Abstract
Objective
This study tested a modified Cognitive Processing Therapy intervention (MCPT) designed as a more flexible administration of the protocol. Number of sessions was determined by client progress toward a priori defined end-state criteria, “stressor sessions” were inserted when necessary, and therapy was conducted by novice CPT clinicians.
Method
A randomized, controlled, repeated measures, semi-crossover design was utilized to 1) test the relative efficacy of the MCPT intervention compared to a Symptom-Monitoring Delayed Treatment (SMDT) condition and 2) to assess within-group variation in change with a sample of 100 male and female interpersonal trauma survivors with posttraumatic stress disorder (PTSD).
Results
Hierarchical linear modeling analyses revealed that MCPT evidenced greater improvement on all primary (PTSD and depression) and secondary (guilt, quality of life, general mental health, social functioning, and health perceptions) outcomes compared with SMDT. After the conclusion of SMDT, participants crossed over to MCPT, resulting in a Combined MCPT sample (n = 69). Of the 50 participants who completed MCPT, 58% reached end-state criteria prior to the 12th session, 8% at session 12, and 34% between sessions 12-18. Maintenance of treatment gains was found at the 3-month follow-up, with only two of the treated sample meeting criteria for PTSD. The use of stressor sessions did not result in poorer treatment outcomes.
Conclusions
Findings suggest that individuals respond at a variable rate to CPT, with significant benefit from additional therapy when indicated and excellent maintenance of gains. The insertion of stressor sessions did not alter the efficacy of the therapy.
Keywords: posttraumatic stress disorder, treatment outcome, cognitive processing therapy, effectiveness, interpersonal assault
A number of psychological interventions have demonstrated substantial empirical support in the remediation of posttraumatic stress disorder (PTSD) over the course of the last two decades, including prolonged exposure (PE), cognitive processing therapy (CPT), and eye movement desensitization reprocessing (EMDR; Institute of Medicine [IOM], 2008). As a result of this growing accumulation of evidence, the scientific community has endorsed specific therapies as “empirically supported” and numerous national organizations designated best practice guidelines (BPGs; e.g., IOM, 2008). Since the establishment of BPGs, efforts toward dissemination of these interventions to community care have significantly increased (Karlin et al., 2010). Despite these historically herculean efforts to disseminate the fruits of interventions developed in academic settings and tested in randomized controlled trials (RCTs), barriers to implementing evidence-based practice (EBP) into clinical care remain.
The extant literature is replete with numerous explanations for these historical difficulties in the successful dissemination and implementation of EBPs (Freiheit, Vye, Swan, & Cady, 2004; Kazdin, 2008). Objections to the integration of EBPs may stem from general dissonance around the application of the seemingly rigid “cookbook approach” of manualized therapies to the perceived complexity of distress observed in many clients seeking services in community care settings. The debate over EBP guidelines began almost immediately following the APA Task Force on Promotion and Dissemination of Psychological Procedures’ (1995) recommendations. A host of criticism for the implausibility of the APA’s recommended use of empirically supported treatments in clinical practice resounded through both clinical and academic circles resulting in a special issue of Journal of Consulting and Clinical Psychology (1998). Some of the strongest criticisms against the proclaimed empirical support of the cited interventions included the lack of flexibility of treatment manuals in RCTs (Beutler & Howard, 1998), the focus on outcome rather than processes of therapy (Barlow, 1996), the fixed number of sessions contained in protocols (Jacobsen & Christensen, 1996), the use of highly trained, expert clinicians to administer the intervention (Chambless & Hollon, 1998), the focus on diagnostic outcome rather than client level of functioning, and lack of overall ecological validity (Persons & Silberschatz, 1998). More recently, participant attrition and non-response rates reported in RCTs have also been cited as evidence that no given psychotherapy has generated sufficient empirical support to be labeled as an EBP for the treatment of PTSD (Schottenbauer, Glass, Arnkoff, Tendick, & Gray, 2008). RCTs for manualized PTSD treatments indicate that approximately one-third of the participants remain refractory to treatment and approximately one-quarter of the samples drop out prematurely (Bradley, Greene, Russ, Dultra, & Westen, 2005; Schottenbauer, Glass, Arnkoff, Tendick, & Gray, 2008). Although continued empirical support and significant advances have accumulated since the beginning of this debate in the 1990s, the integration of EBPs into community care remains challenging at best (Kazdin, 2008). Specifically, with respect to utilizing EBPs in the treatment of PTSD, Cook, Schnurr, and Foa (2004) suggest that researchers actively attend to clinicians’ concerns and challenges regarding the use of manual-based treatment. The current study sought to evaluate modifications to an existing evidence-based protocol (CPT) in an effort to more closely mimic practice by community clinicians and empirically address perceived barriers to implementation of evidence-based practice.
CPT has accumulated significant empirical support and has been identified as an EBP for the treatment of PTSD (IOM, 2008). To date, four RCTs have been published demonstrating the efficacy of the intervention across trauma samples, including female survivors of sexual and physical assault (Resick, Nishith, Weaver, Astin, & Feuer, 2002; Resick, Galovski, et al., 2008), survivors of childhood abuse (Chard, 2005), and veterans (Monson et al., 2006). Consistent with the larger PTSD outcome literature, in which approximately 20% to 50% of the sample remains PTSD-positive after a course of psychotherapy (Bradley et al., 2005; Schottenbauer et al., 2008), results from the CPT trials also leave room for improvement. In comparing the full, 12-session CPT protocol to PE, Resick et al. (2002) reported that 19.5% of the CPT group retained their PTSD diagnosis after completing the 12-session protocol. Similarly, in their dismantling study, Resick, Galovski, and colleagues (2008) reported that 29.6% of the CPT completer group was PTSD-positive at post-treatment. Further inspection of the outcome data in these two CPT trials (Resick et al., 2002; Resick et al., 2008) suggests that it may not be entirely accurate to conceptualize these PTSD positive treatment completers as “refractory” or “non-responders”, despite their PTSD positive status at the end of therapy. It may be more accurate to describe these individuals as “partial responders”, because PTSD and depressive severity scores decreased significantly on average from pre-treatment to post-treatment in this subset of completers (Galovski & Blain, 2008). The downward trends in symptomatology suggest that these individuals may be slower to respond and simply had not yet reached optimal levels of improvement by the conclusion of the 12-session protocol.
Chard (2005) uniformly lengthened the 12-session protocol to a 17-session protocol using a combined individual and group modality. Results from this trial indicate that only 7% of the CPT completers met PTSD criteria at post-treatment assessment. However, it is unknown whether these lower rates of PTSD caseness at treatment’s end can be attributed to the longer course of therapy (as PTSD status was not assessed at session 12), to the combination of group and individual care, or to other possible sources of variance. The question remains whether individuals who retain their PTSD diagnosis following a full course of CPT continue to improve or whether additional therapy will have diminished returns. The current study sought to empirically evaluate the benefit of continued therapy until a specific outcome criterion was met.
There is some evidence to suggest that a portion of CPT completers demonstrate a pattern of response that is consistent with the observed phenomenon of “sudden gains” or significant improvements within a full course of therapy. Kelly, Rizvi, Monson, and Resick (2009) investigated sudden gains (defined as rapid and stable improvement) in a course of CPT for survivors of interpersonal violence suffering from PTSD. Results indicated that sudden gains occurred in approximately 39% of participants. Sudden gains made during the course of therapy predicted greater overall symptom reductions at the conclusion of therapy, but were not related to the amount of symptom reduction at the 6-month follow-up assessment, suggesting that sudden gains can occur in CPT, but that those individuals who did not experience a sudden gain “caught up” over time. However, by definition, a sudden gain reflects significant change between two data points (in this case, treatment sessions). This within-protocol change was previously used to predict the overall degree of change after the participant received the full dose of the therapy. While these findings suggest that the phenomenon of rapid and efficient response to treatment within a standard course of CPT are associated with overall improvement at treatment termination, examination of a flexible termination point defined by pre-determined criterion of good end-state functioning has not been examined. There is little information regarding the maintenance of treatment gains in the long-term for those individuals who indicate a rapid and efficient response to treatment during the administration of the protocol. Finally, there is virtually no information on predictors of early and efficient treatment response versus a longer course of therapy. This study sought to assess whether a trauma survivor suffering from PTSD can achieve good end-state criteria prior to the full dose of therapy and continue to maintain these gains at the long-term follow-up. Possible predictors of efficiency of response were also explored.
Current Study and Aims
The current study examined the efficacy of modifications to an existing EBP, namely CPT. Specifically, the CPT protocol was administered more flexibly by basing therapy termination on specific client gains across a number of domains, instead of terminating therapy based on number of prescribed sessions completed, irrespective of client gains. Secondly, attention was paid to the process of therapy during the protocol by allowing therapists to insert up to two stressor sessions, if needed, during therapy. Third, in answer to the perception that highly trained clinicians administer these protocols in RCTs, Master’s-level clinicians (in psychology or social work) with no prior experience in delivering CPT administered all therapy. Consistent with previous RCTs involving CPT, the sample was recruited from the community, with very few exclusion criteria. Finally, we assessed a range of outcomes to evaluate the impact of treatment on client functioning and quality of life.
