Abstract
A routine of regular exercise is highly effective for prevention and treatment of many common chronic diseases and improves cardiovascular (CV) health and longevity. However, long-term excessive endurance exercise may induce pathologic structural remodeling of the heart and large arteries. Emerging data suggest that chronic training for and competing in extreme endurance events such as marathons, ultramarathons, ironman distance triathlons, and very long distance bicycle races, can cause transient acute volume overload of the atria and right ventricle, with transient reductions in right ventricular ejection fraction and elevations of cardiac biomarkers, all of which return to normal within 1 week. Over months to years of repetitive injury, this process, in some individuals, may lead to patchy myocardial fibrosis, particularly in the atria, interventricular septum, and right ventricle, creating a substrate for atrial and ventricular arrhythmias. Additionally, long-term excessive sustained exercise may be associated with coronary artery calcification, diastolic dysfunction, and large-artery wall stiffening. However, this concept is still hypothetical and there is some inconsistency in the reported findings. Furthermore, lifelong vigorous exercisers generally have low mortality rates and excellent functional capacity. Notwithstanding, the hypothesis that long-term excessive endurance exercise may induce adverse CV remodeling warrants further investigation to identify at-risk individuals and formulate physical fitness regimens for conferring optimal CV health and longevity.
Abbreviations and Acronyms: CAC, coronary artery calcium; CHD, coronary heart disease; CV, cardiovascular; EF, ejection fraction; ET, exercise training; LV, left ventricular; MRI, magnetic resonance imaging; PA, physical activity; RA, right atrium; RV, right ventricular; SCD, sudden cardiac death; VA, ventricular arrhythmia
Regular exercise is one of the cornerstones of therapeutic lifestyle changes for producing optimal cardiovascular (CV) and overall health. Physical exercise, though not a drug, possesses many traits of a powerful pharmacological agent. A routine of daily physical activity (PA) stimulates a number of beneficial physiologic changes in the body and can be highly effective for prevention and treatment of many of our most prevalent and pernicious chronic diseases, including coronary heart disease (CHD), hypertension, heart failure, obesity, depression, and diabetes mellitus.1 People who exercise regularly have markedly lower rates of disability and a mean life expectancy that is 7 years longer than that of their physically inactive contemporaries.2,3 Accordingly, physicians are increasingly prescribing regular exercise training (ET) for their patients. The potential benefits of regular ET are listed in Table 1.4
TABLE 1.
Potential Benefits of Exercise Training
| Related to coronary heart disease risk factors |
| Increases serum high-density lipoprotein cholesterol levels |
| Reduces serum triglyceride and possibly low-density lipoprotein cholesterol levels |
| Reduces indices of obesity |
| Reduces arterial blood pressure |
| Improves insulin sensitivity and glucose levels |
| Improves endothelial function |
| Helps with smoking cessation efforts |
| Reduces psychological stress |
| Hematologic |
| Decreases hematocrit and blood viscosity |
| Expands blood plasma volume |
| Increases red blood cell deformability and tissue-level perfusion |
| Increases circulatory fibrinolytic activity |
| Other |
| Increases coronary flow reserve |
| Increases coronary collateral circulation |
| Increases tolerance of ischemia |
| Increases myocardial capillary density |
| Increases ventricular fibrillation thresholds |
| Reduces atherosclerosis |
| Possibly increases epicardial coronary artery size |
| Reduces major morbidity and mortality |
From Mayo Clin Proc.4
However, as with any pharmacological agent, a safe upper-dose limit potentially exists, beyond which the adverse effects (musculoskeletal trauma, metabolic derangements, CV stress, etc) of physical ET may outweigh its benefits. A very large recent study found that in sedentary individuals, even a modest dose of PA, as little as 15 minutes per day,5 confers substantial health benefits and that these benefits accrue in a dose-dependent fashion up to about an hour per day of vigorous PA, beyond which more ET does not yield further benefits (Figure 1).5,6 Similarly, a 15-year observational study of 52,000 adults found that runners had a 19% lower risk of all-cause mortality compared with nonrunners, with U-shaped mortality curves for distance, speed, and frequency. Running distances of about 1 to 20 miles per week, speeds of 6 to 7 miles per hour, and frequencies of 2 to 5 days per week were associated with lower all-cause mortality, whereas higher mileage, faster paces, and more frequent runs were not associated with better survival.7 A randomized crossover trial assigned 60 male patients with CHD to ET sessions of either 30 or 60 minutes. The 30-minute exercise sessions produced less oxidant stress and improved arterial elasticity, whereas 60-minute sessions worsened oxidant stress and increased vascular stiffness as measured by pulse wave velocity, mainly in older patients.8
FIGURE 1.
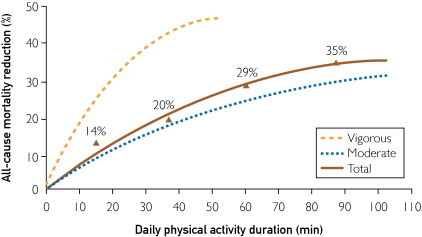
Relationship between dose of physical activity and reduction in all-cause mortality. The mortality benefits of exercise appear with even small amounts of daily exercise and peak at 50 to 60 minutes of vigorous exercise per day.
From Lancet,5 with permission.
Thus, the benefits of ET are attainable with comparatively modest levels of PA. Highly trained endurance athletes often perform strenuous aerobic exercise for several hours daily, often accumulating workloads of 200 to 300 metabolic equivalent hours (metabolic equivalents × hours) per week, which is approximately 5- to 10-fold greater than the standard ET dose recommended for prevention of CHD.1,9 The aim of this review is to explore the hypothesis that long-term excessive endurance ET in some individuals may induce adverse CV structural and electrical remodeling that might diminish some of the benefits conferred by more moderate intensities and durations of ET.
