Abstract
Neurofibromatosis type 2 protein (NF2) has been shown to act as tumor suppressor primarily through its functions as a cytoskeletal scaffold. However, NF2 can also be found in the nucleus, where its role is less clear. Previously, our group has identified JC virus (JCV) tumor antigen (T-antigen) as a nuclear binding partner for NF2 in tumors derived from JCV T-antigen transgenic mice. The association of NF2 with T-antigen in neuronal origin tumors suggests a potential role for NF2 in regulating the expression of the JCV T-antigen. Here, we report that NF2 suppresses T-antigen protein expression in U-87 MG human glioblastoma cells, which subsequently reduces T-antigen-mediated regulation of the JCV promoter. When T-antigen mRNA was quantified, it was determined that increasing expression of NF2 correlated with an accumulation of T-antigen mRNA; however, a decrease in T-antigen at the protein level was observed. NF2 was found to promote degradation of ubiquitin bound T-antigen protein via a proteasome dependent pathway concomitant with the accumulation of the JCV early mRNA encoding T-antigen. The interaction between T-antigen and NF2 maps to the FERM domain of NF2, which has been shown previously to be responsible for its tumor suppressor activity. Co-immunoprecipitation assays revealed a ternary complex among NF2, T-antigen, and the tumor suppressor protein, p53 within a glioblastoma cell line. Further, these proteins were detected in various degrees in patient tumor tissue, suggesting that these associations may occur in vivo. Collectively, these results demonstrate that NF2 negatively regulates JCV T-antigen expression by proteasome-mediated degradation, and suggest a novel role for NF2 as a suppressor of JCV T-antigen-induced cell cycle regulation.
Introduction
Disruption of the Neurofibromatosis type 2 (NF2) gene, on human chromosome 22, leads to the development of the autosomal dominant disorder Neurofibromatosis type 2, characterized by the development of schwannomas, meningiomas, and ependymomas [1]. Though these tumors are typically benign, NF2 loss has been implicated in the progression of many malignant tumors including highly aggressive mesothelioma tumors in humans [2], [3] and mice with heterozygous loss of NF2 are prone to the formation of multiple highly metastatic tumors, predominantly osteosarcomas and fibrosarcomas [4]. Loss of NF2 in glial cultures can lead to hyperproliferation, and formation of tumors in animal models [5]–[7]. Expression of NF2 has been shown to be absent in certain human glioblastomas and reintroduction can greatly suppress their growth [8]–[10].
The NF2 tumor suppressor protein is a member of the ERM family of proteins, which primarily facilitate cell to cell adhesion [11]–[13]. NF2 is responsive to cell confluence and growth factor availability [14]–[16]. Consequently, NF2 aides in the maintenance of contact inhibition of cell growth and anchorage dependence, whereby loss of NF2 facilitates invasion and mobility of transformed cells [6], [17], [18], [28]. NF2 is different from prototypical tumor suppressor proteins, such as p53, in that it is not known to directly affect the cell cycle, but rather acts as a crucial link between the extracellular environment and cell signaling pathways [14], [19]. Theories on the tumor suppressive roles of NF2 have largely been restricted to its actions as a scaffolding protein, however NF2 can be found in the nucleus, where its nuclear localization appears to be mediated by the cell cycle [20]–[22].
Previously, we have discovered the interaction of NF2 with the major regulatory protein of the human polyomavirus, JC virus (JCV), large tumor antigen (T-antigen), in malignant peripheral nerve sheath tumors (mpnsts) derived from JCV T-antigen transgenic mice [23]. JCV persistently infects the majority of individuals worldwide and is the causative agent of the rare but fatal demyelinating disease, progressive multifocal leukoencephalopathy, PML [24]. In addition to its role in PML pathogenesis, JCV has exhibited oncogenic potential in cell culture and experimental animal models where T-antigen expression leads to a broad range of CNS malignancies, most notably the formation of neuronal and glial origin tumors including medulloblastomas, astrocytomas, and primitive neuroectodermal tumors. JCV DNA or T-antigen protein expression has been detected in a similarly broad range of human tumors including medulloblastomas, astrocytomas, ependymomas, as well as CNS lymphomas and tumors of the gastrointestinal tract [25].
Potential mechanisms of JCV T-antigen induced oncogenesis have focused on the ability of T-antigen to disrupt the activity of cell cycle regulatory proteins including p53 and Rb [26], T-antigen's enhancement of oncogenic signaling through the Wnt pathway by stabilizing key members, such as β-catenin, LEF-1, and c-myc [27], and its interaction with DNA repair proteins [28], [29], to name a few. Surprisingly, few mechanisms have been identified that can repress T-antigen-mediated oncogenesis and attention has mainly focused on transcriptional regulation of the JCV promoter (for review see [25]). In addition, many polyomaviruses, including JCV, encode a conserved miRNA targeting the viral early mRNA as an autoregulatory mechanism [30]. Other potential negative regulators of T-antigen expression include SF2/ASF, which inhibits alternative splicing of the JCV early transcript [31], and CBP which partners with p53 to enhance acetylation of T-antigen, affecting its stability [32], [33].
In this study, we provide a new mechanism of tumor suppression by NF2 and demonstrate inhibition of JCV T-antigen expression. Here, we show that NF2, specifically its FERM domain, negatively regulates JCV T-antigen protein levels via a proteasome-mediated pathway in U-87 MG human glioblastoma cells. Our findings also extend to clinically obtained human glioblastomas, where T-antigen, NF2, and p53, can be detected. Taken together, these results provide new insights into the function of NF2, and provide a potential pathway for inhibiting T-antigen function in glial cells.
Results
NF2 Suppresses T-antigen Protein Expression and JCV Promoter Activity
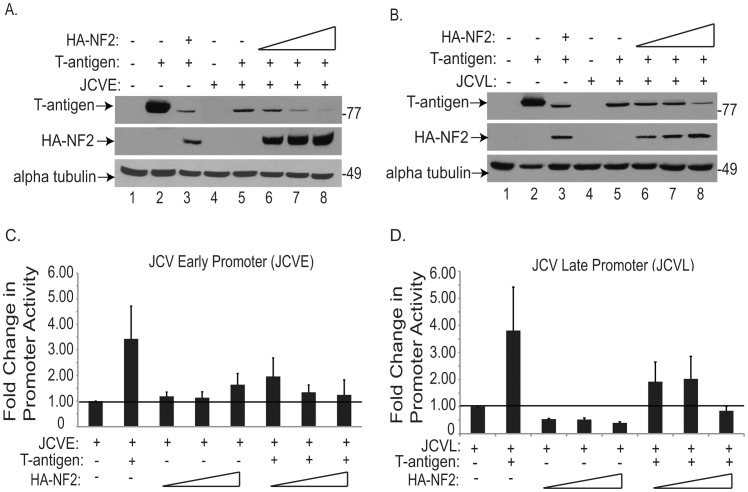
We previously reported that NF2 colocalizes with the JCV early regulatory protein, T-antigen, in the nucleus of malignant peripheral nerve sheath tumors found in JCV T-antigen transgenic mice [23]. Other tumor suppressor proteins, such as p53 and Rb, also share T-antigen as a nuclear binding partner. Typically these interactions inhibit p53 and Rb from acting as negative regulators of the cell cycle. However, p53 can also act as a negative regulator of JCV replication, via its interaction with the JCV promoter [34]. Here, we set out to examine if NF2 may have an effect on the expression of JCV T-antigen protein. To this end, human U-87 MG glioblastoma cells were transiently transfected with plasmids encoding JCV T-antigen and increasing amounts of HA tagged NF2 (HA-NF2). Immunoblotting of these cellular extracts revealed a dose-dependent decline of T-antigen protein expression occurring with increasing expression of NF2 (Figures 1A and 1B). However, when the reciprocal experiment was conducted in this cell culture system, NF2 expression was unaffected in the presence of increasing amounts of T-antigen (data not shown).
