Abstract
OBJECTIVES
To examine differences in functional status among two successive cohorts.
METHODS
The study was a comparative analysis of Jewish respondents aged 75–94 from two nationwide random samples: the Cross-Sectional and Longitudinal Aging Study (1989–1992; N =1200) and the Survey of Health, Ageing, and Retirement in Europe (2005–2006; N =379). Self-reported functional limitation and disability were compared by means of logistic regressions and MANCOVA, controlling for age, gender, origin, education, marital status, income, self-rated health, and home care receipt.
RESULTS
Reported functional limitation decreased in the later cohort (SHARE-Israel), but ADL- and IADL-disability increased. Receipt of home care moderated these effects. ADL- and IADL-disability increased among home-care-receiving respondents in the later cohort whereas functional limitation decreased among respondents not in receipt of home care.
DISCUSSION
The findings suggest that different measures used to assess the disablement process capture different aspects, and that contextual factors influence how older people rate their own functional capacity.
Keywords: functional status, disability, old-old, Israel, CALAS, SHARE, home care
Introduction
Tracing the trends in functional status in an era of population aging is of importance for several reasons. First, the length and the extent of functional decline in late life has direct implications for the quality of longer life among older people (Crimmins, Saito, & Ingegneri, 1997). Second, the ability of societies to continue to meet the needs of their oldest members may be increasingly challenged by an increase in the rates of late life impairment (Chernew, Goldman, Pan, & Shang, 2005; Knickman & Snell, 2002; Manton, Lamb, & Gu, 2007). Third, relatively high rates of functional decline may negatively affect public perceptions as to what it means to grow old (Berkman & Glymour, 2006; Stone, 2003). Given these varied implications of functional status and its concomitants, an accurate assessment of trends in the disablement process is a desirable goal.
Several reports indicate that, of late, functional status is declining more slowly and recent cohorts of older people may be healthier than their predecessors (Freedman, Martin, & Schoeni, 2002; Manton, Corder, & Stallard, 1997; Schoeni, Freedman, & L.G., 2008; Wolf, de Leon, & Glass, 2007). Other studies suggest, however, that these trends may differ among different age groups. Specifically, while the old-old are demonstrating less decline over time, the young-old within the elderly segment of the population seem to be demonstrating more (Chou & Leung, 2008; Seeman, Merkin, Crimmins, & Karlamangla, 2010).
Yet other research suggests that the perceived current decrease in the extent of functional decline might be ending. One study reports an increase of nine percent, between 2000 and 2005, in functional decline among community dwelling older Americans (Fuller-Thomson, Yu, Nuru-Jeter, Guralnik, & Minkler, 2009). Another inquiry notes an increase among older women in Barcelona, but not among the men (Espelt, et al., 2010). Other investigators point out that there is no guarantee that the decline in late-life disability prevalence in the United States will continue into the future (Martin, Schoeni, & Andreski, 2010). Nevertheless, a 3-year longitudinal study in Montreal found that older adults’ functional status may improve even if the participants are disabled (Nikolova, Demers, Beland, & Giroux, 2011).
Making sense of disability trends is further complicated by the context in which the phenomenon is examined. Some studies show that rates of functional decline may differ by country and that different trends may be discerned in different settings (Chou & Leung, 2008; Donald, Foy, & Jagger, 2010; Liu, Chen, Song, Chi, & Zheng, 2009; Sagardui-Villamor, Guallar-Castillon, Garcia-Ferruelo, Banegas, & Rodriguez-Artalejo, 2005; Seeman, et al., 2010). Part of the reasons for these discrepancies is the variation in the measures that are employed to trace the phenomenon in different studies. As a result, aspects of functional decline have been observed to vary even within the same setting (Parker & Thorslund, 2007).
Yet another factor which might affect the reporting of functional status in different settings stems from the relative availability of support services and the administrative and/or clinical criteria which determine eligibility for receipt of these services. As a case in point, the Israeli government began the implementation of community long-term care insurance in 1988 (Schmid, 2005), offering selected home care services to persons with an assessed level of functional disability, for example, personal care and homemaking, transportation to and care in adult day centers, and meal preparation services (Morginstin, Baich-Moray, & Zipkin, 2003). Eligibility for the receipt of these services was based on evaluation of Activities of Daily Living (ADL) and a means test. In 2006 (the year in which our second cohort was interviewed), the officially reported prevalence of those who received home care in Israel was 30.1% of those aged 65 and above (Brodsky, Shnoor, & Be’er, 2011).