Sudden Cardiac Death and Endurance ET
Over the past 35 years, the number of Americans participating in a marathon annually has risen 20-fold; in 2010, an estimated half-million runners completed a marathon in the United States.10 Sudden cardiac death (SCD) among marathoners is very rare, with 1 event per 100,000 participants.6,7,11,12 Although that per-participant risk has not changed over the decades, absolute mortality rates have increased as the number of participants has risen. The final 1 mile of the marathon course represents less than 5% of the total distance of 26.2 miles yet accounts for almost 50% of the SCDs during the race.12,13
The fatality rate for triathlons is approximately twice that of marathons, largely because of increased CV events and drownings during the swim portion of the races.14 The incidence of SCD among collegiate athletes during competition is about 1 per 40,000 participants per year for all athletes.15 It is extremely important to keep in mind that the occurrence of SCD during marathons, triathlons, and collegiate athletic events is rare and should not deter individuals from participating in vigorous ET; the benefits of regular PA to the individual and to society as a whole far outweigh potential risks. At the same time, long-term training for and competing in extreme endurance events may predispose to CV issues that are not seen in more moderate forms of PA.
The causes of SCD during or after extreme exertion in individuals younger than 30 years most commonly include genetic causes such as hypertrophic cardiomyopathy, anomalous coronary arteries, dilated cardiomyopathy, and congenital long QT syndrome. In athletes older than 30 years, CHD and acute myocardial infarction16 and ischemia are the predominant causes of exercise-related SCD.17-23
Animal Studies
In an elegant animal model of excessive endurance ET, rats were trained (in part by prodding with electrical shocks to maintain high-intensity effort) to run strenuously and continuously for 60 minutes daily for 16 weeks, and then they were compared with control sedentary rats.8,24 The running rats developed hypertrophy of the left ventricle (LV) and the right ventricle (RV), diastolic dysfunction, and dilation of the left atria and the right atria (RA); they also showed increased collagen deposition and fibrosis in both the atria and ventricles (Figure 2). Ventricular tachycardia was inducible in 42% of the running rats vs only 6% of the sedentary rats (P=.05). Importantly, the fibrotic changes caused by 16 weeks of intensive ET had largely regressed to normal by 8 weeks after the daily running regimen ceased.
FIGURE 2.
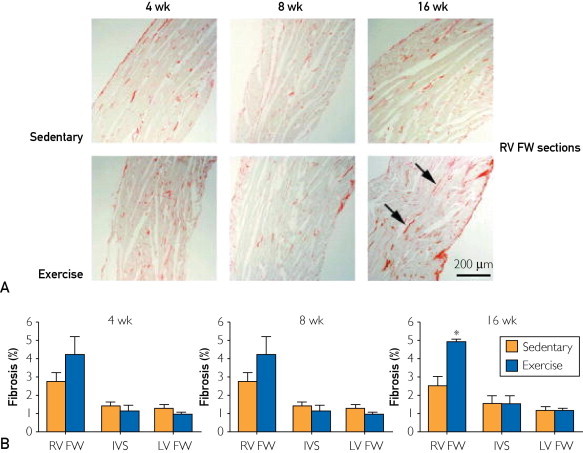
A, Picrosirius-stained photomicrographs of RV sections. By 16 weeks, the RVs of exercising rats show widespread interstitial collagen deposition with disarray of myocardial architecture (arrows). B, Mean ± standard error of the mean collagen content in RV FW, IVS, and LV FW. *P<.05 (exercising vs sedentary rats). FW = free wall; IVS = interventricular septum; LV = left ventricle; RV = right ventricle.
From Circulation,24 with permission.
This animal study found that daily excessive, strenuous, uninterrupted running replicated the adverse cardiac structural remodeling and proarrhythmia substrate noted in observational studies of extreme endurance athletes. These findings support the hypothesis that in some individuals, long-term strenuous daily endurance ET, such as marathon running or professional long-distance cycling, in some individuals may cause cardiac fibrosis (especially in the atria and the RV and interventricular septum), diastolic dysfunction, and increased susceptibility to atrial and ventricular arrhythmias. Many previous animal studies have also found acute, adverse cardiac effects of prolonged (up to 6 hours) endurance exercise, sometimes employing a rat model of cold-water swimming in which the animals were forced to swim to avoid drowning.25 These studies are of uncertain clinical relevance because of the excessively stressful nature of the imposed exercise.
Athlete's Heart
Chronic ET imposes increased hemodynamic demands that alter the loading conditions of the heart, particularly among athletes participating in sports requiring sustained elevations in cardiac work, such as long-distance running, rowing, swimming, and cycling.26 Highly trained individuals develop cardiac adaptations including enlarged LV and RV volumes, increased LV wall thickness and cardiac mass, and increased left atrial size.21-23 In the general population, these structural changes are associated with poor cardiac prognosis.27 However, these structural alterations, together with a preserved LV ejection fraction (EF), have been considered typical findings of the “athlete's heart.”18-20,28 Of concern, accumulating information suggests that some of the remodeling that occurs in endurance athletes may not be entirely benign.17,29-32 For example, in elite athletes, cardiac dimensions do not completely regress to normal levels even several years after the athlete has retired from competition and heavy ET.33
Biomarker Evidence for Cardiac Damage With Extreme Endurance ET
Running is a prototypical natural PA and often plays an integral and important role in an active, healthy lifestyle.9,34-36 However, uninterrupted very long distance running as is generally done while training for and participating in marathons and other extreme endurance events may produce adverse CV effects in susceptible individuals. Serologic markers of cardiac damage, including cardiac troponin, creatine kinase MB, and B-type natriuretic peptide, have been documented to increase in up to 50% of participants during and after marathon running7,10-14 (Figure 3).9,12,37-40 Additionally, transient renal dysfunction has been observed with extreme endurance ET efforts causing volume depletion and diminished renal filtration, with elevations in serum urea nitrogen, serum creatinine, and cystatin C.41 Increased levels of cardiac biomarkers including troponin after extreme ET endurance events, such as marathons, may reflect myocardial cell damage at the sites of myocyte slippage of one cell along another due to loss of integrity of desmosomal connections.15,42 However, the significance of the elevated cardiac biomarkers after endurance efforts remains uncertain, and it has been argued that these may be entirely benign transient increases resulting from CV adaptations to long-term ET.12,16,38,43
FIGURE 3.
