Abstract
Objective
To examine the effect of census caps and unit-based admissions on resident workload, conference attendance, duty hour compliance, and patient safety.
Participants and Methods
We implemented a census cap of 14 patients on 6 Mayo Clinic internal medicine resident hospital services and a unit-based admissions process in which patients and care teams were consolidated within hospital units. All 280 residents and 15,926 patient admissions to resident and nonresident services 1 year before the intervention (September 1, 2006, through August 31, 2007) and 1 year after the intervention (May 1, 2008, through April 30, 2009) were included. Residents' workload, conference attendance, and duty hours were tracked electronically. Patient safety variables including Rapid Response Team and cardiopulmonary resuscitation events, intensive care unit transfers, Patient Safety Indicators, and 30-day readmissions were compared preintervention and postintervention.
Results
After the intervention, residents' mean (SE) ratings of workload appropriateness improved (3.10 [0.08] vs 3.87 [0.08] on a 5-point scale; P<.001), as did conference attendance (1523 [56. 8%] vs 1700 [63.5%] conferences attended; P<.001). Duty hour violations for working more than 30 consecutive hours and not having 10 hours off between duty periods decreased from 77 of 9490 possible violations (0.81%) to 27 (0.28%) and from 70 (0.74%) to 14 (0.15%) violations, respectively (both, P<.001). Thirty-day readmissions to resident services decreased (1010 [18.14%] vs 682 [15. 37%]; P<.001). All other patient safety measures remained unchanged. After adjustment for illness severity, there were no significant differences in patient outcomes between resident and nonresident services.
Conclusion
Census caps and unit-based admissions were associated with improvements in resident workload, conference attendance, duty hour compliance, and readmission rates while patient outcomes were maintained.
Abbreviations and Acronyms: CPR, cardiopulmonary resuscitation; ICU, intensive care unit; RRT, Rapid Response Team
In efforts to decrease resident fatigue and enhance patient safety, much attention has focused on reducing residents' duty hours.1,2 Far less consideration has been given to determining the optimal workload for residents to achieve the best learning and provide safe patient care. However, simply compressing a fixed amount of work into fewer hours may adversely impact residents' education3,4 and may not decrease resident fatigue.5,6 As duty hours are further reduced,2,7 residency programs must ensure that residents' workload is appropriately managed to optimize education and patient safety.
High resident workload has been associated with less sleep while on call, decreased participation in educational activities.8 increased medical errors,9 and higher patient mortality.10 In contrast, reducing workload has been shown to enhance resident satisfaction, increase time for teaching, and improve the quality of residents' discharge summaries.11,12
Inpatient volume (census) for individual residents and the resident team is a major component of residents' workload.13 However, other factors, in addition to patient volume, also contribute to workload.13-16 One such factor is work efficiency, which includes time spent on indirect patient care tasks (eg, placing orders, obtaining test results, documentation) and transit (eg, traveling to and from various hospital units).17-19 Residents taking care of a group of patients who are geographically dispersed throughout hospitals experience inefficiencies related to physical travel between hospital units as well as potential differences in processes and systems of care across units.17,20,21
Recognizing the potential risks associated with high resident workload, we sought to reduce residents' workload by implementing a maximum patient census (ie, census “cap”) of 14 patients on the 6 internal medicine resident hospital services at Mayo Clinic. In addition, to increase work efficiency, we developed a unit-based admissions process in which patients and their multidisciplinary care team were geographically consolidated on a single hospital unit. The aim of this study was to examine the effect of these 2 interventions on residents' perceptions of their workload and education, residents' educational conference attendance, duty hour compliance, and patient safety.
Participants and Methods
Study Design
We conducted a prospective, controlled intervention of the effect of resident service census caps and unit-based admissions on residents' workload, conference attendance, duty hour compliance, and patient safety at Mayo Clinic in Rochester, MN. All 280 residents on 6 internal medicine resident services and all 15,926 patient hospital admissions to the 6 resident and 4 nonresident hospital services 1 year before the intervention (September 1, 2006, through August 31, 2007) and 1 year after the intervention (May 1, 2008, through April 30, 2009) were included. This study was approved by the Mayo Clinic Institutional Review Board.