Figure 1. NF2 suppresses T-antigen protein expression and T-antigen mediated activation of JCVE and JCVL promoters.
U-87 MG glioblastoma cells were transiently transfected with luciferase reporter constructs encoding either the JCVE (a, c) or JCVL (b, d) promoters, and plasmids encoding JCV T-antigen or HA tagged NF2 (HA-NF2). Immunoblotting of protein lysates revealed a dose-dependent decline in the expression of T-antigen, in the presence of increasing amounts of HA-NF2 (a, b lanes 5–8). Extracts were also used to conduct luciferase assays to determine JCVE (c) or JCVL (d) activation in response to these various transfection conditions. Results are shown here as fold change in luciferase activity, relative to the activity of the promoter alone. NF2 does not appreciably affect the activities of either promoter, while T-antigen greatly enhances the activity of both promoters. In combination, NF2 does prevent T-antigen from enhancing the activities of JCVE and JCVL.
In parallel, we investigated the functional effect this decline of T-antigen protein would have on the activity of the JCV promoter. The JCV promoter is bidirectional, with the early promoter (JCVE) encoding the regulatory genes for large and small T-antigens, and the late promoter (JCVL) encoding capsid and accessory genes. Luciferase constructs containing the JCV promoter in either the early or late orientation were co-transfected into U-87 MG cells, along with expression plasmids for T-antigen and HA-NF2. The presence of increasing amounts of NF2 resulted in retention of basal promoter activity of the JCVE promoter (Figure 1C) and minor suppression of JCVL activity (Figure 1D). Since T-antigen activates its own promoter, supplementation with T-antigen enhanced the activity of both early and late promoters; however this effect was ameliorated in the presence of NF2.
To confirm whether the effect of NF2 on JCV promoter activity is due to the decrease in T-antigen levels rather than NF2 acting directly upon the viral promoter, we conducted a chromatin immunoprecipitation (ChIP) assay. For this assay, BSB8 cells, derived from a JCV T-antigen induced primitive neuroectodermal tumor in transgenic mice were utilized [35]. Immunoprecipitation of DNA:protein complexes with antibodies to HA-NF2 and T-antigen, followed by PCR amplification using primers specific for the JCV promoter, detected T-antigen in complex with the JCV promoter. However, HA-NF2 failed to precipitate this DNA region, indicating that NF2 does not directly bind the JCV promoter (data not shown). This result is consistent with a previous study whereby NF2 could not be detected in the chromatin containing fraction of the nucleus [22]. Cumulatively, this data suggests that NF2 downregulates JCV transcription via an indirect mechanism, by reducing T-antigen protein expression, so that T-antigen cannot subsequently enhance viral promoter activity.
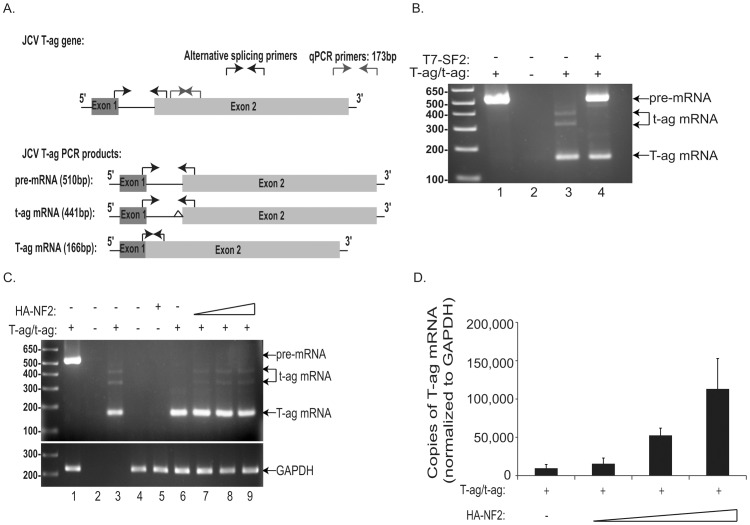
NF2 Facilitates the Accumulation of JCV T-antigen mRNA
To date, only a few proteins are capable of suppressing the typically robust expression of JCV T-antigen in tumor cells. One of these proteins, p53, can suppress T-antigen expression through suppression of the viral promoter [34]. However, based on our findings above we ruled out the possibility of NF2 acting as a negative viral transcriptional regulator. As mentioned earlier, the alternative splicing factor, SF2, has been shown to inhibit the splicing of JCV T-antigen pre-mRNA thus reducing expression of both large and small T-antigens [36]. In order to determine if NF2 functions as an inhibitor of splicing, we utilized primers that can discriminate among JCV T-antigen pre-mRNA, and large and small T-antigen mRNAs, as previously described (Figure 2A, and [36]). We detected large and small T-antigen mRNAs, but not their shared pre-mRNA, in cDNA derived from JCV T-antigen expressing BSB8 cells (Figure 2B). As shown previously, T-antigen pre-mRNA accumulated with co-transfection of T7 tagged SF2 (T7-SF2) (Figure 2B, lane 4), but not with HA-NF2 in U-87 MG cells (Figure 2C, compare lanes 6–9), suggesting that the mechanism by which NF2 suppresses T-antigen protein occurs downstream of alternative splicing events. In addition, the relative amount of mature T-antigen mRNA in U-87 MG cells co-transfected with T-antigen and HA-NF2 was determined using large T-antigen specific primers (Figure 2A) by quantitative real time PCR (qRT-PCR) analysis. We observed a positive correlation between NF2 overexpression and T-antigen mature mRNA levels (Figure 2B). This accumulation of untranslated T-antigen mRNA combined with a reduction in T-antigen at the protein level as seen above (Figure 1) suggests a blockage of T-antigen expression by NF2 through post transcriptional intervention.
Figure 2. NF2 leads to accumulation of T-antigen mRNA, but does not affect its alternative splicing.
Schematic showing all alternatively spliced forms of JCV T-antigen, including the pre-mRNA and both large and small T-antigen mRNAs, and location of primers used for PCR analysis are shown (A, black primers). PCR amplification of cDNA derived from T-antigen expressing BSB8 cells (B, lane 3), detected both large and small T-antigen mRNAs, but not pre-mRNA. Co-transfection of U-87 MG cells with expression plasmids for T-antigen and T7-SF2, an inhibitor of splicing, resulted in an accumulation of pre-mRNA and a reduction in large and small T-antigen mRNAs (B, lane 4). Co-transfection with T-antigen and increasing amounts of HA-NF2 plasmids did not alter the pattern of mRNAs detected (C, compare lanes 6 to 7–9). Q-PCR analysis was also conducted for T-antigen copy number (A, grey primers), expressed as copies of T-antigen mRNA per copy number of the control mRNA GAPDH*, with standard deviations of the mean shown here (D). This assay revealed a dose dependent accumulation of T-antigen mRNA in the presence of NF2. *Note that GAPDH primers used in Panel C only detect human and not mouse GAPDH, therefore a band representing GAPDH from the BSB8 mouse cell line was not detected (C, lane 3).
