Abstract
The transmission of bacteria is more likely to occur from wet skin than from dry skin; therefore, the proper drying of hands after washing should be an integral part of the hand hygiene process in health care. This article systematically reviews the research on the hygienic efficacy of different hand-drying methods. A literature search was conducted in April 2011 using the electronic databases PubMed, Scopus, and Web of Science. Search terms used were hand dryer and hand drying. The search was limited to articles published in English from January 1970 through March 2011. Twelve studies were included in the review. Hand-drying effectiveness includes the speed of drying, degree of dryness, effective removal of bacteria, and prevention of cross-contamination. This review found little agreement regarding the relative effectiveness of electric air dryers. However, most studies suggest that paper towels can dry hands efficiently, remove bacteria effectively, and cause less contamination of the washroom environment. From a hygiene viewpoint, paper towels are superior to electric air dryers. Paper towels should be recommended in locations where hygiene is paramount, such as hospitals and clinics.
The 2009 human swine influenza A (H1N1) pandemic reminded health professionals and the community of the importance of hand hygiene to prevent the spread of diseases.1-8 The effectiveness of hand hygiene in infection control has been recognized since Semmelweis's observation in 1847 that the implementation of hand washing reduced the number of deaths among women with puerperal fever.9 For centuries, hand washing has been considered the most important measure to reduce the burden of health care–associated infection.10-12
Hand washing refers to washing hands with plain or antimicrobial soap and water.13 In actual practice, it can vary considerably from a brief rinse of the hands to extensive scrubbing. With adequate hand washing, significant reductions in the rates of infectious disease have been reported in a variety of settings, such as health care institutions,14,15 the food industry,16,17 child day care centers,18 schools,19-21 and all community and domestic situations.1,22,23 Until now, however, a great number of studies have focused on topics such as hand-washing techniques,24 selection and handling of hand-washing agents,25-27 and how to improve hand hygiene adherence for health care workers.28-31 Less is known about the role of hand drying after washing and the relative efficacy of different hand-drying methods in reducing contamination.
The proper drying of hands should be an essential component of effective hand hygiene procedures.11,13 Coates et al32 reported that washing hands with either soap and water or water alone combined with drying on paper towels can effectively remove bacteria from the hands. However, if hands are only shaken dry after washing, some bacteria are likely to remain. Patrick et al33 investigated the relationship between the amount of residual water left on the hands and bacterial translocation levels. The transmission of bacteria was more likely to occur from wet hands than from dry hands. Merry et al34 also confirmed the important role of residual water on the hands in the level of touch- or contact-associated contamination.
Although studies have reported the importance of thorough hand drying after washing, the role of hand drying has not been widely promoted, and its relevance to hand hygiene and infection control seems to have been overlooked.35 Lack of attention to this aspect may negate the benefits of careful hand washing in health care. So far, little research has been conducted to examine the contribution that proper hand drying makes to the overall effectiveness of hand hygiene practices. The purposes of this article are to provide a systematic review of research examining the performance of different hand-drying methods and make recommendations for future research.
Methods
An extensive literature search was conducted in April 2011, using the electronic databases PubMed, Scopus, and Web of Science. The search was limited to articles published in English from January 1970 through March 2011. The search terms used were hand dryer and hand drying.
Our goal was to analyze the hygienic efficacy of different hand-drying methods and then recommend the best hand-drying option for health care professionals. Two inclusion criteria were used to select articles. First, studies had to compare the hygiene performance of at least 2 hand-drying methods; studies solely focused on reporting the effectiveness of hand drying were excluded. Second, studies had to use an empirical research approach with quantitative outcomes; qualitative and review articles were excluded. We also excluded conference abstracts to focus on more substantial results. Two independent researchers (C.H. and W.M.) participated in all aspects of the review. They compared and discussed their findings with regard to inclusion and exclusion criteria. Disagreements were resolved by discussion with a third member of the team (S.S.).
Data extraction consisted of a 5-stage process (Figure). First, duplicate articles were identified and removed before analysis. Second, the title and abstract of remaining articles were screened for eligibility against the inclusion criteria. Third, full-text articles were retrieved and assessed according to their study design and scientific approach. Fourth, the references and citations of those articles identified were inspected to ensure that all relevant studies were included. Finally, a search of materials (gray literature) that fall outside the mainstream of published journal and monograph literature, such as government documents, conference proceedings, research reports, working papers, discussion papers, and newsletters, was conducted using the Google Scholar search engine.
FIGURE.
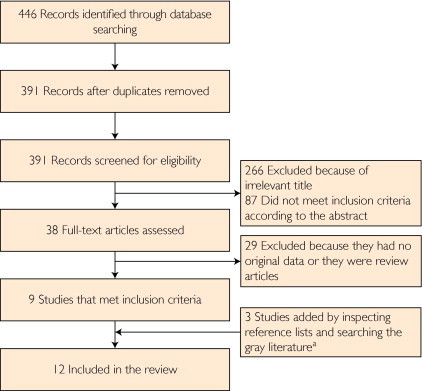
Flow diagram of literature search strategy.
aGovernment documents, conference proceedings, research reports, working papers, discussion papers, and newsletters.