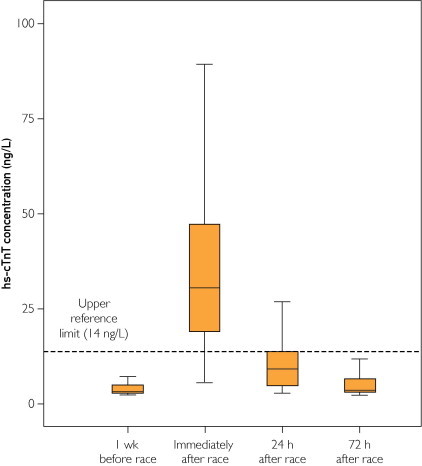
High-sensitivity cardiac troponin T (hs-cTnT) concentrations before, immediately after, and 24 and 72 hours after marathon race.
From Med Sci Sports Exerc,40 with permission.
Adverse Structural Remodeling
Accumulating evidence suggests that the adverse effects of both short-term intense PA and cumulative endurance exercise are most apparent in the right-sided cardiac chambers. Cardiac output at rest is approximately 5 L/min but typically increases 5-fold to about 25 L/min during vigorous ET.21 Long-term daily sessions of hours of continuous strenuous PA cause dilation of the RA and RV. During the postexercise period, the cardiac geometric dimensions are restored, but with this recurrent stretch of the chambers and reestablishment of the chamber geometry, some individuals may be prone to the development of chronic structural changes including chronic dilatation of the RV and RA with patchy myocardial scarring in response to the recurrent volume overload and excessive cardiac strain.17-19,29,44 These abnormalities are often asymptomatic and probably accrue over many years; they might predispose to serious arrhythmias such as atrial fibrillation and/or ventricular arrhythmias (VAs).
A prospective study of 25 runners (13 women and 12 men) found that running a marathon caused acute dilation of the RA and RV, with a sudden decrease in the RVEF.32 La Gerche et al45 studied a cohort of 40 highly trained aerobic athletes after competing in endurance events including marathon (mean time to completion, 3 hours), half-ironman triathlon (5.5 hours), full-ironman triathlon (11 hours), and alpine bicycle race (8 hours). They found that these intense endurance exercise efforts caused elevations in biomarkers of myocardial injury (troponin and B-type natriuretic peptide), which were correlated with reductions in RVEF (Figure 4), but not LVEF, on immediate (mean, 45 minutes) post-race echocardiography. The reductions in RVEF and the increases in RV volumes, which returned entirely to baseline within 1 week, were seen most often in races of longer durations (Figure 5). Of this cohort of endurance athletes, 5 (12.5%) had myocardial scarring as detected by focal gadolinium enhancement on cardiac magnetic resonance imaging (MRI) (Figure 6). The myocardial scarring and chronic RV remodeling were more common in athletes with the largest cumulative experience in competitive endurance events.45 In summary, this study suggests that intense endurance exercise induces acute RV dysfunction while largely sparing the LV. Even when short-term RV recovery appears complete, long-term training for and competing in extreme endurance exercise may lead to myocardial fibrosis and remodeling in a small subgroup.9,20,21,45
FIGURE 4.
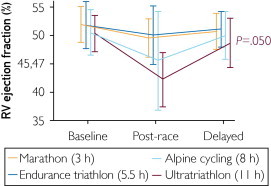
Duration-dependent effect of endurance events on right ventricular (RV) ejection fraction.
From Eur Heart J,45 with permission.
FIGURE 5.
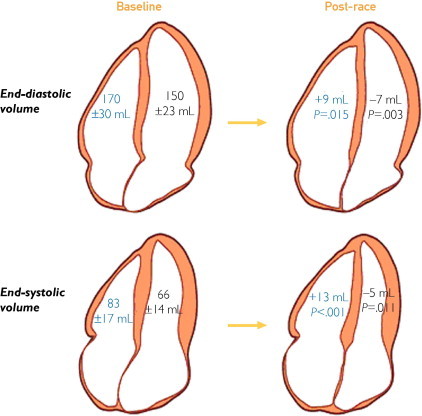
Differential effect of prolonged intense exercise on right and left ventricular volumes. Baseline volumes are shown on the left, and the changes in volume post-race are shown on the right. Right ventricular volumes increased in the post-race setting, whereas left ventricular volumes decreased, resulting in a decrease in right ventricular ejection fraction but not left ventricular ejection fraction.
From Eur Heart J,45 with permission.
FIGURE 6.
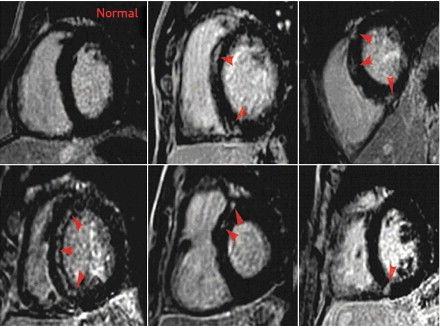
Delayed gadolinium enhancement in 5 athletes. Images of 5 athletes in whom focal delayed gadolinium enhancement was identified in the interventricular septum (arrows), compared with a normal study in an athlete (top left).
From Eur Heart J,45 with permission.
