional behaviors similar to those typically required of patients with schizophrenia on a day-to-day basis. Participants receive an overall score ranging from 0-100, with higher scores indicative of higher functional capacity.
2.3. Statistical Analyses
Initially, we conducted correlation analyses to establish univariate effect sizes (Pearson r) between each of the TPB variables of interest and the frequency of engagement in functional behaviors. Following these initial analyses we tested the TPB model using path analysis, in which attitudes, social norms, and perceived behavioral control were entered as endogenous variables predicting intention to perform functional behaviors. In addition, intention and perceived behavioral control were entered as predictors of true engagement in functional behaviors. Our initial model also included three clinical covariates as predictors of intentions and true engagement in functional behaviors: a) PANSS total scores, b) CDSS scores, and c) UPSA scores. The final model was developed iteratively, in which non-significant clinical covariates were sequentially eliminated until the best-fitting model was identified, as indicated by three goodness-of-fit statistics: a) chi-square, b) comparative fit index (CFI), and c) root mean square error of approximation (RMSEA). A non-significant chi square test, a CFI >.90, and an RMSEA < .08 were considered satisfactory in terms of model fit.
Following our path analyses we conducted a series of secondary analyses to determine if intention to perform specific functional behaviors predicted engagement in that behavior over the following week. Each of the 6 functional behaviors was first recoded to reflect whether or not the individual reported engaging in the behavior. Then, a series of logistic regression analyses was conducted to determine if intention to perform the behavior and perceived control over the behavior significantly predicted engagement in it.
3. Results
3.1. Preliminary Tests
Prior to conducting analyses we examined all variables for normality. First, we examined the TPB constructs of attitudes, norms, control, and intentions, of which only norms was significantly skewed (with a negative skew) and was subjected to transformation to achieve normal distribution. For the individual behaviors, laundry, cooking meals, and activity were positively skewed and socializing was negatively skewed. These variables were transformed to achieve normal approximation. Following transformation, the frequency of the individual behaviors was standardized using z-score transformation to allow behaviors that might occur less frequently (e.g., laundry) to be combined with those that might occur more frequently (e.g., socializing with others). These z-scores were then added to create an overall score reflecting engagement in functional behaviors.
3.2. Zero order Relations between TPB constructs
Pearson correlations between all major study variables are presented in Table 2. As seen, correlations between TPB constructs provided strong support for individual relations between variables. Specifically, participants reported stronger intentions to engage in functional behaviors when they reported more positive attitudes toward these behaviors (r(62) = .58, p < .001), greater social expectations for performing these behaviors (r(62) = .62, p < .001), and greater perceived behavioral control (r(62) = .69, p < .001). Further, intentions (r(62) = .41, p = .001), social norms (r(62) = .27, p = .029), and perceived behavioral control (r(62) = .36, p = .004) were significantly related to performance of functional behaviors, whereas attitudes (r(62) = .23, p = .063) were not.
Table 2.
Zero order correlations between study variables
| Variable | 1. | 2. | 3. | 4. | 5. | 6. | 7. |
|---|---|---|---|---|---|---|---|
| 1. Functional Behaviors | -- | ||||||
| 2. Intentions | .41* | -- | |||||
| 3. Attitudes | .23 | .58* | -- | ||||
| 4. Social Norms | .27* | .62* | .74* | -- | |||
| 5. Perceived Behavioral Control | .36* | .69* | .71* | .57* | -- | ||
| 6. UPSA | −.11 | −.16 | −.03 | .04 | −.10 | -- | |
| 7. PANSS Total | .05 | .07 | .20 | .02 | .19 | -.09 | -- |
| 8. CDSS | −.02 | −.06 | −.07 | .00 | −.20 | .11 | .44* |
Note. p < .05. df = 62. UPSA = UCSD Performance-based Skills Assessment. PANSS = Positive and Negative Syndromes Scale. CDSS = Calgary Depression Scale for Schizophrenia.