All articles identified were critically reviewed by the authors and included as appropriate to provide an overview of the topic. The quality of this review was assessed using a critical appraisal framework. The authors used the Critical Appraisal Skills Programme checklist36 to ensure that the research question had been systematically identified, appraised, and summarized according to predetermined criteria.
Results
A total of 12 articles were included in the review. Paper towels, cloth towels, and hot air dryers are commonly used to dry washed hands. Hands can also dry by evaporation. Air dryers are electric devices used to dry hands, and they may operate either with a button or automatically with an infared sensor.37 In recent years, a new version of air dryer (ie, jet air dryer) has been introduced. According to the manufacturer, a jet air dryer is different from other conventional hot air dryers because it uses a jet of unheated air and incorporates an air filter.38 The hygienic efficacy of hand drying includes drying efficiency, the effective removal of bacteria, and the prevention of cross-contamination.39-41
Drying Efficiency
Patrick et al33 compared the drying efficiency of cloth towels and hot air dryers. The results indicated that residual water was more efficiently removed from the hands by cloth towels. After 10 seconds of drying with a single-serve cloth towel, the residual water on the hands was reduced to 4%. With 15 seconds of drying, the residual water was reduced to 1%. However, hot air dryers were much slower and took 45 seconds to reduce the residual water to 3%. Redway and Fawdar39 examined the drying efficiency of paper towels, hot air dryers, and jet air dryers. They found that paper towels and jet air dryers were almost equally efficient at drying hands. After 10 seconds of drying, both achieved 90% dryness. Hot air dryers took considerably longer and needed a drying time of 40 seconds to achieve a similar dryness.
In addition, Patrick et al33 conducted an observation study in male and female washrooms to determine the length of time that people spent drying their hands. Washrooms had either single-serve cloth towels or hot air dryer systems installed but not both. They found that male users spent an average of 3.5 seconds on cloth towels and 17 seconds under hot air dryers. The same figures for women were 5.2 and 13.3 seconds. They found that using a drying time of 5 seconds with cloth towels would achieve 85% dryness of the hands, but using 20 seconds of drying time under hot air dryers would achieve less than 70% dryness. Knights et al42 also reported that hot air dryers in normal use can only achieve 55% dryness of the hands for men and 68% dryness for women. In contrast, cloth towels and paper towels can generally achieve 90% or more dryness for both sexes.
Removal of Bacteria
Although the degree of wetness encourages the survival and transmission of bacteria on the hands, other factors also influence the hygiene performance of a hand-drying method. Redway and Fawdar39 assessed changes in the number of bacteria on the hands before and after the use of paper towels, hot air dryer, or jet air dryer. Finger pads were sampled by contact plates, and the palms were sampled by swabbing and inoculation of agar plates. They found that paper towels reduced the numbers of all types of bacteria on the hands. However, the hot air dryer increased all types of bacteria on the hands. The jet air dryer also increased most types of bacteria, but the increases were less than with the hot air dryer. In their study, a new hot air dryer and a new jet air dryer were used; hence, the authors claimed that any increases in bacterial numbers after the use of dryers must be due to factors other than the contamination of the dryers themselves.39 Hanna et al43 and Blackmore44 compared the number of bacteria remaining on hands after drying with paper towels, cloth towels, or hot air dryers. Bacteria samples were taken from the hands onto contact plates. The authors also reported that hot air dryers were the least effective method of removing bacteria from washed hands.
In contrast, another study reported that hot air dryers are superior to paper and cloth towels. Ansari et al45 compared the effectiveness of paper towels, cloth towels, and hot air dryers in eliminating rotaviruses and Escherichia coli from the hands. For air drying, the washed finger pads were held 10 cm from the nozzle of hot air dryers for 10 seconds. For drying with paper towels or cloth towels, finger pads were placed onto the absorbent surface with uniform pressure for 10 seconds. The authors did not incorporate any friction in hand drying because of the difficulties in standardizing and accurately representing field conditions. To evaluate the effects of different drying procedures, the microorganisms on the finger pad were eluted with balanced salt solution, and the eluates were then titrated. The study found that drying with hot air dryers produced the highest reduction and drying with cloth towels produced the lowest reduction in the number of both microorganisms. However, Ansari et al45 also mentioned that friction is often applied when hands are dried with paper or cloth towels. Whether friction can result in a further reduction of contamination during hand drying remains to be determined.
Some studies found no significant difference among hand-drying methods for removing bacteria from washed hands. Gustafson et al46 examined the hygiene performance of paper towels, cloth towels, hot air dryers, and spontaneous evaporation. The study compared the difference between the amount of bacteria on the hands after drying by 4 methods. Bacteria were determined using a modified glove-juice sampling procedure, and the results revealed no difference among the 4 methods. Taylor et al47 and Matthews and Newsom48 investigated the residual bacteria on the hands after drying with hot air dryers and paper towels using contact plates. They also found no difference regarding removal of bacteria between the 2 methods.