The primary aim of the current study was to assess the overall efficacy of varying lengths of CPT on PTSD and depression and to evaluate the maintenance of treatment benefits in the follow-up interval. We specifically hypothesized that Modified CPT (MCPT) participants would improve significantly more on primary outcomes, demonstrating large effects in comparison with their symptom monitoring, delayed treatment (SMDT) counterparts. Further, we predicted that the allowance of up to 50% more therapy (if necessary) would decrease the overall proportion of treatment non-responders as compared to previous CPT trials conducted at the same site, using the standardized, 12-session protocol. The effects of this trauma-focused intervention on secondary outcomes, including trauma-related guilt, quality of life, general mental health (psychological distress and emotional wellbeing), social functioning, and general health perceptions, were also assessed in an effort to evaluate the influence of length of treatment on these secondary outcomes. We again hypothesized that the MCPT participants would show significant improvements on secondary outcomes as compared to the SMDT group. It was additionally predicted that length of treatment (number of sessions administered) would not significantly influence outcome on secondary measures. It was also hypothesized that treatment gains would be maintained at the long-term follow-up assessment for all responders, irrespective of number of total treatment sessions. Based on previous literature indicating that older age (Rizvi et al., 2009), higher baseline severity and longer duration of PTSD symptoms (van Minnen et al., 2002), and higher depressive symptoms (Taylor et al., 2001) may predict poorer treatment response, we hypothesized that these variables would likewise predict a longer course of treatment necessary to achieve the study end-state criteria. Finally, the use of stressor sessions and their influence on treatment outcome were assessed. The effect of the interruption of the protocol in the event of client major psychosocial stressor or emergency was unknown, thus no specific predictions were made.
Method
Participants
Male and female participants were recruited from the greater St. Louis metropolitan area through a number of sources, including flyers, advertisements, referrals, and word-of-mouth. Participants had to be at least 18 years of age and meet full criteria for PTSD secondary to a sexual or physical assault in childhood or adulthood as assessed by the Clinician-Administered PTSD Scale (CAPS; Blake et al., 1990). At least 3 months needed to have transpired between the trauma and the initial assessment and individuals could not currently be in an abusive relationship or currently be the target of stalking. Participants could endorse lifetime drug and/or alcohol dependence, but needed to be in remission for at least 6 months. People meeting criteria for alcohol and drug abuse were not excluded from the study. Participants needed to be stable on psychiatric medications for 1-month prior to the initial assessment and needed to hold medication usage constant during treatment. Exclusion criteria included current mania, psychosis, or suicidal intent.
Procedure
Design
A randomized, controlled, repeated measures, semi-crossover design was utilized to test the relative efficacy of Modified Cognitive Processing Therapy (MCPT) compared to a Symptom-Monitoring Delayed Treatment (SMDT) condition. Using a semi-crossover design, the SMDT participants were crossed over to the MCPT condition following 10 weeks of symptom monitoring. The use of the SMDT condition allowed us to control for the passage of time, the therapeutic benefits of symptom monitoring, and minimal therapist contact. The semi-crossover design also ensured that all participants were offered the active treatment and provided increased statistical power to assess the efficiency of response to MCPT. Upon completion of a phone screen to determine eligibility, participants were invited for an initial assessment to read and sign the informed consent. There were no adverse events and the single-site study was conducted with University of Missouri - St. Louis Institutional Review Board approval.
If eligible, participants were randomly assigned in a 1:1 ratio using computer generated simple randomization to MCPT or to SMDT following the pre-treatment assessment. Within the MCPT condition, participant progress on PTSD and depressive symptomatology was evaluated through self-report measures at each treatment session [Posttraumatic Stress Distress Scale (PDS; Foa, Cashman, Jaycox, & Perry, 1997) and Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996)]. MCPT treatment termination occurred when all of the following criteria were met: achievement of specific end-state criterion (PDS ≤ 20 and BDI-II ≤ 18), agreement between the therapist and participant that treatment goals had been attained, and independent assessment and confirmation of participant’s negative PTSD status by a blind rater using the CAPS. These specific criteria for treatment termination were chosen following the precedence of van Minnen and Foa (2006) and Foa et al. (1999) in which a cutoff of 20 on the PTSD Symptom Scale was used to determine “good end-state functioning”. The BDI-II cutoff of 18 was based on the measurement manual outlining normative data and suggesting that a score of 18 equals the upper limit of “mild” depression. Because overall cutoff scores do not always portray significant elevations on individual symptoms (or items) that may certainly warrant additional clinical attention despite the low overall score, we included subjective agreement regarding symptom remediation between the therapist and the participant. Finally, because it is technically possible to remain PTSD positive with a score of 20 on the PDS and reporting bias can exist in the therapy situation (e.g., patient wants to please therapist), a blind rater conducted the CAPS to ensure that the participant no longer met criteria for PTSD.
Participants could complete treatment as early as session 4. Conversely, if a participant had not sufficiently improved on the outcome criterion by the end of the traditional 12-session CPT protocol, up to 6 additional sessions (50% more therapy) of MCPT could be provided. Additionally, in an effort to independently assess symptom severity and PTSD diagnostic status, an independent rater conducted a CAPS (following session 12) for those participants who required more therapy. Thus the primary modification of the CPT protocol consisted of varying the possible course of therapy, as dictated specifically by participant recovery, resulting in a range of 4-18 sessions of CPT.
SMDT participants completed a post-treatment assessment at the conclusion of the 10-week symptom monitoring condition. Data from this assessment constituted the pre-treatment (baseline) data for the MCPT arm of the crossover. Thus, utilizing the semi-crossover design, subjects in the SMDT condition were crossed over to the MCPT condition immediately following completion of the 10 weeks of symptom monitoring and minimal therapist contact. All MCPT participants (immediate and crossed-over) were assessed 2 weeks after completing treatment (irrespective of number of sessions necessary to achieve end-state criterion) and at the 3-month follow-up. Consistent with intention-to-treat principles, treatment drop-outs were invited back for post-treatment and subsequent 3-month follow-up assessments. Post-treatment and follow-up assessments were conducted by raters blind to both randomization and drop-out status. Participants were compensated for assessments ($50 for pre-treatment, $75 for post-treatment, and $100 for 3-month follow-up).
Instruments
Interviews
Clinician-Administered PTSD Scale
(CAPS; Blake et al., 1990) is a widely used clinician-administered diagnostic instrument designed to assess the frequency and intensity of the 17 PTSD symptoms, as well as clinician-rated validity of client report and symptom severity and improvement. Symptoms are rated on separate 5-point frequency and intensity scales ranging from 0 (never) to 4 (daily or almost daily) and from 0 (none) to 4 (extreme), respectively. Symptom items are summed to form a total score, such that higher scores indicate more severe PTSD symptoms (range 0 to 136). The CAPS has demonstrated excellent reliability and validity (Weathers, Keane, & Davidson, 2001). Internal consistency for the 17 PTSD symptoms in current study was high (α = .93).
Structured Clinical Interview for DSM–IV Axis I Disorders — Patient Edition
(SCID; First, Gibbon, Spitzer, & Williams, 1996) is a widely used semi-structured interview designed to assess DSM–IV Axis I diagnoses. The current study utilized the Mood, Anxiety, and Substance Use modules of the SCID. The SCID has well-established psychometrics (First et al., 1996).
Standardized Trauma Interview was adapted from Resick, Galovski, et al. (2008). It is an investigator-generated, clinician-administered interview designed to assess demographic characteristics, information about trauma, and treatment history.
Inter-rater reliability on diagnostic interviews
Inter-rater reliability was conducted for a random sample of interviews in the present study (29 CAPS and 25 SCID). Reliability among coders was high for the CAPS, [κ (current diagnosis) = 1.00; r (total score) = .91], as well as the SCID, [κ (all lifetime diagnoses) = 0.85; κ (all current diagnoses) = 0.74]. Correlations for CAPS clusters were also high (ICC’s = .94 for cluster B, .93 for cluster C, .93 for cluster D).
Self-report measures
Posttraumatic Stress Diagnostic Scale
(PDS; Foa et al., 1997) is a self-report screening and diagnostic instrument which assesses the severity of PTSD symptoms. Its 49 items assess trauma history and symptoms related to a Diagnostic and Statistical Manual 4th editon (DSM-IV; American Psychiatric Association, 2000) PTSD diagnosis. The 17 symptom items are rated on a 4-point scale from 0 (Not at all/ only one time) to 3 (5 or more times a week/ almost always), with higher scores representing more frequent symptoms (range 0 to 51). The PDS score can be evaluated according to the following clinical cutoffs: 0 = no rating, 1–10 = mild, 11–20 = moderate, 21–35 = moderate to severe, and >36 = severe. The PDS has demonstrated good sensitivity, specificity, and reliability (Foa et al., 1997). Internal consistency in the current study was high (α = .95).