The present study had two main objectives: (1) to examine cohort differences in functional status, and (2) to examine whether contextual factors interact with cohort in determining rates of functional decline. Therefore, the current study compared measures of functional limitation and disability in two cohorts of self-responding, community-dwelling persons aged 75–94 in Israel, taking into account the receipt of home care services as well. Functional limitation refers mainly to difficulties in the adaptive use of physical capabilities such as movement and vigor. Disability refers mainly to difficulties in vital self-maintenance capabilities. The current analysis considered both functional limitation and disability indicators because the two are related components in the disablement process. It is important to consider both kinds of indicators for several reasons: 1) measures of functional limitation may identify functional decrements that are not observable from the reporting of more severe outcomes, such as ADL disability, 2) functional limitation has been shown to predict disability in longitudinal epidemiologic studies, and 3) the distinctions between a functional limitation and a disability may not always be obvious (Guralnik and Ferrucci, 2003).
In light of the preceding review of the literature, the current inquiry considers three hypotheses. First, we hypothesize that the extent of functional decline is lower in a later, more recent cohort of older Jewish Israelis than in a previous cohort. Second, we hypothesize that functional status varies in relation to different measures, specifically—functional limitation and disability. Third, we hypothesize that the expected lower functional decline in the later cohort is more evident in measures that are less related to home care eligibility. In this context, we are interested whether changing social contexts influence how older people rate their own functional status. More specifically, the community long-term care insurance law was enacted near the time when the earlier cohort in this study was interviewed whereas the later cohort was interviewed 16 years later. Therefore, the interaction effect of cohort and receiving home care on disability is also examined.
Method
Participants and Procedure
The first sample was part of the Cross-Sectional and Longitudinal Aging Study (CALAS), a multidimensional assessment of the older Jewish population stratified by age group (75–79, 80–84, 85–89, 90–94), gender, and place of birth (Israel, Europe/America, Mideast/North-Africa) (Ben-Ezra & Shmotkin, 2006). The initial random sample was drawn on January, 1989, from the Israel National Population Registry. Wave 1 interviews (of three) were conducted during 1989–1992. A total of 2400 people were sampled for the CALAS study. Of these, 15.7% had died or were not located, and 8.5% had refused to participate, leaving 1820 individuals who were interviewed. Of these, 1,369 were self-respondents and 451 were by proxy (due to incapacity or death after sampling). CALAS participants were interviewed in their residence (home or institution). The two-hour interview was conducted in Hebrew, or in other languages when necessary. The procedure was approved in accordance with Helsinki ethical requirements. Participants signed informed consent. For the purpose of the current study, we excluded participants living in residential facilities, who were included in CALAS (12.3% of self-respondents aged 75–94), but were not included in the SHARE-Israel sample. This restriction resulted in a sample of 1,200 participants from the CALAS for the current analysis.
The second sample was the Israeli component of the Survey of Health, Ageing, and Retirement in Europe (SHARE-Israel) (Litwin, 2009). SHARE-Israel queried Israelis aged 50 or older and their spouses regardless of age using a probability sample of households within 150 representative statistical areas delineated by geographical and sociodemographic criteria. The maximum age in the first wave of the survey was 94 years old. The Wave 1 interviews were conducted from August, 2005, through July, 2006. The sample included 2,598 community (i.e., noninstitutionalized) dwellers in 1,771 households. SHARE-Israel participants were interviewed at home by means of a 90 minute computer-assisted personal interview, and a supplementary drop-off questionnaire. Interviews were conducted in Hebrew, Russian or Arabic. SHARE-Israel received ethical approval by the host University Institutional Review Board. Informed consent was obtained from participants prior to interview. The present analysis excluded participants younger than age 75, who were sampled by SHARE-Israel but not by CALAS. Moreover, the analysis excluded two population groups sampled by SHARE-Israel but not by the CALAS: Arab participants and immigrants from the Former Soviet Union who arrived during the 1990s. These restrictions resulted in a study sample of 379 participants from SHARE-Israel.
Measures
Standard background characteristics (covariates) that were addressed in this analysis and which were available in both surveys included: age, gender, origin (Asian-African origin Jews, European-American origin Jews, and Israeli-born Jews), and marital status (single, married, divorced, and widowed). Level of education was recorded in the CALAS by the number of years of schooling. Income was reported by means of a dichotomized item that asked whether the respondent had only a national insurance allowance or other income sources as well. Those with only a national insurance allowance are considered to have low incomes, insofar as the allotment reflects less than 20% of the average national wage.