Other studies have explored the differential results. Yamamoto et al49 used a contact plate method to evaluate the effect of hot air dryers when hands were rubbed and when hands were held stationary. When hands were rubbed, bacteria on the hands increased significantly after 15 seconds of use. When hands were held stationary, bacteria on the hands decreased. The authors further investigated the differences in bacterial numbers on hands between drying with hot air dryers and paper towels. Paper towels were found to be more effective for removing bacteria from fingertips but not palms and fingers. This study finally concluded that hot air drying of stationary hands for 30 seconds with UV light was more effective for removing bacteria than paper towel drying. Drying with hot air dryers while rubbing hands was less effective than using paper towels. Snelling et al35 compared a jet air dryer against 2 models of hot air dryers with regard to bacterial transfer after drying and the effect of rubbing hands during dryer use. For a drying time of 10 seconds, both hot air dryers were associated with higher levels of bacteria transfer than when no dryer was used at all. However, the jet air dryer led to much less bacterial transfer than hot air dryers. When hot air dryers were used for 30 to 35 seconds, their performance improved greatly but was still worse than that observed with the jet air dryer after 10 seconds of use. Also, rubbing hands when using hot air dryers inhibited the overall reduction in bacterial numbers. To further compare with the paper towel method, the authors sampled bacteria from palms, fingers, and fingertips using contact plates. They found that drying hands with paper towels was the best means of removing bacteria from the hands, particularly from fingertips.
Effect on Cross-contamination
Washrooms and toilets are recognized as places at high risk of bacterial growth and transmission.50 Every time a toilet is flushed, a fine aerosol mist can be sprayed into the air, over an area of up to 6 m2.51,52 This mist may contain many types of fecal bacteria that can cause diseases.53 Ngeow et al54 investigated the potential risk of hot air dryers contributing to airborne infection in a hospital setting. The study compared bacterial dispersal caused by hot air dryers with that caused by paper towels. The dispersal of bacteria by hot air dryers was found within a radius of approximately 3 ft from hot air dryers and to the investigator's laboratory coat. When paper towels were used for hand drying, no dispersal of bacteria was found. The authors therefore claimed that hot air dryers are unsuitable for use in critical care areas because they may contribute to cross-infection either via airborne dissemination or via contaminated personnel. Hanna et al43 also reported that hot air dryers resulted in a substantial number of airborne bacteria in the vicinity of the user, whereas paper and cloth towels produced negligible contamination of the surrounding environment. Redway and Fawdar39 evaluated the contamination of the washroom environment caused by different hand-drying methods. Jet air dryers were found to disperse hand contamination to a distance of at least 2 m. Paper towels and hot air dryers were much better than jet air dryers regarding contamination of the washroom environment. Paper towels were also better than hot air dryers for contamination directly below the device, but there was no difference at greater distances.
Other studies have reported that drying hands with hot air dryers is not likely to generate airborne infection. Taylor et al47 evaluated whether hot air dryers change the levels of airborne microorganisms in the washroom environment. They found that air emitted from the dryer outlet contained fewer microorganisms than air entering the dryers. They also found that levels of microorganisms on the external surfaces of hot air dryers were not different from those on other washroom surfaces. Thus, the authors argued that hot air dryers were appropriate for use in both the health care and food industry. Similarly, Matthews and Newsom48 compared the bacteria aerosols released into the air when drying hands by using 4 different models of hot air dryers and by using paper towels. They found no difference between aerosols liberated by paper towels and 2 models of hot air dryers, whereas the other 2 models of hot air dryers generated fewer aerosols than paper towels. They concluded that hot air dryers were safe from a bacteriologic viewpoint. However, it could be argued that, in these studies, the air from the fans can dilute the aerosols, so the results are not strictly comparable.
Other Issues
User Preference
User preference is an important determinant of hand hygiene adherence.40 A survey of 2000 citizens in Europe was conducted in 2008 to explore user perferences regarding different hand-drying methods.55 The survey revealed that 62% of users chose paper towels as their preferred hand-drying method, followed by hot air dryers (28%) and cloth roller towels (10%). Another survey of 2516 US adults in 2009 still found that most people preferred to dry their hands with paper towels.56 If they had a choice, 55% of respondents selected paper towels, 25% selected jet air dryers, 16% selected hot air dryers, 1% selected cloth roller towels, and 3% were not sure. In Australia, a recent telephone survey found that food manufacturers, facility managers, and commercial cleaners also rated paper towels as their most preferred method of hand drying.57 Hence, given the strong preference for using paper towels, hand hygiene adherence would possibly decrease if paper towels are not available in washrooms.
Skin Irritation
It is known that some antibacterial soaps, surgical hand preparations, and chlorine and iodine solutions can irritate the skin of hands.58,59 Use of air dryers may cause hands to become excessively dry, rough, and red. Hands can become irritated with frequent washing and drying.60 Affected persons often experience a feeling of dryness or burning; skin that feels rough; and erythema, scaling, or fissures. When the hands become irritated, health care workers may not wash their hands as often or as well. Concern regarding this effect of air dryers could become an important cause of poor acceptance of hand hygiene practices.