Beck Depression Inventory-II
(BDI-II; Beck et al., 1996) is a widely used 21-item measure of depressive symptoms. Symptoms are rated on a 4-point severity scale. Total scores are obtained by summing the items, with higher scores indicating increased depressive symptom severity (range 0 to 63). Scores can be clinically evaluated using the following cutoff score guidelines: 0-13 = minimal; 14-19 = mild; 20-28 = moderate; 29-63 = severe. The scale has well-established reliability and validity (Beck et al., 1996). Internal consistency was high in the current study (α = .96).
Trauma Related Guilt Inventory
(TRGI; Kubany et al., 1996) is a 32-item inventory with a 5-point rating scale ranging from 4 (extremely true) to 0 (not at all true). The TRGI has three main scales: global guilt, distress, and guilt cognitions. Intercorrelations between TRGI scales and subscales range between r = .29 and .68, suggesting related but separate constructs are measured. In previous study, internal consistency (α’s ranged from .73 to .91) and test-re-test correlations (ranging from r = .74 to .86) were moderate to high in previous research (Kubany et al., 1996). Internal consistency for the subscales in the current study was moderate to high (α’s = .85 to .91).
Quality of Life Inventory
(QOLI; Frisch, 1994) is a self-report measure developed to assess quality of life across 16 domains (e.g., love, work, play, finances, relationships, etc.). Respondents rate importance of each domain to personal happiness and satisfaction on a 3-point scale from 0 (not important) to 2 (extremely important) and current satisfaction with the domain on a 7-point scale from -3 (very dissatisfied) to +3 (very satisfied). Items from each domain are multiplied to create a weighted score for each domain (range -6 to +6), and total QOLI scores represent the sum of all 16 domains (range -96 to +96). The QOLI has shown adequate convergent and discriminant validity (Frisch, 1994). In the current study, the QOLI demonstrated high internal consistency for weighted scores across time points (α’s = .90).
Medical Outcomes Study 36-Item Short Form Health Survey
(SF-36; McHorney, Ware, Lu, & Sherbourne, 1994) is a 36-item measure which assesses eight major areas of medical health (Ware, Gandek, & IQOLA Project Group, 1994). Scores for each domain range from 0 to 100, with higher scores indicating better functioning. Scale reliability coefficients for all subscales range from .78 to .93 in the original study (McHorney et al., 1994) and content and construct validity have been demonstrated as well (Ware et al., 1994). We specifically assessed change in functioning as measured by the general mental health (psychological distress and emotional wellbeing), social functioning, and general health perceptions scales. The internal consistency for the three scales was moderate to high (α’s = .79 to .87) for the current study.
Therapists and Training
Therapists included five Master-level clinicians (M.A. and L.C.S.W.) who had never treated a CPT case before this trial. Training began with a workshop conducted by the Principal Investigator. The CPT manual was provided in the training as well as relevant readings about the protocol. Clinicians were assigned study clients (primarily based on scheduling and availability) and 2-hour, weekly, supervision meetings commenced. Supervision provided an open forum for clinicians to discuss cases and clinical concerns and receive feedback from peers as well as the principal investigator of the study. This supervision continued through the course of the study. All sessions were video-recorded and portions of sessions were regularly included in supervision for review and feedback.
Adherence and competence
Expert CPT clinicians not otherwise affiliated with the present study conducted adherence and competence ratings for therapy sessions. Individual session elements were rated for presence or absence (adherence) and for quality of present elements (competence) ranging from 1 (not satisfactory) to 7 (excellent), with a 4 (satisfactory) midpoint. Raters coded a total of 103 sessions (17% of the total 609 sessions conducted, including removed participants). Additionally, a second independent rater coded 25 (or 24%) of these sessions to ensure reliability among independent raters. Reliability between coders was acceptable on both the presence of session elements (κ = .69) and the rating of session elements (ICC = .76). Regarding essential but not unique items (e.g., warmth, efficient structuring of session time, etc.), 93% of non-unique elements were judged to be present with 87% of present elements judged as satisfactory or higher, with an average rating of 4.50 (range across therapists = 3.98–5.28). The most frequently missed non-CPT specific items were “not problem solving about homework” (32% missing) and “homework review” (25%).
Of the 103 coded sessions, 92% of the session elements were judged to be present and 85% of present items were judged satisfactory or higher. The most common missing item was completion of the homework check-in log during session (35% of missing items). Significant differences were observed between therapists. Specifically, adherence rates ranged from 73–97% across therapists, χ2 (3, N = 451) = 51.90, p < .0001, with one therapist accounting for 64% of missed adherence items. Differences were also observed for competence, such that satisfactory ratings ranged from 74-97% across therapists, χ2 (3, N = 415) = 20.72, p < .0001. Although there were differences in overall adherence and competence amongst therapists, all means fell between “satisfactory” and “excellent”. There was no difference between therapists on dropout rate (range 17.6–35.7%), χ2 (3, N = 64) = 1.70, p = .636, and no significant difference on average number of sessions between therapists (M = 10.45–11.56; SD = 2.70–5.32), F (3, 45) = .11, p = .954.
Symptom Monitoring Delayed Treatment
Participation in SMDT consisted of daily symptom monitoring of PTSD and depressive symptoms, three phone interviews to conduct a PTSD symptom check with the CAPS, weekly completion of PDS and BDI-II, and access to their therapist through phone check-ins. Therapists inquired about progress with symptom monitoring, overall symptom severity, and general distress, but did not conduct any cognitive therapy or other trauma-focused intervention.
Original CPT
CPT is primarily a cognitive therapy, utilizing cognitive restructuring to accurately integrate assault-related information with previously existing belief systems. The protocol traditionally includes 12 sessions during which the therapist first provides psychoeducation and then uses Socratic dialogue to assist the survivor in resolving inaccurate thoughts or interpretations (i.e., stuck points) resulting from the trauma. The overarching goal is to assist the survivor in identifying and challenging stuck points and developing more accurate and helpful alternate thoughts (Resick, Monson, & Chard, 2008). CPT also includes a written trauma narrative. Clients are asked to write about their “index event” or most distressing trauma (in the event of multiple traumas) and read the account both at home and then to the therapist during sessions 4 and 5, giving survivors the opportunity to process natural emotions connected to the most significant traumatic memory and to identify misperceptions, inaccurate reporting of facts, and omission of important details. The rationale for choosing the “index event” as the initial focus of treatment is to help the client decrease avoidance by tackling the memory of the event that is most likely contributing to the current PTSD symptomatology. It is anticipated that the benefits of the intervention will generalize to additional traumas, but there is room in the protocol to address other events if necessary. Throughout the protocol, survivors learn specific cognitive skills necessary to recognize and challenge stuck points independently. Final sessions focus on specific beliefs commonly affected by traumatic events, including safety, trust, power/control, esteem, and intimacy.
CPT Modifications
The overarching goal of the modified application of the traditional CPT protocol was to more closely mimic actual clinical practice. The primary modifications included individually tailoring the length of the intervention (4-18 possible sessions) with the conclusion of treatment based entirely on the individual participant’s accomplishment of an a priori defined, specific end-state criterion (described above) rather than at the conclusion of the traditional 12-session protocol. Sessions 1 through 12 were identical to the original CPT protocol. Participants could complete treatment as early as session 4, affording the participant the benefit of at least minimal emotion processing and cognitive restructuring. The content of any additional sessions (13-18) was consistent with the original CPT protocol such that participants continued to identify stuck points preventing recovery from PTSD and used the cognitive skills to challenge them. A second protocol modification included the insertion of a “stressor session” within the trauma-focused protocol. This modification was made to address clinical concerns about breaking protocol and potentially diluting the overall efficacy of any given therapy as a result. Clinical trials typically have many safeguards and procedures in place for specific client emergencies such as increased suicidality, risk for harm, and homicidality. However, addressing major psychosocial stressors during the course of a therapy designed to focus primarily on trauma-related material can present a clinical dilemma. On one hand, the clinician does not wish to collude with avoidance (divergence from trauma-related topics may be considered avoidance). On the other hand, significant stressors may emerge during the course of therapy warranting, and perhaps requiring, a break from the topics contained in the protocol and attention to the non-trauma issue. These sessions were only offered when a participant experienced a significant psychosocial stressor or emergency (e.g., family death, diagnosis of life-threatening illness, notice of home foreclosure, sudden loss of job with family needs dependent on income) during the course of therapy. The stressor session then focused on providing support and applying current CPT skills to the issue at hand. Procedurally, if a therapist subjectively deemed that a stressor session was necessary, she would ask the participant if he or she would like to take one session to discuss and work on this stressor. It was the participant’s choice if he/she chose to stay “trauma-focused” (stay on protocol) or utilized a stressor session.