Ector et al29 reported that the decrease in RVEF is less significant in athletes with no symptoms of arrhythmia than in endurance athletes who have symptoms of arrhythmias, in whom the RV size increases and the RVEF is significantly lower. Another study of endurance athletes who have symptoms of VAs found that 50% of them had RV structural abnormalities by MRI.46 This RV dysfunction is likely induced by recurrent extreme and sustained high-level PA, with marked elevations in pulmonary artery pressures of up to 80 mm Hg in some athletes,9 which eventually may cause scattered areas of myocardial injury (as evidenced by the increases in troponin) with subsequent fibrotic scarring, typically in the RV and atria.17,22,23,29,31,32 These observations have led to speculation about the existence of a syndrome of exercise-induced arrhythmogenic RV cardiomyopathy that shares some features with the familial RV disease but is caused by chronic high-level endurance ET rather than a genetic predisposition.9
Another study using MRI to assess the effects of long-term very long distance running on myocardial structure31 comprised 102 ostensibly healthy male runners ranging in age from 50 to 72 years who had completed at least 5 marathons during the previous 3 years, compared with 102 age-matched controls.31 Approximately 12% of these apparently healthy marathon runners have evidence of patchy myocardial scarring, manifested as late gadolinium enhancement; this was 3-fold more common than in age-matched controls. Of additional concern, the CHD event rate during 2-year follow-up was significantly higher in the marathon runners than in controls (P<.0001).31 A similar smaller study found pathologic myocardial fibrosis by cardiac MRI in 6 of 12 asymptomatic men (50%) who were lifelong veteran endurance athletes, but no cases in younger endurance athletes and age-matched controls.24
Aortic stiffness and arterial pulse wave velocity, which are markers for adverse CV prognosis,47,48 may be increased in veteran ultraendurance athletes. A study of 47 individuals who trained extensively for and competed in marathons found that pulse wave velocity and aortic stiffness were significantly higher in the group of marathoners compared with controls.49 It is possible that the sustained shear stress caused by protracted endurance efforts eventually may induce fibrotic changes and decreases in arterial wall elasticity. Diastolic dysfunction of both the RV and LV has also been observed in individuals doing long-term extreme ET and racing.50,51
Coronary Artery Changes
Veteran endurance marathon runners in one study had coronary arteries that, at resting baseline, were similar in size to those of sedentary controls, but the marathoners had greater coronary artery dilating capacity.52 Mohlenkamp et al30 studied 108 middle-aged German long-term marathon runners and compared them with matched nonrunner controls. They observed a greater atherosclerotic burden in the marathoners as documented by higher coronary artery calcium (CAC) scores. Additionally, during follow-up the adverse CV event rates in the marathoners were equivalent to those in a population with established CHD.30 In a similar study, Schwartz et al53 reported on a US cohort of long-term marathon runners, defined as individuals who completed at least 25 marathons over the previous 25 years, and found higher than expected levels of CAC and calcified coronary plaque volume. That study, utilizing computed tomographic coronary angiography, found that the long-term marathoners had significantly more calcified plaque volume than sedentary controls (mean, 274 mm3 vs 169 mm3). In a case report, Goel et al54 observed a 49-year-old marathoner who had significant obstructions in all 3 major epicardial coronary arteries without associated risk factors and who generated protracted oxidative stress with prolonged running.
In another study of veteran endurance athletes, mean LV mass, as determined by MRI, was significantly greater in a group of marathon runners than in controls, and the increased LV mass correlated with higher CAC scores. Specifically, those marathoners with an LV mass greater than 150 g had a significantly higher CAC score than those with an LV mass less than 150 g.30 The investigators also found a mismatch between the risk factor profile and the amount CAC, particularly in the marathoners with an LV mass greater than 150 g.
Pathophysiology of Long-Term Extreme ET
Figure 7 shows the pathophysiology and possible adverse CV consequences (fibrosis, atrial arrhythmias, VAs, and SCD) associated with endurance ET and competition, such as marathon running. Individuals who do long-term ET and race over very long distances induce sustained (often for 1 to several hours daily) elevations in heart rate, blood pressure, cardiac output, and cardiac chamber volumes.9 Heavy and sustained ET generates large quantities of free radicals55 that likely outstrip the buffering capacity of the system, leaving these individuals susceptible to oxidative stress and transient cardiomyocyte dysfunction.45 This repetitive cycle may stimulate immune cells, including lymphocytes, macrophages, and mast cells, to secrete cytokines that signal the myofibroblasts to proliferate and secrete procollagen, which is then cross-linked to form mature collagen,41 eventually resulting in fibrosis deposited in patches in the myocardium and more diffusely in the large arteries.9,46
FIGURE 7.
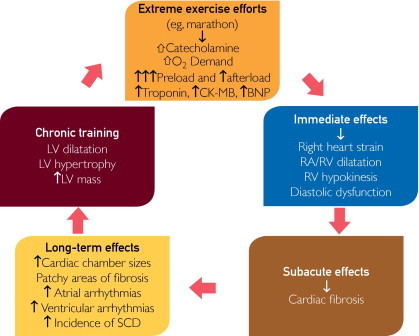
Proposed pathogenesis of cardiomyopathy in endurance athletes. BNP = B-type natriuretic peptide; CK-MB = creatine kinase MB; LV = left ventricle; RA = right atrium; RV = right ventricle; SCD = sudden cardiac death.