In SHARE-Israel, in comparison, education was indicated by seven levels, according to the International Standard Classification of Educational Degrees (ISCED-97; United Nations Educational, Scientific and Cultural Organisation, 1997). These ranged from “pre-primary” (0) to “second stage tertiary education” (6). The income measure was obtained in SHARE-Israel by asking respondents about their income from a range of possible sources (e.g., the national insurance allowance, occupational retirement pension, and disability pension benefit).
In order to conduct cohort comparisons, the education and income measures from the two surveys were harmonized as follows. For education, the years of schooling in the CALAS were transformed into the ISCED categories utilized in SHARE-Israel. For income, the income sources recorded in SHARE-Israel were reduced into a dichotomized measure parallel to the one employed in the CALAS.
Self-rated health status was considered as a control variable, in order to limit the possible effect of subjective health perspectives on the self-reported disability outcomes. However, it was measured on slightly different scales in the respective surveys. In the CALAS, self-rated health status was measured by a single item that ranked one’s current health as 1 (bad), 2 (all right), 3 (good), and 4 (excellent). In SHARE-Israel, this same variable was measured by a single item that ranked current health state as 1 (very bad), 2 (bad), 3 (fair), 4 (good), and 5 (very good). In order to harmonize these items, categories 1 and 2 in the SHARE-Israel measure were combined.
The receipt of home care was measured in the CALAS questionnaire by means of two items: whether or not the respondent received paid personal care (yes/no), and whether or not the respondent received any other paid home assistance (yes/no/don’t know). These items were dichotomized into getting none or getting at least one sort of care. The same area of interest was measured in SHARE-Israel by three items: 1) paid or in-kind personal care, 2) help (paid or in-kind) for housework, and 3) meals-on-wheels. All three of these indicators were coded as yes/no. For the purpose of cohort comparison, the SHARE-Israel probes were dichotomized into getting none or getting at least one sort of care, as was done for the CALAS cohort. As noted earlier, changes in the eligibility criteria for receipt of publicly-funded home care occurred in the years following the CALAS survey, due to the establishment of Long-Term Care Insurance in Israel. In order to take this development into account in the current analysis, we included the receipt of home care as a control variable and also examined its interaction with cohort.
The outcome variable—functional status—was assessed by self-reported functional limitation and by two self-reported disability measures. In these measures higher scores represented more difficulties. The functional limitation measure included three physical activities assessed in both samples, specifically pulling or pushing heavy objects, bending or kneeling, and climbing 10 stairs without resting. The limitations were rated in terms of degree of difficulty on a scale of 0 (no difficulty), 1 (some difficulty), 2 (severe difficulty), and 3 (complete disability) in the CALAS instrument, but with a dichotomized answer (not having difficulties/having difficulties) in the SHARE-Israel survey. Therefore, the CALAS ratings were subsequently dichotomized into having no difficulty or having difficulties (from some difficulty to complete disability).
The two disability measures employed in the analysis were: 1) difficulties in basic activities of daily living (ADL) and 2) difficulties in instrumental activities of daily living (IADL). As the ADL measure differed slightly across the two samples we employed only those activities that were assessed in both samples. These included difficulties in the following functions: crossing a small room, washing, eating, transferring, and toileting. The IADL measure included five activities that were assessed in both samples. These included preparing meals, daily shopping, using the telephone, doing housekeeping and/or heavy housework and handling personal finances. Difficulties in both of these disability measures were rated in the CALAS instrument on a scale of 0 (no difficulty), 1 (some difficulty), 2 (severe difficulty), and 3 (complete disability), but with a dichotomized answer (not having difficulties/having difficulties) in the SHARE-Israel survey. Therefore, here too, the CALAS ratings were dichotomized into having no difficulty or having difficulties (from some difficulty to complete disability).
Analysis
In order to compare functional status in the two cohorts, we performed logistic regression analyses. Background characteristics (age, gender, origin [divided into two dummy-coded variables that controlled for Israeli born], education, marital status [dichotomized into “currently unmarried” and “married”], income, self-rated health, and home care) were entered in Step 1. Cohort was added in Step 2 and its interaction with home care was added in Step 3. The interaction product was computed by multiplying cohort by home care. We used commonly accepted recommendations for the exploration of interactions in logistic regressions (Aiken & West, 1991). ADL-disability, IADL-disability and functional limitation (divided into “no difficulty” and “reporting at least one difficulty”) served consecutively as the dependents. We further performed a multivariate analysis of covariance (MANCOVA) including background characteristics as covariates, cohort and home care as independents, and ADL-disability, IADL-disability, and functional limitations as dependents. Whereas the logistic regression separately examined the likelihood of having at least one difficulty in each functional status measure, the MANCOVA examined the functional status measures, both jointly and separately, in terms of the actual number of difficulties.
