Abstract
Suicide in the US Army is a high-profile public health problem that is complex and poorly understood. Adding to the confusion surrounding Army suicide is the challenge of defining and understanding individuals/populations dying by suicide. Data from recent studies have led to a better understanding of risk factors for suicide that may be specifically associated with military service, including the impact of combat and deployment on increased rates of psychiatric illness in military personnel. The next steps involve applying these results to the development of empirically supported suicide prevention approaches specific to the military population. This special article provides an overview of suicide in the Army by synthesizing new information and providing clinical pearls based on research evidence.
Abbreviations and Acronyms: PTSD, posttraumatic stress disorder; VHA, Veterans Health Administration
Suicide in the US Army increased 80% in 2004 to 2008 above the previous stable suicide rate from 1977 to 2003.1 This increase, corresponding with the beginning of combat operations in Iraq in 2003, has affected soldiers throughout the US Army. Of the 301 confirmed or suspected suicides reported in 2010, 156 soldiers were on active duty, which includes Regular Army and activated Reserve Component soldiers, and 145 were inactive reservists.2 Most recently, the military reported in June 2012 that suicides have outpaced combat casualties since the beginning of the year and that the 154 suicides from January to June represent an 18% increase compared with the same period in 2011.3 Thus, suicide remains a pressing concern in the military population (Figure).4
FIGURE.
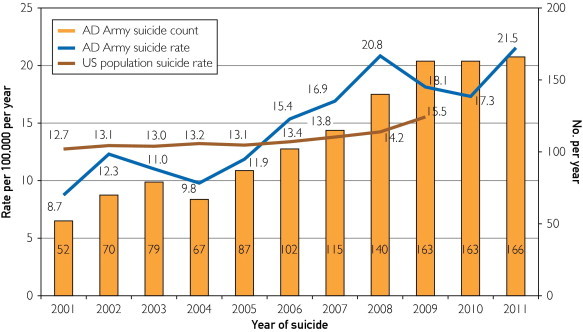
Total active duty (AD) Army suicides and suicide rates vs US population suicide rates by year of suicide (2001-2011). Active duty includes Active Army and activated National Guard and US Army Reserves. Suicides are confirmed or pending confirmation (2 from 2009 and 5 from 2010) by the Armed Forces Medical Examiner System. The AD Army and US population rates are age standardized to the 2000 US Census standard population using the age groups 18 to 24, 25 to 34, and 35 to 64 years. Data sources used include the Armed Forces Medical Examiner System, the Defense Manpower Data Center, the Centers for Disease Control and Prevention Web-based Injury Statistics Query and Reporting System, and the US Census. The calculations were performed in July 2012 by the Behavioral and Social Health Outcomes Program, US Army Institute of Public Health, US Army Public Health Command, Aberdeen Proving Ground, Aberdeen, Maryland.
The focus of this article is to review suicide in one branch of the US military: the Army, both active duty and reserve components. Although many similarities exist between the different branches of the military (Air Force, Coast Guard, Navy, and Marine Corps) and the Army, there are also substantial differences related to service branch size, mission, culture, suicide prevention programs, and fraction of service time deployed as a part of the larger forces in Afghanistan and Iraq. This review also summarizes current literature examining the effects of combat exposure and its relationship with psychiatric illness and suicide. Finally, clinical pearls translating evidence from research to practice to manage suicide risk in soldiers and veterans are discussed.
Overview of Army Components
The US Army is a volunteer force with different service commitment lengths. The Army force in Afghanistan and Iraq consists of active duty and reserve components. The total number of soldiers in both components is approximately 1.1 million, with each being almost equal in size.5 The first component, the Regular Army or Active Army, is the full-time permanent Army. The reserve component consists of the combined members of the Army Reserve and the Army National Guard. More than 500,000 Army Reserve and Army National Guard soldiers have been activated since September 11, 2001.6 Members of the Active Army return to their assigned post, or base, after deploying, where extensive supports are available as soldiers continue working with their primary units. Reservists return to their civilian lives and homes at the conclusion of their deployments.