Noise
Air dryers, particularly jet air dryers, are obviously noisier than paper towels or cloth towels. According to Redway and Fawdar,39 the mean decibel level of using a jet air dryer at 0.5 m was 94 dB, which is in excess of that of a heavy truck passing 3 m away. When 2 jet air dryers were used at the same time, the decibel level at a distance of 2 m was 92 dB. Therefore, in washrooms with jet air dryers, the noise level could constitute a potential risk to those exposed to it for long periods.
Environmental Effect
The use of paper towels may have adverse effects relating to waste disposal and environment sustainability. However, limited research has been conducted to examine the environmental effect of different hand-drying methods. Budisulistiorini61 assessed the life cycle of paper towel and hot air dryer methods for hand drying. According to Budisulistiorini's study, the paper towel method emits relatively higher greenhouse gases than the hot air dryer method (1377 vs 1337 kg of carbon dioxide equivalent). In terms of environment sustainability, the hot air dryer method surpasses the paper towel method with better scores for 6 indicators (respiratory organics, respiratory inorganics, ozone layer, ecotoxicity, acidification/eutrophication, and fossil fuels) compared with 5 indicators (carcinogens, climate change, radiation, land use, and minerals) for paper towels.61
Cost
Using paper towels is more costly than using air dryers. Paper towels must be replaced frequently, whereas air dryers usually require little maintenance. Budisulistiorini61 argued that the paper towel method is labor intensive and also affected by users' behavior. However, air dryers can be costly to purchase and install. Therefore, those responsible for facility management should perform a careful cost analysis to determine whether they are cost-effective in their building.
Discussion
Hand drying should be an essential part of the hand hygiene process in health care.11,13 However, there appears to be little agreement regarding the most hygienic method of hand drying. The results of different studies have also been conflicting.62 Some studies indicated that electric air dryers are of inferior effectiveness when it comes to the issue of hygiene,39,43,44 whereas others were of a firm opinion that they are a safe and effective means of hand drying.47,48
The large discrepancy among studies may be partly explained by the differences in the experimental protocols used. The degree of wetness is an important factor in determining the number of bacteria detected. Taylor et al47 claimed that the contact plate results appeared to reflect the degree of wetness after drying rather than the actual number of bacteria on the hands. Some investigators used a long drying time of hot air dryers in their studies, whereas others used a short drying time. For example, Matthews and Newsom48 used hot air dryers until the study participants had completely dry hands, usually for 1 minute. However, Redway and Fawdar39 attempted to reproduce people's usual hand-drying practices as closely as possible. In their study, the mean hand-drying times were 10 seconds using paper towels and 20 seconds using hot air dryers. So the significantly poorer hygiene performance of hot air dryers could be due to their low drying efficiency and consequently the greater amount of water remaining on the hands.
Although jet air dryers had drying efficiency similar to paper towels, their hygiene performance was still worse than paper towels.39 The differences in bacterial numbers after drying with air dryers and paper towels could be due to other factors rather than the percentage of dryness alone. Friction can dislodge microorganisms from the skin surface during both hand washing and drying. Antimicrobial agents in soaps have too little contact time to have bactericidal effects during a single use or with sporadic washings, making friction the most important element in hand drying.40 It is likely that paper towels work better because they physically remove bacteria from the hands, whereas hot air dryers and jet air dryers cannot.39 In many instances, however, rubbing hands with hot air dryers to hasten drying would only lead to greater bacterial numbers and airborne dissemination.49 It might be that rubbing hands causes bacteria to migrate from the hair follicles to the skin surface.35,44
Many studies have found friction to be a key component in hand drying for removing contamination. For example, Sprunt et al63 and Coates et al32 reported that bacteria were removed from washed hands by the mechanical abrasive action of drying with paper towels. Taylor et al47 and Yamamoto et al49 conducted microbiological testing of the paper towels after use, which indicated that many bacteria were transferred from the hands to paper towels.
Air movement can encourage the dispersal and transmission of bacteria and increase the chance of cross-contamination. Surrounding air in the washroom is recirculated by air dryers. This recirculation may result in the dispersion of infective aerosols already in the atmosphere and those generated by hands being rubbed together for drying.45 Used air dryers in washrooms are often contaminated and can emit bacteria in their air flow.39 So, there is a potential risk of persons standing in front of air dryers acquiring the bacteria being dispersed in the air current toward them. The bacteria can be inhaled or can be deposited on the person's body or clothes, thus making him/her a potential mobile source of infection.54
Overall, the hygienic efficacy of the hand-drying method is not only the percentage of dryness of the hands but also the removal of bacteria from washed hands and the prevention of cross-contamination. Hot air dryers are generally not recommended for use in health care settings because such dryers are relatively slow and noisy and their hygiene performance is questionable.44 Cloth roller towels are not recommended because they can become common-use towels at the end of the roll and can be a source of pathogen transfer to clean hands. Recently, jet air dryers have undergone independent certification within the food safety arena in Australia, attesting to their increased hygiene benefits as opposed to the traditional hot air-drying method.64 However, the criteria and process of obtaining this type of certification remain questionable. The health and safety aspects of jet air dryers for use in locations where hygiene is paramount should still be carefully examined by the scientific community. Therefore, this makes paper towel drying, during which little air movement is generated, the most hygienic option of hand-drying methods in health care.39
The principles of hand hygiene are universal. They do not change because of sex, skin color, or hand size.40 On the basis of our review, drying hands thoroughly with single-use, disposable paper towels is the preferred method of hand drying in terms of hand hygiene. This conclusion raises the question of what types of paper towel should be used for hand drying. Does the quality of paper towel have an effect on hand hygiene adherence? When recycled paper is used for hand drying, what kinds of studies are appropriate to assess the cost benefit of using recycled paper? Many questions remain unanswered. Different types of paper towel may have different absorption characteristics, which can influence their capacity to remove bacteria from washed hands.45 The quality of paper towel is important because poor-quality towels can damage skin by abrasion and ineffective drying.41,65 Recycled paper would be more acceptable in the future because it can contribute to environment sustainability. Such research may have the potential to improve hand hygiene practice and sustainable development significantly.