Resident and Nonresident Hospital Services
During the study period, there were 10 general internal medicine hospital services at Mayo Clinic in Rochester, MN. Six of these were resident services composed of one attending physician, one senior resident, and 3 interns. The remaining 4 services were nonresident services staffed by hospitalists and nurse practitioners. Before the intervention, residents admitted patients to resident services until individual admission maximums were reached, according to existing accreditation requirements.22 Remaining patients were admitted by hospitalists and nurse practitioners to nonresident services. Additionally, there was no dedicated process in place to admit general internal medicine patients to specific hospital units; thus, before the intervention, medical patients were admitted to various units throughout the hospital on the basis of bed availability rather than service assignment. Before the intervention, patients were not triaged to resident or nonresident services on the basis of illness severity.
Intervention
To reduce residents' workload and enhance their ability to attend educational conferences and meet duty hour standards, we implemented a 2-part intervention. First, we initiated a service census cap of 14 patients on each of the 6 general internal medicine resident hospital services. Of note, the Accreditation Council for Graduate Medical Education does not specify a census cap; rather, service census caps are determined by the residents who make up the services. In the most conservative estimate of these requirements, there would be a maximum of 20 patients per team.23 In our intervention, once resident services reached a census of 14 patients, additional patients requiring hospitalization were admitted to nonresident services. Patients perceived to have higher illness severity were preferentially admitted to resident services, and postprocedure and observation patients were preferentially admitted to nonresident services.
Second, we developed a unit-based admissions process in which general internal medicine patients and their resident care team were geographically consolidated on a single hospital unit. Each of the 6 resident services was assigned to a specific hospital unit, and patients admitted to these resident services were assigned to rooms on the corresponding unit; therefore, residents, attending physicians, nurses, allied health professionals, and patients for a given hospital service were all located in the same place.
The intervention was phased in over a period of 9 months from September 1, 2007, through April 30, 2008. The 1-year preintervention period was defined as September 1, 2006, through August 31, 2007, and the 1-year postintervention period was defined as May 1, 2008, through April 30, 2009.
Outcome Measures
The extent to which resident service census caps were successfully implemented was assessed using the maximum midnight patient census (defined as the total number of patients on the resident service at midnight) on each of the 6 resident services. The degree to which admitted patients were successfully located on the home unit of their resident service was examined using the percentage of all admissions located on the appropriate hospital unit.
Residents' perceptions of their workload and education were measured using an electronic survey administered at the end of each residency ward rotation. Survey items were structured on 5-point scales (1 = needs improvement, 3 = average, 5 = top 10% of all rotations). Residents rated the appropriateness of their workload by responding to the following item: “The census/caseload was appropriate to ensure quality patient care and education.” Since one potential consequence of reducing workload may be decreased exposure to an adequate range of patients and diseases, we examined residents' responses to the items “I had the opportunity to manage a wide range of pathology in this specialty” and “I had the opportunity and guidance to develop skills.” Additionally, residents rated the quality of their educational experience overall using the following items: “The rotation conferences were valuable” and “The rotation was a valuable learning experience.”
Residents' conference attendance was recorded daily for each required educational conference using an electronic card-swipe system. Conference attendance was reported as the percentage of total conferences attended. The total number of conferences that residents were expected to attend was adjusted for duty period and days off such that residents were only considered “absent” from a conference if they did not attend a conference that was scheduled during their assigned duty period. Residents were not considered absent from a conference if the conference occurred during their days off or designated rest periods.
Compliance with duty hour standards was measured by residents' self-reporting via monthly electronic surveys at the end of each rotation. Residents were asked to report the number of times during the rotation that they violated the following duty hour standards22: (1) working 30 consecutive hours or less (24 hours per clinical duty period plus 6 hours for patient handoff and education), (2) obtaining 10 hours or more off between duty periods, (3) working 80 hours or less per week averaged over a 4-week period, and (4) obtaining 1 in 7 days off averaged over a 4-week period.