The wars in Afghanistan and Iraq have been the longest in our nation's history. Their length and the unique nature of service have made it difficult to discretely identify, track, and compare affected Army groups at risk for suicide. Many soldiers serving in Iraq and Afghanistan are no longer in the Active Army or Army Reserve. They may have retired, separated, or, in some cases, switched between the active and reserve components or vice versa. All soldiers may potentially receive psychiatric care directly from the military, in Veterans Health Administration (VHA) facilities, from civilian practices, or from a combination of these settings. Further complicating suicide surveillance, soldiers who previously identified mental health problems via postdeployment screening are significantly more likely to leave the service than are soldiers who did not.7
Veterans are broadly defined as individuals who previously served in the military. Although descriptions in media and research publications sometimes identify those who receive care in VHA facilities as the largest population of all veterans, only 36% (7.9 million) of the estimated 22 million veterans in 2007 received care at VHA facilities.8 Note that this figure may be an overestimate of veterans who received care as VHA facilities may also provide services to staff members, active duty personnel, and surviving spouses of veterans. Although the suicide rate in veterans receiving care at VHA facilities is higher than that in the general population,9-11 there is ongoing controversy12 regarding whether there are increased rates of suicide in the larger population of all veterans. Definitive data comparing the suicide status of Iraq and Afghanistan war veterans with that of veterans of other wars is not currently available.13
Suicide in the United States
In 2009, suicide was the tenth leading cause of death in the United States, accounting for 36,909 deaths.14 Men died at a rate of almost 4 to 1 compared with women, with suicides accounting for 2.4% of all US male deaths and 0.6% of all female deaths.14 Twice as many individuals died by suicide compared with homicide in 2009.14
Suicide is a multifactorial, complex behavior modified by genetic, environmental, and cultural influences.15-18 Current theoretical models of suicide posit an underlying risk/capacity for suicide that when combined acutely with psychosocial stress/loss leads to suicidal behavior.19,20 Completed suicide is relatively rare vs the prevalence of thoughts of suicide, serious planning of suicide, and suicide attempts.21 A previous suicide attempt increases the risk of later death by suicide.22 Suicidal behavior is more common in the young and is strongly associated with substance abuse and dependence.21
The most common factor increasing the risk of suicide and suicide-related behaviors is psychiatric illness. Psychological autopsy study meta-analyses found that more than 90% of those dying by suicide have psychiatric illness.23,24 Despite years of research into the clinical and demographic variables associated with suicide, there is no predictive model or patient risk assessment tool that can accurately identify those who will take their own lives or what their final pathways to suicide will be.25,26 Suicide's relative rarity also presents challenges to proving that interventions targeting psychiatric illness, promoting individual resiliency, or reducing other suicide risk factors are effective in preventing suicide.27
The Healthy Soldier Effect
The military, owing to screening processes and the nature of military service, is not comparable in general health or medical outcomes with the larger US population.28 The term healthy soldier effect has been coined to describe the decrease in all-cause mortality observed in military members, particularly in the period immediately after they leave the service.29,30
Physical examinations and screening of individuals' medical and psychiatric histories are conducted before entry into the Army. Basic educational and physical standards must be met and maintained to stay in the Army. Potential recruits with preexisting psychiatric illness are often excluded from military service. Once on active duty, service members who develop a serious mental illness (eg, schizophrenia or bipolar disorder) are medically retired from the service.31,32 Soldiers identified with conduct problems and personality disorders incompatible with military service may be administratively separated (discharged without benefits or medical retirement).31,32 Those with alcohol use disorders unresponsive to treatment are separated from the military. Members abusing drugs face administrative action, discharge, or even incarceration under the Uniform Code of Military Justice.
Sociocultural protective factors for the military include 100% employment, guaranteed housing, and higher educational levels compared with the general population. All service members have access to quality medical care, and there are ongoing efforts to track population levels of health and readiness.
Historical Army Suicide Rates
A simple review of unadjusted, historical Army suicide rates reflects essentially the same suicide rate in the US Army as in the general US population. Demographically, compared with the larger US population (median age, 37.2 years; 50.8% female and 49.2% male), the Army force is younger and consists of 86% men and 14% women.33 After adjustment for age and sex, Army (and military) suicide rates have been consistently approximately 20% lower than those of the US general population.34 More than 90% of those dying by suicide in the Army are men compared with 78.8% male and 21.2% female in the general population.35
Why has the suicide rate been lower? Beyond the sociocultural protective factors for suicide described earlier, preservice screening and medical retirements for those with serious mental illness have raised questions about whether decreased rates are due to a lower prevalence of psychiatric illness in the Army. However, there is still a baseline Army population with psychiatric illness undetected on initial entry screening. This group consists of those with preexisting mental illness and those who develop psychiatric syndromes during their Army service.
To identify baseline rates of psychiatric illness in service members and the effects of military service on mental health, the Millennium Cohort Study36 was developed to follow service members across a 22-year period. Members of all branches of the military are represented, and monitoring continues after participants leave the military. Data covering the period up to the beginning of the Iraq War (2001-2003)36 found a baseline prevalence of mental disorders within the expected levels of US general population research samples. These data included prevalence estimates for depressive disorders and anxiety disorders, such as posttraumatic stress disorder (PTSD). Alcohol abuse rates were consistent with or slightly higher than those of nonmilitary populations.37
In the US general population, individuals with depression or substance use disorders compose most total suicides. This is based on their combined relative risk and higher prevalence in the United States.15 Based on Millennium Cohort research, mental disorder prevalence in the military was similar to that in the civilian population at the beginning of combat operations in Iraq.
Combat and Deployment Effects
Information on the impact of combat and deployment is available through 2 mechanisms. The first method is from soldiers' self-report while undergoing various military screenings. Information from military predeployment and postdeployment self-reports shows that rates of major depression, generalized anxiety, PTSD, and substance misuse are increased after deployment and are positively correlated with the intensity and duration of combat experiences.7,38-45 The onset of symptoms and their resolution or continuation is also related to time after deployment.39 These data, though, may not capture the full extent of combat and deployment effects on psychiatric illness and potential suicide risk. Nonconfidential self-report data have been criticized for underestimating combat and deployment effects due to potential stigma bias. Service members may not self-report owing to a perceived potential effect on their performance reports, opportunities for promotion, security clearances, and career field.
The second method for collecting information on soldier health related to combat and deployment is from anonymous/nonattributable responses. A 2011 study assessing the effect of anonymity on symptom screening after combat deployment for depression, PTSD, or mental health problems and for interest in seeking care found that anonymous disclosure resulted in 2 to 4 times higher reporting than did nonconfidential screening.42 One-fifth of soldiers reported that they were not comfortable in giving honest responses to nonconfidential screening questions.42 Extrapolating these results, most soldiers with problems do not self-identify.