Results
Table 1 presents the background characteristics of the two samples. The CALAS sample was somewhat older than the corresponding SHARE-Israel sample. It also included more men, had a greater proportion of Israeli born respondents (but a smaller proportion of persons of European-American origin), and included more married respondents. The SHARE-Israel sample was more highly educated, on average. The two samples did not differ on income and self-rated health, but the CALAS sample was in receipt of more home care. However, after controlling for age, the samples did not differ in the percentage of home care receivers (B=−0.04, OR=0.95, 95% CI=0.72–1.25, p=0.73). Table 2 shows proportions and means indicating functional decline for both cohorts.
Table 1.
Distribution of Background Characteristics in Two Cohort Samples
| CALAS: 1989 cohort (N = 1200) | SHARE-Israel: 2005 cohort (N = 379) | Difference test | |
|---|---|---|---|
| Age | t(1577) = 10.04*** | ||
| M | 83.10 | 80.06 | |
| SD | 5.32 | 4.44 | |
| Gender (%) | χ2(1, N=1579) = 4.17* | ||
| Women | 44.9 | 50.9 | |
| Men | 55.1 | 49.1 | |
| Origin (%) | χ2(2, N=1579) = 58.17*** | ||
| Asia-Africa | 32.7 | 30.6 | |
| Europe-America | 37.0 | 56.2 | |
| Israel | 30.3 | 13.2 | |
| Educationa | t(1525) = −6.06*** | ||
| M | 1.96 | 2.54 | |
| SD | 1.58 | 1.66 | |
| Marital status (%) | χ2(1, N=1573) = 9.54** | ||
| Currently unmarriedb | 53.4 | 55.7 | |
| Married | 46.6 | 44.3 | |
| Income (%) | χ2(1, N=1529) = 1.50 | ||
| Only national insurance | 41.8 | 38.2 | |
| Other sources | 58.2 | 61.8 | |
| Self-rated healthc | t(1560) = −1.80 | ||
| M | 1.98 | 2.07 | |
| SD | 0.84 | 0.93 | |
| Home care (%) | χ2(1, N=1460) = 4.81* | ||
| Not receiving | 65.6 | 71.8 | |
| Receiving | 34.4 | 28.2 |
Note. Data of individual variables were occasionally missing for 0–102 and 0–17 participants in the CALAS and SHARE-Israel, respectively.
Rated on a scale from 0 (pre-primary education) to 6 (second stage tertiary education).
Includes the categories “single,” “divorced,” and “widower.”
Rated on a scale from 1 (bad) to 4 (excellent).
p < .05,
p < .01,
p < .0001.
Table 2.
Functional Decline in the Two Cohorts
| ADL-disability | IADL-disability | Functional limitation | |
|---|---|---|---|
| CALAS: 1989 cohort (N = 1200) | 26.7% 0.62 (1.44)a | 44.0% 1.03 (1.43) | 74.2% 1.76 (1.23) |
| SHARE-Israel: 2005 cohort (N = 379) | 36.9% 1.07 (1.66) | 50.5% 1.35 (1.53) | 66.5% 1.37 (1.16) |
In each cell percentages refer to participants reporting at least one difficulty, means refer to number of reported difficulties, and standard deviations are in parentheses. Percentages and means are adjusted for covariates (age, gender, origin, education, marital status, income, self-rated health, and home care).
ADL=Activities of daily living; IADL=Instrumental activities of daily living.
Table 3 shows the results of the logistic regressions. As can be seen, being older, with lower education, and receiving home care were related to poorer functional status across all three measures. The coefficients for cohort show that ADL- and IADL- disability were higher in the SHARE-Israel cohort while functional limitation was higher in the prior CALAS cohort. The cohort by home care interaction was significant for all three outcome measures.
Table 3.
