Abstract
Capsules protect bacteria against phagocytic clearance. Capsular polysaccharides or polyglutamates have evolved also to resist antigen presentation by immune cells, thereby interfering with the production of opsonophagocytic antibodies. Linking capsular material to a carrier protein stimulates its presentation to the immune system. For many conjugate vaccines this is achieved by a process of random chemical cross-linking. Here we describe a new technology, designated sortase-conjugation, which generates a single amide bond between the C-terminal end of a carrier protein and the capsular material. Sortase-conjugation was used to link the poly-D-γ-glutamic acid (PDGA) capsule of Bacillus anthracis to the receptor binding domain (D4) of protective antigen (PagA). When used as a vaccine, PDGA-D4 conjugate elicited robust antibody responses against both capsule and D4. Immunization with PDGA-D4 afforded guinea pigs complete protection against anthrax challenge with wild-type or pagA mutant B. anthracis Ames.
1. Introduction
Avery and colleagues discovered that Streptococcus pneumoniae elaborates a polysaccharide capsule that, when isolated and injected into animals, elicited poor antibody responses [1, 2]. However, antibody production could be stimulated by chemically crosslinking capsule material with a carrier protein [3, 4]. This technology formed the basis of conjugate vaccines that elicit opsonophagocytic antibodies against capsules, thereby generating protection from bacterial diseases [5, 6]. For example, conjugate vaccines protect against Hemophilus influenzae [7], Neisseria meningitidis [8] and Streptococcus pneumoniae [6, 9]. A general feature of chemical crosslinking is the random nature of forming bonds between reactive hydroxyl, carbonyl, carboxyl, and amino groups in carbohydrates and amino acids [10]. Although essential for vaccine manufacturing, chemical crosslinking provides limited rational insight into conjugate antigens as its products are heterogeneous mixtures of molecules. Here we describe sortase-conjugation, a technology that employs a recombinant carrier protein with a C-terminal LPXTG motif [11]. Sortase A cleaves the LPXTG motif [12] and links the C-terminal threonine to a specific amino group within the capsular preparation. Sortase-conjugation was used to synthesize an anthrax conjugate vaccine.
The Gram-positive, spore forming bacterium Bacillus anthracis is the causative agent of anthrax [13]. Infectious spores of B. anthracis germinate in host tissues and replicate as chains of vegetative bacilli, enclosed by a large poly-D-γ-glutamic acid (PDGA) capsule that prevents phagocytosis [14, 15]. Bacilli secrete three proteins - lethal factor (LF), edema factor (EF) and protective antigen (PA) - that assemble into the lethal (LF and PA) and edema toxins (EF and PA) [16, 17]. PA interacts with anthrax toxin receptors to translocate LF and EF into host cells [18], where toxins exert their zinc protease (LF) and adenylate cyclase (EF) functions [19, 20]. The two virulence strategies of B. anthracis, toxin secretion and capsule formation, are encoded by two large virulence plasmids pXO1 and pXO2 [21 , 22]. Loss of virulence plasmid occurs under laboratory conditions and prompted the development of attenuated vaccine strains, Pasteur (pXO1−, pXO2+) and Sterne (pXO1+, pXO2−)[23, 24]. Recent work used chemical crosslinking to conjugate PDGA capsule preparations or synthetic polyglutamates to bovine serum albumin [25], Pseudomonas aeruginosa exotoxin A [26], keyhole limpet hemocyanin [27], PA [28] or the outer membrane complex (OMPC) of Neisseria meningitides type B [29] and observed production of specific antibodies in immunized mice [26, 30]. One of these vaccines, the OMPC conjugate to capsular material, was tested in a mouse model of subcutaneous anthrax challenge and was shown to protect immunized animals against fully virulent B. anthracis Ames spores [29].
2. Materials and Methods
2.1. Bacillus anthracis growth and spore preparations
B. anthracis cultures were grown overnight in Luria broth with or without 0.8% sodium bicarbonate at 37°C and diluted in fresh medium at 37°C. Antibiotics were added to cultures for plasmid selection: 100 μg/ml ampicillin and 50 μg/ml kanamycin for Escherichia coli strains and 20 μg/ml kanamycin for B. anthracis strains. For spore preparation, vegetative cultures of B. anthracis Ames wild-type, pagA or capD mutants were sporulated in modified G medium (0.2% yeast extract, 0.0025% CaCl2 dihydrate, 0.05% KH2PO4, 0.00976% MgSO4 anhydrous, 0.005% MnCl2·4H2O, 0.00073% ZnSO4·7H2O, 0.00005% FeSO4·7H2O, 0.2% (NH4)2·SO4 [31]) until >99% sporulation was observed by light microscopy. Endospores were heat-treated at 68°C for 1h to kill vegetative cells. Spores were washed with sterile ddH2O three times, suspended in sterile H2O and stored frozen at -80°C. Endospore preparations were plated on LB agar to determine CFUs. Endospore preparations were examined by microscopy and found to be >99% purity with no observable vegetative cells or debris. For capsule production, B. anthracis strains were grown in a capsule inducing medium [0.8% nutrient broth (pH 6.8),0.3% yeast extract, 0.7% NaHCO3, 10% horse serum, 25 mM HEPES-KOH, pH 7.5, 1.5% agar] overnight at 37°C in 5% CO2 [32].