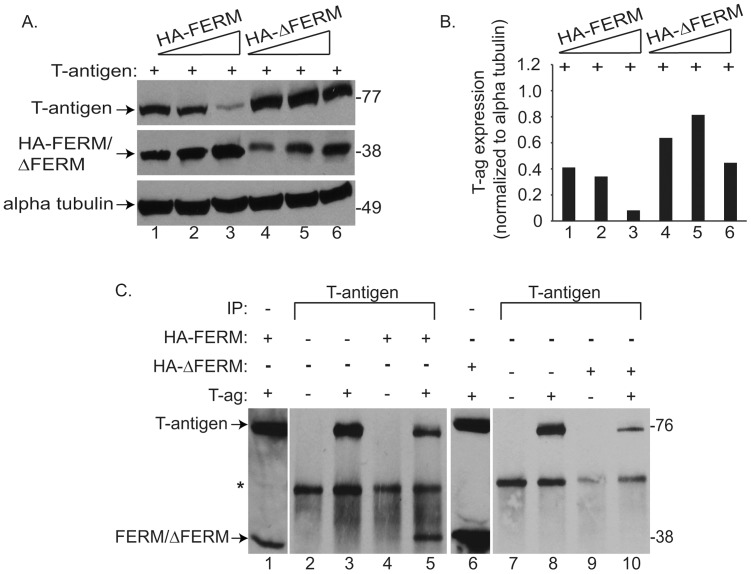
The FERM Domain of NF2 is Responsible for its Binding and Degradation of T-antigen
To establish the region of NF2 responsible for its interactions with T-antigen, we utilized two truncations mutants of full length NF2, one containing the amino terminal FERM (Band 4.1, ezrin, radixin, moesin) domain (HA-FERM) and the other representing the C terminal half of the NF2 protein (HA-ΔFERM). The FERM domain of NF2 is responsible for its anchorage to the plasma membrane and actin binding [37]–[39]. Further, this domain is suggested to be the tumor suppressive region of NF2 in that it is necessary to prevent cellular proliferation in response to mitogenic signaling, as demonstrated by reductions in growth factor receptor signaling, MTT conversion, and colony formation in soft agar [22], [38], [40], [41]. Co-transfection of these NF2 mutants into U-87 MG cells along with T-antigen, revealed a dose-dependent decline in T-antigen levels with the HA-FERM mutant, similar to full length NF2 (Figure 3A, lanes 1–3), while T-antigen expression remained unaltered in the presence of the HA-ΔFERM mutant (Figure 3A, lanes 4–6). Further, co-immunopreciptation (Co-IP) assays in lysates from these cells revealed that T-antigen binds to the FERM, but not ΔFERM region of NF2 (Figure 3C, compare lanes 5 and 10). These studies further suggest that the FERM domain of NF2 is required for its tumor suppressive capabilities, specifically in T-antigen mediated malignancies.
Figure 3. NF2 utilizes a proteasomal-dependent mechanism to promote the degradation of ubiquitin-bound T-antigen.
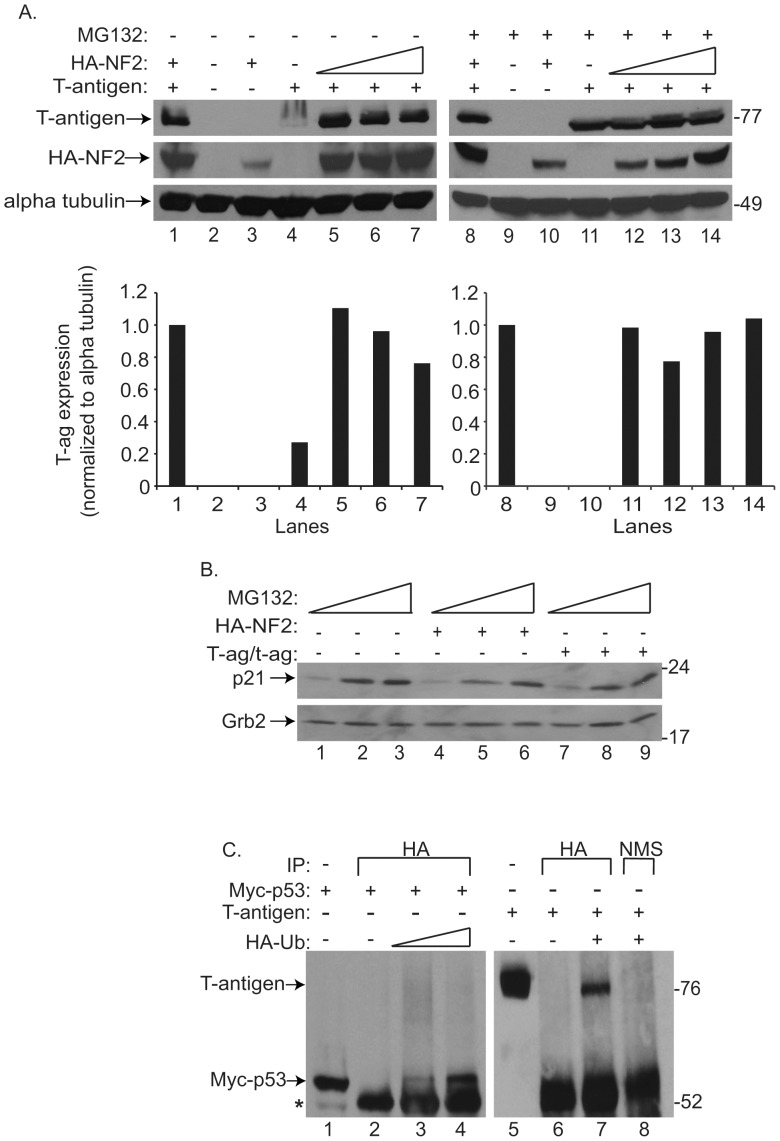
To determine if NF2 utilizes the proteasome to enhance T-antigen protein turnover, U-87 MG cells, transfected with HA-NF2 and T-antigen, were treated with the general proteasome inhibitor, MG132 (A, right), or vehicle (A, left). As shown earlier (Figures 1A and 1B), enhanced expression of NF2, suppresses that of T-antigen (A, left top and bottom). However, this affect was abolished with the addition of MG132 (A, right top and bottom). Band intensity representing T-antigen expression was quantified, normalized to its loading control, and shown as fold change relative to lane 1 (A, bottom left and right). p21, a protein known to be subjected to proteasomal degradation, was immunoblotted for in extracts of untransfected U-87 MG cells or those transfected with HA-NF2 or T-antigen alone, exposed to increasing concentrations of MG132 (B). Expression of this protein increased with drug exposure (B, compare lanes 1, 4, and 7 to subsequent lanes), indicating the effectiveness of MG132 to inhibit degradation of proteins subjected to proteasomal degradation. The ability of T-antigen to bind to ubiquitin, a key post-translational protein attached to proteasome targeted proteins, was assessed by Co-IP. U-87 MG cells were transfected with combinations of Myc tagged p53 (Myc-p53), T-antigen, and HA tagged ubiquitin (HA-Ub), protein complexes were immunoprecipitated with an anti HA antibody or normal mouse serum. Subsequent immunoblotting demonstrated that p53 and T-antigen were not precipitated by the HA antibody alone (C, lanes 2 and 6), but did when co-transfected with HA-Ub (C, lanes 3–4 and 7). Collectively, these results provide the first evidence that T-antigen can bind ubiquitin and suggest that T-antigen is subjected to proteasome-mediated degradation.