Statistical Methods
Hierarchical linear modeling (Raudenbush & Bryk, 2002) was used to examine the impact of MCPT on the repeated outcome measurements in three ways. First, MCPT was compared to SMDT in the intent-to-treat (ITT) randomization sample (n = 100) to examine pre-treatment to post-treatment change. Second, we replicated these analyses including only the participants who completed their initial study condition (n = 70) in order to assess the effects of treatment on those who completed the intervention. Third, hierarchical linear modeling was used to model change over the study period in the Combined MCPT treatment sample (i.e., those initially randomized to MCPT and those who crossed over to MCPT following SMDT; n = 69) on pre-treatment, post-treatment, and follow-up time points that were all considered to be class (categorical) time points in the models. Change trajectories were created for each participant by specifying individual-level random intercepts and slopes to model variability in the degree of symptom presentation at baseline, as well as variability in response to treatment.
Randomization was effective as no outcome variable had different baseline values by treatment group (p > .25). Because of the nature of the expected change, the trajectories were modeled using polynomial models consisting of an intercept, slope, and quadratic term (for Combined MCPT models). The intercept was coded to represent the baseline level of the outcome variable. The slope estimated the linear change over time and represented the increase or decrease in the variable. Finally, in the Combined MCPT analyses, the quadratic term estimated the acceleration or deceleration over time and reflected changes during the follow-up period (e.g., slowing of change during a maintenance of gains in the follow-up period).
The primary analyses were defined as group differences on the primary treatment targets (i.e., the slopes of the CAPS, PDS, and BDI-II) in the ITT and completer samples. Change over time on the CAPS, PDS and BDI-II was the primary analysis in the Combined MCPT sample. To hold the primary analyses to the nominal level of statistical significance, a Bonferroni correction was applied to the slope parameters of these three outcomes (i.e., α = 0.05/3 = 0.016). On completion of the primary analyses, secondary analyses were conducted to assess the influence of the intervention on additional domains of functioning. The secondary analyses were defined as group differences on secondary treatment targets (i.e., the slopes of TRGI, SF-36, and QOLI) in the ITT and completer samples. Change over time on the TRGI, SF-36, and QOLI was defined as the secondary analyses in the Combined MCPT sample. Multiple regression analysis was employed to test potential predictors of efficiency of response.
An ITT philosophy was used for creation of the primary outcome models. Although 100 participants were enrolled, 25 of these contributed only one score that could be used in the models. Sensitivity of the estimates to missing data was examined using a model that assumed the data were missing at random that used all available measurements (presented below). HLM analyses were conducted using SAS 9.2 (SAS, Inc., Cary, NC). All other analyses were conducted using SPSS 18.0 (SPSS, Inc. Chicago, IL).
Results
Study Sample
Initial randomization participants
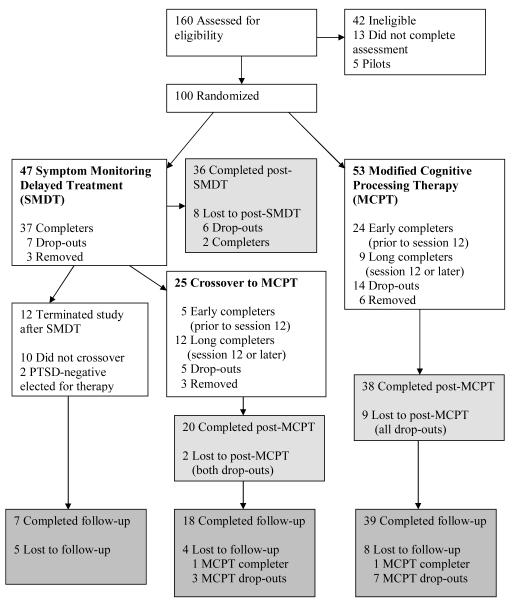
In all, 160 men and women were assessed for eligibility (see Figure 1). Of these, 42 did not meet study criteria, an additional 13 individuals did not complete the assessment, and 5 were included as non-randomized training cases. Of the 100 people randomized into the trial, 9 met initial study exclusion criteria subsequent to randomization [medication instability (n = 4), current substance dependence (n = 2), current abusive relationship (n = 2), current psychosis (n = 1)]. These 9 individuals were retained in the ITT sample. The ITT study sample thus consisted of 100 participants (69 women and 31 men). Observed sample sizes ranged across measures and treatment groups at pre-treatment (MCPT ns = 49-53; SMDT ns = 41-47) and post-treatment (MCPT ns = 34-48; SMDT ns = 32-37).
Figure 1.
Flow of participant progress through the study protocol.
Crossover participants
Following completion of the SMDT condition, SMDT participants were invited to cross over to the MCPT condition. Thirty-seven participants completed SMDT. Twelve of the 37 participants did not cross over to MCPT. Of these 12, 2 no longer met criteria for PTSD and did not wish to pursue treatment, 1 reported no longer being interested in the program, and the remaining 9 participants were either no longer able to participate due to relocation or changes in schedule (n = 2) or for unknown reasons (n = 7). Twenty-five total participants crossed over to MCPT from SMDT (3 were removed, including 2 participants who no longer met criteria for PTSD but wanted to participate in therapy and one participant who was exposed to a criterion A event between SMDT and commencement of MCPT and needed to be treated out of protocol, 5 dropped out of treatment, and 17 completed). Thus the Combined MCPT treatment sample consisted of 69 participants who we intended to treat with MCPT (22 crossovers and 47 original MCPT). A total of 50 individuals completed MCPT.
Demographics
Participant age ranged from 19 to 68 (M = 39.80, SD = 11.74). The group described themselves as predominantly Black (51%) or White (42%). A total of 7% described themselves as Hispanic. Most of the sample was single (58%), 21% were married or living with someone, and 21% were separated, divorced, or widowed. The majority reported at least some post-high school education (64%), with a mean of 13.10 years of education (SD = 2.78), and 67% reported an income of $20,000 or less.
Trauma history
There were no differences between treatment conditions in the ITT study sample on type of index event, time since trauma, or other aspects of lifetime trauma history. Participants reported a complex trauma history, with lifetime endorsements of child sexual abuse (68%), child physical abuse (59%), adult sexual assault (52%), adult physical assault (67%), and domestic violence (54%). Participants identified a worst event (or “index event”) for the assessment of PTSD and initial treatment focus. Index events in the ITT randomization sample were 44% child sexual abuse, 12% child physical abuse, 22% adult sexual assault, and 22% adult physical assault. Time since the index event ranged from 3 months to 52.7 years (M = 228.8 months, SD = 191.7).
Axis I comorbidity
The SCID was used to assess the presence of comorbid Axis I disorders. The vast majority (85%) of participants met criteria for at least one current comorbid Axis I disorder at pre-treatment, with major depressive disorder (48%) and panic disorder (25%) being the most common current comorbid psychopathology. Although current alcohol and substance dependence were exclusion criteria, approximately 36% of the sample met criteria for a lifetime history of alcohol dependence and 34% met criteria for lifetime substance dependence. Although participants reported current alcohol and substance use, no participants were diagnosed with substance abuse or alcohol abuse disorders. Fourteen percent of the participants would have met criteria for lifetime alcohol abuse and 13% would have met criteria for substance abuse at some point in their lifetime. There were no baseline differences in current or lifetime presence of comorbid Axis I disorders.
Study Retention
Of the 100 randomized participants, 21 dropped out of their initial treatment condition (14.9% SMDT, 26.4% MCPT; see Figure 1). Drop-out percentages were not significantly different across the initial randomization conditions (χ2 (1; N = 91) = 2.47, p = .116, Cramer’s V = .165). However, study drop-outs had significantly higher pre-treatment CAPS severity (p = 0.028). There were also trends for study drop-outs to be younger (p = 0.081) and to have lower household income (p = 0.074). No differences were found on depression severity or trauma variables. Fifty percent of the 14 participants who dropped out of active treatment stated major, ongoing psychosocial stressors as the reason for leaving therapy. These stressors included issues such as lack of transportation or childcare, home foreclosure, need to move out of state, and imprisonment. The other half of the drop-outs did not report a reason for terminating early.
Treatment Outcomes
Primary outcomes ITT randomization
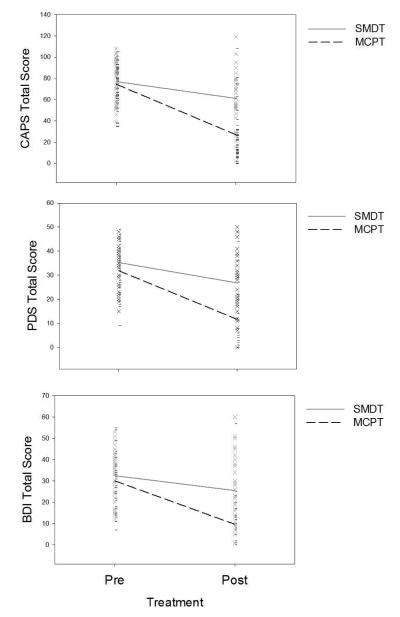
All three primary outcomes (CAPS, PDS, BDI-II) exhibited statistically significant individual variability in intercepts (i.e., baseline levels) as well as slopes (i.e., degree of change), ps < .001. This meaningful variance in the random effects indicates that participants exhibited a large degree of individual differences in how they presented to treatment and how they benefited from it. Figure 2 displays the variability in pre-treatment and post-treatment scores.