2.2. Bacillus anthracis mutants and plasmids
B. anthracis Sterne 34F2 pXO1 was used as a template for PCR amplification of two 1 kb DNA fragments flanking the pagA gene using the primers pagA1 (5′-TTTGGATCCGAGATGAAAATGGTAATATAGCGAATA-3′) and pagA2 (5′-TTTCCCGGGATACGTTCTCCTTTTTGTATAAAATTAAA-3′)(PCR 1) as well as pagA3 (5′-TTTCCCGGG GGTAATTCTAGGTGATTTTTAAATTATCT-3′)and pagA 4 (5′-TTTGAATTCATGTGCCATTGTTTTTAAAAGTTC-3′) (PCR2). PCR products 1 and 2 were restricted with BamH1/XmaI and XmaI/EcoRI, respectively, and ligated into pTS1 cut with BamH1/EcoR1. The recombinant plasmid, pJWK374A was cut with SmaI and ligated to the kanamycin resistance cassette flanked by SmaI1 sites to generate pJWK374B. Plasmid pJWK374B was transformed into E. coli strain K1077 (dam−, dcm−), non-methylated DNA purified and electroporated into B. anthracis Sterne as previously described [33]. Allelic replacement and selection for a kan resistant pagA mutant followed an earlier protocol [34]. Nucleic acid sequences of wild-type and mutant allele were verified by DNA sequencing. The capD variant of B. anthracis Ames has been previously described [32]. The B. anthracis Sterne pagA mutant allele was transduced into B. anthracis Ames strain using CP-51 phage [21]. In brief, the B. anthracis pagA Sterne mutant was grown overnight at 30°C in NBY supplemented with 0.5 % glycerol broth and kanamycin 20 μg/ml, and then refreshed in NBY supplemented with 0.5% glycerol for 3-5 hours at 37°C. Following infection of 100 μl of refreshed donor strain with 100 μl CP-51 WT phage stock, 4 ml of PA soft agar was added and the transduction mix was plated on NBY plates with 0.5 % glycerol. Following 30-46 hours incubation at 30°C, the soft agar was scraped off into 5 ml PA broth. Following centrifugation, the supernatant was passed through 0.22 μm sterile filter.
2.3. Fractionation of Bacillus anthracis cultures
B. anthracis strains were grown overnight in LB with or without 0.8% sodium bicarbonate as indicated. Overnight cultures were diluted 1:100 in fresh medium and grown to an optical density of 3 at 600 nm (A600 3). Total proteins in the cell culture (Total) were obtained by precipitating 1 ml of the culture with 7.5 % trichloroacetic acid (TCA). To assay for protein secretion in the medium, 3 ml of the culture was centrifuged for 5 min at 6,000 ×g. Proteins in 1 ml of supernatant (Sup) were precipitated with 7.5% trichloroacetic acid (TCA). All TCA precipitates were washed with ice-cold acetone, solubilized in 50 μl of 0.5 M Tris-HCl (pH 8.0)/4% SDS and heated at 90°C for 10 min. Proteins were separated on SDS/PAGE and transferred to PVDF membrane for immunoblot analysis with appropriate rabbit polyclonal antibodies. Immunoreactive signals were revealed by using a secondary antibody coupled to horseradish peroxidase and chemiluminescence.
2.4. Sortase conjugation
The D4 domain sequence was amplified with the primers D4-1 (5′-tttggatcctttcattatgatagaaataacatagcagttg-3′) and D4-2 (5′-tttgaattcttattcacccgtagccggaagagcttgagctcctatctcatagccttttttagaaa-3′) primers using pXO1 template DNA. The PCR product was digested with BamHI and EcoRI, inserted into pGEX-2T (GE healthcare, USA) to generate pYT10, which was transformed into E. coli and transformants selected on Luria agar with ampicillin (100 μg/ml). An N-terminal truncated recombinant sortase A (SrtAΔN) was purified as described previously [12]. For GST-D4 purification, E. coli BL21 (DE3) (pYT10) was grown in LB broth at 37°C to OD600 0.6 and induced with 1 mM IPTG for 3 hours. Cells were sedimented by centrifugation, suspended in 30 mL buffer A [50 mM Tris-HCl (pH 7.5), 150 mM NaCl] and lysed in a French pressure cell at 14,000 psi. The extract was centrifuged at 29,000 ×g for 30 min, and the supernatant was applied to 1 ml of glutathione agarose, pre-equilibrated with buffer A. The column was washed with 40 ml of buffer A, and GST-D4 protein was eluted in 5 ml of buffer B [50 mM Tris-HCl (pH 7.5), 150 mM NaCl, 20 mM glutathione]. Excess glutathione was removed by dialysis against buffer A.
The transpeptidation reaction was carried out in 0.5 ml 100 mM HEPES, 150 mM NaCl, 5 mM CaCl2 (pH 7.5) with 0.2 mM GST-D4, 0.1 mM sortase and 1 mM nucleophile (NH2-Gly5-PDGA10) for 12 hours at 37°C. Reaction products were subjected to glutathione agarose affinity chromatography. After washing with buffer A, GST tag was cleaved off with thrombin. Ion-exchange chromatography through MonoQ column (GE-healthcare, USA) was used to purify PDGA-D4 from D4. The reaction products were analyzed by analytical RP-HPLC and characterized with MALDI-MS.
2.5. Animal models of anthrax infection
All animal experiments followed protocols that were reviewed, approved, and supervised by the Institutional Animal Care and Use Committee and the Select Agent Committee at the University of Chicago.
Six week old, female C57BL/6 mice (Jackson Laboratory) were challenged by intra-peritoneal injection of B. anthracis spore suspensions in 100 μl PBS. Aliquots of the spore inoculum were spread on agar plates to enumerate the challenge dose. Infected animals were monitored in 12 hour intervals for survival or a moribund state (inability to remain upright, weight loss, non-responsive to touch) for 14 days. Moribund animals were killed by inhalation of compressed CO2 and cervical dislocation.