NF2 Promotes Proteasomal-mediated Degradation of T-antigen
NF2 interacts with a wide array of cellular proteins, including the ubiquitin ligases Mdm2 and DCAF1 [22], [42] to promote the degradation of targeted proteins via the proteasome. To determine whether NF2 functions through the proteasome to regulate T-antigen expression, we exposed U-87 MG cells, transfected with T-antigen and HA-NF2 constructs, to the proteasomal inhibitor, MG132. Increasing amounts of NF2 led to a decline in T-antigen protein in samples treated with vehicle alone (Figure 4A, left), while treatment with MG132 ameliorated these affects, such that T-antigen expression was unaltered in the presence of NF2 (Figure 4A, right). Increasing amounts of MG132 led to an accumulation of p21, another protein known to be regulated by this pathway (Figure 4B), indicating the stabilization of proteins subjected to proteasomal degradation. To date, this is the first evidence of proteasomal involvement in the stability of any polyomavirus tumor antigen. A key post-translational modification involved in the targeting of a protein to the proteasome is ubiquitination. To evaluate the ability of JCV T-antigen to bind ubiquitin we conducted a Co-IP assay with T-antigen and an HA-tagged ubiquitin construct (HA-Ub). Using p53 as a protein known to bind ubiquitin, we were able to demonstrate the binding of T-antigen to ubiquitin (Figure 4C, lane 7). Together this data implicates that T-antigen may be subjected to destruction via the ubiquitin-proteasome and that NF2 can enhance this process.
Figure 4. NF2 requires its FERM domain to bind and suppress T-antigen expression.
To elucidate the domain of NF2 responsible for the downregulation of T-antigen protein expression, U-87 MG cells were cotransfected with T-antigen and increasing amounts of either HA-FERM or HA-ΔFERM NF2 truncation mutants (A). Immunoblotting revealed a dose-dependent decline in T-antigen expression in the presence of HA-FERM (A, lanes 1–3), but not HA-ΔFERM (A, lanes 4–6), indicating that the FERM domain is necessary for this mechanism. Band intensity representing T-antigen expression was quantified, normalized to its loading control (B). Lysates from U-87 MG cells co-transfected with T-antigen, HA-FERM, and HA-ΔFERM were utilized for Co-IP with T-antigen antibodies (C). In this assay, we demonstrate the ability of T-antigen to bind to the FERM (C, lane 5), but not ΔFERM (C, lane 10) region of NF2, further implicating FERM to be the necessary region facilitating the interaction among NF2 and T-antigen.
NF2, T-antigen, and p53 Interact in Human Glioblastomas
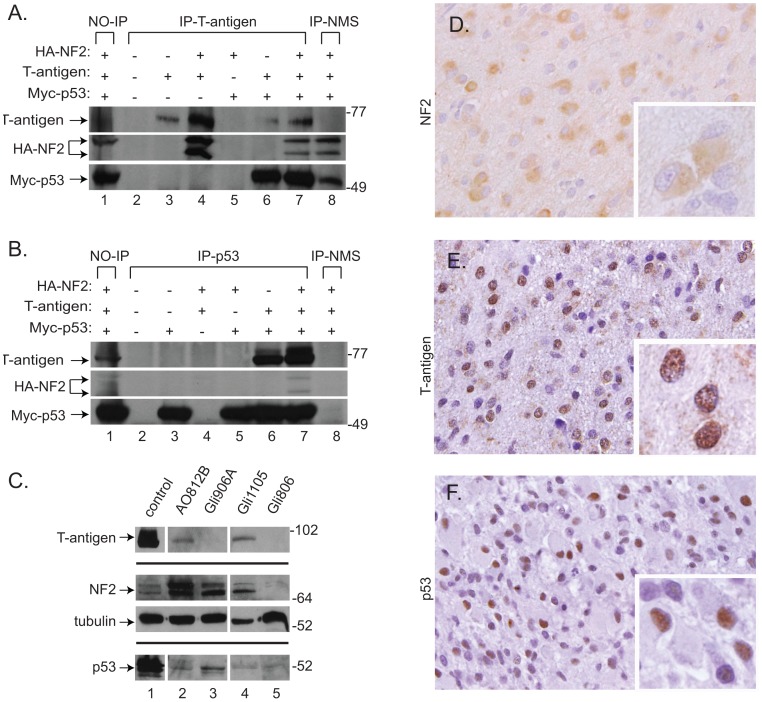
NF2, T-antigen, and p53 were previously shown to form a ternary complex in T-antigen positive tumors derived from JCV T-antigen transgenic mice [23]. Yet, it has not been determined if these proteins interact in human tumors or if NF2 and p53 can bind together in the absence of T-antigen. To this end, Co-IP assays were conducted using antibodies against both T-antigen and Myc-tagged p53 (Myc-p53) in extracts from transfected U-87 MG glioblastoma cells. T-antigen was observed to bind to both NF2 and p53, individually (Figure 5A, lanes 4 and 6 respectively) and in complex (Figures 5A and 5B, lane 7). Interestingly, binding between NF2 and p53 independent of T-antigen was not observed (Figure 5B, compare lane 5 to 7), although there is mounting evidence of a tumor suppressive synergy that exists between them [4], [43], [44].
Figure 5. NF2, T-antigen, and p53 complex in human glioblastoma cells and are detected in high grade glioma samples.
Immunoprecipitation of HA-NF2, T-antigen, and Myc-p53 proteins was performed using extracts from transiently transfected U-87 MG cells with antibodies against T-antigen (A), p53 antibody (B), or normal mouse serum as negative controls (A and B, lane 8), followed by immunoblotting to detect the presence of T-antigen, HA-NF2, or Myc-p53. As previously described, T-antigen binds NF2 (A, lane 4) and p53 (A and B, lane 6), individually. These proteins form a ternary complex (A and B, lane 7), however NF2 and p53 do not bind in the absence of T-antigen (B, lane 5). Protein lysates were prepared from fresh tissue specimens of surgically resected high grade gliomas utilized for immunoblotting revealed the presence of NF2 and p53 in an anaplastic oligodendroglioma (A, lane 2), as well as three glioblastomas (C, lanes 3–5). T- antigen was also detected in two of these tumor samples (C, lanes 2 and 4). Further, tumor tissue obtained from surgically resected high grade gliomas tumor, was paraffin embedded and used for immunohistochemistry. In the glioblastoma sample shown in Panel C, lane 4 (Gli1105), we detected cytoplasmic NF2 expression (Figure 5D). In comparable sections of the same glioblastoma sample T-antigen (E) and p53 (F) were localized to the nucleus. Panels D-F, original magnification x400; insets, original magnification, x1000; hematoxylin counterstain.
We then assayed human high grade gliomas resected from patients for the presence of these proteins. Using immunoblotting of fresh tumor tissue, we observed the presence of significant levels of NF2 in three of four high grade glioma tumors analyzed while p53 levels were more variable (Figure 5C). In addition, we detected T-antigen protein in one anaplastic oligodendroglioma (AO812B) and one grade IV glioblastoma (Gli1105). Interestingly, high levels of NF2 and p53 were detected in another glioblastoma sample (Gli906A) in the absence of T-antigen (Figure 5C). Immunohistochemical analysis of parallel sections from one of the T-antigen positive samples (Gli1105) revealed a predominantly cytoplasmic pattern for NF2, while T-antigen and p53 were detected in the nuclei of a subset of tumor cells (Figure 5D–F). NF2 is typically examined in tumor tissues at the gene level to screen for gene deletion, i.e. LOH or mutational inactivation. However, here we examine the role of the NF2 protein as a tumor suppressor, rather than its loss of function. We were able to detect NF2 by immunohistochemistry and Western blotting in Gli1105, and as shown in Figure 5C, varying levels of NF2 are seen in the tumor tissues including some with a more prominent upper band likely representing the phosphorylated form of the protein, suggesting that total levels, as well as phosphorylation status may affect its function in human tumors.