Deployment also results in higher rates of aggressive behaviors and alcohol misuse.46 Although aggressive behaviors are not defined as psychiatric syndromes, aggression and impulsivity have been identified as suicide risk factors.47,48 In recently published research, aggressive behaviors were defined in terms of how often personnel “got angry with someone and kicked or smashed something, slammed the door, punched the wall, etc”; “threatened someone with physical violence”; or “got into a fight with someone and hit the person” in the past month.46 Approximately 40% of soldiers acknowledged postdeployment aggressive behaviors compared with a predeployment rate of 11.2% from an earlier separate research sample.38 From epidemiologic data and theoretical models, various combinations of psychiatric illness, aggressive behavior, and alcohol misuse may result in a transition from psychiatric syndromes alone to actual suicidal behavior.49-51
Multiple Deployments
Army soldiers are typically deployed for 12 months, although actual lengths of deployment may vary. The recommended frequency for deployment of active Army soldiers had been 1 year deployed with a goal of 2 years back (ie, “dwell time”) at their home base. Reserve Army troops previously cycled for 1 year of deployment followed by 5 years of dwell time. However, the heavy demands of the 2 wars have led to an inability to meet dwell time recommendations for both components.52 As a result of mounting concerns about deployment impact, in August 2011, the Army announced a change in deployment length to 9 months53 with a continued goal of 2 years of dwell time at home.
A 2012 study41 from the Naval Health Research Center quantified the impact of multiple deployments on the development of psychiatric illness in the Marine Corps. Marines with 2 deployments had higher rates of PTSD compared with those with only 1 deployment.41 A longer dwell time relative to first deployment, that is, more time spent at home base after initial deployment, was associated with a reduced odds of having PTSD and other psychiatric disorders. These findings are consistent with previous Army research and assessments.40,43
Current Army Suicide Rates
As noted at the beginning of this article, the Army suicide rate increased 80% from 2004 to 2008.1 In 2008, the age- and sex-adjusted suicide rate in the Army was greater than the civilian average for the first time in recorded history.1 The Army rate in 2008 of 20.2 per 100,000 person-years was well above the expected rate of 12.2 per 100,000 person-years and higher than the US general population rate of 19.2 per 100,000 person-years in 2006,35 adjusted for the makeup of the Active Duty Army.
Reserve component rates have not previously been tracked closely and are difficult to compare with historic Regular Army rates. However, current rates are concerning. In 2010, Army National Guard rates were 31 per 100,000 person-years vs 24 per 100,000 person-years in the Army Reserve.54 This compared with a then 2010 rate of 25 per 100,000 person-years for the Regular Army.54 The 2007 civilian age-adjusted rate was 20.3 per 100,000 person-years for comparison purposes.54
Clinical Care Use and Suicide
A 2012 report by Bachynski et al1 using Army-level data provides information on the relationships among combat and deployment, clinical care, and suicide. Using data from 2 larger Defense Department tracking and surveillance systems, they found that an increase in suicides paralleled a marked increase in psychiatric treatment rates.1 Between 2003 and 2008, the psychiatric illness treatment rate, defined by outpatient visits, increased from 116 per 100,000 person-years to 216 per 100,000 person-years,1 nearly double that found at the beginning of the Iraq War. Soldiers with depression were 11 times more likely to die by suicide, and those with anxiety disorders (PTSD included) were 10 times more likely to die by suicide.1
From 2003 to 2008, the rate of psychiatric hospitalizations in Army personnel almost doubled.1 Consistent with wider clinical practice and past research,55,56 soldiers hospitalized for psychiatric disorders were at greatest risk for suicide. Specifically, soldiers with a psychiatric inpatient stay died by suicide at a rate 15 times higher than soldiers who had not been hospitalized.1 Finally, the study results suggest that psychiatric hospitalizations were the most common reason for inpatient admissions in the military from 2003 to 2008, which is a change from previous hospitalization trends.57
Although previous research reflects increased rates of psychiatric illness and inpatient psychiatric hospitalizations, there seems to be a gap in terms of service members receiving outpatient clinical care for psychiatric issues. Previous research found that of service members meeting the criteria for a mental disorder on military postdeployment screening, only 23% to 40% sought care.38 In addition, a recent study by Ilgen et al11 found that approximately 50% of suicide decedents in the VHA did not have a formal psychiatric diagnosis at the time of death. Although suicide may occur in a relatively brief window of time for some individuals, it is also likely that many veterans simply were not engaged in mental health services in the months preceding their death. The underuse of clinical services may be related to concerns of stigma against personnel seeking help and treatment. Notably, service members who screen positive for a mental disorder have been shown to be twice as likely to report stigmatization as a possible barrier to seeking clinical care compared with those not screening positive.38
Suicide Research
To address this public health crisis in the active military and with veterans, the US government has dedicated an unprecedented increase in research funding to specifically address suicide.58 The Army has also taken immediate actions to change policies and procedures to decrease stigma for seeking mental health care.33 Military medical surveillance and preexisting research efforts combined with new civilian and military research projects have generated critical information on the effect of combat and deployment on psychiatric illness and suicide.
Other research efforts include measurement of the effects of improved screening for suicide risk, ongoing monitoring of suicide and suicidal behavior, and assessment of antidepressant drug use on suicide rates.58 Randomized controlled trials adapting evidence-based therapies, for example, cognitive behavior therapy, are under way in different clinical settings to identify whether they may be efficacious in military populations. Treatments aimed at higher-risk subgroups, including soldiers hospitalized for psychiatric disorders, are being developed and tested using best practice principles.58 Beyond research studies, an infrastructure to identify pressing needs and disseminate applicable research findings is being developed. This effort is aimed at speeding translation of interventions into practice.