Figure 2.
Pre- to post-treatment change on the three primary outcome measures across initial randomization conditions.
Participants randomized to the MCPT group exhibited statistically greater reductions in the three primary outcome measures. Although SMDT participants had a decrease of 15.8 points on the CAPS, MCPT participants exhibited an additional 31.7-point reduction, p < .001. The SMDT group reported a decrease of 8.5 points on the PDS, but participants in the MCPT group exhibited an additional 11.8-point reduction, p < .001. Finally, participants in the SMDT reported a decrease of 7.0 points on the BDI-II, whereas participants in the MCPT group exhibited an additional 13.2-point reduction, p < .001. Table 1 displays fitted values (least square means and standard errors) for ITT randomization groups. In the completer analyses (all ps < .001), the SMDT group decreased 15.3 points on the CAPS while the MCPT group exhibited an additional 34.4-point decrease. The SMDT group reported a decrease of 8.9 points on the PDS, but participants in the MCPT group exhibited an additional 12.7-point reduction. Finally, participants in the SMDT reported a decrease of 8.2 points on the BDI-II, whereas participants in the MCPT group exhibited an additional 13.0-point reduction.
Table 1.
Pre and Post-treatment least square means, standard errors for ITT Randomization Groups across Measured Outcome Variables
| MCPTa |
SMDTb |
||||
|---|---|---|---|---|---|
| Pre-treatment LSM (SE) |
Post- treatment LSM (SE) |
Pre-treatment LSM (SE) |
Post-treatment LSM (SE) |
Hedge’s g* | |
| CAPS | 74.45 (2.42) | 26.96 (3.88) | 77.00 (2.57) | 61.18 (3.98) | 1.35 |
| PDS | 31.88 (1.25) | 11.63 (2.01) | 35.28 (1.34) | 26.81 (2.07) | .86 |
| BDI-II | 30.06 (1.53) | 9.67 (2.06) | 32.50 (1.65) | 25.51 (2.13) | .92 |
| TRGI global guilt |
2.24 (0.18) | 1.11 (0.18) | 2.38 (0.19) | 2.09 (0.18) | 0.72 |
| TRGI distress | 3.04 (0.10) | 1.98 (0.14) | 3.25 (0.11) | 2.97 (0.14) | .80 |
| TRGI guilt cognitions |
1.57 (0.11) | 0.88 (0.11) | 1.62 (0.12) | 1.43 (0.11) | 0.67 |
| QOLI | 1.18 (4.65) | 21.87 (5.69) | -0.17 (4.81) | 3.05 (5.89) | 0.47 |
| SF-36 social functioning |
42.87 (4.06) | 73.87 (4.56) | 37.45 (4.29) | 39.88 (4.69) | .95 |
| SF-36 emotional well being |
41.29 (2.77) | 66.51 (3.62) | 40.89 (2.91) | 42.93 (3.83) | 1.04 |
| SF-36 general health |
50.43 (3.38) | 64.63 (3.48) | 50.35 (3.56) | 50.53 (3.66) | 0.81 |
Note. CAPS = Clinician Administered PTSD Scale; MCPT = Modified Cognitive Processing Therapy; PDS = Posttraumatic Stress Diagnostic Scale; QOLI = Quality of Life Inventory; SF-36 = Short Form 36 Health Survey; SMDT = Symptom Monitoring Delayed Treatment; TRGI = Trauma-related Guilt Inventory.
Hedge’s g was calculated between the linear slopes of the two groups.
MCPT: pretreatment ns range from 49 to 53, posttreatment ns range from 34 to 48
SMDT: pretreatment ns range from 41 to 47, posttreatment ns range from 32 to 37
Secondary outcomes ITT randomization
Participants randomized to the MCPT group exhibited statistically greater reductions on all secondary outcomes (QOLI, SF-36, and TRGI). Table 1 depicts all fitted values on secondary outcomes for ITT randomization groups. MCPT participants evidenced an additional 17.4 -point improvement in overall quality of life on the QOLI as compared to the stable scores observed in the SMDT, p < .025. A similar pattern was observed across domains of social functioning, general health perceptions, and emotional wellbeing on the SF-36, with participants exhibiting significant improvements when compared to the SMDT (all ps < .001; range: 14.0 to 28.6 points). The MCPT group also demonstrated greater improvements (all ps < .002; range: -0.5 to -0.8 points) in the three primary guilt subscales of the TRGI guilt subscales (global guilt, distress, and guilt cognitions) compared to the SMDT group. All contrasts remained statistically significant after the Bonferroni correction. The completer analyses showed similar results with the MCPT participants exhibiting significant improvements compared to controls on the SF-36 subscales (all ps < .001; range: 14.5 to 31.2 points), and TRGI subscales (all ps < .001; range: 0.6 to 1.1).
Treatment retention - Combined MCPT
Of the 69 participants designated to receive MCPT (those initially randomized to MCPT and those who crossed over to MCPT following SMDT), 19 dropped out of treatment. Participants who dropped out were significantly different than those who completed treatment. Treatment drop-outs were younger (p < .038), had fewer years of education (p < .001), and had lower annual household income (p < .011). Treatment drop-outs also had significantly higher pre-treatment CAPS severity (p < .001). No differences in trauma variables were observed. Similar to previous studies (Resick et al., 2002; Resick et al., 2008), the vast majority of drop-outs occurred early in the therapy such that 74% of the drop-outs terminated prior to session 3.
MCPT efficiency of response to treatment
Of the 50 combined MCPT completers, only 4 participants met a priori end-state criterion (PDS ≤ 20 and BDI-II ≤ 18, agreement by therapist and participant, and independent evaluation with CAPS to ensure PTSD negative diagnostic status) exactly at session 12. The majority of the participants (58%) met end-state criteria prior to session 12 (M number of sessions = 7.5) and were thus considered “early completers”. Early completers’ (n = 29) mean post-treatment symptom scores surpassed the proposed end state criteria, PDS: M = 4.6, SD = 5.8; BDI-II: M = 4.0, SD = 5.2. Thirteen of the 50 Combined MCPT completers required additional therapy beyond session 12, reaching the end-state criteria in an average of 15.2 MCPT sessions. Of these 13 participants, 9 reached the a priori determined end-state criteria. Together, individuals who met end-state criteria at (n = 4) or beyond (n = 13) session 12 (n = 17; hereafter described as “long completers”) also reported post-treatment symptom scores that surpassed the study end-state criteria (PDS M = 14.25, SD = 12.15; BDI-II M = 13.00, SD = 8.67). The remaining 4 participants (designated as “non-responders” by study criteria) did not reach the study end-state criteria by session 18 (the maximum number of sessions allowed in the trial). These 4 participants’ CAPS scores revealed that one participant experienced 0% change across 18 sessions of therapy, while the remaining 3 participants reported 20%, 25%, and 48% symptom decreases at post-treatment, respectively. All 4 retained their PTSD diagnosis at post-treatment. At the 3-month follow-up assessment interval, all early and long completers maintained their PTSD negative status. Of the 4 non-responders, 2 individuals realized additional improvement and were PTSD-negative according to blind independent raters at the follow-up assessment. Thus, of the 50 participants who completed MCPT, only 2 remained PTSD-positive at the 3-month follow-up. Table 2 displays fitted values for each outcome measure at each assessment interval for the Combined MCPT treatment status groups: early completers (prior to session 12), long completers (session 12 or later; including the 4 non-responders), and drop-outs. Table 2 also displays effects sizes representing group differences in the rates of change between early versus long treatment completers.
Table 2.