Discussion
NF2 is a putative tumor suppressor for glioblastoma growth, in that it is lost in many patient samples and cell lines. Reintroduction of NF2 in these cells can significantly inhibit cell proliferation, cellular transformation, and tumorigenesis [8]–[10]. While NF2 is not solely localized in the cytoplasm, the potential functions of nuclear NF2 remain unclear. Previous studies from our group indicate that the JCV regulatory protein, T-antigen, binds to NF2, but the functional significance of this interaction had not been elucidated [23]. Here, we provide evidence for a novel role of NF2 as an inhibitor of oncogenic JCV T-antigen expression in glioblastoma cells.
NF2 joins a list of only two other proteins, including p53 and SF2, that downregulate the expression of JCV T-antigen. P53 does so by binding to the JCV bidirectional promoter and preventing the transcription of T-antigen [34]. Since we could not detect NF2 interaction with the JCV promoter by ChIP assay (data not shown) nor observe an impact on promoter activity in the absence of T-antigen (Figures 1D and 1E), regulation of T-antigen by NF2 at the level of the JCV promoter appears unlikely. SF2, on the other hand, inhibits the processing of T-antigen pre-mRNA into its mature form needed for protein translation [36]. The ability for NF2 to serve in a similar capacity is also unlikely as we were unable to observe an accumulation of T-antigen pre-mRNA upon overexpression of NF2 (Figure 2C). Instead, our data suggests that NF2, specifically its tumor suppressive FERM domain, facilitates the proteasomal degradation of ubiquitin bound T-antigen. However, the accumulation of T-antigen mRNA that we observed in the presence of NF2 (Figure 2D), suggests the possibility that NF2 may also inhibit T-antigen at the level of translation. NF2 has been previously implicated to act as an inhibitor of translation [41], [45], [46]. Conversely, expression of SV40 T-antigen can activate cap-dependent protein translation [47]. Both large and small T-antigens appear to be downregulated by NF2 (Beltrami et al, unpublished observations) suggesting a common mechanism for their inhibition and, indeed, they do share a portion of their 5′ mRNA sequences and amino termini (Beltrami, unpublished observation). Further defining NF2′s potential to regulate proteasome cargo or perhaps mRNA levels, as well as identifying its cellular target proteins, are the logical next steps.
Though NF2 is traditionally viewed as a cytoplasmic scaffold, it also has tumor suppressive roles in the nucleus. NF2 has not been shown to directly regulate the cell cycle; however its presence promotes cell cycle arrest in schwannoma, primary endothelial, mesothelioma, and patient-derived meningioma cells [14], [22], [48], [49]. An intriguing protein of interest, which may link NF2 to the cell cycle, is the cyclin dependent kinase inhibitor, p21. Through its interactions with Mdm2, NF2 enhances the transcription of p21, a well established inhibitor of cell cycle progression [42], [50]. Furthermore, NF2 inhibits PAK2 from acting as a positive transcriptional regulator of the cell cycle enhancer, cyclin D1 [51]. Interestingly, T-antigen promotes the stabilization of Rac1, another cyclin D1 enhancer [52], [53]. These studies have led some to speculate that NF2 may have a novel role as an upstream cell cycle regulator [22].
While NF2 is typically a cytoplasmic protein, we have previously shown its nuclear co-localization with T-antigen in tumors derived from JCV T-antigen transgenic mice. The pattern of NF2 localization in the human high grade gliomas we examined was predominantly cytoplasmic, though examination of a more extensive set of clinical samples would be informative. In any case, many prominent nuclear proteins are regulated within the cytoplasmic compartment, p53 regulation by MDM2 is one relevant example, and a portion of T-antigen can be detected within the cytoplasm as well as in the membrane fraction of cells. A direct interaction between NF2 and p53 was not observed in the absence of T-antigen, but previous studies have suggested significant overlap between these two pathways. Interestingly, NF2 and p53 were detected in one of our glioblastoma tissue samples (Gli906A) by immunoblotting, even in the absence of T-antigen (Figure 5C). The NF2 and p53 genes are linked in the mouse genome, and loss of both genes leads to the development of multiple highly metastatic tumors [4], [44], [54] and in meningiomas, the loss of functional NF2 and p53 correlate with enhanced tumor grade [43]. At the molecular level, NF2 was shown to upregulate transcription of the p53 gene, stabilize p53 protein, and sensitize cells to p53 induced apoptosis [42]. Since NF2 and p53 do not appear to directly bind together, other cellular mediators must facilitate their interactions. One such protein may include Mdm2, the p53 ubiquitin ligase, which has been shown to bind both p53 and NF2 in isolation [42].
In our limited analysis of patient derived gliomas, we have detected both nuclear and cytoplasmic interactions among NF2 and T-antigen. There are several possibilities as to the outcome of these interactions. Nuclear NF2, in its binding to T-antigen, may prevent it from sequestering p53 and Rb and overriding their control of the cell cycle. To explore this possibility, we will investigate if NF2 can aide T-antigen expressing gliomas in regaining control of the cell cycle. In light of our recent data on the proteasomal mediated degradation of T-antigen, perhaps cytoplasmic NF2 acts as a chaperone protein to guide ubiquitin-tagged T-antigen to the proteasome. In which case, the ubiquitin ligases known to interact with NF2, namely Mdm2 and DCAF1, would be attractive candidates to explore for their ability to degrade T-antigen. Further, we were not able to determine if the p53 we detected by either immunoblotting or immunohistochemistry is wild type or mutant in these glioma samples. Previously, we have observed wild-type p53 in nervous system tumors from T-antigen transgenic mice and have demonstrated that T-antigen only interacts with wild type and not mutant p53 [23], [35], [55]. We therefore hypothesize that T-antigen would associate with wild-type p53. However, immunohistochemical detection in formalin-fixed tissue does not allow the distinction between wild-type and mutant forms of p53, therefore other means, i.e. gene sequencing or immunoprecipitation analysis would be necessary to determine the p53 status of the human tumors.
Alteration of p53 remains one of the key genetic changes in human glioblastoma and its mutation or loss has been reported in some percentage of all subtypes of glioblastomas thus far described [56]. While NF2 inactivation has been linked to schwannomas and other tumors such as mesotheliomas, loss of NF2 expression appears to be infrequent in human glioblastoma, though it has been reported in up to one third of cases [10]. Indeed, we have observed high levels of NF2 expression in high grade gliomas. However, it is important to establish whether the presence of a tumor suppressor protein such as p53 or NF2 indicates a functional protein, as the pathway may be blocked downstream and thus unable to halt cell proliferation. Should the tumor suppressor pathway be intact, it may be possible to alter the blockage and thus restore cell cycle control. Visualizing the interactive nature of these proteins in human samples provides us with a better understanding of the complex interplay among tumor suppressors and oncoproteins that shape glioblastoma growth.
Materials and Methods
Ethics Statement - clinical Samples
Human brain tumor tissue was obtained from surgical resections or brain biopsy under the approval of the Temple University Institutional Review Board (IRB). Written informed consent for all samples was obtained and any clinical samples presented in this study have been coded and deidentified.
Plasmids and Cell Lines
The JCVE and JCVL promoter regions, from the Mad-4 strain of JC virus were cloned into separate pGL3 Basic Vectors, upstream of the luc2P reporter gene [57]. The expression constructs for JCV T-antigen and human p53, were created by PCR amplification and cloning into the Kpn1 and EcoR1 sites, and the EcoR1 and Not1 sites of pcDNA6/myc-His vector (Invitrogen), respectively. The HA-tagged NF2 expression construct was created by cloning into the pcDNA3 vector as described previously [23]. The T7 tagged SF2 (T7-SF2) expression construct was a gift from Ilker Sariyer [36], and the HA-tagged ubiquitin plasmid (HA-Ub) was purchased (Addgene). The U-87 MG glioblastoma cell line was obtained from the ATCC and cultured in 1x DMEM-low glucose media (GIBCO), with 10% fetal bovine serum, and 0.5 µg/µl gentamicin. The JCV T-antigen positive cell line used in this study, BSB8, was derived from JCV T-antigen transgenic mice [35], and cultured in the same media.