Logistic Regression Coefficients of Probability of Functional Decline
| ADL-disability | IADL-disability | Functional limitation | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| B | OR | 95% CI | B | OR | 95% CI | B | OR | 95% CI | |
| Step 2 | |||||||||
| Age | 0.09 | 1.10*** | 1.07–1.13 | 0.10 | 1.10*** | 1.07–1.13 | 0.07 | 1.07*** | 1.04–1.10 |
| Gender(Women)a | 0.08 | 1.08 | 0.79–1.49 | 0.54 | 1.72*** | 1.27–2.35 | 0.60 | 1.83*** | 1.32–2.54 |
| Origin (Asia-Africa) | 0.07 | 1.07 | 0.73–1.56 | 0.17 | 1.19 | 0.82–1.73 | 0.90 | 2.46*** | 1.65–3.66 |
| Origin (Europe-America) | −0.35 | 0.69* | 0.49–0.99 | −0.26 | 0.77 | 0.54–1.08 | 0.21 | 1.24 | 0.88–1.74 |
| Educationb | −0.12 | 0.88* | 0.79–0.97 | −0.05 | 0.94 | 0.86–1.04 | −0.05 | 0.94 | 0.86–1.03 |
| Marital status(Married)c | −0.44 | 0.64** | 0.46–0.87 | −0.32 | 0.72* | 0.53–0.98 | −0.15 | 0.85 | 0.62–1.17 |
| Income(other income sources)d | −0.11 | 0.89 | 0.68–1.17 | 0.11 | 1.11 | 0.86–1.45 | −0.10 | 0.90 | 0.68–1.19 |
| Self-rated health | −0.98 | 0.37*** | 0.30–0.45 | −0.99 | 0.37*** | 0.31–0.44 | −1.04 | 0.35*** | 0.29–0.41 |
| Home care(receiving)e | 1.01 | 2.76*** | 2.08–3.65 | 1.11 | 3.04*** | 2.26–4.09 | 1.04 | 2.77*** | 1.95–3.93 |
| Cohort(SHARE-Israel)f | 0.80 | 2.24*** | 1.59–3.14 | 0.36 | 1.44* | 1.05–1.99 | −0.47 | 0.62** | 0.45–0.86 |
| Step 3 | |||||||||
| Cohort X home care | 0.81 | 2.25* | 1.17–4.31 | 0.75 | 2.13* | 1.06–4.27 | 0.95 | 2.60* | 1.03–6.56 |
| Nagelkerke R2 | .31*** | .36*** | .35*** | ||||||
Note. N=1235–1384 respondents after a listwise deletion of cases with missing data. The dependent variables were coded as 0=no difficulty reported, 1=reporting at least one difficulty. Only the additional interaction term is shown in the results of Step 3. ADL=Activities of daily living; IADL=Instrumental activities of daily living. OR=Odds ratio. CI=Confidence interval.
Coded as 1=Men; 2=Women.
Rated on a scale from 0 (pre-primary education) to 6 (second stage tertiary education).
Coded as 1=Not married; 2=Married.
Coded as 1=Only National Insurance; 2=Other income sources.
Coded as 1=Not receiving; 2=Receiving.
Coded as 1=CALAS; 2=SHARE-Israel.
p < .05;
p < .01;
p < .0001.
In order to explore the interactions, cohort was regressed on functional status (controlling for covariates), separately for those who did not receive home care and for those who did. Among those who did not receive home care, we found that cohort contributed to a small degree to the variance in ADL-disability (B=0.55, OR=1.68, 95% CI=1.05–2.68, p<.05) and did not contribute to the variance in IADL-disability (B=0.18, OR=1.20, 95% CI=0.81–1.77, p=0.35). However, it did contribute to the variance in the functional limitation outcome measure (B=−0.64, OR=0.52, 95% CI=0.36–0.75, p=0.001; that is, higher functional limitation was observed in the CALAS cohort).
Among those who did receive home care we found that the cohort variable contributed to the variance in ADL-disability (B=1.22, OR=3.39, 95% CI=1.99–5.76, p<0.0001; i.e., higher ADL-disability in SHARE-Israel) and contributed to the variance in IADL-disability (B=0.97, OR=2.65, 95% CI=1.40–5.02, p=0.003; i.e., higher IADL-disability in SHARE-Israel). However, it did not contribute to the variance in the functional limitation measure (B=0.22, OR=1.24, 95% CI=0.49–3.14, p=0.63). In summary, ADL and IADL difficulties were higher in the SHARE-Israel sample, but mainly for those who were in receipt of home care. In comparison, functional limitation was higher among the respondents in the CALAS sample, but only for those who were in not receipt of home-delivered care.