Proarrhythmic Effects of Excessive Endurance ET
Although it has been recognized that elite-level endurance athletes commonly have electrocardiographic abnormalities and atrial and ventricular ectopy,28,44,54 these functional adaptations traditionally have not been thought to predispose to serious arrhythmias or SCD. However, it appears that adverse cardiac remodeling induced by excessive ET can create an arrhythmogenic substrate, and rhythm abnormalities may be the most common CV problems encountered by veteran endurance athletes.29,31,54 Indeed, long-term sustained vigorous aerobic ET such as marathon or ultramarathon running or professional cycling has been associated with as much as a 5-fold increase in the prevalence of atrial fibrillation.19,30,31,37,55-63
Potential mechanisms underlying the association of long-term excessive exercise and atrial fibrillation are speculative but may include increased vagal and sympathetic tone, bradycardia, inflammatory changes, atrial wall fibrosis, and increased atrial size.59 Some data indicate that atrial size may be larger in veteran endurance athletes than in age-matched sedentary controls.64 Indeed, the left atrium may be enlarged in as many as 20% of competitive athletes, and this may be a predictor for atrial fibrillation.59,64
In addition, complex ventricular ectopy, including ventricular tachycardia and rarely SCD,11 occurs even in very fit individuals.12,29 Despite the fact that these studies generally excluded athletes with findings suggestive of familial arrhythmogenic RV dysplasia, the VAs typically originate from a mildly dysfunctional RV and/or the interventricular septum.20,29,46,65,66 The patchy myocardial fibrosis (fibrillary collagen deposition) that may develop as a reparative response to damaged myocardium can favor reentry, which is well established as a substrate for arrhythmia.29,51
Long-term extreme endurance ET and competition also stimulate multiple other disruptions, including episodic release of excessive catecholamines with resultant coronary vasoconstriction, chronic elevations of heart rate, changes in free fatty acid metabolism, lactic acidosis, and metabolic derangements.41
Risk Stratification For Endurance Athletes
Currently, we have no proven screening methods for detecting potential CV pathologic changes associated with extreme endurance ET. A logical strategy for now might be to deploy postcompetition cardiac biomarkers, echocardiography, and/or advanced imaging such as cardiac MRI to identify individuals at risk for and/or with subclinical adverse structural remodeling and substrate for arrhythmias, but the cost would likely be prohibitive.65 Computed tomography for CAC scoring may be useful, particularly for those older than 50 years who have been training extensively for and competing in extreme endurance events. Exercise testing generally has not been found to be helpful in screening extreme endurance athletes, nor has cost-effectiveness or clinical yield been found with the other testing described earlier.
An obligatory pattern of compulsive and excessive daily exercise has been described that may have adverse long-term mental and physical health consequences.67 A questionnaire developed to identify obligatory exercisers may be useful for screening veteran endurance athletes.68
Conclusion
In some individuals, long-term excessive endurance ET may cause adverse structural and electrical cardiac remodeling, including fibrosis and stiffening of the atria, RV, and large arteries. This theoretically might provide a substrate for atrial and ventricular arrhythmias and increase CV risk. Further investigation is warranted to identify the exercise threshold for potential toxicity, screening for at-risk individuals, and ideal ET regimens for optimizing CV health. For now, on the basis of animal and human data, CV benefits of vigorous aerobic ET appear to accrue in a dose-dependent fashion up to about 1 hour daily, beyond which further exertion produces diminishing returns and may even cause adverse CV effects in some individuals.
Consensus Guidelines for Physical Activity and Public Health from the American Heart Association and American College of Sports Medicine call for at least 150 minutes per week of moderate ET or 75 minutes per week of vigorous ET in the general adult population.1 Those guidelines also suggest that larger doses of ET may be necessary in some groups, such as those with or at risk for CHD (30 to 60 minutes daily), adults trying to prevent the transition to overweight or obesity (45 to 60 minutes per day), and formerly obese individuals trying to prevent weight regain (60 to 90 minutes per day). The guidelines also caution that high-intensity ET increases risk of musculoskeletal injuries and adverse CV events.1,42
Article Highlights.
-
■
People who exercise regularly have markedly lower rates of disability and a mean life expectancy that is 7 years longer than that of their physically inactive contemporaries. However, a safe upper-dose limit potentially exists, beyond which the adverse effects of exercise may outweigh its benefits.
-
■
Chronic intense and sustained exercise can cause patchy myocardial fibrosis, particularly in the atria, interventricular septum, and right ventricle, creating a substrate for atrial and ventricular arrhythmias.
-
■
Chronic excessive sustained exercise may also be associated with coronary artery calcification, diastolic dysfunction, and large-artery wall stiffening.
-
■
Veteran endurance athletes in sports such as marathon or ultramarathon running or professional cycling have been noted to have a 5-fold increase in the prevalence of atrial fibrillation.
-
■
Intense endurance exercise efforts often cause elevation in biomarkers of myocardial injury (troponin and B-type natriuretic peptide), which were correlated with transient reductions in right ventricular ejection fraction.
Supplemental Online Material
Author Interview Video
References
- 1.Haskell W.L., Lee I.M., Pate R.R. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1081–1093. doi: 10.1161/CIRCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- 2.Sarna S., Sahi T., Koskenvuo M., Kaprio J. Increased life expectancy of world class male athletes. Med Sci Sports Exerc. 1993;25(2):237–244. [PubMed] [Google Scholar]
- 3.Chakravarty E.F., Hubert H.B., Lingala V.B., Fries J.F. Reduced disability and mortality among aging runners: a 21-year longitudinal study. Arch Intern Med. 2008;168(15):1638–1646. doi: 10.1001/archinte.168.15.1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lavie C.J., Thomas R.J., Squires R.W., Allison T.G., Milani R.V. Exercise training and cardiac rehabilitation in primary and secondary prevention of coronary heart disease. Mayo Clin Proc. 2009;84(4):373–383. doi: 10.1016/S0025-6196(11)60548-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wen C.P., Wai J.P., Tsai M.K. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Lancet. 2011;378(9798):1244–1253. doi: 10.1016/S0140-6736(11)60749-6. [DOI] [PubMed] [Google Scholar]
- 6.O'Keefe J.H., Patil H.R., Lavie C.J. Exercise and life expectancy. Lancet. 2012;379(9818):799. doi: 10.1016/S0140-6736(12)60339-0. author reply 800-801. [DOI] [PubMed] [Google Scholar]
- 7.Lee J., Patte R., Lavie C.J., Blair S.N. Running and all-cause mortality risk: is more better? Med Sci Sports Exerc. 2012;44(6):990–994. [Google Scholar]
- 8.Michaelides A.P., Soulis D., Antoniades C. Exercise duration as a determinant of vascular function and antioxidant balance in patients with coronary artery disease. Heart. 2011;97(10):832–837. doi: 10.1136/hrt.2010.209080. [DOI] [PubMed] [Google Scholar]
- 9.Sharma S., Zaidi A. Exercise-induced arrhythmogenic right ventricular cardiomyopathy: fact or fallacy? Eur Heart J. 2012;33(8):938–940. doi: 10.1093/eurheartj/ehr436. [DOI] [PubMed] [Google Scholar]
- 10.USA Marathoning: 2007 Overview: MarathonGuide.com Web site. http://www.marathonguide.com/features/Articles/2007RecapOverview.cfm Accessed January 23, 2012.