Female Hartley guinea pigs (250-350 g) were infected by subcutaneous injection of spores into the inguinal fold of the hind leg. Animals were observed for morbidity and mortality over 14 days. All animals were subjected to necropsy and their site of infection, spleen, liver and lungs removed. Organs were immediately fixed by submersion in 10% neutral-buffered formalin. Samples were submitted to the University of Chicago Animal Pathology Core for serial 4-μm thin sections of embedded tissues and staining with hematoxylin–eosin. Tissue samples were viewed by light microscopy. Organ samples isolated during necropsy were also homogenized in phosphate buffered saline, serially diluted, and plated on LB to enumerate bacterial load as CFU. Alternatively, samples were fixed with neutral buffered formalin and stained with India ink to visualize the capsule of bacilli.
Groups of female Hartley guinea-pigs (250-280 g) were immunized by intramuscular injection into the hind leg with 0.2 ml of 50 μg of PA (List Biological Laboratories, Inc.), D4 or PDGA-D4 absorbed to 25% aluminum hydroxide (Alhydrogel) on days 0, 14 and 28. As a control, 250 μl AVA (Biothrax) was administered at the same time. Blood was collected on day 35 to measure serum antibody titers before challenge. Levels of guinea pig serum immunoglobulin G (IgG) reactive with specific antigens were determined by a custom enzyme-linked immunosorbent assay (ELISA). Briefly, serum samples representative of the immunization groups were aliquoted on microtiter plates pre-coated with purified PA, D4 (5 μg/ml) or PDGA-D4 (20 μg/ml). Binding of serum antibody was detected with secondary antibodies against specific immunoglobulin (anti-guinea pig).
2.6. Statistical analysis
Data were processed using GraphPad PRISM 5.0 software to generate graphs and for statistical analyses. Statistical analysis of serum antibody levels was performed in pairwise comparison using the unpaired two-tailed Student’s t-test. Bacterial load data were also analyzed for statistical significance with the unpaired two-tailed Student’s t-test. Comparisons of animal survival between two groups were evaluated with the Log-rank test.
3. Results
3.1. Sortase-ligation generates the PDGA-D4 conjugate vaccine
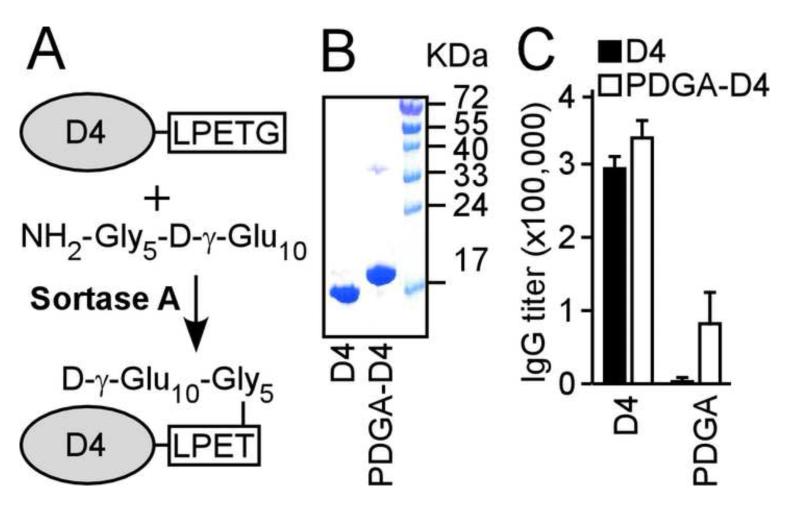
A glutathione S-transferase hybrid with the D4 receptor binding domain of PA, the target of PA toxin neutralizing antibodies [35, 36], was engineered to harbor a C-terminal LPETG motif that is recognized and cleaved by sortase A [37](Fig. 1). We selected NH2-Gly5-γ-D-Glu10 as capsule antigen because this synthetic polyglutamate had previously been well characterized as a chemically crosslinked antigen [30]. Purified GST-D4 was incubated with sortase A [12] and NH2-Gly5-γ-D-Glu10 as a nucleophile (Fig. 1A). The transpeptidation product, D4-LPXT-Gly5-γ-D-Glu10 (designated PDGA-D4), was cleaved off GST and purified (Fig. 1B). When examined by immunoblotting, PDGA-D4 reacted with both PA- and PDGA-specific antibodies, revealing the presence of both antigen determinants in the conjugated product (data now shown). Purified D4 as well as PDGA-D4 were adsorbed to aluminum hydroxide (alhydrogel) and injected into guinea pigs. PDGA-D4 elicited antibody responses against both PDGA capsule and the D4 domain of PA (Fig. 1C). As a control, non-conjugated D4 antigen did not elicit PDGA antibodies (Fig. 1C) and synthetic polyglutamates do not to elicit humoral immune responses [26].
Fig. 1.
Sortase-conjugation generates the PDGA-D4 vaccine. (A) Sortase links the amino group of a synthetic poly-γ-D-glutamate (NH2-Gly5-D-γ-Glu10) to the LPETG sorting signal engineered at the C-terminal end of the protective antigen D4 domain. (B) Sortase-conjugation of PDGA to D4 results in a mobility shift of PDGA-D4 on 15% Coomassie-stained SDS-PAGE. (C) Using a prime-two-booster schedule, guinea pigs (n=7) were immunized with either D4 or PDGA-D4 adsorbed to aluminum hydroxide and serum IgG analyzed for immune reactivity to either D4 or PDGA antigen. Data are representative of two independent determinations.