Patient safety outcomes determined for all patients included: (1) Rapid Response Team (RRT) events, defined as the number of patients who required one or more emergency consultations from the hospital RRT; (2) cardiopulmonary resuscitation (CPR) events, defined as the number of patients who required emergency CPR one or more times; (3) intensive care unit (ICU) transfers, defined as the number of patients who required one or more transfers from the medical ward to an ICU; (4) Patient Safety Indicators (PSIs), defined as the number of patients experiencing one or more of the 20 indicators from Agency for Healthcare Research and Quality Patient Safety Indicators24 version 3.2, modified to exclude conditions present on admission; and (5) 30-day readmissions, defined as the number of patients dismissed from the hospital who required readmission to the same hospital within 30 days of dismissal.
Data Analyses
Changes in residents' workload, conference attendance, and duty hour compliance were compared between the preintervention and postintervention time periods using mixed linear regression models or Fisher exact tests with continuity correction as appropriate.
To compare changes in patient outcomes between the resident and nonresident services before and after the intervention, a difference-in-difference analysis was performed. This allowed us to examine if the direction and scale of the changes in outcomes differed between the 2 types of services from the before to after time periods. The difference-in-difference models were fit for each of the patient safety variables, including RRT and CPR events, ICU transfers, PSIs, and 30-day readmissions. Since patients with greater illness severity were preferentially admitted to resident services in the postintervention period, models were adjusted for anticipated differences in illness severity and patient complexity using University Health System Consortium expected mortality and expected length of stay.25 To account for multiple comparisons, a significance level of 0.01 was used. All calculations were performed using SAS statistical software (version 9.1; SAS Institute Inc, Cary, NC).
Results
Census Caps and Unit-Based Admissions
A total of 15,926 patient admissions were performed by resident and nonresident services during the study period. The resident services performed 5567 patient admissions during the preintervention period and 4436 admissions during the postintervention period, whereas the nonresident services performed 2315 patient admissions before the intervention compared with 3608 admissions during the postintervention period.
The Figure shows the maximum midnight patient census among the 6 resident services during the study period. Before the intervention, the maximum midnight census on any one of the 6 resident services ranged from 8 to 19 patients, whereas the maximum census ranged from 8 to 14 patients after the intervention. None of the 6 resident services exceeded the census cap of 14 patients during the postintervention period. The mean (SD) midnight census across the 6 resident services was 9.4 (3.1) in the preintervention and 9.1 (2.2) in the postintervention period.
FIGURE.
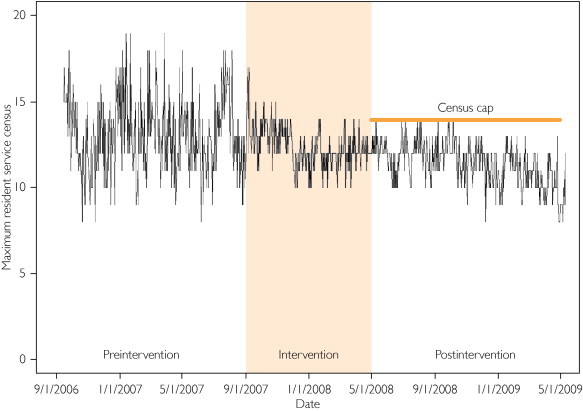
Maximum patient census among 6 internal medicine resident services recorded daily at midnight. No services exceeded the census cap of 14 patients per resident service in the postintervention period.
The number of patients on resident services who were admitted to their home unit increased from 3887 (69.8%) unit-based admissions before the intervention to 4053 (91.4%) unit-based admissions after the intervention (P<.001). Because both resident and nonresident services admit patients from the same larger population of general internal medicine patients seen at Mayo Clinic, the number of unit-based admissions to nonresident services also increased after intervention.
Resident Workload, Education, and Conference Attendance
After the intervention, residents' perceptions of the appropriateness of their workload improved from a mean (SE) of 3.10 (0.08) to 3.87 (0.08) on the 5-point scale (P<.001) (Table 1). According to the previously established 0.01 threshold of significance for this study, there were no statistically significant changes in residents' perceptions of their opportunities for managing a wide range of pathology (P=.05) and opportunities for developing skills (P=.06) before compared with after the intervention. Residents' ratings of the value of the rotation conferences (P=.04) and learning experience overall (P=.27) remained high and unchanged after the intervention (Table 1).