Antibodies
Antibodies used for immunoblotting in this study included: HA-11 mouse monoclonal (clone 12CA5, Boehringer Mannheim), SV40 T-antigen Ab2 mouse monoclonal, which cross-reacts with JCV T-antigen, (clone pAb416, Oncogene Research Products), Myc mouse monoclonal (clone 9B11, Cell Signaling), p21 rabbit polyclonal (sc-756, Santa Cruz Biotechnologies) and alpha tubulin mouse monoclonal (clone B-5-1-2, Sigma Aldrich). For immunoprecipitation the following antibodies were utilized: SV40 T-antigen Ab2 mouse monoclonal, HA-11 mouse monoclonal, and p53 Ab-1 mouse monoclonal (clone pAb421, Wilex, Cambridge, MA). Immunohistochemistry was performed using NF2 rabbit polyclonal (C-18, Santa Cruz Biotechnologies), p53 mouse monoclonal (D07, Dako) and T-antigen mouse monoclonal (SV40 T-antigen Ab2). Patient samples were immunoblotted using NF2 rabbit polyclonal (C-18), T-antigen mouse monoclonal (SV40 T-antigen Ab2), and p53 sheep polyclonal (Ab-7, Millipore, Billerica, MA).
Luciferase Assay
U-87 MG cells were transfected in quadruplicate with increasing concentrations of expression plasmids for HA-NF2, T-antigen, and JCVE or JCVL reporter plasmids using Fugene 6 transfection reagent (Roche) in Optimem media (GIBCO) and total amounts of DNA were normalized with pcDNA3.1 (empty vector). Cells were harvested 48 hours post transfection in 1× passive lysis buffer (Promega) and luciferase activity was conducted with 10 µg of protein lysates using the Luciferase Assay System kit (Promega), measured with a Femtomaster FB 12 luminometer (Zylux Co.), and quantified to give a RLU/sec/10 µg of protein.
Immunoblotting
Whole cell extracts were prepared in 1x Promega passive lysis buffer or 0.5% NP-40, TNN buffer containing mammalian protease inhibitor cocktail (Sigma Aldrich). Proteins were separated by 9 or 12% SDS-PAGE, and transferred to nitrocellulose or PVDF membranes. Blots were blocked in 10% milk in 1× PBST, then incubated in primary antibodies for 2 hours at room temperature or overnight at 4°C. This was followed by washing, then incubation with secondary antibodies conjugated to horseradish peroxidase for detection with ECL chemiluminescence (GE Healthcare) or secondary antibodies conjugated to alkaline phosphatase for detection with CDP-Star (Perkin Elmer). Bands were quantified, using ImageJ software, and normalized to loading control.
Co-immunoprecipitation
U-87 MG cells were transfected with expression plasmids as described in their respective figures. Forty-eight hours after transfection, whole cell extracts were prepared in 0.5% NP-40, TNN buffer containing mammalian protease inhibitor cocktail (Sigma Aldrich) and 0.1 µg/µl DNase1 (Roche). 150 µg of protein lysates were incubated overnight at 4°C with 1 µg of antibodies against either p53 (Ab-1), HA-11 tag, or T-antigen (SV40 T-antigen Ab2). Immunocomplexes were isolated by incubation with Pansorbin cells (Calbiochem) in TNN buffer, at 4°C for 2 hours. Complexes were then washed 3–4 times in TNN buffer, eluted in 2× SDS-PAGE sample buffer and subjected to immunoblot analysis.
Proteasomal Inhibition Assay
U-87 MG cells were transfected with plasmids encoding T-antigen and increasing amounts of HA-NF2. Media was then supplemented with either 10 µM the proteasome inhibitor MG132 (Calbiochem) in DMSO or an equal amount of DMSO for 8 hours before harvesting. Whole cell extracts were prepared 48 h after transfection in TNN buffer and immunoblotted to detect T-antigen, HA-NF2, and alpha tubulin expression. In parallel, U-87 MG, untrasfected or transfected with either HA-NF2 or T-antigen plasmids, were exposed to DMSO or MG132 in DMSO (1 or 10 µM) for 8 hours. Prepared extracts were immunoblotted for the detection of p21 expression.
Alternative Splicing PCR and qRT-PCR
RNA was extracted from U-87 MG cells transfected with either HA-NF2, T-antigen, or T7-SF2 constructs alone, or in combination, using the RNeasy kit (Qiagen), following manufacturer’s instructions. Samples were then treated with DNAse 1 (Roche) and RNAse inhibitor (Roche). Samples were subjected to PCR to verify absence of DNA contamination with primers specific for human GAPDH DNA: forward primer 5′ GAAGATGGTGATGGGATTTC 3′, reverse primer 5′ GAAGGTGAAGGTCGGAGTC 3′ at 50°C for 2 min (1×), 95°C for 10 min (1×), 95°C for 30 s/53°C for 30 s (45×), and 4°C for 1 min. When DNA was undetectable in these RNA samples, the reverse transcriptase enzyme from the Moloney Murine Leukemia Virus (Mo-MuLV RT), dNTPs, and random hexamers (Invitrogen) were used to synthesize cDNA. A portion of this cDNA was used for PCR reactions with primers to detect alternatively spliced forms of JCV T-antigen as described previously [36]: forward (4801–4780) 5′-CCTGATTTTGGTACATGGAA-3′, and reverse (4291–4313) 5′-GTGGGGTAGAGTGTTGGGATCCT-3′. The remaining cDNA was used for Q-PCR analysis of T-antigen mRNA copy number. The following primers (20 µM) and a FAM fluorophore labeled mRNA probe (10 µM) specific to JCV T-antigen were used in the PCR reaction: forward primer (4255–4274) 5′ AGTCTTTAGGGTCTTCTACC 3′, reverse primer (4408–4427) 5′ GTGCCAACCTATGGAACAG 3′, probe (4303–4327) 5′ FAM-AGTGTTGGGATCCTGTGTTTTCATCATC-BHQ1 3′. The PCR conditions for T-antigen amplification were 50°C for 2×min (1×), 95°C for 10×min (1×), 95°C for 15 s (45×), and 60°C for 1 min (1×). The standard mRNA copy number for each reaction was normalized to the average GAPDH copy number for those reaction conditions. The primers and probes used for the GAPDH PCR reactions 5′-HEX-CAAGCTTCCCGTTCTCAGCC-BHQ1–3′. All q-PCR reactions were performed in Universal Taq Man PCR Master Mix (Applied Biosystems) and amplified using the iCycler thermocycler (BioRad Laboratories).
Immunohistochemistry
Patient tumor resection samples were fixed in formalin for 24 hour, embedded in paraffin, and sectioned into 4µm slices using a Microm HM315 (Fisher Scientific). Paraffin was melted and slides were cleared in xylenes, and rehydrated in descending concentrations of ethanol. Antigen retrieval was conducted by warming slides in citrate buffer at 95°C for 30 min. Endogenous peroxidases were quenched in a solution of methanol and 30% peroxide for 20×min. Slides were blocked in normal goat or normal horse serum, for rabbit and mouse antibodies, respectively. Primary antibodies to NF2 (C-18), p53 (D-07) and T-antigen (SV40 T-antigen Ab2) were incubated on the slides overnight in a humidified chamber. For immunohistochemical analysis, slides were incubated with the appropriate biotinylated secondary antibody, followed avidin-biotin complexes for 1hr (Vector Laboratories). Slides were developed using DAB (Sigma Aldrich), dehydrated, counter stained with hematoxylin, mounted with Permount, and visualized by bright field microscopy.