3.2. PDGA-D4 elicits specific antibodies that protect guinea pigs against anthrax
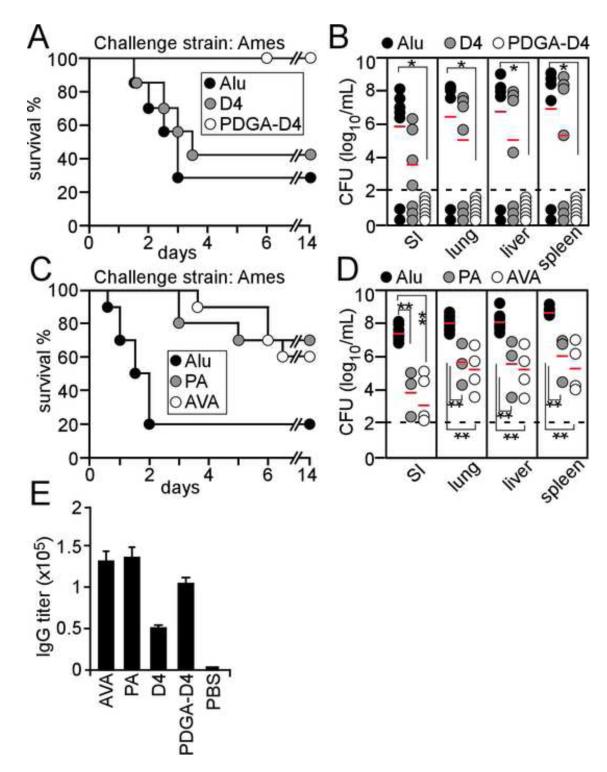
Cohorts of guinea-pigs (n=7) were immunized by intramuscular injection with a prime-two booster immunization schedule of 50 μg PDGA-D4 or D4 adsorbed to aluminum hydroxide in fourteen day intervals. Two-weeks following the final booster, animals were challenged with 1.6×103 spores derived from B. anthracis Ames (80 LD50 doses) (Fig. 2). As a control, animals that did not receive vaccine or adjuvant (mock) were not protected against lethal anthrax challenge (Fig. 3E). Most of the animals that received aluminum hydroxide succumbed to B. anthracis Ames challenge (Fig. 2A). Nevertheless, depending on the challenge dose, 10-25% of aluminum hydroxide treated animals survived (Fig. 2A). This is an expected result, as the adjuvant effect of aluminum hydroxide in guinea pigs generates non-specific protection against anthrax [38]. In contrast to D4 immunized animals, which exhibited no disease protection compared to aluminum hydroxide, all guinea pigs that received PDGA-D4 vaccine survived the B. anthracis Ames spore challenge (P<0.01)(Fig. 2A). At the end of the observation period, animals were euthanized and subjected to necropsy. Microbiological analysis of tissue homogenates from PDGA-D4 immunized guinea pigs failed to detect B. anthracis, suggesting that the conjugate vaccine induced sterilizing immunity (Fig. 2B). Aluminum hydroxide or D4 immunized animals that succumbed to anthrax disease harbored high loads of vegetative bacilli at the site of infection (SI) as well as in liver, lung or spleen tissues (Fig. 2B). As compared to aluminum hydroxide alone, immunization with D4 did not cause a significant reduction in the load of vegetative bacilli in guinea pig organ tissue (Fig. 2B).
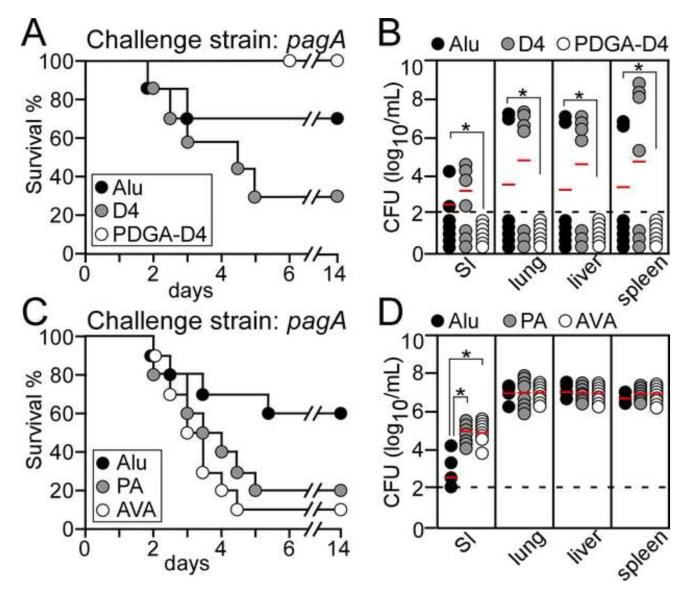
Fig. 2.