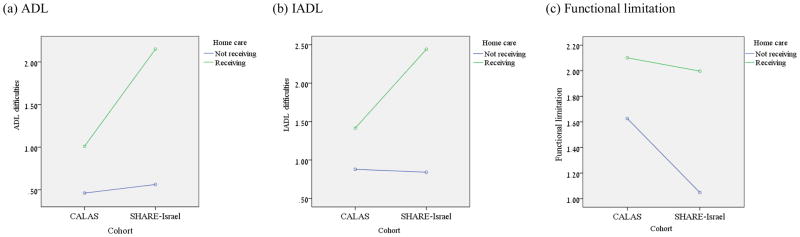
The MANCOVA results revealed that there was an overall effect for the cohort variable (Wilks’ λ =.92, p<.0001) and an overall cohort by home care interaction effect (Wilks’ λ =.97, p<.0001). Moreover, the ADL and IADL difficulties were found to be higher in the SHARE-Israel sample compared to the CALAS respondents: F(1,1383)=39.39, p<.0001, , and F(1,1383)=28.41, p<.0001, , respectively. Functional limitation was higher in the CALAS sample members compared to their counterparts in the SHARE-Israel survey: F(1,1383)=19.18, p<.0001, . All three cohort by home care interaction terms were significant as well: FADL(1,1383)=30.06, p<.0001, , FIADL(1,1383)=35.78, p<.0001, , and F Functional limitation(1,1383)=10.07, p<.01, . A plot of these interactions is presented in Figure 1. The figure demonstrates the same trend that was found in the logistic regressions.
Figure 1.
Functional Decline as a Function of Cohort X Home Care Interaction
Note. ADL = Activities of Daily Living. IADL = Instrumental Activities of Daily Living.
Discussion
This study examined functional status across two successive cohorts of Jewish-Israelis aged 75–94 years. The first study hypothesis, which assumed that the rate of functional decline would decrease across cohorts, received only partial support. That is, the respondents in the SHARE-Israel sample (the later cohort) indeed reported having less functional limitation. However, the two measures of disability—ADL and IADL—were actually higher among the SHARE respondents. This result lends support to the second hypothesis examined in the current analysis that functional decline rates vary in relation to different measures. As the present study indeed showed, the variation in the measures employed actually revealed opposing results.
The answer for this particular discrepancy may lie in the findings related to the third hypothesis in the present inquiry. We hypothesized that lower functional decline in the later cohort would be more evident in measures less related to home care eligibility. Analysis of the interactions of home care and cohort vis-à-vis functional status showed that this was indeed the case. That is, the findings revealed that self-rated ADL and IADL difficulties were higher among the SHARE-Israel respondents who were in receipt of home care than among their CALAS counterparts. As recalled, this later cohort was interviewed after a national program for community long term insurance was already well established. Eligibility for this publicly funded benefit was dependent upon certified disability, as reflected in ADL and IADL-disability ratings. It could be, therefore, that the higher reported disability found in the SHARE-Israel cohort was a function of these respondents’ desire to justify receipt of this social insurance benefit. This was because alternative means of assistance were hardly available, making the community long term insurance a prime target.
At the same time, we cannot rule out the possibility that the community long term care insurance mechanism may have effectively distinguished between those who were disabled and those who were not disabled, explaining why the SHARE-Israel home-care recipients had higher rates of disability. This latter explanation is partially supported by the finding that non-recipients of home care in the SHARE-Israel sample reported fewer difficulties in their functional limitation. Still, unlike the previous explanation, this one does not help to understand the main effect of cohort (higher ADL/IADL-disability in SHARE-Israel).
An additional possible explanation of the cohort differences in relation to reported functional status across these two cohorts should also be considered. It is primarily historical in nature. We note that the members of the CALAS cohort reached mid-life prior to the founding of the State of Israel. This was a period in which a pioneering ethos reigned in major segments of the society (Paine, 1993). As a result, individuals may have tended to view physical difficulties in a more stoic manner. That is, despite having had more physical limitations, they nevertheless reported their dependency levels in day to day tasks as lower.
In comparison, the respondents aged 75 and older in the SHARE-Israel sample reached mid-life after the founding of the State. That is, they reached maturity in an era when greater recognition and legitimacy was given to the need for and provision of formal services, as befits an emerging state structure. This may explain why the SHARE-Israel respondents saw their day to day dependency levels as higher, despite their actually reporting lower functional limitation.
In sum, this analysis shows that functional limitation among Jewish older-old persons in Israel may indeed be declining, as has been found in some other populations. However, the study also found that self-perceived disability in at least part of this same population has apparently increased. We suggest that this particular increase might be a function of changed eligibility criteria for public long-term care benefits. It may also be related to changing views about functional dependency and its legitimacy within Israeli society.