TABLE 1.
Residents' Perceptions of Workload and Education Before and After Implementation of Census Caps and Unit-Based Admissions
| Preintervention, mean (SD)a | Postintervention, mean (SD)a | P valueb | |
|---|---|---|---|
| Census/caseload was appropriate | 3.10 (0.08) | 3.87 (0.08) | <.001 |
| Opportunity to manage diverse pathology | 3.85 (0.07) | 3.65 (0.05) | .05 |
| Opportunity and guidance to develop skills | 3.78 (0.06) | 3.80 (0.06) | .06 |
| Conferences were valuable | 3.62 (0.07) | 3.82 (0.04) | .04 |
| Rotation was a valuable learning experience | 3.86 (0.07) | 3.75 (0.27) | .27 |
Scale of 1 to 5: 1 = rotation needs improvement; 5 = top 10% of all rotations.
Mixed linear regression model accounting for possible repeated measures within participants.
Among the 280 residents, there were 5358 possible conferences to attend during the study period. Before the intervention, residents attended 1523 of 2679 possible conferences (56.8%), compared with 1700 of 2679 possible conferences (63.5%) after the intervention (P<.001).
Duty Hour Compliance
Table 2 shows the changes in the frequency of duty hour violations after compared with before the intervention. Among the 280 residents in the study, violations of the duty hour requirement to work no more than 30 consecutive hours (including 24 hours for clinical work plus 6 hours for patient handoff and education) decreased from 77 of 9490 possible violations (0.81%) before the intervention to 27 (0.28%) violations after the intervention (P<.001). Likewise, violations of the duty hour requirement to obtain 10 hours off between duty periods decreased from 70 of 9490 possible violations (0.74%) before the intervention to 14 (0.15%) after the intervention (P<.001). Violations of the duty hour requirements to work 80 hours or less per week (P=.13) and to have 1 in 7 days off (P=.99) were infrequent and remained statistically unchanged with the intervention (Table 2).
TABLE 2.
Duty Hour Violations Among 280 Residents Before and After Implementation of Census Caps and Unit-Based Admissions
| Preintervention violations (%) | Postintervention violations (%) | Relative riska | P valueb | |
|---|---|---|---|---|
| Working ≤30 consecutive hoursc | 77 (0.81) | 27 (0.28) | 0.35 | <.001 |
| Obtaining ≤10 hours off between duty periodsc | 70 (0.74) | 14 (0.15) | 0.20 | <.001 |
| Working ≥80 hours per weekd | 19 (6.09) | 10 (3.21) | 0.53 | .13 |
| Obtaining <1 in 7 days offd | 2 (0.64) | 1 (0.32) | 0.50 | .99 |
Risk of a violation in the postintervention period relative to the preintervention period.
Calculated using Fisher exact test with continuity correction.
Of 9490 possible violations among 280 residents.
Of 312 possible violations among 280 residents.
Patient Safety
Table 3 shows the difference-in-difference analysis of patient safety measures among resident and nonresident services before and after the intervention. The 30-day readmission rate significantly decreased on resident services, from 1010 (18.14%) readmissions preintervention to 682 (15.37%) postintervention (P<.0001). However, after adjusting for expected mortality and expected length of stay, the P value for the change in readmission rates was P=.04, which did not meet the statistical significance threshold set for this study (Table 3). The difference-in-difference analysis adjusted for expected mortality and expected length of stay also showed no differences in RRT events, CPR events, ICU transfers, and PSIs between resident and nonresident services before compared with after the intervention.
TABLE 3.