PDGA-D4 protects guinea pigs from challenge with wild-type B. anthracis Ames spores. (A) Guinea pigs (n=7) were immunized with a prime-two booster schedule with either PDGA-D4 or D4 alone adsorbed to Alhydrogel adjuvant (aluminum hydroxide) or with adjuvant alone (Alu). Animals were challenged by subcutaneous inoculation with 1.6×103 B. anthracis Ames spores and monitored over 14 days for disease and survival. (B) B. anthracis replication in guinea pigs infected as described in (A) at either the site of infection (SI) or in lung, liver and spleen tissues. Bacterial load was determined by plating homogenized tissues on agar and enumerating colony formation. (C) Guinea pigs (n=10) were immunized with anthrax vaccine adsorbed (AVA, BioThrax®), protective antigen (PA) adsorbed to Alhydrogel or Alhydrogel adjuvant alone (Alu) using the same schedule and challenge as in (A). (D) B. anthracis replication in guinea pigs infected as described in (C). The Log-rank test was used to determine significance in animal survival (A and C): PDGA-D4 vs. Alu, P<0.01; AVA vs. Alu, P<0.01; PA vs. Alu, P<0.01. The two-tailed unpaired student’s t-test was used to analyze differences in B. anthracis load in guinea pig tissues of vaccine cohorts compared with adjuvant control (Alu): *P<0.01,**P<0.001. (E) Guinea pigs (n=10) were immunized with a prime-two-booster schedule in 14 day intervals using either AVA, PA, D4 or PDGA-D4 adsorbed to Alhydrogel or a mock (PBS/Alhydrogel) control. PA-specific serum IgG titers of animals were analyzed on day 36 of the immunization schedule. All animal data are representative of two independent determinations.
Fig. 3.
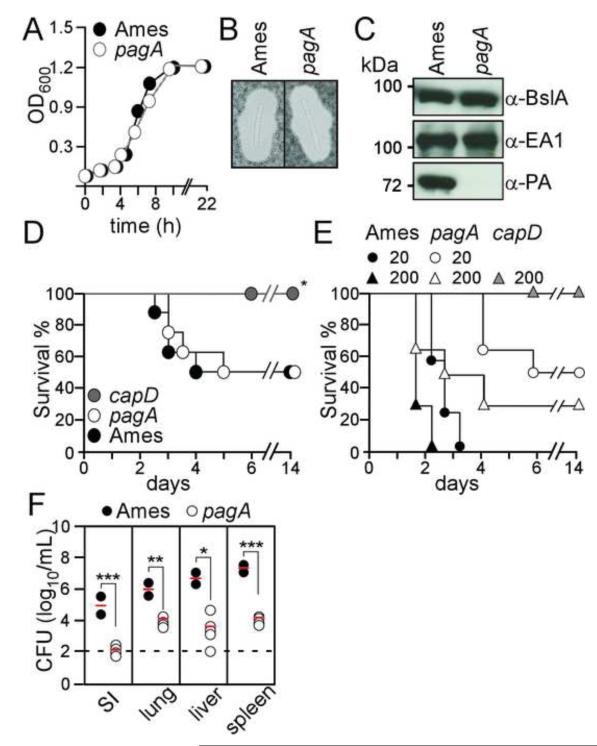
Protective antigen (pagA) deficient Bacillus anthracis Ames are attenuated in guinea pigs. (A) Growth of wild-type and pagA mutant B. anthracis Ames in LB broth cultures were monitored as the absorbance at 600 nm. (B) B. anthracis wild-type (Ames) and pagA mutant strains were grown in the presence of carbon dioxide and stained with India ink to reveal the poly-D-γ-glutamic acid (PDGA) capsule. (C) Immunoblotting of B. anthracis culture supernatants with rabbit antibodies specific for BslA, EA1 and protective antigen (PA). (D) Wild-type B. anthracis (Ames), pagA and capD mutant spores (3×102 CFU) were injected into the peritoneal cavity of C57Bl/6 mice and animal morbidity and mortality was monitored. Statistical significance was examined with the Log-rank test (* indicates P <0.01). Data are representative of two independent determinations. (E) B. anthracis wild-type (Ames), pagA and capD mutant spores were injected into the inguinal fold of guinea pigs; animal survival and disease were monitored. The Log-rank test was used to determine significance in animal survival: capD (200 spores) vs. wild-type (Ames) (20 spores); P<0.01. (F) B. anthracis replication at the site of infection (SI) or dissemination into lung, liver and spleen was enumerated by plating homogenized tissues on agar media and incubation for colony formation. Differences in bacterial load between wild-type (Ames) and pagA mutant were examined with the unpaired two-tailed student’s t-test: *P<0.05, **P<0.001, ***P<0.0001. Data are representative of two independent determinations.
We sought to compare PDGA-D4 with established anthrax vaccines, either purified protective antigen (PA) or anthrax vaccine absorbed (AVA), the aluminum hydroxide adsorbed precipitate of B. anthracis V63340 77/-NP1-R (pXO1+, pXO2−) culture supernatants [39]. PA is the principal immunogen of AVA [40] and purified PA is pursued as a next generation human anthrax vaccine [39]. Cohorts of guinea-pigs (n=10) were immunized by intramuscular injection with 50 μg PA adsorbed to aluminum hydroxide or 250 μl AVA (Biothrax®) using the same prime-two booster schedule and challenge dose as described above. Immunization with AVA, PA, PDGA-D4 or D4 alone raised PA-specific IgG antibody responses in guinea pigs (Fig. 2E). PA as well as AVA immunization afforded guinea pigs significant protection from B. anthracis Ames challenge (P<0.01; Fig. 2C). AVA or PA immunization reduced the bacterial load at the site of infection as well as in lung, liver and spleen tissues (Fig. 2D). Nevertheless, neither of the two vaccines elicited full protection or sterilizing immunity against anthrax disease (Fig. 2D).