The maintenance of a clean environment around paper towels is also important. Paper towels deposited in bins could act as a bacteriologic reservoir if disposal is not managed properly.47 Regular sanitary cleaning of washrooms is the only way to reduce bacteria numbers and prevent cross-contamination.51 Moreover, paper towels require delivery to users from dispensers. The risk of potential contamination among dispenser exits, paper towels, and hands should be considered in the design, construction, and use of paper towel dispensers.66 Architects working in the health care industry should also be aware of these issues when designing equipment for new facilities.67
Conclusion
Hand hygiene has the potential to prevent diseases and reduce health care–associated infections. The proper drying of hands after washing should be an essential component of effective hand hygiene procedures. Most studies have found that paper towels can dry hands efficiently, remove bacteria effectively, and cause less contamination of the washroom environment. From a hygiene standpoint, paper towels are superior to air dryers; therefore, paper towels should be recommended for use in locations in which hygiene is paramount, such as hospitals and clinics. The provision of paper towels should also be considered as a means of improving hand hygiene adherence among health care workers. Our findings may have implications for health professionals and medical educators aiming to design effective programs to promote hand hygiene practices.
Article Highlights.
-
■
Hand washing is the most important measure to reduce the burden of health care–associated infection.
-
■
Because the transmission of bacteria is more likely to occur from wet skin than from dry skin, the proper drying of hands after washing should be an essential component of hand hygiene procedures.
-
■
The hygienic efficacy of hand drying includes drying efficiency, the effective removal of bacteria, and the prevention of cross-contamination.
-
■
From a hygiene viewpoint, paper towels are superior to electric air dryers.
-
■
Drying hands thoroughly with single-use, disposable paper towels is the preferred mothod of hand drying in health care.
-
■
The provision of paper towels should be considered as a means of improving hand hygiene adherence among health care workers.
Acknowledgments
We thank Shannon Rutherford, PhD, senior lecturer of the Griffith University, for her helpful comments in the preparation of the submitted manuscript.
Footnotes
Potential Competing Interests: Susan Stack has served as an occupational health and safety consultant for Kimberly-Clark, Sydney, Australia.
Supplemental Online Material
Author Interview Video
References
- 1.Cowling B., Chan K., Fang V. Facemasks and hand hygiene to prevent influenza transmission in households. Ann Intern Med. 2009;151(7):437–446. doi: 10.7326/0003-4819-151-7-200910060-00142. [DOI] [PubMed] [Google Scholar]
- 2.Cheng V., Tai J., Wong L. Prevention of nosocomial transmission of swine-origin pandemic influenza virus A/H1N1 by infection control bundle. J Hosp Infect. 2010;74(3):271–277. doi: 10.1016/j.jhin.2009.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fitzgerald D.A. Human swine influenza A [H1N1]: practical advice for clinicians early in the pandemic. Paediatr Respir Rev. 2009;10(3):154–158. doi: 10.1016/j.prrv.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 4.Balkhy H., Abolfotouh M., Al-Hathlool R., Al-Jumah M. Awareness, attitudes, and practices related to the swine influenza pandemic among the Saudi public. BMC Infect Dis. 2010;10:42. doi: 10.1186/1471-2334-10-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park J.H., Cheong H.K., Son D.Y., Kim S.U., Ha C.M. Perceptions and behaviors related to hand hygiene for the prevention of H1N1 influenza transmission among Korean university students during the peak pandemic period. BMC Infect Dis. 2010;10:222. doi: 10.1186/1471-2334-10-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Talaat M., Afifi S., Dueger E. Effects of hand hygiene campaigns on incidence of laboratory-confirmed influenza and absenteeism in schoolchildren, Cairo, Egypt. Emerg Infect Dis. 2011;17(4):619–625. doi: 10.3201/eid1704.101353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aiello A., Murray G., Perez V. Mask use, hand hygiene, and seasonal influenza-like illness among young adults: a randomized intervention trial. J Infect Dis. 2010;201(4):491–498. doi: 10.1086/650396. [DOI] [PubMed] [Google Scholar]