Clinical Lessons Learned
Some insights for daily clinical practice can be taken from completed research studies and translated into practice. These include increasing evidence of sleep disturbances as warning signs for suicide and suicide-related behaviors, growing concerns related to the overprescription of opioid analgesics in patients with PTSD and other psychiatric diagnoses, and increased emphasis on restriction of access to firearms in those at risk for suicide.
Sleep disturbances have been previously identified as a risk factor for suicide.59-62 Ribiero et al,62 in a cross-sectional and longitudinal correlational study of young adults in the military, found that self-reported insomnia symptoms were associated with suicidal ideation even after controlling for depression, hopelessness, PTSD diagnosis, anxiety symptoms, and drug and alcohol abuse. When only depression and hopelessness were controlled, insomnia symptoms were uniquely predictive of suicide attempts in the month after assessment. Complaints of insomnia or other sleep disturbances in otherwise healthy soldiers, reservists, or veterans may signal the need for taking a careful history and screening for depression, substance misuse, and PTSD. These complaints may also serve as opportunities for referring those potentially needing more intensive treatment.
Opioid analgesic prescription in the United States continues to increase dramatically in parallel with rising rates of opioid misuse, unintentional overdose, and death.63-67 Unintentional overdose deaths, primarily with opioids, now outnumber traffic fatalities in many states. Individuals with psychiatric illness are overrepresented among those receiving opiate prescriptions and those taking overdoses.66 This same trend has been seen in former military personnel.
A 2012 VHA study68 analyzed the association between opioid prescription and clinical outcomes in Iraq and Afghanistan veterans with and without psychiatric disorders. Seal et al68 found that individuals with a PTSD diagnosis were almost 3 times as likely as veterans without a psychiatric diagnosis to be prescribed opioid analgesics. Iraq and Afghanistan veterans with a PTSD diagnosis who were prescribed opioids were significantly more likely to have opioid-related accidents and overdoses, alcohol and nonopioid drug-related accidents and overdoses, and self-inflicted and violence-related injuries.68 Similar to larger US practice trends,67 opioids were dispensed despite the presence of comorbid alcohol use and concomitant use of benzodiazepines.
Caution should be used in prescribing opioids for all patients with chronic, noncancer pain. The State of Washington has developed helpful guidelines for opioid prescribing69 for patients with chronic, noncancer pain that incorporate dosing guidelines and screening tools to address high-risk use and psychiatric illness and that provide recommendations for when to refer patients for specialty-level care. These guidelines69 seem temporally associated with a decrease in opiate dosage equivalents per patient, a reduction in the number of patients prescribed daily doses exceeding guidelines, and a decline in opioid-related deaths.70
Finally, 2 evidence-based strategies27 to consider for upstream suicide prevention (ie, before patients engage in a suicide attempt) include (1) improving primary care physician recognition and treatment of depression and (2) restricting access to lethal means in those at risk for suicide.27 Previous research suggests that patients who die by suicide are more likely to have visited a primary care physician within 1 month of their death than a mental health clinician.71 Programs developed to improve primary care clinicians' recognition and treatment of depression have resulted in decreased suicide rates.72-74 For a more extensive review of suicide risk management and depression in primary care, see the August 2011 issue of Mayo Clinic Proceedings.75
The second strategy focuses on restricting access to firearms since they are the means of choice for almost 70% of soldiers dying by suicide.33,35,58 Veterans are more likely to own firearms and are significantly more likely than the general population to die by firearms suicide.76 All veterans with psychiatric illness should be asked about firearms access and encouraged to deposit weapons in safe storage or remove them altogether from the home if an individual is experiencing increased psychiatric symptoms77 (eg, severe anxiety or hopelessness) or elevated chemical abuse that could raise the risk of suicidal action.78 There is a well-developed research literature on the increased risk of suicide in states and homes with increased rates of firearm ownership.79-82
Conclusion
The enormity of a person's death by suicide is not something defined abstractly by rates per 100,000, psychiatric diagnoses, or concepts such as impulsivity or aggression. Each death is a complex tragedy with indescribable effects on those left behind. Prevention of suicide in the military will require multiple interventions using a comprehensive public health framework that includes ongoing monitoring and research to better identify, understand, and modify the complex contributory risk factors.
In an Army population with markedly higher levels of psychiatric illness than before the 2003 initiation of the Iraq war, additional resources for diagnosis and treatment need to be allocated. Rising clinical demands may require the introduction of new models of care (eg, collaborative care) and the recruitment of physicians with skill sets commensurate with cutting-edge suicide prevention. Evidence-based treatment will need to be integrated into prevention strategies that must be adapted to the needs of a highly mobile force whose members frequently change bases and deploy to theaters of war.
With the return of US forces from Iraq in 2011 and the announced withdrawal of troops from Afghanistan in the near future, public awareness and concern may decrease about military suicides, specifically in those affected by the recent Middle East wars. Despite the end of large-scale military operations in Afghanistan and Iraq, the effects on the mental health of active duty service members, reservists, and veterans is only just beginning to be felt. Moreover, the potential effect on service members of their war experiences may manifest indefinitely into the future in the form of emerging psychiatric illnesses. The development of a model for suicide prevention in service members and veterans will require a national effort, public and private, sustained for the foreseeable future.
Acknowledgments
For their analysis and support, we thank Amy Millikan, MD, MPH, Eren Youmans, PhD, and the staff at the Behavioral and Social Health Outcomes Program, US Army Institute of Public Health, US Army Public Health Command, Aberdeen Proving Ground, Aberdeen, Maryland.