3.3. Virulence of capsule and pagA mutant Bacillus anthracis
We sought to examine the efficacy of AVA, PA and PDGA-D4 vaccines against B. anthracis Ames variants lacking the corresponding traits of vaccine antigens. To do so, we isolated a B. anthracis Ames mutant harboring a replacement of the pagA gene on the pXO1 virulence plasmid with the kanamycin resistance marker. The pagA mutant as well as a previously isolated capsule (capD) variant [32] formed spores and replicated in laboratory media at the same rate as wild-type bacilli (Fig. 3A). Growth in the presence of 5% CO2 led to the formation of encapsulated vegetative forms for both wild-type and pagA mutant bacilli (Fig. 3B) but not for capD mutants [32]. Cultures of vegetative bacilli grown in the presence of bicarbonate were centrifuged, thereby separating extracellular media and bacterial sediment. Proteins in the supernatant were precipitated with TCA and probed by immunoblotting (Fig. 3C). B. anthracis Ames secreted PA into the culture medium, whereas the pagA mutant strain did not (Fig. 3C). As a control, the pagA mutant expressed the pXO1-encoded S-layer-associated protein BslA [41] at a level similar to wild-type bacilli (Fig. 3C).
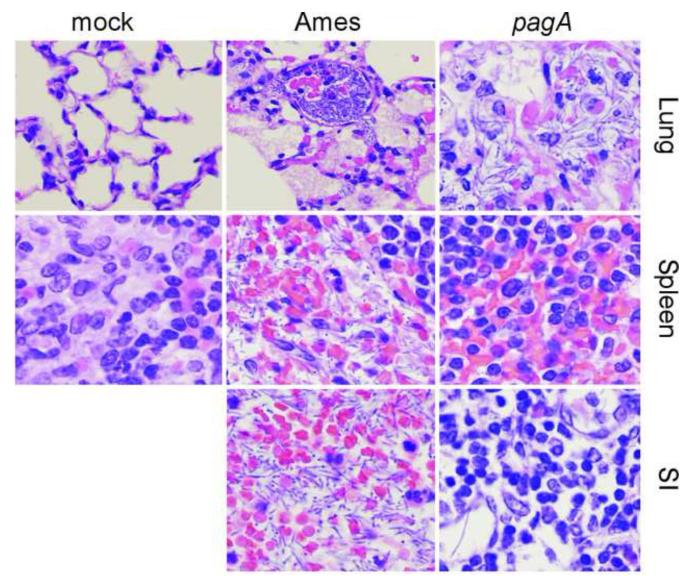
We asked whether the pagA mutant isolated here displayed the same level of virulence as a variant with the omega-kanamycin cassette replacing pagA, which displays no virulence defect in mice [42]. Spores (300 CFU) derived from B. anthracis Ames wild-type or the pagA mutant were injected into the peritoneal cavity of C57BL/6 mice (Fig. 3D). Both wild-type and pagA mutant bacilli replicated in murine tissues and killed about half of the experimental animals (Fig. 3D). These data are in agreement with earlier work, reporting that pagA mutant B. anthracis spores do not display a virulence defect in a subcutaneous injection model for anthrax disease in mice [42]. As a control, intraperitoneal injection of 300 spores derived from the B. anthracis Ames capD mutant [32] did not cause lethal disease in mice (Fig. 3D). Guinea pigs (n=10, 6-week old females) were infected with B. anthracis spores and animal survival was monitored (Fig. 3E). Animals infected with 20 or 200 spores of B. anthracis Ames succumbed to challenge within four days (Fig. 3E). By comparison, animals infected with pagA mutant spores displayed delayed time-to-death and increased survival (Fig. 3E). In contrast to the 10 fold increase in LD50 dose of the pagA mutation, deletion of capD causes a 1,000 fold reduction in virulence [32]. Animals infected with 200 spores of wild-type B. anthracis Ames displayed massive replication of vegetative forms at the SI (105 CFU) as well as pathogen dissemination to lung, liver and spleen (Fig. 3F). Edema and hemorrhage were detected at the SI and in peripheral organs of B. anthracis Ames infected guinea pigs (Fig. 4). Histopathology revealed B. anthracis vegetative forms with massive invasion of polymorphonuclear leukocytes and macrophages (Fig. 4). Replication of the pagA mutant at the site of infection was reduced by about 2-3 log10 CFU (P<0.0001) (Fig. 3F) and did not elicit edema or hemorrhage (Fig. 4). Dissemination of the pagA mutant to liver, lung and spleen tissues was also reduced by 2-3 log10 CFU (Fig. 3F). The severe attenuation caused by the capD deletion prevented further analysis of this mutant for vaccine efficacy studies.
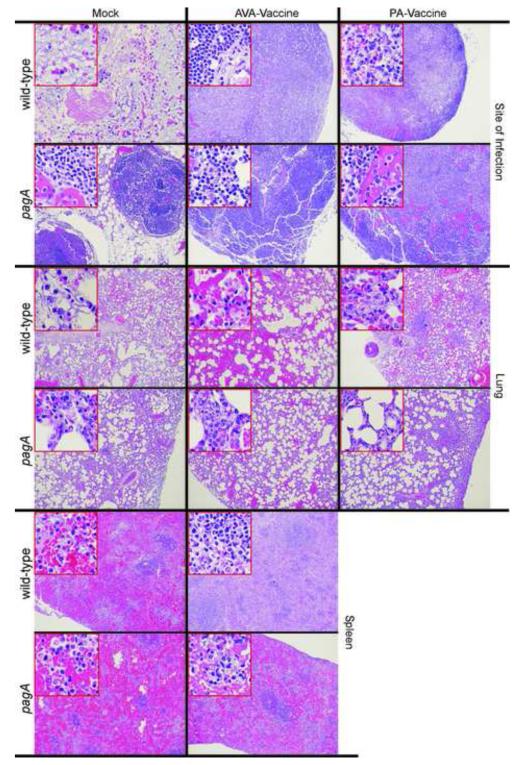
Fig. 4.