- 8.Sullivan S.J., Jacobson R.M., Dowdle W.R., Poland G.A. 2009 H1N1 influenza. Mayo Clin Proc. 2010;85(1):64–76. doi: 10.4065/mcp.2009.0588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stewardson A., Pittet D. Ignác Semmelweis—celebrating a flawed pioneer of patient safety. Lancet. 2011;378(9785):22–23. doi: 10.1016/s0140-6736(11)61007-6. [DOI] [PubMed] [Google Scholar]
- 10.Goldmann D. System failure versus personal accountability—the case for clean hands. N Engl J Med. 2006;355(2):121–123. doi: 10.1056/NEJMp068118. [DOI] [PubMed] [Google Scholar]
- 11.Boyce J., Pittet D. Guideline for hand hygiene in health-care settings: recommendations of the healthcare infection control practices advisory committee and the HICPAC/SHEA/APIC/IDSA hand hygiene task force. Infect Control Hosp Epidemiol. 2002;23(12, suppl):S3–S40. doi: 10.1086/503164. [DOI] [PubMed] [Google Scholar]
- 12.Pittet D., Allegranzi B., Sax H. Evidence-based model for hand transmission during patient care and the role of improved practices. Lancet Infect Dis. 2006;6(10):641–652. doi: 10.1016/S1473-3099(06)70600-4. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization . WHO Guidelines on Hand Hygiene in Health Care. World Health Organization; Geneva, Switzerland: 2009. [Google Scholar]
- 14.Allegranzi B., Pittet D. Role of hand hygiene in healthcare-associated infection prevention. J Hosp Infect. 2009;73(4):305–315. doi: 10.1016/j.jhin.2009.04.019. [DOI] [PubMed] [Google Scholar]
- 15.Herud T., Nilsen R.M., Svendheim K., Harthug S. Association between use of hand hygiene products and rates of health care-associated infections in a large university hospital in Norway. Am J Infect Control. 2009;37(4):311–317. doi: 10.1016/j.ajic.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 16.Todd E., Greig J., Bartleson C., Michaels B. Outbreaks where food workers have been implicated in the spread of foodborne disease, part 5: sources of contamination and pathogen excretion from infected persons. J Food Prot. 2008;71(12):2582–2595. doi: 10.4315/0362-028x-71.12.2582. [DOI] [PubMed] [Google Scholar]
- 17.Green L., Radke V., Mason R. Factors related to food worker hand hygiene practices. J Food Prot. 2007;70(3):661–666. doi: 10.4315/0362-028x-70.3.661. [DOI] [PubMed] [Google Scholar]
- 18.Kinnula S., Tapiainen T., Renko M., Uhari M. Safety of alcohol hand gel use among children and personnel at a child day care center. Am J Infect Control. 2009;37(4):318–321. doi: 10.1016/j.ajic.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 19.Guinan M., McGuckin M., Ali Y. The effect of a comprehensive handwashing program on absenteeism in elementary schools. Am J Infect Control. 2002;30(4):217–220. doi: 10.1067/mic.2002.120366. [DOI] [PubMed] [Google Scholar]
- 20.Early E., Battle K., Cantwell E., English J., Lavin J., Larson E. Effect of several interventions on the frequency of handwashing among elementary public school children. Am J Infect Control. 1998;26(3):263–269. doi: 10.1016/s0196-6553(98)80011-4. [DOI] [PubMed] [Google Scholar]
- 21.Lopez-Quintero C., Freeman P., Neumark Y. Hand washing among school children in Bogotá, Colombia. Am J Public Health. 2009;99(1):94–101. doi: 10.2105/AJPH.2007.129759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aiello A., Coulborn R., Perez V., Larson E. Effect of hand hygiene on infectious disease risk in the community setting: a meta-analysis. Am J Public Health. 2008;98(8):1372–1381. doi: 10.2105/AJPH.2007.124610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rabie T., Curtis V. Handwashing and risk of respiratory infections: a quantitative systematic review. Trop Med Int Health. 2006;11(3):258–267. doi: 10.1111/j.1365-3156.2006.01568.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith S. A review of hand washing techniques in primary care and community settings. J Clin Nurs. 2009;18(6):786–790. doi: 10.1111/j.1365-2702.2008.02546.x. [DOI] [PubMed] [Google Scholar]
- 25.Sickbert-Bennett E., Weber D., Gergen-Teague M., Sobsey M., Samsa G., Rutala W. Comparative efficacy of hand hygiene agents in the reduction of bacteria and viruses. Am J Infect Control. 2005;33(2):67–77. doi: 10.1016/j.ajic.2004.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Todd E., Greig J., Michaels B., Bartleson C., Smith D., Holah J. Outbreaks where food workers have been implicated in the spread of foodborne disease, part 11: use of antiseptics and sanitizers in community settings and issues of hand hygiene compliance in health care and food industries. J Food Prot. 2010;73(12):2306–2320. doi: 10.4315/0362-028x-73.12.2306. [DOI] [PubMed] [Google Scholar]