Pre-treatment, Post-treatment, and Follow-up least square means, standard errors for Combined MCPT Groups across Measured Outcome Variables
| Early Completers (n = 29) |
Long Completers (n = 21) |
Drop-outs (n = 19) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre LSM (SE) |
Post LSM (SE) |
FU LSM (SE) |
Pre LSM (SE) |
Post LSM (SE) |
FU LSM (SE) |
Pre LSM (SE) |
Post LSM (SE) |
FU LSM (SE) |
Hedge’s g* |
|
| CAPS | 67.86 (3.54) |
12.48 (3.54) |
10.76 (3.54) |
69.81 (4.17) |
34.76 (4.17) |
29.62 (4.17) |
82.42 (4.38) |
70.37 (4.38) |
68.58 (4.38) |
0.57 |
| PDS | 28.62 (1.76) |
4.61 (1.79) |
4.72 (1.76) |
33.33 (2.23) |
17.89 (2.17) |
17.84 (2.17) |
33.16 (2.17) |
30.05 (2.17) |
30.17 (2.23) |
0.57 |
| BDI-II | 26.93 (2.00) |
4.04 (2.04) |
3.61 (2.04) |
31.90 (2.41) |
17.14 (2.36) |
18.05 (2.36) |
32.61 (2.54) |
28.22 (2.54) |
27.78 (2.54) |
0.59 |
| TRGI global guilt | 2.47 (0.22) |
1.01 (0.22) |
0.84 (0.22) |
2.18 (0.26) |
1.45 (0.26) |
1.02 (0.26) |
2.22 (0.27) |
1.92 (0.27) |
2.16 (0.28) |
0.28 |
| TRGI distress | 3.08 (0.15) |
1.66 (0.15) |
1.65 (0.15) |
3.24 (0.18) |
2.63 (0.17) |
2.51 (0.17) |
2.89 (0.18) |
2.78 (0.18) |
2.89 (0.18) |
0.60 |
| TRGI guilt cognitions |
1.56 (0.12) |
0.77 (0.13) |
0.69 (0.12) |
1.39 (0.16) |
1.05 (0.15) |
0.98 (0.15) |
1.48 (0.15) |
1.39 (0.15) |
1.36 (0.15) |
0.48 |
| QOLI | 8.70 (6.01) |
32.28 (5.76) |
41.41 (5.54) |
-13.00 (6.79) |
5.88 (6.99) |
6.17 (6.79) |
-2.93 (7.70) |
-4.17 (11.76) |
-2.67 (11.76) |
0.30 |
| SF-36 social functioning |
43.75 (5.07) |
84.26 (4.97) |
77.31 (4.97) |
35.00 (5.76) |
51.19 (5.64) |
51.25 (5.78) |
40.28 (6.09) |
42.19 (9.13) |
59.72 (8.61) |
0.43 |
| SF-36 emotional well being |
46.31 (3.92) |
77.86 (3.78) |
78.67 (3.85) |
33.60 (4.47) |
49.71 (4.36) |
52.20 (4.47) |
33.78 (4.71) |
36.57 (7.56) |
48.00 (6.66) |
0.45 |
| SF-36 general health |
51.92 (4.68) |
71.96 (4.51) |
75.74 (4.60) |
54.25 (5.34) |
56.90 (5.21) |
55.00 (5.34) |
35.83 (5.63) |
43.75 (8.44) |
51.11 (7.96) |
0.66 |
Note. FU=Follow-up; CAPS = Clinician Administered PTSD Scale; MCPT = Modified Cognitive Processing Therapy; PDS = Posttraumatic Stress Diagnostic Scale; QOLI = Quality of Life Inventory; SF-36 = Short Form 36 Health Survey; SMDT = Symptom Monitoring Delayed Treatment; TRGI = Trauma-related guilt Inventory.
Hedge’s g represents early and long completers’ linear slope comparison.
Primary outcomes Combined MCPT
Participants in the Combined MCPT treatment sample (n = 69) evidenced significant reductions on primary outcome measures (CAPS, PDS, and BDI-II; ps < .001). To assess the overall impact of number of sessions on linear change (pre to follow-up), we conducted a secondary analysis on treatment completers (including the 4 non-responders) examining the actual number of treatment sessions as a predictor. The impact of number of sessions on overall change on the CAPS was statistically significant indicating that each increase in session number was associated with a 1.63 points diminished response in change in CAPS score to follow-up, p < .03, such that those who took longer to complete treatment evidenced less overall change on the CAPS. This association must be interpreted with caution because the number of sessions administered was directly determined by symptom presentation. The BDI-II and PDS models were statistically non-significant, indicating that the number of sessions did not impact change on these indices.
Secondary outcomes Combined MCPT
Participants in the Combined MCPT treatment sample also evidenced statistically significant reductions on secondary outcome measures (QOLI, SF-36, and TRGI; ps < .003). Multilevel modeling was again used to assess change over time in the combined treatment sample. The Combined MCPT treatment sample demonstrated significant improvements in quality of life over time (p < .003). Regarding social functioning and emotional well being (SF-36), participants demonstrated significant change over time, with some slowing in change over time to maintained gains at follow-up (ps < .001). Physical health perceptions (SF-36) indicated that the overall Combined MCPT sample changed significantly over time (p < .001). Finally, the Combined MCPT sample also changed significantly on global guilt, guilt cognitions, and guilt distress (p’s < .001) with significant slowing in the rate of change over time (p’s < .001).
Predictors of treatment response
Preliminary analyses were conducted to identify predictors of treatment response. Participant age, time since index event, and pre-treatment CAPS and BDI-II scores were identified as potential predictors of length of therapy required to meet study end-state criteria (number of sessions) within the Combined MCPT completer sample (n = 50). Initial correlations revealed that only time since trauma (r = .33, p < .018) and initial depression severity (r = .34, p < .015) were associated with number of sessions. Age (r = .08, p < .585) and CAPS severity (r = .20, p < .160) were not significantly associated with response efficiency. Next, predictor variables were entered into a step-wise multiple regression. In the first step, time since trauma (β = .32, p < .017) and BDI-II scores (β = .33, p < .014) were statistically significant (F = 6.57, p < .003, R2 = .22). In the second step, age and CAPS severity were entered to account for covariance. The overall model remained significant (F = 3.38, p < .017, R2 = .23), and the individual predictors, time since trauma (β = .36, p < .014) and BDI-II (β = .32, p < .036), remained largely unaffected.
Stressor Sessions
A total of 13 stressor sessions were conducted with 13 clients. Reasons for the use of stressor sessions included death of family members, conviction and prison sentencing, job and housing losses, and other social and legal concerns. Participants who utilized stressor sessions were more depressed at pre-treatment than those who did not use stressor sessions (t = -2.29, p < .025); however, stressor session users did not differ from participants who did not use stressor sessions on number of trauma-focused sessions (t = -1.62, p < .110) or post-treatment PTSD or depressive symptoms (t = -1.15 and -1.91, respectively, p < .051). Thus, it appears that the insertion of a stressor session did not interrupt the administration of the protocol or the success of the trauma-focused intervention.
Discussion
This study represents the first effort to evaluate the efficiency of response to treatment for PTSD by flexibly administering a protocol-driven, EBP for PTSD in a multiply traumatized, community sample of male and female interpersonal assault survivors. The results from the initial randomization of the study provide support for the overall efficacy of the modifications of the original CPT protocol (MCPT) as compared to a minimal contact, symptom monitoring delayed treatment condition (SMDT). The large effect sizes observed in the current trial are similar to previous research (Resick et al., 2002; Monson et al., 2006) and suggest that the modifications to the CPT protocol did not diminish the efficacy of the intervention. Interestingly, although MCPT was clearly superior to SMDT, a palliative effect of minimal therapist contact and daily symptom monitoring was noted as the control condition significantly improved over time on PTSD and depressive symptoms. The observed improvements certainly fall short of the large effect sizes of established, evidence-based therapies, but the results suggest that discussing one’s trauma in the presence of a supportive individual (during the six hour pre-treatment assessment), tracking one’s symptoms on a daily basis, and establishing even minimal contact with a therapist over a period weeks (phone check-ins) may serve to decrease avoidance and help speed recovery. The improvements observed in the control condition of this trial are not entirely surprising as previous research (i.e., in alcohol abuse treatment; Clifford, Maisto, & Davis, 2007) has demonstrated that exposure to structured assessment may modify symptoms, providing a beneficial effect independent of the administered intervention. Likewise, daily symptom monitoring was another important component of the control condition and previous literature has demonstrated some therapeutic benefit associated with such monitoring (i.e., in anger-related interventions; Galovski & Blanchard, 2002). Finally, there is a wealth of literature demonstrating benefits associated with the therapeutic relationship, rapport and other nonspecific factors (Bjornsson, 2011). These outcomes in this study’s control condition suggest that a thorough, initial assessment conducted in a supportive environment, continued monitoring of trauma symptoms, and at least some minimal contact with a therapist in the interim before therapy commences may be helpful (and even therapeutic) in outpatient care or in situations involving a naturally occurring delay before treatment.