3.3. Path Analysis of the TPB model
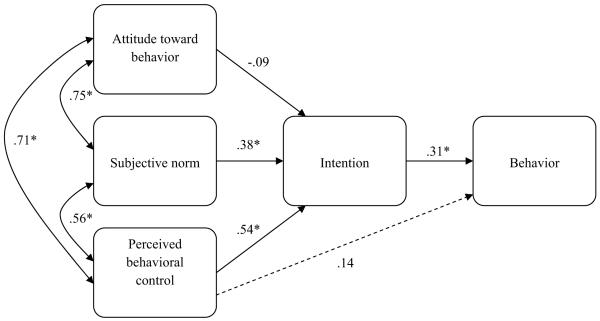
Results of our path analysis indicated that our saturated model, which used clinical covariates as predictors of intention and behaviors, had poor model fit (chi-square = 33.08, df = 22, p = .003). Subsequent analyses indicated that optimal model fit was achieved when testing the TPB alone (chi-square = 0.36, df = 2, p = .835; CFI = 1.0; RMSEA = 0.0, 90% CI = .00-.14). Figure 1 presents standardized path coefficients for our final model with unstandardized coefficients presented in the text that follows. Specifically, social norms (B = 0.43, SE = 0.14; p = .003) and levels of perceived control (B = 0.12, SE = 0.03; p < .001) were positively associated with intention to perform functional behaviors. However, attitudes were not significantly related to intentions (B = −0.03, SE = 0.06, p = .538). As a whole, attitudes, norms, and control accounted for 55.4% of the variance in intentions to perform functional behaviors. In turn, stronger intention to perform behaviors was associated with greater engagement in functional behaviors (B = 0.19, SE = 0.10, p = .05). However, perceived control was not significantly related to engagement in functional behaviors (B = 0.02, SE = 0.02, p = .360). Together, these variables accounted for 17.8% of the variance in functional behaviors.
Figure 1.
Path analysis of the relations between TPB constructs and patient report of functional behaviors (N = 64).
Note. Standardized path coefficients appear along single-headed arrows. Values along double-headed arrows represent correlation coefficients. *p ≤.05.
3.4. Logistic Regression Analyses Predicting Presence of Functional Behaviors
3.4.1. Use of Medications
Results of our first logistic regression indicated that greater intention to take medications significantly predicted whether participants took their own medications (yes vs. no; OR = 2.13, 95% CI = 1.37-3.33). A follow-up analysis indicated that intentions remained significant (OR = 2.68, 95% CI = 1.34-5.38) even when controlling for perceived behavioral control (OR = 0.93, 95% CI = 0.79-1.10), PANSS Total symptoms (OR = 1.00, 95% CI = 0.96-1.05), depressive symptoms (OR = 0.94, 95% CI = 0.79-1.11), and UPSA scores (OR = 0.99, 95% CI = 0.95-1.03).
3.4.2. Doing Laundry
Greater intention to do laundry significantly predicted whether or not participants did their own laundry (OR = 2.48, 95% CI = 1.55-3.96). A follow-up analysis showed that intention remained significant (OR = 1.99, 95% CI = 1.10-3.59) when controlling for perceived behavioral control (OR = 1.14, 95% CI = 0.96-1.34), PANSS Total symptoms (OR = 1.00, 95% CI = 0.95-1.04), depressive symptoms (OR = 0.99, 95% CI = 0.83-1.18), and UPSA scores (OR = 0.98, 95% CI = 0.93-1.02).
3.4.3. Cooking Meals
Participants with greater intention to cook meals were significantly more likely to cook their own meals (OR = 1.93, 95% CI = 1.07-3.48). However, this association became non-significant (OR = 2.59, 95% CI = 0.91-7.33) when controlling for perceived behavioral control (OR = 1.04, 95% CI = 0.83-1.31), PANSS Total symptoms (OR = 1.06, 95% CI = 1.00-1.12), depressive symptoms (OR = 0.93, 95% CI = 0.76-1.14), and UPSA scores (OR = 1.10, 95% CI = 1.01-1.20).
3.4.4. Household Cleaning
Again, stronger intentions to clean one’s house or room predicted greater likelihood this behavior occurred (OR = 1.83, 95% CI = 1.17-2.88), but this relationship became non-significant (OR = 1.80, 95% CI = 0.96-3.39) after controlling for perceived behavioral control (OR = 1.04, 95% CI = 0.90-1.20), PANSS Total symptoms (OR = 0.99, 95% CI = 0.95-1.04), depressive symptoms (OR = 1.01, 95% CI = 0.84-1.21), and UPSA scores (OR = 1.04, 95% CI = 0.99-1.09).