- 27.Edson R.S., Bundrick J.B., Litin S.C. Clinical pearls in infectious diseases. Mayo Clin Proc. 2011;86(3):245–248. doi: 10.4065/mcp.2010.0491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O'Boyle C., Henly S., Larson E. Understanding adherence to hand hygiene recommendations: the theory of planned behavior. Am J Infect Control. 2001;29(6):352–360. doi: 10.1067/mic.2001.18405. [DOI] [PubMed] [Google Scholar]
- 29.Haas J., Larson E. Measurement of compliance with hand hygiene. J Hosp Infect. 2007;66(1):6–14. doi: 10.1016/j.jhin.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 30.Pittet D., Hugonnet S., Harbarth S. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Lancet. 2000;356(9238):1307–1312. doi: 10.1016/s0140-6736(00)02814-2. [DOI] [PubMed] [Google Scholar]
- 31.Erasmus V., Daha T.J., Brug H. Systematic review of studies on compliance with hand hygiene guidelines in hospital care. Infect Control Hosp Epidemiol. 2010;31(3):283–294. doi: 10.1086/650451. [DOI] [PubMed] [Google Scholar]
- 32.Coates D., Hutchinson D., Bolton F. Survival of thermophilic campylobacters on fingertips and their elimination by washing and disinfection. Epidemiol Infect. 1987;99(2):265–274. doi: 10.1017/s095026880006773x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Patrick D., Findon G., Miller T. Residual moisture determines the level of touch-contact-associated bacterial transfer following hand washing. Epidemiol Infect. 1997;119(3):319–325. doi: 10.1017/s0950268897008261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Merry A., Miller T., Findon G., Webster C., Neff S. Touch contamination levels during anaesthetic procedures and their relationship to hand hygiene procedures: a clinical audit. Br J Anaesth. 2001;87(2):291–294. doi: 10.1093/bja/87.2.291. [DOI] [PubMed] [Google Scholar]
- 35.Snelling A.M., Saville T., Stevens D., Beggs C.B. Comparative evaluation of the hygienic efficacy of an ultra-rapid hand dryer vs conventional warm air hand dryers. J Appl Microbiol. 2011;110(1):19–26. doi: 10.1111/j.1365-2672.2010.04838.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Public Health Resource Unit Critical Appraisal Skills Programme (CASP): Making Sense of Evidence. http://www.sph.nhs.uk/sph-files/casp-appraisal-tools/S.Reviews%20Appraisal%20Tool.pdf Accessed April 26, 2011.
- 37.American Dryer Hand Dryers. http://www.americandryer.com/hand-dryers/ Accessed April 12, 2011.
- 38.Dyson Airblade: The Most Hygienic Hand Dryer. http://www.dysonairblade.com/technology/hygiene.asp Accessed April 2, 2011.
- 39.Redway K., Fawdar S. European Tissue Symposium: A Comparative Study of Three Different Hand Drying Methods: Paper Towel, Warm Air Dryer, Jet Air Dryer. http://www.europeantissue.com/pdfs/090402-2008%20WUS%20Westminster%20University%20hygiene%20study,%20nov2008.pdf Accessed April 22, 2011.
- 40.Todd E.C.D., Michaels B.S., Smith D., Greig J.D., Bartleson C.A. Outbreaks where food workers have been implicated in the spread of foodborne disease, part 9: washing and drying of hands to reduce microbial contamination. J Food Prot. 2010;73(10):1937–1955. doi: 10.4315/0362-028x-73.10.1937. [DOI] [PubMed] [Google Scholar]
- 41.Jumaa P. Hand hygiene: simple and complex. Int J Infect Dis. 2005;9(1):3–14. doi: 10.1016/j.ijid.2004.05.005. [DOI] [PubMed] [Google Scholar]
- 42.Knights B., Evans C., Barrass S., McHardy B. Hand Drying: An Assessment of Efficiency and Hygiene of Different Methods: A Survey Carried Out by the Applied Ecology Research Group for the Association of Makers of Soft Tissue Papers. University of Westminster; London, UK: 1993. [Google Scholar]
- 43.Hanna P.J., Richardson B.J., Marshall M. A comparison of the cleaning efficiency of three common hand drying methods. Appl Occup Environ Hyg. 1996;11(1):37–43. [Google Scholar]
- 44.Blackmore M. A comparison of hand drying methods. Cater Health. 1989;1(1):189–198. [Google Scholar]
- 45.Ansari S., Springthorpe V., Sattar S., Tostowaryk W., Wells G. Comparison of cloth, paper, and warm air drying in eliminating viruses and bacteria from washed hands. Am J Infect Control. 1991;19(5):243–249. doi: 10.1016/s0196-6553(05)80256-1. [DOI] [PubMed] [Google Scholar]
- 46.Gustafson D.R., Vetter E.A., Arson D.R.L. Effects of 4 hand-drying methods for removing bacteria from washed hands: a randomized trial. Mayo Clin Proc. 2000;75(7):705–708. doi: 10.4065/75.7.705. [DOI] [PubMed] [Google Scholar]
- 47.Taylor J., Brown K., Toivenen J., Holah J. A microbiological evaluation of warm air hand driers with respect to hand hygiene and the washroom environment. J Appl Microbiol. 2000;89(6):910–919. doi: 10.1046/j.1365-2672.2000.01122.x. [DOI] [PubMed] [Google Scholar]