Histopathology of anthrax disease in guinea pigs caused by subcutaneous injection of B. anthracis Ames wild-type or pagA mutant spore. Tissue from the site of infection (SI) of guinea pigs challenged with B. anthracis Ames or the pagA mutant strain as well as lung or spleen tissues were fixed, thin-sectioned, stained with hematoxylin-eosin and light microscopy images captured (40× magnification). Tissues from mock infected animals are included as a control.
3.4. PDGA-D4 protects guinea pigs against challenge with pagA mutant bacilli
Cohorts of guinea-pigs were immunized by intramuscular injection with three doses of 50 μg PA, D4, PDGA-D4 or mock (PBS) adsorbed to aluminum hydroxide or 250 μl AVA in fourteen day intervals. Two-weeks following the final immunization, animals were challenged with 3.6×103 spores derived from the B. anthracis pagA mutant (Fig. 5). PDGA-D4 immunization protected all guinea pigs against challenge with the pagA mutant strain (Fig. 5A). Compared to aluminum hydroxide treated animals, immunization with the D4 antigen did not increase the survival of guinea pigs subsequently challenged with the pagA mutant strains (Fig. 5A). When analyzed for bacterial load in host tissues, B. anthracis vegetative forms or spores were not detected in the tissues of PDGA-D4 immunized animals (Fig. 5B). In contrast, animals that had been immunized with D4 alone and that succumbed to pagA mutant challenge harbored large numbers bacilli at the SI and in liver, lung or spleen tissues (Fig. 5B). AVA and PA immunized guinea pigs were also not protected against challenge with pagA mutant spores when compared with the adjuvant alone control cohort (Fig. 5C). To test whether immunization with AVA or PA affected the ability of pagA mutants to replicate in host tissues, we examined the bacterial load at the SI and distant organ sites. Compared to mock immunized animals, AVA or PA vaccinated guinea pigs harbored an increased load of the pagA mutant at the SI but not in peripheral organ tissues (Fig. 5D). Similar results as described above for 3.2×103 pagA mutant spores with PDGA-D4 and AVA immunized guinea pigs were obtained when vaccinated animals received a challenge of 2×104 pagA mutant spores (Fig. 6).
Fig. 5.
PDGA-D4 immunized guinea pigs are protected against anthrax challenge with pagA mutant spores. (A) Guinea pigs (n=7) were immunized with a prime-two booster schedule with either PDGA-D4 or D4 alone adsorbed to Alhydrogel or with adjuvant alone (Alu). Animals were challenged by subcutaneous inoculation with 3.2×103 spores derived from the B. anthracis Ames pagA variant and monitored over 14 days for disease and survival. (B) B. anthracis pagA replication in guinea pigs infected as described in (A) at either the site of infection (SI) or in lung, liver and spleen tissues. Bacterial load was determined by plating homogenized tissues on agar and enumerating colony formation. (C) Guinea pigs (n=10) were immunized with anthrax vaccine adsorbed (AVA / BioThrax®), protective antigen (PA) adsorbed to Alhydrogel or Alhydrogel adjuvant alone (Alu) using the same schedule and challenge as in (A). (D) B. anthracis replication in guinea pigs infected as described in (C). The Log-rank test was used to determine significance in animal survival (A and C): PDGA-D4 vs. Alu, P<0.01; Alu vs. AVA, P<0.01; Alu vs. PA, P<0.01. The two-tailed unpaired student’s t-test was used to analyze differences in B. anthracis load in guinea pig tissues of vaccine cohorts compared with adjuvant control (Alu): *P<0.01. All animal data are representative of two independent determinations.
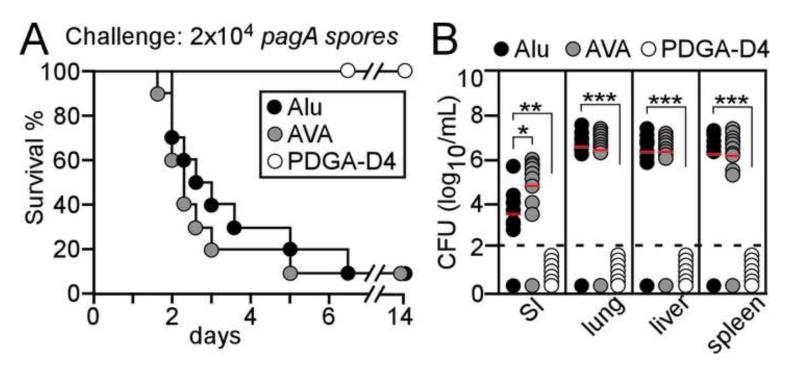
Fig. 6.
PDGA-D4 immunized guinea pigs are protected against anthrax challenge with pagA mutant spores. (A) Guinea pigs (n=10) were immunized with a prime-two booster schedule with either PDGA-D4 adsorbed to Alhydrogel or anthrax vaccine adsorbed (AVA / BioThrax®) or with adjuvant alone (Alu). Animals were challenged by subcutaneous inoculation with 2×104 spores derived from the B. anthracis Ames pagA variant and monitored over 14 days for disease and survival. (B) B. anthracis pagA replication in guinea pigs infected as described in (A) at either the site of infection (SI) or in lung, liver and spleen tissues. Bacterial load was determined by plating homogenized tissues on agar and enumerating colony formation. The Log-rank test was used to determine significance in animal survival (A): PDGA-D4 vs. Alu, P<0.001; PDGA-D4 vs. AVA, P<0.001. The two-tailed unpaired student’s t-test was used to analyze differences in B. anthracis load in guinea pig tissues of vaccine cohorts compared with adjuvant control (Alu): *P≤0.01, *P≤0.001, *P≤0.001. All animal data are representative of two independent determinations.