3.4.5. Planning Fun Activities
There was not a significant relationship between intention to plan an activity and actual performance of this behavior (OR = 1.33, 95% CI = 0.78-2.27). Further, none of our covariates was significantly associated with planning of activities, with odds ratios ranging from 0.93 for CDSS to 1.17 for perceived behavioral control.
3.4.6. Socializing with Others
Finally, greater intention to socialize was associated with stronger likelihood of socializing with others (OR = 5.42, 95% CI = 1.49-19.70). This relationship remained significant (OR = 8.41, 95% CI = 1.14-61.86) when controlling for perceived behavioral control (OR = 0.99, 95% CI = 0.63-1.57), PANSS Total symptoms (OR = 0.97, 95% CI = 0.89-1.06), depressive symptoms (OR = 1.25, 95% CI = 0.87-1.81), and UPSA scores (OR = 0.97, 95% CI = 0.87-1.08).
4. Discussion
This is one of the first to studies to investigate functional behaviors of people with schizophrenia from a social environmental perspective. Results indicated that the TPB is a promising model to predict everyday functional behaviors in this population. Consistent with the TPB, stronger social norms and increased perceived behavioral control were significantly related to greater intentions to perform functional behaviors. However, attitudes toward functional behaviors did not significantly predict intentions in our multivariate path model. Also consistent with the TPB, intentions served as the strongest direct predictor of engagement in functional behaviors. Good support was found for our findings in comparison with the proportion of variance typically accounted for by the TPB. In this study, a medium-large correlation (r = .41) between intention and behavior was found, which is consistent with the average intention-behavior correlations across four meta-analytic studies encompassing a variety of health behaviors (Armitage and Conner, 2001; Godin and Kok, 1996; Randall and Wolff, 1994; Sheeran and Orbell, 1998). However, somewhat divergent from the TPB, perceived control did not directly predict engagement in functional behaviors in our path model, although the zero order correlation (r = .36) was comparable to those of previous applications of the TPB. Further, consistent with the TPB, other variables (symptoms of psychopathology, functional capacity, and depressive symptoms) were not related to intention or behavior.
These findings lend initial support to the prospect that patients with schizophrenia make reasoned decisions for or against engaging in functional behaviors. This “reasoned action” entails being motivated to initiate the behavior (i.e., intention). Motivation, or intention to perform behaviors, may be influenced by cognitions that the behavior is useful and important, that important others believe it is essential they engage in the behavior, and that the individual perceives he/she has the ability to successfully carry out the behavior. One caveat, however, of this implication is that intention appears more powerful as a predictor of some functional behaviors than others. Specifically, results of our logistic regression analyses suggest that intention significantly predicted medication-taking, doing laundry, and socializing with others, even when controlling for other factors deemed important to functioning. However, while intention also predicted cooking and cleaning behaviors in our univariate model, significance of these effects was lost when controlling for other factors. Thus, when evaluating the value of the TPB one should consider the specific behavior being targeted. We will note, however, that although our multivariate logistic regression analyses did not reach significance for cooking and cleaning, the effect sizes for intention in these models were not changed substantially from the univariate models, suggesting that power may have been limited by our relatively small sample size.
One implication of these findings is that interventions targeting functional outcomes may benefit from targeting components of the TPB. Specifically, interventions that rely on homework for continued practice and subsequent mastery of skill(s), including the currently recommended skills-training interventions for schizophrenia (Dixon et al., 2010), may produce stronger effects if attitudes, norms, and control are targeted as a means of improving the patient’s motivation to learn, practice, and master these skills in his/her real-world environment. Indeed, in the absence of strong social norms or environments that facilitate continued practice, completion of homeworks as intended is questionable (Dixon et al., 2010). More recently, skills-training interventions have made use of novel techniques, some of which target constructs in the TPB, to facilitate real-world practice of skills (Glynn et al., 2002; Kopelowicz et al., 2003). However, although more recent skills-training interventions make use of social reinforcement and encouragement to enhance real-world effects of these interventions, formal assessment of TPB constructs as “motivation enhancers” or as mediators of treatment outcome is lacking. To date, two cross-sectional studies support the assertion that TPB precursors to motivation may improve the capacity-to-functioning relationship. The first found that individuals with greater skills and stronger confidence in their ability to perform the behavior were rated as having greater functioning than those with high skill but low confidence (Cardenas et al., 2012). The second found that individuals with low control over behaviors (i.e., more restrictive living circumstances) were less likely to demonstrate good real-world functioning despite having adequate capacity (Gupta et al., 2012). We recommend that future skills-training intervention studies formally examine the role of TPB constructs in predicting motivation to practice skills, as well as mediate treatment efficacy.