- 11.Redelmeier D.A., Greenwald J.A. Competing risks of mortality with marathons: retrospective analysis. BMJ. 2007;335(7633):1275–1277. doi: 10.1136/bmj.39384.551539.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim J.H., Malhotra R., Chiampas G. Cardiac arrest during long-distance running races. N Engl J Med. 2012;366(2):130–140. doi: 10.1056/NEJMoa1106468. [DOI] [PubMed] [Google Scholar]
- 13.Sheppard M.N. The fittest person in the morgue? Histopathology. 2012;60(3):381–396. doi: 10.1111/j.1365-2559.2011.03852.x. [DOI] [PubMed] [Google Scholar]
- 14.Harris K.M., Henry J.T., Rohman E., Haas T.S., Maron B.J. Sudden death during the triathlon. JAMA. 2010;303(13):1255–1257. doi: 10.1001/jama.2010.368. [DOI] [PubMed] [Google Scholar]
- 15.Harmon K.G., Asif I.M., Klossner D., Drezner J.A. Incidence of sudden cardiac death in National Collegiate Athletic Association athletes. Circulation. 2011;123(15):1594–1600. doi: 10.1161/CIRCULATIONAHA.110.004622. [DOI] [PubMed] [Google Scholar]
- 16.Albano A.J., Thompson P.D., Kapur N.K. Acute coronary thrombosis in Boston marathon runners. N Engl J Med. 2012;366(2):184–185. doi: 10.1056/NEJMc1111015. [DOI] [PubMed] [Google Scholar]
- 17.Maron B.J., Pelliccia A., Spirito P. Cardiac disease in young trained athletes: insights into methods for distinguishing athlete's heart from structural heart disease, with particular emphasis on hypertrophic cardiomyopathy. Circulation. 1995;91(5):1596–1601. doi: 10.1161/01.cir.91.5.1596. [DOI] [PubMed] [Google Scholar]
- 18.Pluim B.M., Zwinderman A.H., van der Laarse A., van der Wall E.E. The athlete's heart: a meta-analysis of cardiac structure and function. Circulation. 2000;101(3):336–344. doi: 10.1161/01.cir.101.3.336. [DOI] [PubMed] [Google Scholar]
- 19.Maron B.J., Pelliccia A. The heart of trained athletes: cardiac remodeling and the risks of sports, including sudden death. Circulation. 2006;114(15):1633–1644. doi: 10.1161/CIRCULATIONAHA.106.613562. [DOI] [PubMed] [Google Scholar]
- 20.Spirito P., Pelliccia A., Proschan M.A. Morphology of the ”athlete's heart” assessed by echocardiography in 947 elite athletes representing 27 sports. Am J Cardiol. 1994;74(8):802–806. doi: 10.1016/0002-9149(94)90439-1. [DOI] [PubMed] [Google Scholar]
- 21.Pelliccia A., Culasso F., Di Paolo F.M., Maron B.J. Physiologic left ventricular cavity dilatation in elite athletes. Ann Intern Med. 1999;130(1):23–31. doi: 10.7326/0003-4819-130-1-199901050-00005. [DOI] [PubMed] [Google Scholar]
- 22.Pelliccia A., Maron B.J., Di Paolo F.M. Prevalence and clinical significance of left atrial remodeling in competitive athletes. J Am Coll Cardiol. 2005;46(4):690–696. doi: 10.1016/j.jacc.2005.04.052. [DOI] [PubMed] [Google Scholar]
- 23.Pelliccia A., Maron B.J., Spataro A., Proschan M.A., Spirito P. The upper limit of physiologic cardiac hypertrophy in highly trained elite athletes. N Engl J Med. 1991;324(5):295–301. doi: 10.1056/NEJM199101313240504. [DOI] [PubMed] [Google Scholar]
- 24.Benito B., Gay-Jordi G., Serrano-Mollar A. Cardiac arrhythmogenic remodeling in a rat model of long-term intensive exercise training. Circulation. 2011;123(1):13–22. doi: 10.1161/CIRCULATIONAHA.110.938282. [DOI] [PubMed] [Google Scholar]
- 25.Praphatsorna P., Thong-Ngama D., Kulaputanaa O., Klaikaewb N. Effects of intense exercise on biochemical and histological changes in rat liver and pancreas. Asian Biomedicine. 2010;4(4):619–625. [Google Scholar]
- 26.Middleton N., Shave R., George K. Altered left ventricular diastolic filling following a marathon is a reproducible phenomenon. Int J Cardiol. 2007;122(1):87–89. doi: 10.1016/j.ijcard.2006.11.042. [DOI] [PubMed] [Google Scholar]
- 27.Patel D.A., Lavie C.J., Milani R.V., Ventura H.O. Left atrial volume index predictive of mortality independent of left ventricular geometry in a large clinical cohort with preserved ejection fraction. Mayo Clin Proc. 2011;86(8):730–737. doi: 10.4065/mcp.2010.0682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maron B.J. Hypertrophic cardiomyopathy and other causes of sudden cardiac death in young competitive athletes, with considerations for preparticipation screening and criteria for disqualification. Cardiol Clin. 2007;25(3):399–414. doi: 10.1016/j.ccl.2007.07.006. vi. [DOI] [PubMed] [Google Scholar]
- 29.Ector J., Ganame J., van der Merwe N. Reduced right ventricular ejection fraction in endurance athletes presenting with ventricular arrhythmias: a quantitative angiographic assessment. Eur Heart J. 2007;28(3):345–353. doi: 10.1093/eurheartj/ehl468. [DOI] [PubMed] [Google Scholar]