Acknowledgments
The authors wish to thank past and present members of the Department of Neuroscience/Center for Neurovirology for their support and sharing of ideas and reagents. We would also like to thank the Temple University Neurosurgery Tumor Bank for providing clinical samples of glioblastoma.
Funding Statement
This investigation was sponsored by the National Institutes of Health under a Ruth L. Kirchstein National Research Service Award (1T32MH079785) providing support to Sarah Beltrami. This study utilized services offered by core facilities of the Comprehensive NeuroAIDS Center (CNAC NIMH Grant Number P30MH092177) at Temple University School of Medicine. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Martuza RL, Eldridge R (1988) Neurofibromatosis 2 (bilateral acoustic neurofibromatosis). N Engl J Med 318(11): 684–8. [DOI] [PubMed] [Google Scholar]
- 2. Evans DG, Huson SM, Donnai D, Neary W, Blair V, et al. (1992) A clinical study of type 2 neurofibromatosis. Q J Med 84(304): 603–18. [PubMed] [Google Scholar]
- 3. Sekido Y (2011) Inactivation of Merlin in malignant mesothelioma cells and the Hippo signaling cascade dysregulation. Pathol Int 61(6): 331–44. [DOI] [PubMed] [Google Scholar]
- 4. McClatchey AI, Saotome I, Mercer K, Crowley D, Gusella JF, et al. (1998) Mice heterozygous for a mutation at the Nf2 tumor suppressor locus develop a range of highly metastatic tumors. Genes Dev 12(8): 1121–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Morrison H, Sperka T, Manent J, Giovannini M, Ponta H, et al. (2007) Merlin/neurofibromatosis type 2 suppresses growth by inhibiting the activation of Ras and Rac. Cancer Res 67(2): 520–7. [DOI] [PubMed] [Google Scholar]
- 6. Johnson KC, Kissil JL, Fry JL, Jacks T (2002) Cellular transformation by a FERM domain mutant of the Nf2 tumor suppressor gene. Oncogene 21(39): 5990–7. [DOI] [PubMed] [Google Scholar]
- 7. Houshmandi SS, Emnett RJ, Giovannini M, Gutmann DH (2009) The neurofibromatosis 2 protein, merlin, regulates glial cell growth in an ErbB2- and Src-dependent manner. Mol Cell Biol 29(6): 1472–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lee H, Kim D, Dan HC, Wu EL, Gritsko TM, et al. (2007) Identification and characterization of putative tumor suppressor NGB, a GTP-binding protein that interacts with the neurofibromatosis 2 protein. Mol Cell Biol 27(6): 2103–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lau YK, Murray LB, Houshmandi SS, Xu Y, Gutmann DH, et al. (2008) Merlin is a potent inhibitor of glioma growth. Cancer Res 68(14): 5733–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Morales FC, Molina JR, Hayashi Y, Georgescu MM (2010) Overexpression of ezrin inactivates NF2 tumor suppressor in glioblastoma. Neuro Oncol 12(6): 528–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rouleau GA, Merel P, Lutchman M, Sanson M, Zucman J, et al. (1993) Alteration in a new gene encoding a putative membrane-organizing protein causes neurofibromatosis type 2. Nature 363(6429): 515–21. [DOI] [PubMed] [Google Scholar]
- 12. Trofatter JA, MacCollin MM, Rutter JL, Murrell JR, Duyao MP, et al. (1993) A novel moesin-, ezrin-, radixin-like gene is a candidate for the neurofibromatosis 2 tumor suppressor. Cell 75(4): 826. [DOI] [PubMed] [Google Scholar]
- 13. Tsukita S, Yonemura S (1997) ERM (ezrin/radixin/moesin) family: from cytoskeleton to signal transduction. Curr Opin Cell Biol 9(1) 70–5: 5. [DOI] [PubMed] [Google Scholar]
- 14. Morrison H, Sherman LS, Legg J, Banine F, Isacke C, et al. (2001) The NF2 tumor suppressor gene product, merlin, mediates contact inhibition of growth through interactions with CD44. Genes Dev 15(8): 968–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Shaw RJ, Paez JG, Curto M, Yaktine A, Pruitt WM, et al. (2001) The NF2 tumor suppressor, merlin, functions in Rac-dependent signaling. Dev Cell 1(1): 63–72. [DOI] [PubMed] [Google Scholar]
- 16. Grönholm M, Teesalu T, Tyynelä J, Piltti K, Böhling T, et al. (2005) Characterization of the NF2 protein merlin and the ERM protein ezrin in human, rat, and mouse central nervous system. Mol Cell Neurosci 28(4): 683–93. [DOI] [PubMed] [Google Scholar]
- 17. McClatchey AI (2003) Merlin and ERM proteins: unappreciated roles in cancer development? Nat Rev Cancer 3(11): 877–83. [DOI] [PubMed] [Google Scholar]
- 18. Bosco EE, Nakai Y, Hennigan RF, Ratner N, Zheng Y (2010) NF2-deficient cells depend on the Rac1-canonical Wnt signaling pathway to promote the loss of contact inhibition of proliferation. Oncogene 29(17): 2540–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. McClatchey AI, Giovannini M (2005) Membrane organization and tumorigenesis–the NF2 tumor suppressor, Merlin. Genes Dev 19(19): 2265–77. [DOI] [PubMed] [Google Scholar]
- 20. Kressel M, Schmucker B (2002) Nucleocytoplasmic transfer of the NF2 tumor suppressor protein merlin is regulated by exon 2 and a CRM1-dependent nuclear export signal in exon 15. Hum Mol Genet 11(19): 2269–78. [DOI] [PubMed] [Google Scholar]
- 21. Muranen T, Grönholm M, Renkema GH, Carpén O (2005) Cell cycle-dependent nucleocytoplasmic shuttling of the neurofibromatosis 2 tumour suppressor merlin. Oncogene 24(7): 1150–8. [DOI] [PubMed] [Google Scholar]
- 22. Li W, You L, Cooper J, Schiavon G, Pepe-Caprio A, et al. (2010) Merlin/NF2 suppresses tumorigenesis by inhibiting the E3 ubiquitin ligase CRL4(DCAF1) in the nucleus. Cell 140(4): 477–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Shollar D, Del Valle L, Khalili K, Otte J, Gordon J (2004) JCV T-antigen interacts with the neurofibromatosis type 2 gene product in a transgenic mouse model of malignant peripheral nerve sheath tumors. Oncogene 23(32): 5459–67. [DOI] [PubMed] [Google Scholar]
- 24. Padgett BL, Walker DL, ZuRhein GM, Hodach AE, Chou SM (1976) JC Papovavirus in progressive multifocal leukoencephalopathy. J Infect Dis 133(6): 686–90. [DOI] [PubMed] [Google Scholar]
- 25. White MK, Gordon J, Reiss K, Del Valle L, Croul S, et al. (2005) Human polyomaviruses and brain tumors. Brain Res Brain Res Rev 50(1): 69–85. [DOI] [PubMed] [Google Scholar]
- 26. Krynska B, Gordon J, Otte J, Franks R, Knobler R, et al. (1997) Role of cell cycle regulators in tumor formation in transgenic mice expressing the human neurotropic virus, JCV, early protein. J Cell Biochem 67(2): 223–30. [DOI] [PubMed] [Google Scholar]
- 27. Gan DD, Reiss K, Carrill T, Del Valle L, Croul S, et al. (2001) Involvement of Wnt signaling pathway in murine medulloblastoma induced by human neurotropic JC virus. Oncogene 20(35): 4864–70. [DOI] [PubMed] [Google Scholar]
- 28. Lassak A, Del Valle L, Peruzzi F, Wang JY, Enam S, et al. (2002) Insulin receptor substrate 1 translocation to the nucleus by the human JC virus T-antigen. J Biol Chem 277(19): 17231–8. [DOI] [PubMed] [Google Scholar]