There are limitations to this study. First, the majority of participants resided in Board and Care (B&C) facilities, environments that may not support full independence in functional behaviors. Specifically, B&C facilities may not allow residents to cook, take their own medications, or plan their own outings, even when individuals are functionally capable of doing so (Mausbach et al., 2008b), and this may prevent them from learning and mastering the skills necessary to promote independent living (Gupta et al., 2012). We recommend expanding this study to include individuals residing in more diverse residential settings, ranging from assisted-living arrangements to fully independent ones.
Second, our study utilized self-reported engagement in functional behaviors, with no proxy-based reports of behavior. In their meta-analysis of the TPB, Armitage and Conner (2001) reported that intention was more strongly correlated with self-reported behavior than proxy-reported. Further, recent studies have reported on the accuracy of self-reported functioning in patients with schizophrenia (Bowie et al., 2007; Sabbag et al., 2011; Sabbag et al., 2012). These studies suggest that self-reports generally do not agree with proxy or performance-based ratings of functioning. However, these studies investigated congruence in quality of functioning rather than quantity. In contrast, our study focused exclusively on the initiation and quantity of behaviors. Nonetheless, future research should replicate these findings using other reports of behavioral initiation, with very clear descriptions on what qualifies as initiating a behavior.
Third, because this study reflects an initial attempt to validate the TPB for predicting functional behaviors in schizophrenia, we did not include other potentially important predictors of motivation (i.e., intent) or functional outcomes. These might include variables such as self-identity (Armitage and Conner, 1999; Sparks and Guthrie, 1998; Terry et al., 1999) as well as a more complete look into motivational processes in this population that evaluate the value of TPB constructs simultaneously with other biopsychosocial predictors such as cognitive functioning, variation in prefrontal and subcortical mesolimbic dopamine systems (Barch and Dowd, 2010), and variables related to the expectancy-value theory of motivation (Choi et al., 2010).
Finally, one issue that remains is the added value of the TPB over other well-established cognitive and behavioral theories. While the current study cannot address the added value of TPB components such as social norms or perceived behavioral control relative to dimensions such as negative self-beliefs or automatic thoughts common to cognitive-behavior therapies, we note that the TPB represents a novel area of investigation in the field of schizophrenia research, particularly intervention research. Specifically, the TPB has been the basis of dozens of unique interventions designed to promote behavior change, most notably health behaviors (Hardeman et al., 2002), yet none of these interventions focused on changing behavior in patients with schizophrenia. In addition, Hardeman and colleagues (2002) suggest that although other cognitive and behavioral theories (e.g., Social Cognitive Theory (Bandura, 1986)) have been the foundation of many behavior change interventions, the TPB stands apart from SCT with its strong emphasis on changing behavioral intentions (i.e., motivation), particularly among individuals who may lack intention to perform particular behaviors. Finally, in many cases, the TPB is not the sole theoretical basis of interventions. Rather, the TPB often is included alongside other social and cognitive theories (e.g., Social Cognitive Theory). This suggests that interventions based on other cognitive theories may indeed incorporate aspects of the TPB, and researchers could then compare these combined intervention models to stand-alone interventions to determine the added benefit of the TPB. We welcome and recommend this line of researchers.
In spite of these limitations, the results of this study demonstrate the efficacy of the TPB model to explain the value in assessing intention, and to a lesser degree perceived behavioral control, when attempting to predict future behaviors in individuals with schizophrenia. Future studies would benefit from manipulating the environment in a way to increase attitudes, subjective norms, and perceived behavioral control, which would likely have direct implications on intentions and subsequent behaviors. For example, if someone is not expected to clean their own living space, nor is it the expectation for similar individuals in their living environment, the individual is less likely to have any intentions to engage in the behavior in question. The TPB has consistently demonstrated that changing these factors could directly impact behavioral change. Developing a better understanding of human social behavior as it pertains to individuals with schizophrenia can help reduce the economic burden associated with of this disease, and hopefully start paving the way for improving overall quality of life in those with serious mental illness.