Patient Safety Measures Among 15,926 Patients on Resident and Nonresident Services Before and After Implementation of Census Caps and Unit-Based Admissions
| Variable | Service type | Preintervention, No. (%) | Postintervention, No. (%) | P value | Difference-in-difference adjusted P valuea |
|---|---|---|---|---|---|
| Rapid Response Team eventsb | Resident | 92 (1.65) | 94 (2.12) | .09 | .99 |
| Nonresident | 59 (2.55) | 81 (2.25) | .45 | ||
| Cardiopulmonary resuscitation eventsc | Resident | 30 (0.54) | 20 (0.45) | .54 | .19 |
| Nonresident | 8 (0.35) | 14 (0.39) | .79 | ||
| Intensive care unit transfersd | Resident | 260 (4.67) | 235 (5.30) | .15 | .88 |
| Nonresident | 113 (4.88) | 134 (3.71) | .03 | ||
| Patient Safety Indicatorse | Resident | 48 (0.86) | 38 (0.86) | .98 | .59 |
| Nonresident | 20 (0.86) | 16 (0.44) | .04 | ||
| Thirty-day readmissionsf | Resident | 1010 (18.14) | 682 (15.37) | <.0001 | .04 |
| Nonresident | 350 (15.12) | 508 (14.08) | .27 |
Adjusted for expected mortality and expected length of stay.
Number of patients who required emergency consultations from the hospital Rapid Response Team.
Number of patients who required emergency cardiopulmonary resuscitation one or more times.
Number of patients who required one or more transfers from the medical ward to an intensive care unit.
Number of patients who experienced one or more of the 20 indicators from Agency for Healthcare Research and Quality Patient Safety Indicators version 3.2, modified to exclude conditions present on admission.
Number of patients who required readmission to the same hospital within 30 days of dismissal.
Discussion
We sought to reduce resident workload and enhance education by implementing a census cap and a unit-based admissions process on internal medicine resident hospital services. This model led to enhanced resident satisfaction with their workload, improved conference attendance, and fewer duty hour violations while maintaining a high standard of patient safety on both resident and nonresident services.
It is noteworthy that in this study, implementation of a census cap did not decrease the average number of patients admitted by residents; however, the day-to-day variability in patient census substantially decreased. Thus, residents' overall exposure to patients was unchanged by the intervention, but residents experienced fewer extremes in patient volume (high and low) after implementation of a census cap. We hypothesize that greater stability in workload provided residents with a more predictable daily routine that allowed them to plan ahead to attend educational conferences and complete their work within duty hour limitations. Furthermore, after census variability was reduced, residents reported that their workload was more appropriate, but they did not perceive a decrease in their opportunities to manage patients and develop clinical skills. This finding underscores an important strength of this intervention, namely, successful workload reduction without a concomitant reduction in learning opportunities. Previous studies have shown declines in clinical and operative experience after duty hour reductions26-29; therefore, it is imperative that programs find ways to manage workload within duty hour limits without compromising learning.30 We present one model that appears to have extinguished census peaks, which have been shown to adversely impact education,8 while maintaining the breadth of clinical experience believed necessary to attain clinical competency.31
Improvements in conference attendance and duty hour compliance may also be explained by increased work efficiency attributable to the unit-based admissions process. After the intervention, more than 90% of patients were successfully admitted to the appropriate hospital unit, resulting in less time wasted on resident travel between units and enhanced work flow. The importance of maximizing efficiency is highlighted by the findings of work sampling studies showing that as much as 35% of residents' work on hospital wards is spent on activities of marginal or no educational value.17,18 Additionally, the burden of clerical work facing today's residents is exceedingly high.32 Unit-based admissions may be one potential approach to reducing inefficiency in residents' work. Future studies should explore other potential sources of inefficiency, including medical records, documentation, transfers of care, and discharge planning.
After adjustment for illness severity, there were no differences in any of the patient safety variables among patients hospitalized on resident and nonresident services after the intervention. Although the number of patients readmitted to resident services within 30 days of hospital dismissal significantly decreased after compared with before the intervention, this difference did not meet our threshold for statistical significance in the difference-in-difference model. Thus, census caps and unit-based admissions do not appear to have compromised patient safety.