The study also suggests that investigators must look beyond single outcome measurements in their search for explanations of the trends in functional status (Gronvik, 2009). Our results showed discrepant results in functional limitation as opposed to ADL- and IADL-disability across the studied cohorts. While both of these phenomena indicate disablement, the latter also reflects the extent of motivation and efficiency whereby people transform their functional ability into independent functioning. Accordingly, self reports of ADL and ADL difficulties involve subjective and personality aspects (e.g., self perception, resolve, self reliance skills) that go beyond mere functional limitation difficulties.
A few study limitations should be noted as well. First, despite the efforts to achieve maximum harmonization of the measures, it could be that the indicators of home care may have varied somewhat across the two surveys, due to their slightly different phrasing. This might be why there were no significant differences in the respective percentage of home care recipients across the two survey cohorts. Second, cohort comparisons, due to their single-time measurements, cannot confirm a change in functional status, but only differences in the respective cohorts. Longitudinal studies can provide more insight regarding changes in functional status over time. Another possible limitation is related to the fact that the two studies compared in this analysis examined somewhat different data sets which employed different sampling frames and assumptions. Finally, we cannot discount that there may have been other events that occurred in the sixteen years between the surveys which influenced the findings, such as socio-economic changes.
Nevertheless, the current investigation has unique advantages. First is its comparison of different cohorts within a single society in relation to functional status and accompanying sociodemographic characteristics. Second, the inquiry uniquely considered a number of outcome measures across the two different cohorts, controlling for a key contextual factor that stemmed from social policy, namely, home care availability/eligibility. Indeed, as the analysis showed, accessibility to home care services may interface with the reporting of self rated functional difficulties.
In conclusion, we recommend that further investigation should take into account the distinctions that exist in the functional status of older people. We also recommend that additional attention be paid to changing social contexts that may influence how older people rate vital aspects of their functional capability. Consideration of these aspects can contribute to a better understanding of the dynamics behind self-reported functional decline in aging populations.
References
- Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Ben-Ezra M, Shmotkin D. Predictors of mortality in the old-old in Israel: The cross-sectional and longitudinal aging study. Journal of the American Geriatrics Society. 2006;54(6):906–911. doi: 10.1111/j.1532-5415.2006.00741.x. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Glymour MM. How society shapes aging: the centrality of variability. Daedalus. 2006;135(1):105–114. [Google Scholar]
- Brodsky J, Shnoor Y, Be’er S, editors. The elderly in Israel: The 2010 statistical abstract. Jerusalem: The Brookdale Institute; 2011. [Google Scholar]
- Chernew ME, Goldman DP, Pan F, Shang BP. Disability and health care spending among Medicare beneficiaries. Health Affairs. 2005;24:6–W45R52. doi: 10.1377/hlthaff.w5.r42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou KL, Leung JCB. Disability trends in Hong Kong community-dwelling Chinese older adults - 1996, 2000, and 2004. Journal of Aging and Health. 2008;20(4):385–404. doi: 10.1177/0898264308315852. [DOI] [PubMed] [Google Scholar]
- Crimmins EM, Saito Y, Ingegneri D. Trends in disability-free life expectancy in the United States, 1970–90. Population and Development Review. 1997;23(3):555–572. [Google Scholar]
- Donald IP, Foy C, Jagger C. Trends in disability prevalence over 10 years in older people living in Gloucestershire. Age and Ageing. 2010;39(3):337–342. doi: 10.1093/ageing/afq015. [DOI] [PubMed] [Google Scholar]
- Espelt A, Font-Ribera L, Rodriguez-Sanz M, Artazcoz L, Ferrando J, Plaza A, et al. Disability Among Older People in a Southern European City in 2006: Trends in Gender and Socioeconomic Inequalities. Journal of Womens Health. 2010;19(5):927–933. doi: 10.1089/jwh.2009.1608. [DOI] [PubMed] [Google Scholar]