- 30.Mohlenkamp S., Lehmann N., Breuckmann F. Running: the risk of coronary events; prevalence and prognostic relevance of coronary atherosclerosis in marathon runners. Eur Heart J. 2008;29(15):1903–1910. doi: 10.1093/eurheartj/ehn163. [DOI] [PubMed] [Google Scholar]
- 31.Breuckmann F., Mohlenkamp S., Nassenstein K. Myocardial late gadolinium enhancement: prevalence, pattern, and prognostic relevance in marathon runners. Radiology. 2009;251(1):50–57. doi: 10.1148/radiol.2511081118. [DOI] [PubMed] [Google Scholar]
- 32.Trivax J.E., Franklin B.A., Goldstein J.A. Acute cardiac effects of marathon running. J Appl Physiol. 2010;108(5):1148–1153. doi: 10.1152/japplphysiol.01151.2009. [DOI] [PubMed] [Google Scholar]
- 33.Pelliccia A., Maron B.J., De Luca R., Di Paolo F.M., Spataro A., Culasso F. Remodeling of left ventricular hypertrophy in elite athletes after long-term deconditioning. Circulation. 2002;105(8):944–949. doi: 10.1161/hc0802.104534. [DOI] [PubMed] [Google Scholar]
- 34.Seifi-Skishahr F., Siahkohian M., Nakhostin-Roohi B. Influence of aerobic exercise at high and moderate intensities on lipid peroxidation in untrained men. J Sports Med Phys Fitness. 2008;48(4):515–521. [PubMed] [Google Scholar]
- 35.O'Keefe J.H., Vogel R., Lavie C.J., Cordain L. Achieving hunter-gatherer fitness in the 21(st) century: back to the future. Am J Med. 2010;123(12):1082–1086. doi: 10.1016/j.amjmed.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 36.O'Keefe J.H., Vogel R., Lavie C.J., Cordain L. Exercise like a hunter-gatherer: a prescription for organic physical fitness. Prog Cardiovasc Dis. 2011;53(6):471–479. doi: 10.1016/j.pcad.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 37.Neilan T.G., Januzzi J.L., Lee-Lewandrowski E. Myocardial injury and ventricular dysfunction related to training levels among nonelite participants in the Boston marathon. Circulation. 2006;114(22):2325–2333. doi: 10.1161/CIRCULATIONAHA.106.647461. [DOI] [PubMed] [Google Scholar]
- 38.Shave R., Baggish A., George K. Exercise-induced cardiac troponin elevation: evidence, mechanisms, and implications. J Am Coll Cardiol. 2010;56(3):169–176. doi: 10.1016/j.jacc.2010.03.037. [DOI] [PubMed] [Google Scholar]
- 39.Neumayr G., Gaenzer H., Pfister R. Plasma levels of cardiac troponin I after prolonged strenuous endurance exercise. Am J Cardiol. 2001;87(3):369–371. doi: 10.1016/s0002-9149(00)01382-5. A310. [DOI] [PubMed] [Google Scholar]
- 40.Scherr J., Braun S., Schuster T. 72-h kinetics of high-sensitive troponin T and inflammatory markers after marathon. Med Sci Sports Exerc. 2011;43(10):1819–1827. doi: 10.1249/MSS.0b013e31821b12eb. [DOI] [PubMed] [Google Scholar]
- 41.McCullough P.A., Chinnaiyan K.M., Gallagher M.J. Changes in renal markers and acute kidney injury after marathon running. Nephrology. 2011;16(2):194–199. doi: 10.1111/j.1440-1797.2010.01354.x. [DOI] [PubMed] [Google Scholar]
- 42.La Gerche A., Robberecht C., Kuiperi C. Lower than expected desmosomal gene mutation prevalence in endurance athletes with complex ventricular arrhythmias of right ventricular origin. Heart. 2010;96(16):1268–1274. doi: 10.1136/hrt.2009.189621. [DOI] [PubMed] [Google Scholar]
- 43.Harper R.W. Exercise-induced troponin elevation: not necessarily a benign phenomenon. J Am Coll Cardiol. 2010;56(25):2145. doi: 10.1016/j.jacc.2010.08.618. author reply 2145-2146. [DOI] [PubMed] [Google Scholar]
- 44.Nassenstein K., Breuckmann F., Lehmann N. Left ventricular volumes and mass in marathon runners and their association with cardiovascular risk factors. Int J Cardiovasc Imaging. 2009;25(1):71–79. doi: 10.1007/s10554-008-9337-x. [DOI] [PubMed] [Google Scholar]
- 45.La Gerche A., Burns A.T., Mooney D.J. Exercise-induced right ventricular dysfunction and structural remodelling in endurance athletes. Eur Heart J. 2012;33(8):995–1006. doi: 10.1093/eurheartj/ehr397. [DOI] [PubMed] [Google Scholar]
- 46.Heidbuchel H., Hoogsteen J., Fagard R. High prevalence of right ventricular involvement in endurance athletes with ventricular arrhythmias: role of an electrophysiologic study in risk stratification. Eur Heart J. 2003;24(16):1473–1480. doi: 10.1016/s0195-668x(03)00282-3. [DOI] [PubMed] [Google Scholar]
- 47.Agabiti-Rosei E., Mancia G., O'Rourke M.F. Central blood pressure measurements and antihypertensive therapy: a consensus document. Hypertension. 2007;50(1):154–160. doi: 10.1161/HYPERTENSIONAHA.107.090068. [DOI] [PubMed] [Google Scholar]
- 48.Laurent S., Cockcroft J., Van Bortel L. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006;27(21):2588–2605. doi: 10.1093/eurheartj/ehl254. [DOI] [PubMed] [Google Scholar]
- 49.Vlachopoulos C., Kardara D., Anastasakis A. Arterial stiffness and wave reflections in marathon runners. Am J Hypertens. 2010;23(9):974–979. doi: 10.1038/ajh.2010.99. [DOI] [PubMed] [Google Scholar]