This study has several limitations. First, this is a single-institution study; thus, generalizability has not been established. This model should be tested at other institutions to determine feasibility in other settings and reproducibility of outcomes. Second, our intervention had 2 components (census cap and unit-based admissions), and we are unable to determine the relative contribution of each individual component to the observed outcomes. However, this is a common feature of complex interventions implemented in actual clinical practice settings.33 Third, although this study is strengthened by the inclusion of a comparison group, which is often lacking in educational interventions,34 we acknowledge that the nonresident internal medicine hospital services were not a perfect comparator. Physicians on nonresident services do not have inpatient teaching obligations, which may allow them greater time to dedicate to patient care. Furthermore, because both resident and nonresident services admit patients from the same larger pool of medical patients requiring admission to Mayo Clinic, changes on one service may affect the other. In this study, as the percentage of unit-based admissions increased on the resident services, the percentage of unit-based admissions also increased on the nonresident services, though to a lesser extent. Fourth, resident duty hour violations and resident perception of workload were self-reported. Finally, we did not examine changes in objective measures of learning, such as performance on in-service examinations.
Conclusion
These limitations notwithstanding, this study describes a model for reducing residents' workload while enhancing conference attendance and duty hour compliance and maintaining patient safety. In this era of further duty hour reform, residency programs are seeking new and innovative ways to redesign their programs to maximize education while maintaining safe, high-quality patient care.35-38 This model, incorporating census caps and unit-based admissions, is one for residency programs to consider as they attempt to implement the new duty hour standards.
Acknowledgments
The internal funding source had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, and approval of the manuscript. Dr Reed had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the analysis.
Footnotes
For editorial comment, see page 311
Grant Support: Internal support was received through the Mayo Clinic Internal Medicine Residency Office of Educational Innovations as part of the Accreditation Council for Graduate Medical Education Educational Innovations Project.
Supplemental Online Material
Author Interview Video
References
- 1.Institute of Medicine . Resident Duty Hours: Enhancing Sleep, Supervision, and Safety. National Academies Press; Washington, DC: 2008. [PubMed] [Google Scholar]
- 2.Nasca T.J., Day S.H., Amis E.S., Jr, ACGME Duty Hour Task Force The new recommendations on duty hours from the ACGME Task Force. N Engl J Med. 2010;363(2):e3. doi: 10.1056/NEJMsb1005800. [DOI] [PubMed] [Google Scholar]
- 3.Lin G.A., Beck D.C., Stewart A.L., Garbutt J.M. Resident perceptions of the impact of work hour limitations. J Gen Intern Med. 2007;22(7):969–975. doi: 10.1007/s11606-007-0223-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vidyarthi A.R., Katz P.P., Wall S.D., Wachter R.M., Auerbach A.D. Impact of reduced duty hours on residents' educational satisfaction at the University of California, San Francisco. Acad Med. 2006;81(1):76–81. doi: 10.1097/00001888-200601000-00019. [DOI] [PubMed] [Google Scholar]
- 5.Friesen L.D., Vidyarthi A.R., Baron R.B., Katz P.P. Factors associated with intern fatigue. J Gen Intern Med. 2008;23(12):1981–1986. doi: 10.1007/s11606-008-0798-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Antiel R.A., Thompson S.M., Hafferty F.W. Duty hour recommendations and implications for meeting the ACGME core competencies: views of residency directors. Mayo Clin Proc. 2011;86(3):185–191. doi: 10.4065/mcp.2010.0635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Accreditation Council for Graduate Medical Education Approved Standards. http://acgme-2010standards.org/ Accessed August 23, 2011.