Acknowledgements
Funding from this study was provided by the National Institute of Mental Health (NIMH) through awards R01 MH084967 and P30 MH080002.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Addington D, Addington J. A depression rating scale for schizophrenics. Schizophrenia Research. 1990;3:247–251. doi: 10.1016/0920-9964(90)90005-r. [DOI] [PubMed] [Google Scholar]
- Ajzen I. The Theory of Planned Behavior. Organ Behav Hum Decis Process. 1991;50:179–211. [Google Scholar]
- Ajzen I. Perceived behavioral control, self-efficacy, locus of control, and the theory of planned behavior. Journal of Applied Social Psychology. 2002;32:1–20. [Google Scholar]
- Anthony WA, Blanch A. Supported employment for persons who are psychiatrically disabled: an historical and conceptual perspective. Psychosocial Rehabilitation Journal. 1987;11:5–23. [Google Scholar]
- Armitage CJ, Conner M. The theory of planned behaviour: Assessment of predictive validity and ‘perceived control. British Journal of Social Psychology. 1999;38:35–54. [Google Scholar]
- Armitage CJ, Conner M. Efficacy of the Theory of Planned Behaviour: a meta-analytic review. British Journal of Social Psychology. 2001;40:471–499. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- Aubin G, Stip E, Gelinas I, Rainville C, Chapparo C. Daily activities, cognition and community functioning in persons with schizophrenia. Schizophrenia Research. 2009;107:313–318. doi: 10.1016/j.schres.2008.08.002. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Prentice-Hall; Englewood Cliffs, NJ: 1986. [Google Scholar]
- Barch DM, Dowd EC. Goal representations and motivational drive in schizophrenia: the role of prefrontal-striatal interactions. Schizophrenia Bulletin. 2010;36:919–934. doi: 10.1093/schbul/sbq068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowie CR, Leung WW, Reichenberg A, McClure MM, Patterson TL, Heaton RK, Harvey PD. Predicting schizophrenia patients’ real-world behavior with specific neuropsychological and functional capacity measures. Biological Psychiatry. 2008;63:505–511. doi: 10.1016/j.biopsych.2007.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowie CR, Reichenberg A, Patterson TL, Heaton RK, Harvey PD. Determinants of real-world functioning performance in Schizophrenia: Correlations with cognition, functional capacity, and symptoms. American Journal of Psychiatry. 2006;163:418–425. doi: 10.1176/appi.ajp.163.3.418. [DOI] [PubMed] [Google Scholar]
- Bowie CR, Twamley EW, Anderson H, Halpern B, Patterson TL, Harvey PD. Self-assessment of functional status in schizophrenia. Journal of Psychiatric Research. 2007;41:1012–1018. doi: 10.1016/j.jpsychires.2006.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns T, Patrick D. Social functioning as an outcome measure in schizophrenia studies. Acta Psychiatr Scand. 2007;116:403–418. doi: 10.1111/j.1600-0447.2007.01108.x. [DOI] [PubMed] [Google Scholar]
- Cardenas V, Abel S, Bowie CR, Tiznado D, Depp CA, Patterson TL, Jeste DV, Mausbach BT. When Functional Capacity and Real-World Functioning Converge: The Role of Self-Efficacy. Schizophrenia Bulletin. 2012 doi: 10.1093/schbul/sbs004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi J, Fiszdon JM, Medalia A. Expectancy-value theory in persistence of learning effects in schizophrenia: role of task value and perceived competency. Schizophrenia Bulletin. 2010;36:957–965. doi: 10.1093/schbul/sbq078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen CI, Cohen GD, Blank K, Gaitz C, Katz IR, Leuchter A, Maletta G, Meyers B, Sakauye K, Shamoian C. Schizophrenia and older adults: An overview: Directions for research and policy. American Journal of Geriatric Psychiatry. 2000;8:19–28. doi: 10.1097/00019442-200002000-00003. [DOI] [PubMed] [Google Scholar]
- Conley RR. The burden of depressive symptoms in people with schizophrenia. Psychiatr Clin North Am. 2009;32:853–861. doi: 10.1016/j.psc.2009.09.001. [DOI] [PubMed] [Google Scholar]