- 29. Trojanek J, Croul S, Ho T, Wang JY, Darbinyan A, et al. (2006) T-antigen of the human polyomavirus JC attenuates faithful DNA repair by forcing nuclear interaction between IRS-1 and Rad51. J Cell Physiol 206(1): 35–46. [DOI] [PubMed] [Google Scholar]
- 30. Seo GJ, Fink LH, O'Hara B, Atwood WJ, Sullivan CS (2008) Evolutionarily conserved function of a viral microRNA. J Virol 82(20): 9823–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Uleri E, Beltrami S, Gordon J, Dolei A, Sariyer IK (2011) Extinction of Tumor Antigen Expression by SF2/ASF in JCV-Transformed Cells. Genes Cancer 2(7): 728–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Shimazu T, Komatsu Y, Nakayama KI, Fukazawa H, Horinouchi S, et al. (2006) Regulation of SV40 large T-antigen stability by reversible acetylation. Oncogene 25(56): 7391–400. [DOI] [PubMed] [Google Scholar]
- 33. Poulin DL, Kung AL, DeCaprio JA (2004) p53 targets simian virus 40 large T antigen for acetylation by CBP. J Virol 78(15): 8245–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Staib C, Pesch J, Gerwig R, Gerber JK, Brehm U, et al. (1996) p53 inhibits JC virus DNA replication in vivo and interacts with JC virus large T-antigen. Virology 219(1): 237–46. [DOI] [PubMed] [Google Scholar]
- 35. Krynska B, Del Valle L, Gordon J, Otte J, Croul S, et al. (2000) Identification of a novel p53 mutation in JCV-induced mouse medulloblastoma. Virology 274(1): 65–74. [DOI] [PubMed] [Google Scholar]
- 36. Sariyer IK, Khalili K (2011) Regulation of human neurotropic JC virus replication by alternative splicing factor SF2/ASF in glial cells. PLoS One 6(1): e14630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Barret C, Roy C, Montcourrier P, Mangeat P, Niggli V (2000) Mutagenesis of the phosphatidylinositol 4,5-bisphosphate (PIP(2)) binding site in the NH(2)-terminal domain of ezrin correlates with its altered cellular distribution. J Cell Bio 151(5): 1067–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Cole BK, Curto M, Chan AW, McClatchey AI (2008) Localization to the cortical cytoskeleton is necessary for Nf2/merlin-dependent epidermal growth factor receptor silencing. Mol Cell Biol 28(4): 1274–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Mani T, Hennigan RF, Foster LA, Conrady DG, Herr AB, et al. (2011) FERM domain phosphoinositide binding targets merlin to the membrane and is essential for its growth suppressive function. Mol Cell Biol 31(10): 1983–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kissil JL, Wilker EW, Johnson KC, Eckman MS, Yaffe MB, et al. (2003) Merlin, the product of the Nf2 tumor suppressor gene, is an inhibitor of the p21-activated kinase, Pak1. Mol Cell. 12(4): 841–9. [DOI] [PubMed] [Google Scholar]
- 41. Scoles DR, Yong WH, Qin Y, Wawrowsky K, Pulst SM (2006) Schwannomin inhibits tumorigenesis through direct interaction with the eukaryotic initiation factor subunit c (eIF3c). Hum Mol Genet 15(7): 1059–70. [DOI] [PubMed] [Google Scholar]
- 42. Kim H, Kwak NJ, Lee JY, Choi BH, Lim Y, et al. (2004) Merlin neutralizes the inhibitory effect of Mdm2 on p53. J Biol Chem 279(9): 7812–8. [DOI] [PubMed] [Google Scholar]
- 43. Chang Z, Guo CL, Ahronowitz I, Stemmer-Rachamimov AO, MacCollin M, et al. (2009) A role for the p53 pathway in the pathology of meningiomas with NF2 loss. J Neurooncol 91(3): 265–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kalamarides M, Acosta MT, Babovic-Vuksanovic D, Carpen O, Cichowski K, et al. (2011) Neurofibromatosis 2011: a report of the Children's Tumor Foundation Annual Meeting. Acta Neuropathol (123(3)) 369–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Benkirane M, Neuveut C, Chun RF, Smith SM, Samuel CE, et al. (1997) Oncogenic potential of TAR RNA binding protein TRBP and its regulatory interaction with RNA-dependent protein kinase PKR. EMBO J 16(3): 611–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. López-Lago MA, Okada T, Murillo MM, Socci N, Giancotti FG (2009) Loss of the tumor suppressor gene NF2, encoding merlin, constitutively activates integrin-dependent mTORC1 signaling. Mol Cell Biol 29(15): 4235–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Yu Y, Kudchodkar SB, Alwine JC (2005) Effects of simian virus 40 large and small tumor antigens on mammalian target of rapamycin signaling: small tumor antigen mediates hypophosphorylation of eIF4E-binding protein 1 late in infection. J Virol 79(11): 6882–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Ikeda K, Saeki Y, Gonzalez-Agosti C, Ramesh V, Chiocca EA (1999) Inhibition of NF2- negative and NF2-positive primary human meningioma cell proliferation by overexpression of merlin due to vector-mediated gene transfer. J Neurosurg 91(1): 85–92. [DOI] [PubMed] [Google Scholar]
- 49. Okada T, Lopez-Lago M, Giancotti FG (2005) Merlin/NF-2 mediates contact inhibition of growth by suppressing recruitment of Rac to the plasma membrane. J Cell Biol 171(2): 361–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Lu Z, Hunter T (2010) Ubiquitylation and proteasomal degradation of the p21(Cip1), p27(Kip1) and p57(Kip2) CDK inhibitors. Cell Cycle 9(12): 2342–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Xiao GH, Gallagher R, Shetler J, Skele K, Altomare DA, et al. (2005) The NF2 tumor suppressor gene product, merlin, inhibits cell proliferation and cell cycle progression by repressing cyclin D1 expression. Mol Cell Biol 25(6): 2384–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Mamidipudi V, Zhang J, Lee KC, Cartwright CA (2004) RACK1 regulates G1/S progression by suppressing Src kinase activity. Mol Cell Biol 24(15): 6788–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Bhattacharyya R, Noch EK, Khalili K (2007) A novel role of Rac1 GTPase in JCV T-antigen mediated beta-catenin stabilization. Oncogene 26(55): 7628–36. [DOI] [PubMed] [Google Scholar]
- 54. Altomare DA, Vaslet CA, Skele KL, De Rienzo A, Devarajan K, et al. (2005) A mouse model recapitulating molecular features of human mesothelioma. Cancer Res 65(18): 8090–5. [DOI] [PubMed] [Google Scholar]
- 55. Gordon J, Del Valle L, Otte J, Khalili K (2000) Pituitary neoplasia induced by expression of human neurotropic polyomavirus, JCV, early genome in transgenic mice. Oncogene 19(42): 4840–6. [DOI] [PubMed] [Google Scholar]
- 56. Riddick G, Fine HA (2011) Integration and analysis of genome-scale data from gliomas. Nat. Rev. Neurol 7: 439–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Stettner MR, Nance JA, Wright CA, Kinoshita Y, Kim WK, et al. (2009) SMAD proteins of oligodendroglial cells regulate transcription of JC virus early and late genes coordinately with the Tat protein of human immunodeficiency virus type 1. J Gen Virol 90(8): 2005–14. [DOI] [PMC free article] [PubMed] [Google Scholar]