The opinions expressed in this article are the authors' alone. They do not represent the official positions, statements, or policies of the US Army, the Department of Defense, Mayo Clinic, or the University of Washington.
Footnotes
Potential Competing Interests: Dr Lineberry is a subject matter expert for suicide prevention for the US Army. Dr O'Connor is a research consultant for a Military Operational Medical Research Program–funded study measuring the efficacy of the Collaborative Assessment and Management of Suicidality compared with treatment as usual for suicidal active duty military personnel.
Supplemental Online Material
Author Interview Video
References
- 1.Bachynski KE, Canham-Chervak M, Black SA, Dada EO, Millikan AM, Jones BH. Mental health risk factors for suicides in the US Army, 2007-8 [published online March 7, 2012]. Inj Prev. [DOI] [PubMed]
- 2.Department of Defense Army releases December suicide data. 2010. http://www.defense.gov/releases/release.aspx?releaseid=14213 Accessed January 19, 2011.
- 3.Williams T. Suicides outpacing war deaths for troops. New York Times. June 8 2012:A10. http://www.nytimes.com/2012/06/09/us/suicides-eclipse-war-deaths-for-us-troops.html?_r=2 Accessed June 24, 2012. [Google Scholar]
- 4.Behavioral and Social Health Outcomes Program, US Army Institute of Public Health. Total Active Duty Army Suicides and Suicide Rate vs US Population Rate by Year of Suicide, 2001-2011: Calculations Performed July 2012. Aberdeen Proving Ground, Aberdeen, MD: Behavioral and Social Health Outcomes Program, US Army Institute of Public Health, US Army Public Health Command.
- 5.US Army Comptroller Fiscal year 2010: United States Army annual financial report; 2010. http://comptroller.defense.gov/cfs/fy2010/02_Department_of_the_Army/Fiscal_Year_2010_Department_of_Army_Financial_Statements_and_Notes.pdf Accessed June 24, 2012.
- 6.Office of the Assistant Secretary of Defense for Reserve Affairs The seven reserve components: 3rd quarter FY 2010. http://ra.defense.gov/documents/publications/The 7 Reserve Components.pdf Accessed June 24, 2012.
- 7.Hoge C.W., Auchterlonie J.L., Milliken C.S. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. 2006;295(9):1023–1032. doi: 10.1001/jama.295.9.1023. [DOI] [PubMed] [Google Scholar]
- 8.Congressional Budget Office The healthcare system for veterans: an interim report. December 21, 2007. http://www.cbo.gov/ftpdocs/88xx/doc8892/maintext.3.1.shtml Accessed June 24, 2012.
- 9.McCarthy J.F., Valenstein M., Kim H.M., Ilgen M., Zivin K., Blow F.C. Suicide mortality among patients receiving care in the Veterans Health Administration health system. Am J Epidemiol. 2009;169(8):1033–1038. doi: 10.1093/aje/kwp010. [DOI] [PubMed] [Google Scholar]
- 10.Blow F.C., Bohnert A.S., Ilgen M.A. Suicide mortality among patients treated by the Veterans Health Administration from 2000 to 2007. Am J Public Health. 2012;102(S1):S98–S104. doi: 10.2105/AJPH.2011.300441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ilgen M.A., Bohnert A.S., Ignacio R.V. Psychiatric diagnoses and risk of suicide in veterans. Arch Gen Psychiatry. 2010;67(11):1152–1158. doi: 10.1001/archgenpsychiatry.2010.129. [DOI] [PubMed] [Google Scholar]
- 12.Miller M., Azrael D., Barber C., Mukamal K., Lawler E. A call to link data to answer pressing questions about suicide risk among veterans. Am J Public Health. 2012;102(S1):S20–S22. doi: 10.2105/AJPH.2011.300572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kang H.K., Bullman T.A. Risk of suicide among US veterans after returning from the Iraq or Afghanistan war zones. JAMA. 2008;300(6):652–653. doi: 10.1001/jama.300.6.652. [DOI] [PubMed] [Google Scholar]
- 14.National Center for Injury Prevention and Control, Centers for Disease Control and Prevention FastStats: suicide and self-inflicted injury. http://www.cdc.gov/nchs/fastats/suicide.htm Accessed June 24, 2012.