- Conley RR, Ascher-Svanum H, Zhu B, Faries DE, Kinon BJ. The burden of depressive symptoms in the long-term treatment of patients with schizophrenia. Schizophrenia Research. 2007;90:186–197. doi: 10.1016/j.schres.2006.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon LB, Dickerson F, Bellack AS, Bennett M, Dickinson D, Goldberg RW, Lehman A, Tenhula WN, Calmes C, Pasillas RM, Peer J, Kreyenbuhl J. The 2009 schizophrenia PORT psychosocial treatment recommendations and summary statements. Schizophrenia Bulletin. 2010;36:48–70. doi: 10.1093/schbul/sbp115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eccles JS, Wigfield A. Motivational beliefs, values, and goals. Annu Rev Psychol. 2002;53:109–132. doi: 10.1146/annurev.psych.53.100901.135153. [DOI] [PubMed] [Google Scholar]
- Fett AK, Viechtbauer W, Dominguez MD, Penn DL, van Os J, Krabbendam L. The relationship between neurocognition and social cognition with functional outcomes in schizophrenia: A meta-analysis. Neuroscience and Biobehavioral Reviews. 2011;35:573–588. doi: 10.1016/j.neubiorev.2010.07.001. [DOI] [PubMed] [Google Scholar]
- Fishbein M, Ajzen I. Beliefs, attitudes, intention, and behavior. John Wiley; New York: 1975. [Google Scholar]
- Francis JJ, Eccles MP, Johnston M, Walker A, Grimshaw J, Foy R, Kaner EFS, Smith L, Bonetti D. Constructing questionnaires based on the Theory of Planned Behaviour: A manual for health services researchers. Center for Health Services Research, University of Newcastle; Newcastle upon Tyne: 2004. [Google Scholar]
- Glynn SM, Marder SR, Liberman RP, Blair K, Wirshing WC, Wirshing DA, Ross D, Mintz J. Supplementing clinic-based skills training with manual-based community support sessions: effects on social adjustment of patients with schizophrenia. Am J Psychiatry. 2002;159:829–837. doi: 10.1176/appi.ajp.159.5.829. [DOI] [PubMed] [Google Scholar]
- Godin G, Kok G. The theory of planned behavior: A review of its applications to health-related behaviors. American Journal of Health Promotion. 1996;11:87–98. doi: 10.4278/0890-1171-11.2.87. [DOI] [PubMed] [Google Scholar]
- Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? American Journal of Psychiatry. 1996;153:321–330. doi: 10.1176/ajp.153.3.321. [DOI] [PubMed] [Google Scholar]
- Green MF. Cognitive impairment and functional outcome in schizophrenia and bipolar disorder. J Clin Psychiatry. 2006;67:e12. [PubMed] [Google Scholar]
- Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: Are we measuring the “right stuff”? Schizophrenia Bulletin. 2000;26:119–136. doi: 10.1093/oxfordjournals.schbul.a033430. [DOI] [PubMed] [Google Scholar]
- Gupta M, Bassett E, Iftene F, Bowie CR. Functional outcomes in schizophrenia: Understanding the competence-performance discrepancy. Journal of Psychiatric Research. 2012;46:205–211. doi: 10.1016/j.jpsychires.2011.09.002. [DOI] [PubMed] [Google Scholar]
- Hardeman W, Johnston M, Johnston DW, Bonetti D, Wareham NJ, Kinmonth AL. Application of the Theory of Planned Behaviour in behaviour change interventions: A systematic review. Psychology & Health. 2002;17:123–158. [Google Scholar]
- Kay SR, Fiszbein A, Opler LA. The Positive And Negative Syndrome Scale (PANSS) for schizophrenia. Schizophrenia Bulletin. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Kopelowicz A, Wallace CJ, Liberman RP, Aguirre F, Zarate R, Mintz J. The use of the Theory of Planned Behavior to predict medication adherence in schizophrenia. Clinical Schizophrenia & Related Psychoses. 2007;1:227–242. [Google Scholar]
- Kopelowicz A, Zarate R, Gonzalez Smith V, Mintz J, Liberman RP. Disease management in Latinos with schizophrenia: a family-assisted, skills training approach. Schizophr Bull. 2003;29:211–227. doi: 10.1093/oxfordjournals.schbul.a006999. [DOI] [PubMed] [Google Scholar]
- Leifker FR, Bowie CR, Harvey PD. Determinants of everyday outcomes in schizophrenia: the influences of cognitive impairment, functional capacity, and symptoms. Schizophrenia Research. 2009;115:82–87. doi: 10.1016/j.schres.2009.09.004. [DOI] [PubMed] [Google Scholar]