- 50.Wilson M., O'Hanlon R., Prasad S. Diverse patterns of myocardial fibrosis in lifelong, veteran endurance athletes. J Appl Physiol. 2011;110(6):1622–1626. doi: 10.1152/japplphysiol.01280.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Oxborough D., Birch K., Shave R., George K. ”Exercise-induced cardiac fatigue”: a review of the echocardiographic literature. Echocardiography. 2010;27(9):1130–1140. doi: 10.1111/j.1540-8175.2010.01251.x. [DOI] [PubMed] [Google Scholar]
- 52.Haskell W.L., Sims C., Myll J., Bortz W.M., St Goar F.G., Alderman E.L. Coronary artery size and dilating capacity in ultradistance runners. Circulation. 1993;87(4):1076–1082. doi: 10.1161/01.cir.87.4.1076. [DOI] [PubMed] [Google Scholar]
- 53.Schwartz J., Merkel-Kraus S., Duval S. 2010. Does elite athleticism enhance or inhibit coronary artery plaque formation?: Paper presented at: American College of Cardiology 2010 Scientific Sessions. Atlanta, GA. [Google Scholar]
- 54.Goel R., Majeed F., Vogel R. Exercise-induced hypertension, endothelial dysfunction, and coronary artery disease in a marathon runner. Am J Cardiol. 2007;99(5):743–744. doi: 10.1016/j.amjcard.2006.09.127. [DOI] [PubMed] [Google Scholar]
- 55.Vlachopoulos C., Aznaouridis K., Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol. 2010;55(13):1318–1327. doi: 10.1016/j.jacc.2009.10.061. [DOI] [PubMed] [Google Scholar]
- 56.Mont L., Elosua R., Brugada J. Endurance sport practice as a risk factor for atrial fibrillation and atrial flutter. Europace. 2009;11(1):11–17. doi: 10.1093/europace/eun289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Westrol M.S., Kapitanyan R., Marques-Baptista A., Merlin M.A. Causes of sudden cardiac arrest in young athletes. Postgrad Med. 2010;122(4):144–157. doi: 10.3810/pgm.2010.07.2181. [DOI] [PubMed] [Google Scholar]
- 58.Rector R.S., Rogers R., Ruebel M., Hinton P.S. Participation in road cycling vs running is associated with lower bone mineral density in men. Metabolism. 2008;57(2):226–232. doi: 10.1016/j.metabol.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 59.Mont L., Sambola A., Brugada J. Long-lasting sport practice and lone atrial fibrillation. Eur Heart J. 2002;23(6):477–482. doi: 10.1053/euhj.2001.2802. [DOI] [PubMed] [Google Scholar]
- 60.Elosua R., Arquer A., Mont L. Sport practice and the risk of lone atrial fibrillation: a case-control study [published correction appears in Int J Cardiol. 2007;123(1):74] Int J Cardiol. 2006;108(3):332–337. doi: 10.1016/j.ijcard.2005.05.020. [DOI] [PubMed] [Google Scholar]
- 61.Molina L., Mont L., Marrugat J. Long-term endurance sport practice increases the incidence of lone atrial fibrillation in men: a follow-up study. Europace. 2008;10(5):618–623. doi: 10.1093/europace/eun071. [DOI] [PubMed] [Google Scholar]
- 62.Mont L., Tamborero D., Elosua R. Physical activity, height, and left atrial size are independent risk factors for lone atrial fibrillation in middle-aged healthy individuals. Europace. 2008;10(1):15–20. doi: 10.1093/europace/eum263. [DOI] [PubMed] [Google Scholar]
- 63.Aizer A., Gaziano J.M., Cook N.R., Manson J.E., Buring J.E., Albert C.M. Relation of vigorous exercise to risk of atrial fibrillation. Am J Cardiol. 2009;103(11):1572–1577. doi: 10.1016/j.amjcard.2009.01.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kirchhof P., Lip G.Y., Van Gelder I.C. Comprehensive risk reduction in patients with atrial fibrillation: emerging diagnostic and therapeutic options—a report from the 3rd Atrial Fibrillation Competence NETwork/European Heart Rhythm Association consensus conference. Europace. 2012;14(1):8–27. doi: 10.1093/europace/eur241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Biffi A., Pelliccia A., Verdile L. Long-term clinical significance of frequent and complex ventricular tachyarrhythmias in trained athletes. J Am Coll Cardiol. 2002;40(3):446–452. doi: 10.1016/s0735-1097(02)01977-0. [DOI] [PubMed] [Google Scholar]
- 66.Burstein B., Nattel S. Atrial fibrosis: mechanisms and clinical relevance in atrial fibrillation. J Am Coll Cardiol. 2008;51(8):802–809. doi: 10.1016/j.jacc.2007.09.064. [DOI] [PubMed] [Google Scholar]
- 67.Wilson J.N., Markey C.N., Markey P.M. Fitness correlates of obligatory versus health motives for exercise: an examination of men in the military. Psychol Sport Exer. 2012;13(4):371–377. [Google Scholar]
- 68.Griffiths M.D., Szabo A., Terry A. The exercise addiction inventory: a quick and easy screening tool for health practitioners. Br J Sports Med. 2005;39(6):e30. doi: 10.1136/bjsm.2004.017020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Author Interview Video