- Freedman VA, Martin LG, Schoeni RF. Recent trends in disability and functioning among in the United States - A systematic review. JAMA-Journal of the American Medical Association. 2002;288(24):3137–3146. doi: 10.1001/jama.288.24.3137. [DOI] [PubMed] [Google Scholar]
- Fuller-Thomson E, Yu B, Nuru-Jeter A, Guralnik JM, Minkler M. Basic ADL Disability and Functional Limitation Rates Among Older Americans From 2000–2005: The End of the Decline? Journals of Gerontology: Biological Sciences and Medical Sciences. 2009;64(12):1333–1336. doi: 10.1093/gerona/glp130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gronvik L. Defining disability: effects of disability concepts on research outcomes. International Journal of Social Research Methodology. 2009;12(1):1–18. [Google Scholar]
- Guralnik JM, Ferrucci L. Assessing the building blocks of function: Utilizing measures of functional limitation. American Journal of Preventive Medicine. 2003;25(3Sii):112–121. doi: 10.1016/s0749-3797(03)00174-0. [DOI] [PubMed] [Google Scholar]
- Knickman JR, Snell EK. The 2030 problem: Caring for aging Baby Boomers. Health Services Research. 2002;37(4):849–884. doi: 10.1034/j.1600-0560.2002.56.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litwin H. Understanding aging in a Middle Eastern context: The SHARE-Israel survey of persons aged 50 and older. Journal of Cross-Cultural Gerontology. 2009;24(1):49–62. doi: 10.1007/s10823-008-9073-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu JF, Chen G, Song XM, Chi I, Zheng XY. Trends in Disability-Free Life Expectancy Among Chinese Older Adults. Journal of Aging and Health. 2009;21(2):266–285. doi: 10.1177/0898264308328978. [DOI] [PubMed] [Google Scholar]
- Manton KG, Corder L, Stallard E. Chronic disability trends in elderly United States populations: 1982–1994. Proceedings of the National Academy of Sciences of the United States of America. 1997;94(6):2593–2598. doi: 10.1073/pnas.94.6.2593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manton KG, Lamb VL, Gu XL. Medicare cost effects of recent US disability trends in the elderly - Future implications. Journal of Aging and Health. 2007;19(3):359–381. doi: 10.1177/0898264307300186. [DOI] [PubMed] [Google Scholar]
- Martin LG, Schoeni RF, Andreski PM. Trends in health of older adults in the united states: past, present, future. Demography. 2010;47:S17–S40. doi: 10.1353/dem.2010.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morginstin B, Baich-Moray S, Zipkin A. Long-Term Care Insurance in Israel: Three Years Later. Ageing International. 2003;20(2):27–31. [Google Scholar]
- Nikolova R, Demers L, Beland F, Giroux F. Transitions in the functional status of disabled community-living older adults over a 3-year follow-up period. Archives of Gerontology and Geriatrics. 2011;52(1):12–17. doi: 10.1016/j.archger.2009.11.003. [DOI] [PubMed] [Google Scholar]
- Paine R. Israel: The making of self in the “pioneering” of the nation. Ethnos. 1993;58(3–4):222–240. [Google Scholar]
- Parker MG, Thorslund M. Health trends in the elderly population: Getting better and getting worse. Gerontologist. 2007;47(2):150–158. doi: 10.1093/geront/47.2.150. [DOI] [PubMed] [Google Scholar]
- Sagardui-Villamor J, Guallar-Castillon P, Garcia-Ferruelo M, Banegas JR, Rodriguez-Artalejo F. Trends in disability and disability-free life expectancy among elderly people in Spain: 1986–1999. Journals of Gerontology: Biological Sciences and Medical Sciences. 2005;60(8):1028–1034. doi: 10.1093/gerona/60.8.1028. [DOI] [PubMed] [Google Scholar]
- Schmid H. The Israeli long-term care insurance law: Selected issues in providing home care services to the frail elderly. Health and Social Care in the Community. 2005;13(3):191–200. doi: 10.1111/j.1365-2524.2005.00548.x. [DOI] [PubMed] [Google Scholar]
- Schoeni RF, Freedman VA, Martin LG. Why is late-life disability declining? Milbank Quarterly. 2008;86:47–89. doi: 10.1111/j.1468-0009.2007.00513.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman TE, Merkin SS, Crimmins EM, Karlamangla AS. Disability Trends Among Older Americans: National Health and Nutrition Examination Surveys, 1988–1994 and 1999–2004. American Journal of Public Health. 2010;100(1):100–107. doi: 10.2105/AJPH.2008.157388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone SD. Disability, dependence, and old age: Problematic constructions. Canadian Journal on Aging-Revue Canadienne Du Vieillissement. 2003;22(1):59–67. [Google Scholar]
- Wolf DA, de Leon CFM, Glass TA. Trends in rates of onset of and recovery from disability at older ages: 1982–1994. Journals of Gerontology: Psychological Sciences and Social Sciences. 2007;62(1):S3–S10. doi: 10.1093/geronb/62.1.s3. [DOI] [PubMed] [Google Scholar]