- 15.Li Z., Page A., Martin G., Taylor R. Attributable risk of psychiatric and socio-economic factors for suicide from individual-level, population-based studies: a systematic review. Soc Sci Med. 2011;72(4):608–616. doi: 10.1016/j.socscimed.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 16.Pedersen N.L., Fiske A. Genetic influences on suicide and nonfatal suicidal behavior: twin study findings. Eur Psychiatry. 2010;25(5):264–267. doi: 10.1016/j.eurpsy.2009.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wasserman D., Wasserman J., Sokolowski M. Genetics of HPA-axis, depression and suicidality. Eur Psychiatry. 2010;25(5):278–280. doi: 10.1016/j.eurpsy.2009.12.016. [DOI] [PubMed] [Google Scholar]
- 18.Hawton K., van Heeringen K. Suicide. Lancet. 2009;373(9672):1372–1381. doi: 10.1016/S0140-6736(09)60372-X. [DOI] [PubMed] [Google Scholar]
- 19.Van Orden K.A., Witte T.K., Cukrowicz K.C., Braithwaite S.R., Selby E.A., Joiner T.E., Jr The interpersonal theory of suicide. Psychol Rev. 2010;117(2):575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mann J.J., Waternaux C., Haas G.L., Malone K.M. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry. 1999;156(2):181–189. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- 21.Substance Abuse and Mental Health Services Administration The NSDUH report: suicidal thoughts and behaviors among adults. September 17, 2009. http://www.samhsa.gov/data/2k9/165/suicide.htm Accessed June 24, 2012. [PubMed]
- 22.Isometsa E.T., Lonnqvist J.K. Suicide attempts preceding completed suicide. Br J Psychiatry. 1998;173(Dec):531–535. doi: 10.1192/bjp.173.6.531. [DOI] [PubMed] [Google Scholar]
- 23.Arsenault-Lapierre G., Kim C., Turecki G. Psychiatric diagnoses in 3275 suicides: a meta-analysis. BMC Psychiatry. 2004;4(Nov):37. doi: 10.1186/1471-244X-4-37. http://www.biomedcentral.com/1471-244X/4/37 Accessed June 24, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bertolote J.M., Fleischmann A. Suicide and psychiatric diagnosis: a worldwide perspective. World Psychiatry. 2002;1(3):181–185. [PMC free article] [PubMed] [Google Scholar]
- 25.Oquendo M.A., Currier D., Mann J.J. Prospective studies of suicidal behavior in major depressive and bipolar disorders: what is the evidence for predictive risk factors? Acta Psychiatr Scand. 2006;114(3):151–158. doi: 10.1111/j.1600-0447.2006.00829.x. [DOI] [PubMed] [Google Scholar]
- 26.Pokorny A.D. Prediction of suicide in psychiatric patients: report of a prospective study. Arch Gen Psychiatry. 1983;40(3):249–257. doi: 10.1001/archpsyc.1983.01790030019002. [DOI] [PubMed] [Google Scholar]
- 27.Mann J.J., Apter A., Bertolote J. Suicide prevention strategies: a systematic review. JAMA. 2005;294(16):2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 28.McLaughlin R., Nielsen L., Waller M. An evaluation of the effect of military service on mortality: quantifying the healthy soldier effect. Ann Epidemiol. 2008;18(12):928–936. doi: 10.1016/j.annepidem.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 29.Kang H.K., Bullman T.A. Mortality among U.S. veterans of the Persian Gulf War. N Engl J Med. 1996;335(20):1498–1504. doi: 10.1056/NEJM199611143352006. [DOI] [PubMed] [Google Scholar]
- 30.Rothberg J.M., Bartone P.T., Holloway H.C., Marlowe D.H. Life and death in the US Army: in Corpore sano. JAMA. 1990;264(17):2241–2244. [PubMed] [Google Scholar]
- 31.Hoge C.W., Lesikar S.E., Guevara R. Mental disorders among U.S. military personnel in the 1990s: association with high levels of health care utilization and early military attrition. Am J Psychiatry. 2002;159(9):1576–1583. doi: 10.1176/appi.ajp.159.9.1576. [DOI] [PubMed] [Google Scholar]
- 32.Hoge C.W., Toboni H.E., Messer S.C., Bell N., Amoroso P., Orman D.T. The occupational burden of mental disorders in the U.S. military: psychiatric hospitalizations, involuntary separations, and disability. Am J Psychiatry. 2005;162(3):585–591. doi: 10.1176/appi.ajp.162.3.585. [DOI] [PubMed] [Google Scholar]
- 33.Headquarters, Department of the Army Army 2020: generating the health and discipline of the force: ahead of the strategic reset: report 2012. http://usarmy.vo.llnwd.net/e2/c/downloads/232541.pdf Accessed June 24, 2012.
- 34.Eaton K.M., Messer S.C., Garvey Wilson A.L., Hoge C.W. Strengthening the validity of population-based suicide rate comparisons: an illustration using U.S. military and civilian data. Suicide Life Threat Behav. 2006;36(2):182–191. doi: 10.1521/suli.2006.36.2.182. [DOI] [PubMed] [Google Scholar]
- 35.Chiarelli P.W. Army health promotion risk reduction suicide prevention report 2010. http://csf.army.mil/downloads/HP-RR-SPReport2010.pdf Accessed June 24, 2012.
- 36.Ryan M.A., Smith T.C., Smith B. Millennium Cohort: enrollment begins a 21-year contribution to understanding the impact of military service. J Clin Epidemiol. 2007;60(2):181–191. doi: 10.1016/j.jclinepi.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 37.Riddle J.R., Smith T.C., Smith B. Millennium Cohort: the 2001-2003 baseline prevalence of mental disorders in the U.S. military. J Clin Epidemiol. 2007;60(2):192–201. doi: 10.1016/j.jclinepi.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 38.Hoge C.W., Castro C.A., Messer S.C., McGurk D., Cotting D.I., Koffman R.L. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351(1):13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- 39.Milliken C.S., Auchterlonie J.L., Hoge C.W. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA. 2007;298(18):2141–2148. doi: 10.1001/jama.298.18.2141. [DOI] [PubMed] [Google Scholar]
- 40.Harben J., Mental Health Advisory Team VI http://www.armymedicine.army.mil/news/releases/20091113mhatvi.cfm Accessed June 24, 2012.