- Mausbach BT, Bowie CR, Harvey PD, Twamley EW, Goldman SR, Jeste DV, Patterson TL. Usefulness of the UCSD Performance-based Skills Assessment (UPSA) for predicting residential independence in patients with chronic schizophrenia. Journal of Psychiatric Research. 2008a;42:320–327. doi: 10.1016/j.jpsychires.2006.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mausbach BT, Depp CA, Cardenas V, Jeste DV, Patterson TL. Relationship between functional capacity and community responsibility in patients with schizophrenia: Differences between independent and assisted living settings. Commun Ment Health J. 2008b;44:385–391. doi: 10.1007/s10597-008-9141-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mausbach BT, Moore R, Bowie C, Cardenas V, Patterson TL. A review of instruments for measuring functional recovery in those diagnosed with psychosis. Schizophrenia Bulletin. 2009;35:307–318. doi: 10.1093/schbul/sbn152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEachan RRC, Conner M, Taylor NJ, Lawton RJ. Prospective prediction of health-related behaviours with the Theory of Planned Behaviour: a meta-analysis. Health Psychology Review. 2011;5:97–144. [Google Scholar]
- Palmer BW, Heaton SC, Jeste DV. Older patients with schizophrenia: challenges in the coming decades. Psychiatric Services. 1999;50:1178–1183. doi: 10.1176/ps.50.9.1178. [DOI] [PubMed] [Google Scholar]
- Patterson TL, Goldman S, McKibbin CL, Hughs T, Jeste DV. UCSD Performance-based Skills Assessment: Development of a new measure of everyday functioning for severely mentally ill adults. Schizophrenia Bulletin. 2001;27:235–245. doi: 10.1093/oxfordjournals.schbul.a006870. [DOI] [PubMed] [Google Scholar]
- Randall DM, Wolff JA. The time interval in the intention-behaviour relationship: Meta-analysis. British Journal of Social Psychology. 1994;33:405–418. [Google Scholar]
- Sabbag S, Twamley EM, Vella L, Heaton RK, Patterson TL, Harvey PD. Assessing everyday functioning in schizophrenia: not all informants seem equally informative. Schizophr Res. 2011;131:250–255. doi: 10.1016/j.schres.2011.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabbag S, Twamley EW, Vella L, Heaton RK, Patterson TL, Harvey PD. Predictors of the accuracy of self assessment of everyday functioning in people with schizophrenia. Schizophrenia Research. 2012;137:190–195. doi: 10.1016/j.schres.2012.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheeran P. Intention-behavior relations: A conceptual and empirical review. European Review of Social Psychology. 2002;21:1–36. [Google Scholar]
- Sheeran P, Orbell S. Do intentions predict condom use? Meta-analysis and examination of six moderator variables. British Journal of Social Psychology. 1998;37:231–250. doi: 10.1111/j.2044-8309.1998.tb01167.x. [DOI] [PubMed] [Google Scholar]
- Slade E, Salkever D. Symptom effects on employment in a structural model of mental illness and treatment: Analysis of patients with schizophrenia. The Journal of Mental Health Policy and Economics. 2001;4:25–34. [PubMed] [Google Scholar]
- Sparks P, Guthrie CA. Self-Identity and the Theory of Planned Behavior: A Useful Addition or an Unhelpful Artifice?1. Journal of Applied Social Psychology. 1998;28:1393–1410. [Google Scholar]
- Terry DJ, Hogg MA, White KM. The theory of planned behaviour: Self-identity, social identity and group norms. British Journal of Social Psychology. 1999;38:225–244. doi: 10.1348/014466699164149. [DOI] [PubMed] [Google Scholar]
- Twamley EW, Doshi RR, Nayak GV, Palmer BW, Golshan S, Heaton RK, Patterson TL, Jeste DV. Generalized cognitive impairments, ability to perform everyday tasks, and level of independence in community living situations of older patients with psychosis. Am J Psychiatry. 2002;159:2013–2020. doi: 10.1176/appi.ajp.159.12.2013. [DOI] [PubMed] [Google Scholar]
- Wu EQ, Birnbaum HG, Shi L, Ball DE, Kessler RC, Moulis M, Aggarwal J. The Economic Burden of Schizophrenia in the United States in 2002. Journal of Clinical Psychiatry. 2005;66:1122–1129. doi: 10.4088/jcp.v66n0906. [DOI] [PubMed] [Google Scholar]