Following the conclusion of the SMDT condition, participants meeting criteria for PTSD were offered the MCPT, thereby increasing statistical power to assess the overall efficiency of response to treatment. In this study, response to MCPT treatment was dictated by specific end-state criteria, thus treatment’s end was not prescribed by the conclusion of the protocol irrespective of client progress. Results showed that MCPT completers met the study end-state criteria at a variable rate, ranging from 4 to 18 sessions of therapy. Outcome data from the Combined MCPT treatment completer sample were compelling. We were surprised to see that the majority (58%) of treated participants achieved the a priori end-state criteria prior to completion of the full standard 12-session treatment protocol, despite the chronic and severe nature of the sample. On average, our early treatment completers required 7.5 sessions of CPT (range 4-11) to achieve substantial treatment gains on both PTSD and depressive symptoms. Of the 50 completers, 46 were able to achieve the study end-state criteria. This resulted in only 4 participants (8%) remaining PTSD-positive by treatment’s end (session 18). Interestingly, had we concluded the treatment at session 12 (the endpoint of the original CPT protocol), 34% of our sample would have been considered “non-responders” as they were still PTSD-positive at session 12 (as diagnosed by blind raters using the CAPS). This percentage of non-responders maps onto previous CPT treatment trials conducted in the same location with a similar sample of interpersonal assault survivors. Resick et al. (2002) reported that 19.5% of the participants in the CPT condition retained their PTSD diagnosis at post-treatment while 29.6% of CPT completers were PTSD positive in the CPT dismantling trial (Resick et al., 2008). In recent reviews, the PTSD outcome literature reflects a range of 20-50% non-response to treatment across interventions, trials, and samples (Bradley et al., 2005; Schottenbauer et al., 2008). Our study indicates that PTSD and depressive symptoms can continue to improve with additional therapy, offering substantial benefit to those individuals who do not realize more efficient and rapid response in a standardized protocol.
Follow-up assessment results indicated excellent maintenance of treatment gains for the entire sample. One concern with terminating treatment prior to the administration of the full protocol was that the early treatment completers may not receive the full benefit of the intervention and their treatment gains may be rather spurious in nature. Results showed the opposite, such that early completers’ treatment gains were well maintained. Conversely, the longer treatment completers were not as efficient in their overall treatment response during the course of therapy, raising potential concern for relapse. However, this subset of the sample also demonstrated maintenance of treatment benefits. In fact, 2 of the 4 PTSD-positive participants continued to show improvement over the follow-up interval such that only 2 of the 50 individuals who completed a course of MCPT were PTSD-positive at the end of the study.
To date, CPT has accumulated substantial evidence demonstrating success in decreasing not only PTSD and depressive symptoms, but also across a wide range of secondary outcomes including guilt (Resick et al., 2002), health-related concerns (Galovski, Monson, Bruce & Resick, 2009), and psychosocial functioning (Galovski, Sobel, Phipps, & Resick, 2005). Results of the current study suggest that similar gains were made in these secondary outcomes irrespective of the number of sessions needed to complete therapy. It appears that early treatment responders’ gains in the PTSD and depression extend to secondary outcomes despite the abbreviated course of treatment. Thus, a participant who received less therapy (due to rapid response to PTSD and depression) did not lose any benefit with respect to trauma-related guilt, quality of life, general mental health, social functioning, or general health perceptions. At the other end of the treatment response spectrum, participants who required additional therapy to reach the end-state criteria (long completers) also indicated similar gains on most secondary outcomes (general health was an exception). These findings pose interesting questions for future research. Are the early treatment completers efficient in all areas of recovery because they are able to apply the intervention more easily to both primary and secondary symptomatology? Or do the reductions in the PTSD and depression then lead to the improvements in more general measures of well-being, life satisfaction, and psychosocial functioning?
Potential predictors of efficiency of response were tested in an effort to identify variables that may contribute to longer courses of treatment. Consistent with previous research in outpatient care (Chard, Schumm, Owens, & Cottingham, 2010), the amount of time since the index trauma was a significant predictor of number of sessions required to achieve study end-state criteria in our study. Age was not, however, a predictor of a longer course of therapy. Rizvi et al. (2009) found that younger age, but not time since index trauma, was associated with improved treatment outcomes in a standard 12-session protocol of CPT. However, it is unknown whether this effect would have been diminished with additional treatment. In other words, had those study participants received more CPT treatment specifically, would the older clients have eventually achieved the same outcomes? In our study, utilizing a variable course of therapy, age did not predict length of therapy, but chronicity of PTSD did. It is possible that living with PTSD for extended periods of time (irrespective of current age of the client) may result in more diffuse distress, overall role impairment, and subsequent deficits in functioning. A chronic PTSD clinical presentation may present additional challenges in therapy, requiring a longer course of treatment. Elevated depression prior to therapy also emerged as a significant predictor of length of treatment. This finding was also reported in outpatient VA treatment settings in which elevated pre-treatment depression were associated with longer courses of treatment (Chard et al., 2010). The presence of elevated depression prior to treatment may portend a longer road to recovery. Our study indicates that continuing the course of CPT is warranted if resolution of PTSD and depressive symptoms has not been fully achieved by the end of the standard 12-session protocol. Had we ended treatment at session 12, one-third of our sample would have been deemed refractory to treatment. Despite elevated depression, other Axis I and Axis II comorbidity, chronic PTSD, and complex trauma histories in this sample, we were able to effectively and significantly reduce symptomatology in all but four (8%) of our study participants. Two of those four participants continued to improve after the conclusion of therapy. The remaining two participants exhibited essentially no change (0% and 20% symptom decrease respectively) across therapy. These data highlight the importance of repeated assessment of client progress at each session and the incorporation of these data into treatment planning, particularly regarding extending the length of the treatment. In the event of downward progression of symptoms across sessions but less than optimal overall recovery by protocol’s end, our data provide evidence for continuing the protocol with an expectation of significant treatment gains.
This study is not without limitations. First and foremost, the attrition rate remains high and consistent with the larger literature (Bradley et al., 2005; Schottenbauer et al., 2008). The allowance of separate sessions to address client major life stressors and individually tailoring treatment length by participant did not substantially reduce our attrition rates. Future modifications may consider specifically targeting attrition so that more clients can realize the benefits of EBPs such as CPT. The role of practice work outside of the session warrants closer scrutiny in subsequent research beyond client-reported number of minutes of between-session practice. Our treatment outcomes are based on the number of actual sessions a participant attended, but the amount of practice work between sessions may have varied considerably between subjects and differentially contributed to the final symptom reductions. Finally, our study end state criteria bears scrutiny. Although both study criteria (PDS < 20 & BDI-II < 18) were established based on previous literature and established normative data, future study may reconsider these end state criteria in an effort to establish even more stringent outcomes. For instance, a score of 18 on the BDI-II is considered the high end of a “mild” level of depression. However, clinicians may hope for even more improvement before believing a client is “done” with therapy. Both our early responders and long responders exceeded this a priori criteria with means of 5 and 13 respectively on the BDI-II. However, it remains unknown if our longer completers may have benefited from striving for a more stringent end state goal.
The more flexible administration of an evidence-based protocol such as CPT is not without its potential hazards. Although community clinicians novice to CPT administered the protocol in this study, strict compliance with the protocol was maintained (and evaluated by expert CPT clinicians in the field for adherence and competence). Although the length of therapy was varied as dictated by participant progress, the content of the sessions was consistent with the original protocol. Additional sessions (13-18) consisted of specific CPT elements designed to target remaining client stuck points and continue to hone cognitive skills. No novel material was introduced in these sessions. The content of the optional stressor sessions was also consistent with cognitive strategies taught in the CPT protocol. In summary, these results suggest that a shorter and protocol-driven course of CPT may be a viable option for trauma survivors. Additionally, for those survivors who may not realize an early or efficient response, continuing the course of therapy may result in continued and substantial gains.
Acknowledgements
This work was supported by the National Institute of Mental Health (NIMH) 1R34MH074937 grant awarded to Tara E. Galovski at the University of Missouri- St. Louis. We thank the clinicians and research assistants affiliated with this project as well as the generous individuals who participated in this trial.
Contributor Information
Juliette M. Mott, Michael E. DeBakey Veterans Affairs Medical Center Veterans Affairs & South Central Mental Illness, Research, Education, and Clinical Center
Lisa Elwood, University of Indianapolis.
Timothy Houle, Wake Forest University.