- 8.Arora V.M., Georgitis E., Siddique J. Association of workload of on-call medical interns with on-call sleep duration, shift duration, and participation in educational activities. JAMA. 2008;300(10):1146–1153. doi: 10.1001/jama.300.10.1146. [DOI] [PubMed] [Google Scholar]
- 9.Vidyarthi A.R., Auerbach A.D., Wachter R.M., Katz P.P. The impact of duty hours on resident self reports of errors. J Gen Intern Med. 2007;22(2):205–209. doi: 10.1007/s11606-006-0065-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ong M., Bostrom A., Vidyarthi A., McCulloch C., Auerbach A. House staff team workload and organization effects on patient outcomes in an academic general internal medicine inpatient service. Arch Intern Med. 2007;167(1):47–52. doi: 10.1001/archinte.167.1.47. [DOI] [PubMed] [Google Scholar]
- 11.McMahon G.T., Katz J.T., Thorndike M.E., Levy B.D., Loscalzo J. Evaluation of a redesign initiative in an internal-medicine residency. N Engl J Med. 2010;362(14):1304–1311. doi: 10.1056/NEJMsa0908136. [DOI] [PubMed] [Google Scholar]
- 12.Coit M.H., Katz J.T., McMahon G.T. The effect of workload reduction on the quality of residents' discharge summaries. J Gen Intern Med. 2011;26(1):28–32. doi: 10.1007/s11606-010-1465-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fletcher K.E., Reed D.A., Arora V.M. Doing the dirty work: measuring and optimizing resident workload. J Gen Intern Med. 2011;26(1):8–9. doi: 10.1007/s11606-010-1558-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fletcher K., Lamba A., Schapira M., Singh S. Development of an internal medicine workload intensity measure for hospital work. J Gen Intern Med. 2010;25(suppl 1):252–253. [Google Scholar]
- 15.Weinger M.B., Reddy S.B., Slagle J.M. Multiple measures of anesthesia workload during teaching and nonteaching cases. Anesth Analg. 2004;98(5):1419–1425. doi: 10.1213/01.ane.0000106838.66901.d2. [DOI] [PubMed] [Google Scholar]
- 16.Dellit T.H., Armas-Loughran B., Bosl G.J., Sepkowitz K.A., Thaler H., Blaskovich J. A method for assessing house staff workload as a function of length of stay. JAMA. 2001;286(9):1023–1024. doi: 10.1001/jama.286.9.1023. [DOI] [PubMed] [Google Scholar]
- 17.Dresselhaus T.R., Luck J., Wright B.C., Spragg R.G., Lee M.L., Bozzette S.A. Analyzing the time and value of housestaff inpatient work. J Gen Intern Med. 1998;13(8):534–540. doi: 10.1046/j.1525-1497.1998.00164.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boex J.R., Leahy P.J. Understanding residents' work: moving beyond counting hours to assessing educational value. Acad Med. 2003;78(9):939–944. doi: 10.1097/00001888-200309000-00022. [DOI] [PubMed] [Google Scholar]
- 19.Redding D.A., Robinson S. Interruptions and geographic challenges to nurses' cognitive workload. J Nurs Care Qual. 2009;24(3):194–200. doi: 10.1097/01.NCQ.0000356907.95076.31. [DOI] [PubMed] [Google Scholar]
- 20.Batsis J.A., Naessens J.M., Keegan M.T., Huddleston P.M., Wagie A.E., Huddleston J.M. Cost savings of hip arthroplasty patients on specialized orthopedic surgery units. Am J Orthop (Belle Mead NJ) 2009;38(1):E5–E11. [PubMed] [Google Scholar]
- 21.Gabow P.A., Karkhanis A., Knight A., Dixon P., Eisert S., Albert R.K. Observations of residents' work activities for 24 consecutive hours: implications for workflow redesign. Acad Med. 2006;81(8):766–775. doi: 10.1097/00001888-200608000-00016. [DOI] [PubMed] [Google Scholar]
- 22.Philibert I., Friedmann P., Williams W.T., ACGME Work Group on Resident Duty Hours New requirements for resident duty hours. JAMA. 2002;288(9):1112–1114. doi: 10.1001/jama.288.9.1112. [DOI] [PubMed] [Google Scholar]
- 23.Accreditation Council for Graduate Medical Education Internal Medicine Program Requirements. http://acgme.org/acWebsite/RRC_140/140_prIndex.asp Accessed November 17, 2011.