- 41.Macgregor A.J., Han P.P., Dougherty A.L., Galarneau M.R. Effect of dwell time on the mental health of US military personnel with multiple combat tours. Am J Public Health. 2012;102(suppl 1):S55–S59. doi: 10.2105/AJPH.2011.300341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Warner C.H., Appenzeller G.N., Grieger T. Importance of anonymity to encourage honest reporting in mental health screening after combat deployment. Arch Gen Psychiatry. 2011;68(10):1065–1071. doi: 10.1001/archgenpsychiatry.2011.112. [DOI] [PubMed] [Google Scholar]
- 43.Reger M.A., Gahm G.A., Swanson R.D., Duma S.J. Association between number of deployments to Iraq and mental health screening outcomes in US Army soldiers. J Clin Psychiatry. 2009;70(9):1266–1272. doi: 10.4088/JCP.08m04361. [DOI] [PubMed] [Google Scholar]
- 44.Eisen S.V., Schultz M.R., Vogt D. Mental and physical health status and alcohol and drug use following return from deployment to Iraq or Afghanistan. Am J Public Health. 2012;102(S1):S66–S73. doi: 10.2105/AJPH.2011.300609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shen Y.-C., Arkes J., Williams T.V. Effects of Iraq/Afghanistan deployments on major depression and substance use disorder: analysis of active duty personnel in the US military. Am J Public Health. 2012;102(S1):S80–S87. doi: 10.2105/AJPH.2011.300425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Thomas J.L., Wilk J.E., Riviere L.A., McGurk D., Castro C.A., Hoge C.W. Prevalence of mental health problems and functional impairment among active component and National Guard soldiers 3 and 12 months following combat in Iraq. Arch Gen Psychiatry. 2010;67(6):614–623. doi: 10.1001/archgenpsychiatry.2010.54. [DOI] [PubMed] [Google Scholar]
- 47.Kendler K.S. Genetic and environmental pathways to suicidal behavior: reflections of a genetic epidemiologist. Eur Psychiatry. 2010;25(5):300–303. doi: 10.1016/j.eurpsy.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 48.Mann J.J., Currier D.M. Stress, genetics and epigenetic effects on the neurobiology of suicidal behavior and depression. Eur Psychiatry. 2010;25(5):268–271. doi: 10.1016/j.eurpsy.2010.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nock M.K., Hwang I., Sampson N. Cross-national analysis of the associations among mental disorders and suicidal behavior: findings from the WHO World Mental Health Surveys. PLoS Med. 2009;6(8):e1000123. doi: 10.1371/journal.pmed.1000123. http://www.plosmedicine.org/article/info%3Adoi%2F10.1371%2Fjournal.pmed.1000123 Accessed June 24, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nock M.K., Hwang I., Sampson N.A., Kessler R.C. Mental disorders, comorbidity and suicidal behavior: results from the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15(8):868–876. doi: 10.1038/mp.2009.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bryan C.J., Cukrowicz K.C., West C.L., Morrow C.E. Combat experience and the acquired capability for suicide. J Clin Psychol. 2010;66(10):1044–1056. doi: 10.1002/jclp.20703. [DOI] [PubMed] [Google Scholar]
- 52.Gates R.M. Defense Secretary Gates Opening Statement at Senate Hearing; 2009. http://www.armed-services.senate.gov/statemnt/2009/January/Gates%2001-27-09.pdf Accessed June 24, 2012.
- 53.McIlvane R. Army News Service. August 8, 2011. Army Guard to begin nine-month deployments in 2012.http://www.ng.mil/news/archives/2011/08/080811-Army.aspx Accessed June 24, 2012. [Google Scholar]
- 54.Griffith J. Suicide in the Army National Guard: an empirical inquiry. Suicide Life Threat Behav. 2012;42(1):104–119. doi: 10.1111/j.1943-278X.2011.00075.x. [DOI] [PubMed] [Google Scholar]
- 55.Valenstein M., Kim H.M., Ganoczy D. Higher-risk periods for suicide among VA patients receiving depression treatment: prioritizing suicide prevention efforts. J Affect Disord. 2009;112(1-3):50–58. doi: 10.1016/j.jad.2008.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Meehan J., Kapur N., Hunt I.M. Suicide in mental health in-patients and within 3 months of discharge: national clinical survey. Br J Psychiatry. 2006;188(Feb):129–134. doi: 10.1192/bjp.188.2.129. [DOI] [PubMed] [Google Scholar]
- 57.Zoroya G. USA Today. May 14, 2010. Mental care stays are up in military.http://www.usatoday.com/news/military/2010-05-14-mental-health_N.htm Accessed June 24, 2012. [Google Scholar]
- 58.Department of Defense Suicide Prevention Task Force on the Prevention of Suicide by Members of the Armed Forces The challenge and the promise: strengthening the force, preventing suicide and saving lives. August 2010. http://www.health.mil/dhb/downloads/Suicide Prevention Task Force final report 8-23-10.pdf Accessed June 24, 2012.