References
- American Psychological Association . Diagnostic and statistical manual of mental disorders. 4th ed., text revision Author; Washington DC: 2000. [Google Scholar]
- Barlow DH. The effectiveness of psychotherapy: Science and policy. Clinical Psychology: Science and Practice. 1996;3:236–240. doi:10.1111/j.1468-2850.1996.tb00075.x. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory. 2nd ed The Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Beutler LE, Howard KI. Clinical utility research: An introduction. Journal of Clinical Psychology. 1998;54:297–301. doi: 10.1002/(sici)1097-4679(199804)54:3<297::aid-jclp1>3.0.co;2-n. doi:10.1002/(SICI)1097-4679(199804)54:3<297::AID-JCLP1>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- Bjornsson AJ. Beyond the “psychological placebo”: Specifying the nonspecific in psychotherapy. Clinical Psychology Science and Practice. 2011;18:113–118. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Klauminzer G, Charney DS, Keane TM. A clinician rating scale for assessing current and lifetime PTSD: The CAPS-1. Behavior Therapist. 1990;18:187–188. [Google Scholar]
- Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. American Journal of Psychiatry. 2005;16:214–227. doi: 10.1176/appi.ajp.162.2.214. doi:10.1176/appi.ajp.163.2.330. [DOI] [PubMed] [Google Scholar]
- Chambless DL, Hollon SD. Defining empirically supported therapies. Journal of Consulting and Clinical Psychology. 1998;66:7–18. doi: 10.1037//0022-006x.66.1.7. doi:10.1037/0022-006X.66.1.7. [DOI] [PubMed] [Google Scholar]
- Chard K. An evaluation of Cognitive Processing Therapy for the treatment of posttraumatic stress disorder related to childhood sexual abuse. Journal of Consulting and Clinical Psychology. 2005;73:965–971. doi: 10.1037/0022-006X.73.5.965. doi:10.1037/0022-006X.73.5.965. [DOI] [PubMed] [Google Scholar]
- Chard K, Schumm JA, Owens GP, Cottingham SM. A Comparison of OEF and OIF and Vietnam veterans receiving outpatient Cognitive Processing Therapy. Journal of Traumatic Stress. 2010;23(1):25–32. doi: 10.1002/jts.20500. DOI:10.1002/jts.20500. [DOI] [PubMed] [Google Scholar]
- Clifford PR, Maisto SA, David CM. Alcohol treatment research assessment exposure reactivity effects: Part I. Alcohol use and its related consequences. Journal of Studies on Alcohol and Drugs. 68(4):519–528. doi: 10.15288/jsad.2007.68.519. [DOI] [PubMed] [Google Scholar]
- Cook JM, Schnurr PP, Foa EB. Bridging the gap between posttraumatic stress disorder research and clinical practice: The example of exposure therapy. Psychology: Theory, Research, Practice, and Training. 2004;41(4):374–387. Doi:10.1037/0033-3204.41.4.374. [Google Scholar]
- First M, Gibbon M, Spitzer RL, Williams JBW. Structured clinical interview for DSM-IV Axis I disorders. SCID-I version 2.0 Biometrics Research Department; New York State Psychiatric Institute; New York: 1996. [Google Scholar]
- Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychological Assessment. 1997;9:445–451. doi:10.1037/1040-3590.9.4.445. [Google Scholar]
- Frieheit SR, Vye C, Swan R, Cady M. Cognitive-behavioral therapy for anxiety: Is dissemination working? The Behavior Therapist. 2004;27:25–32. [Google Scholar]
- Frisch MB. Manual and treatment guide for the Quality of Life Inventory (QOLI) Pearson Assessments and National Computer Systems; Minneapolis, MN: 1994. [Google Scholar]
- Galovski TE, Blain L, Kehle SM. Establishing the effectiveness of Cognitive Processing Therapy (CPT). The clinical effectiveness of empirically-supported treatments for PTSD; Symposium conducted at the annual convention of the International Society for Traumatic Stress Studies; Chicago, IL. Nov, 2008. [Google Scholar]
- Galovski TE, Blanchard EB. The effectiveness of a brief, psychological intervention on aggressive driving. Behaviour, Research and Therapy. 2002;40:1385–1402. doi: 10.1016/s0005-7967(01)00100-0. [DOI] [PubMed] [Google Scholar]
- Galovski TE, Monson CA, Bruce S, Resick PA. Does cognitive-behavioral therapy for PTSD improve perceived health? Journal of Traumatic Stress. 2009;22:197–204. doi: 10.1002/jts.20418. doi:10.1002/jts.20418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galovski TE, Sobel AA, Phipps KA, Resick PA. Trauma recovery: Beyond posttraumatic stress disorder and other Axis I symptom severity. In: Corales TA, editor. Trends in posttraumatic stress disorder research. Nova Science Publishers, Inc.; New York: 2005. pp. 207–227. [Google Scholar]
- Institute of Medicine . Treatment of posttraumatic stress disorder: An assessment of the evidence. National Academy Press; Washington, DC: 2008. [Google Scholar]
- Jacobsen NS, Christensen A. Studying the effectiveness of psychotherapy: How well can clinical trials do the job? American Psychologist. 1996;51:1030–1039. doi: 10.1037//0003-066x.51.10.1031. doi:10.1037/0003-066X.51.10.1031. [DOI] [PubMed] [Google Scholar]
- Karlin BE, Ruzek JI, Chard KM, Eftekhari A, Monson CM, Hembree EA, Foa EB. Dissemination of evidence-based psychological treatments for posttraumatic stress disorder in the Veterans Health Administration. Journal of Traumatic Stress. 2010;23:663–673. doi: 10.1002/jts.20588. doi:10.1002/jts.20588. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Evidence-based treatment and practice: New opportunities to bridge clinical research and practice, enhance the knowledge base, and improve patient care. American Psychologist. 2008;63:146–159. doi: 10.1037/0003-066X.63.3.146. doi:10.1037/0003-066X.63.3.146. [DOI] [PubMed] [Google Scholar]
- Kelly KA, Rizvi SL, Monson CM, Resick PA. The impact of sudden gains in cognitive behavioral therapy for posttraumatic stress disorder. Journal of Traumatic Stress. 2009;22:287–293. doi: 10.1002/jts.20427. doi:10.1002/jts.20427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubany ES, Haynes SN, Abueg FR, Manke FP, Brennan JM, Stahura C. Development and validation of the Trauma-Related Guilt Inventory. Psychological Assessment. 1996;8:428–444. doi:10.1037/1040-3590.8.4.428. [Google Scholar]
- McHorney CA, Ware JE, Jr., Lu JF, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): III. Medical Care. 32:40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- Monson CM, Schnurr PP, Resick PA, Friedman MJ, Xoung-Xu Y, Stevens SP. Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2005;74:898–907. doi: 10.1037/0022-006X.74.5.898. doi:10.1037/0022-006X.74.5.898. [DOI] [PubMed] [Google Scholar]
- Persons JB, Silberschatz G. Are results of randomized controlled trials useful to psychotherapists? Journal of Consulting and Clinical Psychology. 1998;66:126–135. doi: 10.1037//0022-006x.66.1.126. doi:10.1037/0022-006X.66.1.126. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2nd ed Sage; Newbury Park, CA: 2002. [Google Scholar]
- Resick PA, Galovski TE, Uhlmansiek M, Scher CD, Clum G, Young-Xu Y. A randomized clinical trial to dismantle components of cognitive processing therapy for posttraumatic stress disorder in female victims of interpersonal violence. Journal of Consulting and Clinical Psychology. 2008;76:243–258. doi: 10.1037/0022-006X.76.2.243. doi:10.1037/0022-006X.76.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Monson CM, Chard KM. Cognitive processing therapy: Veteran/military version. Department of Veterans’ Affairs; Washington, DC: 2008. [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology. 2002;70:867–879. doi: 10.1037//0022-006x.70.4.867. doi:10.1037/0022-006X.70.4.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizvi SL, Vogt DS, Resick PA. Cognitive and affective predictors of treatment outcome in cognitive processing therapy and prolonged exposure for posttraumatic stress disorder. Behaviour Research and Therapy. 2009;47(9):737–743. doi: 10.1016/j.brat.2009.06.003. doi: 10.1016/j.brat.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schottenbauer MA, Glass CR, Arnkoff DB, Tendick V, Gray SH. Nonresponse and dropout rates in outcome studies on PTSD: Review and methodological considerations. Psychiatry. 2008;71:134–68. doi: 10.1521/psyc.2008.71.2.134. doi:10.1521/psyc.2008.71.2.134. [DOI] [PubMed] [Google Scholar]
- Task Force on Promotion and Dissemination of Psychological Procedures Training in and dissemination of empirically-validated psychological procedures: Report and Recommendations. The Clinical Psychologist. 1995;48:3–23. [Google Scholar]
- Taylor S, Fedoroff IC, Koch WJ, Thordarson DS, Fecteau G, Nicki RM. Posttraumatic stress disorder arising after road traffic collisions: Patterns of response to cognitive-behavior therapy. Journal of Consulting and Clinical Psychology. 2001;69(3):541–551. doi: 10.1037/0022-006X.69.3.541. [PubMed] [Google Scholar]
- van Minnen A, Arntz A, Keijsers GPJ. Prolonged exposure in patients with chronic PTSD: Predictors of treatment outcome and dropout. Behaviour Research and Therapy. 2002;40(4):439–457. doi: 10.1016/s0005-7967(01)00024-9. doi:10.1016/S0005-7967(01)00024-9. [DOI] [PubMed] [Google Scholar]
- Ware JE, Gandek B, IQOLA Project Group The SF-36 Health Survey: Development and use in mental health research and the IQOLA project. International Journal of Mental Health. 1994;23:49–73. [Google Scholar]
- Weathers FW, Keane TM, Davidson JR. Clinician-Administered PTSD Scale: A review of the first ten years of research. Depression and Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. doi:10.1002/da.1029. [DOI] [PubMed] [Google Scholar]