- 24.Agency for Healthcare Research and Quality; Rockville, MD: March 2008. Patient Safety Indicators Technical Specifications Version 3.2. [Google Scholar]
- 25.Meurer S. Mortality Measurement. Agency for Healthcare Research and Quality; Rockville, MD: February 2009. Mortality Risk Adjustment Methodology for University Health System's Clinical Data Base.http://www.ahrq.gov/qual/mortality/Meurer.htm Accessed August 23, 2011. [Google Scholar]
- 26.Carlin A.M., Gasevic E., Shepard A.D. Effect of the 80-hour work week on resident operative experience in general surgery. Am J Surg. 2007;193(3):326–329. doi: 10.1016/j.amjsurg.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 27.Damadi A., Davis A.T., Saxe A., Apelgren K. ACGME duty-hour restrictions decrease resident operative volume: a 5-year comparison at an ACGME-accredited university general surgery residency. J Surg Educ. 2007;64(5):256–259. doi: 10.1016/j.jsurg.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 28.Kairys J.C., McGuire K., Crawford A.G., Yeo C.J. Cumulative operative experience is decreasing during general surgery residency: a worrisome trend for surgical trainees? J Am Coll Surg. 2008;206(5):804–811. doi: 10.1016/j.jamcollsurg.2007.12.055. [DOI] [PubMed] [Google Scholar]
- 29.Weatherby B.A., Rudd J.N., Ervin T.B., Stafford P.R., Norris B.L. The effect of resident work hour regulations on orthopaedic surgical education. J Surg Orthop Adv. 2007;16(1):19–22. [PubMed] [Google Scholar]
- 30.Wayne D.B., Arora V.M. Duty hour reform and internal medicine residency training: no time to lose. J Gen Intern Med. 2009;24(10):1169–1170. doi: 10.1007/s11606-009-1093-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Green M.L., Aagaard E.M., Caverzagie K.J. Charting the road to competence: developmental milestones for internal medicine residency training. J Grade Med Educ. 2009;1(1):5–20. doi: 10.4300/01.01.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oxentenko A.S., West C.P., Popkave C., Weinberger S.E., Kolars J.C. Time spent on clinical documentation: a survey of internal medicine residents and program directors. Arch Intern Med. 2010;170(4):377–380. doi: 10.1001/archinternmed.2009.534. [DOI] [PubMed] [Google Scholar]
- 33.Medical Research Council Developing and evaluating complex interventions: new guidance. http://www.mrc.ac.uk/Utilities/Documentrecord/index.htm?d=MRC004871 Accessed August 23, 2011.
- 34.Reed D.A., Cook D.A., Beckman T.J., Levine R.B., Kern D.E., Wright S.M. Association between funding and quality of published medical education research. JAMA. 2007;298(9):1002–1009. doi: 10.1001/jama.298.9.1002. [DOI] [PubMed] [Google Scholar]
- 35.Crowley M.J., Barkauskas C.E., Srygley F.D. A comparative resident site visit project: a novel approach for implementing programmatic change in the duty hours era. Acad Med. 2010;85(7):1140–1146. doi: 10.1097/ACM.0b013e3181e18cee. [DOI] [PubMed] [Google Scholar]
- 36.Meyers F.J., Weinberger S.E., Fitzgibbons J.P., Glassroth J., Duffy F.D., Clayton C.P., Alliance for Academic Internal Medicine Education Redesign Task Force Redesigning residency training in internal medicine: the consensus report of the Alliance for Academic Internal Medicine Education Redesign Task Force. Acad Med. 2007;82(12):1211–1219. doi: 10.1097/ACM.0b013e318159d010. [DOI] [PubMed] [Google Scholar]
- 37.Weinberger S.E., Smith L.G., Collier V.U., Education Committee of the American College of Physicians Redesigning training for internal medicine. Ann Intern Med. 2006;144(12):927–932. doi: 10.7326/0003-4819-144-12-200606200-00124. [DOI] [PubMed] [Google Scholar]
- 38.Holmboe E.S., Bowen J.L., Green M. Reforming internal medicine residency training: a report from the Society of General Internal Medicine's task force for residency reform. J Gen Intern Med. 2005;20(12):1165–1172. doi: 10.1111/j.1525-1497.2005.0249.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Author Interview Video