- 48.Matthews J.A., Newsom S.W.B. Hot air electric hand driers compared with paper towels for potential spread of airborne bacteria. J Hosp Infect. 1987;9(1):85–88. doi: 10.1016/0195-6701(87)90101-0. [DOI] [PubMed] [Google Scholar]
- 49.Yamamoto Y., Ugai K., Takahashi Y. Efficiency of hand drying for removing bacteria from washed hands: comparison of paper towel drying with warm air drying. Infect Control Hosp Epidemiol. 2005;26(3):316–320. doi: 10.1086/502546. [DOI] [PubMed] [Google Scholar]
- 50.Hambraeus A., Malmborg A. Disinfection or cleaning of hospital toilets—an evaluation of different routines. J Hosp Infect. 1980;1(2):159–163. doi: 10.1016/0195-6701(80)90048-1. [DOI] [PubMed] [Google Scholar]
- 51.Mendes M.F., Lynch D.J. A bacteriological survey of washrooms and toilets. J Hyg. 1976;76(2):183–190. doi: 10.1017/s002217240005508x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Scott E., Bloomfield S.F. A bacteriological investigation of the effectiveness of cleaning and disinfection procedures for toilet hygiene. J Appl Bacteriol. 1985;59(3):291–297. doi: 10.1111/j.1365-2672.1985.tb01791.x. [DOI] [PubMed] [Google Scholar]
- 53.Jackson M., Aldred J., Canady J., Corsi R., Siegel J. The potential role of toilets as a vector for transmission of infectious disease. http://www.ce.utexas.edu/prof/Siegel/papers/conference/jackson_2010_toilet_iaqvec2010.pdf Accessed May 21, 2011.
- 54.Ngeow Y.F., Ong H.W., Tan P. Dispersal of bacteria by an electric air hand dryer. Malays J Pathol. 1989;11:53–56. [PubMed] [Google Scholar]
- 55.INTERMETRA Business & Market Research Group Study of the consumers' attitudes to different handdrying systems for European Tissue Symposium June 2008. http://www.europeantissue.com/pdfs/090415%20Intermetra%20Users%20preference%20study%204%20countries%202008%20Report%20June%202008.pdf Accessed May 8, 2011.
- 56.Paper towels prove most hygienic in restroom study. http://www.csdecisions.com/2009/06/08/paper-towels-prove-most-hygienic-in-restroom-study/ Accessed May 16, 2011.
- 57.Stack S., Pringle N. Hand drying research: food manufacturers, facility managers, and commercial cleaners. http://www.stackmasula.com.au/documents/FootprintsHandDryingResearchReport.pdf Accessed November 18, 2011.
- 58.Boyce J., Kelliher S., Vallande N. Skin irritation and dryness associated with two hand-hygiene regimens: soap-and-water hand washing versus hand antisepsis with an alcoholic hand gel. Infect Control Hosp Epidemiol. 2000;21(7):442–448. doi: 10.1086/501785. [DOI] [PubMed] [Google Scholar]
- 59.Sickbert-Bennett E.E., Weber D.J., Gergen-Teague M.F., Rutala W.A. The effects of test variables on the efficacy of hand hygiene agents. Am J Infect Control. 2004;32(2):69–83. doi: 10.1016/j.ajic.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 60.Pedersen L., Held E., Johansen J., Agner T. Less skin irritation from alcohol-based disinfectant than from detergent used for hand disinfection. Br J Dermatol. 2005;153(6):1142–1146. doi: 10.1111/j.1365-2133.2005.06875.x. [DOI] [PubMed] [Google Scholar]
- 61.Budisulistiorini S.H. Life cycle assessment of paper towel and electric dryer as hand drying method in the University of Melbourne. http://staff.undip.ac.id/env/budisulistiorini/files/2009/08/LCA-Paper-Towel-and-Electric-Dryer.pdf Accessed May 28, 2011.
- 62.Larmer P.J., Tillson T.M., Scown F.M., Grant P.M., Exton J. Evidence-based recommendations for hand hygiene for health care workers in New Zealand. N Z Med J. 2008;121(1272):69–81. [PubMed] [Google Scholar]
- 63.Sprunt K., Redman W., Leidy G. Antibacterial effectiveness of routine hand washing. Pediatrics. 1973;52(2):264–271. [PubMed] [Google Scholar]
- 64.HACCP Australia HACCP Australia Food Safety Bulletin, Issue 10, 2009. http://www.haccp.com.au/documents/bulletin10.pdf Accessed April 26, 2011.
- 65.Gould D. Hand decontamination: nurses' opinions and practices. Nurs Times. 1995;91(17):42–45. [PubMed] [Google Scholar]
- 66.Harrison W.A., Griffith C.J., Ayers T., Michaels B. Bacterial transfer and cross-contamination potential associated with paper-towel dispensing. Am J Infect Control. 2003;31(7):387–391. doi: 10.1067/mic.2003.81. [DOI] [PubMed] [Google Scholar]
- 67.Harrison W.A., Griffith C.J., Michaels B., Ayers T. Technique to determine contamination exposure routes and the economic efficiency of folded paper-towel dispensing. Am J Infect Control. 2003;31(2):104–108. doi: 10.1067/mic.2003.71. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Author Interview Video