- 59.McCall W.V. Insomnia is a risk factor for suicide: what are the next steps? Sleep. 2011;34(9):1149–1150. doi: 10.5665/SLEEP.1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fawcett J., Scheftner W.A., Fogg L. Time-related predictors of suicide in major affective disorder. Am J Psychiatry. 1990;147(9):1189–1194. doi: 10.1176/ajp.147.9.1189. [DOI] [PubMed] [Google Scholar]
- 61.Bjorngaard J.H., Bjerkeset O., Romundstad P., Gunnell D. Sleeping problems and suicide in 75,000 Norwegian adults: a 20 year follow-up of the HUNT I study. Sleep. 2011;34(9):1155–1159. doi: 10.5665/SLEEP.1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ribeiro J.D., Pease J.L., Gutierrez P.M. Sleep problems outperform depression and hopelessness as cross-sectional and longitudinal predictors of suicidal ideation and behavior in young adults in the military. J Affect Dis. 2012;136(3):343–350. doi: 10.1016/j.jad.2011.09.049. [DOI] [PubMed] [Google Scholar]
- 63.Centers for Disease Control and Prevention (CDC) Vital signs: overdoses of prescription opioid pain relievers—United States, 1999-2008. MMWR Morb Mortal Wkly Rep. 2011;60(43):1487–1492. [PubMed] [Google Scholar]
- 64.Bohnert A.S., Valenstein M., Bair M.J. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315–1321. doi: 10.1001/jama.2011.370. [DOI] [PubMed] [Google Scholar]
- 65.Maxwell J.C. The prescription drug epidemic in the United States: a perfect storm. Drug Alcohol Rev. 2011;30(3):264–270. doi: 10.1111/j.1465-3362.2011.00291.x. [DOI] [PubMed] [Google Scholar]
- 66.Paulozzi L.J., Weisler R.H., Patkar A.A. A national epidemic of unintentional prescription opioid overdose deaths: how physicians can help control it. J Clin Psychiatry. 2011;72(5):589–592. doi: 10.4088/JCP.10com06560. [DOI] [PubMed] [Google Scholar]
- 67.Centers for Disease Control and Prevention (CDC) CDC grand rounds: prescription drug overdoses: a U.S. epidemic. MMWR Morb Mortal Wkly Rep. 2012;61(1):10–13. [PubMed] [Google Scholar]
- 68.Seal K.H., Shi Y., Cohen G. Association of mental health disorders with prescription opioids and high-risk opioid use in US veterans of Iraq and Afghanistan. JAMA. 2012;307(9):940–947. doi: 10.1001/jama.2012.234. [DOI] [PubMed] [Google Scholar]
- 69.State of Washington Agency Medical Directors Group Interagency guideline on opioid dosing for chronic non-cancer pain: an educational aid to improve care and safety with opioid therapy: 2010 update. http://www.gencymeddirectors.wa.gov/Files/OpioidGdline.pdf Accessed June 24, 2012.
- 70.Franklin G.M., Mai J., Turner J., Sullivan M., Wickizer T., Fulton-Kehoe D. Bending the prescription opioid dosing and mortality curves: impact of the Washington State opioid dosing guideline. Am J Ind Med. 2012;55(4):325–331. doi: 10.1002/ajim.21998. [DOI] [PubMed] [Google Scholar]
- 71.Luoma J.B., Martin C.E., Pearson J.L. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry. 2002;159(6):909–916. doi: 10.1176/appi.ajp.159.6.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rutz W., von Knorring L., Walinder J. Frequency of suicide on Gotland after systematic postgraduate education of general practitioners. Acta Psychiatr Scand. 1989;80(2):151–154. doi: 10.1111/j.1600-0447.1989.tb01318.x. [DOI] [PubMed] [Google Scholar]
- 73.Rutz W., von Knorring L., Walinder J. Long-term effects of an educational program for general practitioners given by the Swedish Committee for the Prevention and Treatment of Depression. Acta Psychiatr Scand. 1992;85(1):83–88. doi: 10.1111/j.1600-0447.1992.tb01448.x. [DOI] [PubMed] [Google Scholar]
- 74.Szanto K., Kalmar S., Hendin H., Rihmer Z., Mann J.J. A suicide prevention program in a region with a very high suicide rate. Arch Gen Psychiatry. 2007;64(8):914–920. doi: 10.1001/archpsyc.64.8.914. [DOI] [PubMed] [Google Scholar]
- 75.McDowell A.K., Lineberry T.W., Bostwick J.M. Practical suicide-risk management for the busy primary care physician. Mayo Clin Proc. 2011;86(8):792–800. doi: 10.4065/mcp.2011.0076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Miller M., Barber C., Young M., Azrael D., Mukamal K., Lawler E. Veterans and suicide: a reexamination of the National Death Index–Linked National Health Interview Survey. Am J Public Health. 2012;102(S1):S154–S159. doi: 10.2105/AJPH.2011.300409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Busch K.A., Fawcett J., Jacobs D.G. Clinical correlates of inpatient suicide. J Clin Psychiatry. 2003;64(1):14–19. doi: 10.4088/jcp.v64n0105. [DOI] [PubMed] [Google Scholar]
- 78.Rudd M.D., Berman A.L., Joiner T.E., Jr Warning signs for suicide: theory, research, and clinical applications. Suicide Life Threat Behav. 2006;36(3):255–262. doi: 10.1521/suli.2006.36.3.255. [DOI] [PubMed] [Google Scholar]
- 79.Miller M. Preventing suicide by preventing lethal injury: the need to act on what we already know. Am J Public Health. 2012;102(Sl):e1–e3. doi: 10.2105/AJPH.2012.300662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Miller M., Azrael D., Barber C. Suicide mortality in the United States: the importance of attending to method in understanding population-level disparities in the burden of suicide. Annu Rev Public Health. 2012;33:393–408. doi: 10.1146/annurev-publhealth-031811-124636. [DOI] [PubMed] [Google Scholar]
- 81.Miller M., Azrael D., Hemenway D. Household firearm ownership and suicide rates in the United States. Epidemiology. 2002;13(5):517–524. doi: 10.1097/00001648-200209000-00006. [DOI] [PubMed] [Google Scholar]
- 82.Miller M., Azrael D., Hepburn L., Hemenway D., Lippmann S.J. The association between changes in household firearm ownership and rates of suicide in the United States, 1981-2002. Inj Prev. 2006;12(3):178–182. doi: 10.1136/ip.2005.010850. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Author Interview Video