3.5. Histopathology of anthrax disease caused by wild-type and pagA mutant bacilli
Guinea pigs that had been immunized with PA, AVA or PBS-aluminum hydroxide (mock) and infected with wild-type or pagA mutant B. anthracis Ames spores were monitored for the development of anthrax disease and were then euthanized and necropsied. Tissues from the site of infection, the lung or the spleen were analyzed for histopathology using thin-sectioned hematoxylin-eosin stained samples (Fig. 7). As compared to mock (PBS-aluminum hydroxide) immunized guinea pigs, AVA as well as PA immunization ameliorated the severity of hemorrhagic lesions, immune cell necrosis and vegetative replication associated with B. anthracis Ames spore inoculation at the SI (Fig. 7). Instead, PA and AVA vaccinated animals formed a granuloma at the SI, which appeared to restrict replication and dissemination of the germinated pathogen (Fig. 7). In PBS-aluminum hydroxide treated animals, vegetative replication of the pagA mutant occurred within a similar granuloma (Fig. 7). SI lesions in AVA or PA immunized guinea pigs challenged with pagA mutant spores were marked by hemorrhagic zones and necrosis of immune cells (Fig. 7).
Fig. 7.
Histopathology of AVA and PA vaccinated guinea pigs following challenge with B. anthracis spores. Guinea pigs (n=10) were immunized with a prime-two booster schedule with either AVA or PA adsorbed to Alhydrogel or a mock (PBS/Alhydrogel) control and challenged by subcutaneous inoculation with B. anthracis Ames (wild-type) or pagA mutant spores. Moribund animals were killed and the inguinal site of infection, the lung as well as spleen tissues were removed during necropsy. Tissues were fixed, thin-sectioned, stained with hematoxylin-eosin and light microscopy images captured (macro images are 4.2× and insets 40× magnification of histology slides except the SI of the mock immunized animal, which was captured at 20× magnification). Tissues from mock (PBS-aluminum hydroxide) immunized animals are included as a control.
Mock immunized guinea pigs infected with B. anthracis Ames spores developed interstitial pneumonia with a large burden of vegetative bacilli (Fig. 7). Lung histopathology of mock immunized animals infected with the pagA mutant showed a large immune cell infiltrate and moderate replication of the pathogen (Fig. 7). AVA or PA immunization limited B. anthracis Ames (wild-type) replication within the lung: only sporadic immune cell infiltrates and occasional vegetative forms could be detected (Fig. 7). When AVA or PA immunized guinea pigs were challenged with pagA mutant bacilli, the lung interstitial space was enlarged by infiltrates of healthy or necrotic immune cells and the vegetative forms of pagA mutant bacilli (Fig. 7).
Virulent B. anthracis strains replicate to the highest numbers in the spleen of their infected hosts (Fig. 2B). As expected, large numbers of B. anthracis Ames vegetative forms established microcolonies in spleen tissues of mock immunized animals (Fig. 7). Vegetative forms of the pagA mutant were associated with moderate immune cell infiltrates without changing the overall architecture of the spleen (Fig. 7). Spleen tissues of AVA immunized guinea pigs did not reveal anthrax pathology when animals were infected with B. anthracis Ames spores (Fig. 7). However, AVA-vaccinated animals challenged with pagA mutant spores displayed vegetative forms and immune cell infiltrates replacing the red and white pulp architecture of spleen tissue (Fig. 7). Of note, in PDGA-D4 immunized animals, tissues from the SI, liver, lung or spleen of guinea pigs that had been challenged with wild-type or pagA mutant B. anthracis Ames spores did not harbor histopathology lesions.
4. Discussion
Sortase-conjugation is an enzymatic technology that generates capsule-conjugates with an engineered carrier protein. A key strength of this technology is its ability to generate a single amide bond linking capsular material to a protein carrier. Virtually any protein carrier can be used for this technology provided the LPXTG motif (sortase recognition sequence) is engineered into the recombinant protein [43]. Thus, sortase-conjugation introduces molecular biology tools into the design of bacterial conjugate vaccines to exploit the availability of hybrid proteins with unique adjuvant and antigenic attributes for the design of specific conjugates. Depending on the sortase enzyme [43], sortase-conjugation can use many different nucleophiles, which under physiological conditions are provided by the cell wall cross-bridges in bacterial peptidoglycan [44]. Sortases have been modified to recognize different nucleophiles [45] and may therefore be engineered to recognize a broad spectrum of chemically heterogeneous nucleophiles from the polysaccharides or polyglutamates found in bacterial capsules.
We applied sortase-conjugation towards the development of an anthrax vaccine. By linking the C-terminal end of the D4 domain to a fifteen residue peptide harboring a ten residue poly-D-γ-glutamate, we generated a conjugate that raised both D4- and PDGA-specific immune responses and protected guinea pigs against lethal challenge with fully virulent B. anthracis Ames spores. Of note, immune responses derived from the D4 domain alone did not raise protection, indicating that protective immunity derived from the PDGA-D4 vaccine is raised by antibodies that recognize γ-D-glutamate10. Longer polyglutamate peptides may raise higher antibody titers than the 10-mer used in this report [30]. If so, sortase-conjugated anthrax vaccines may be improved by linking the C-terminal end of full length PA, which (unlike D4) alone elicits significant protective immunity in guinea pigs, to capsule peptides with increased length.
We examined B. anthracis variants lacking the corresponding traits of vaccine antigens for their ability to escape protective immunity. Previous work demonstrated that pagA (PA), cya (EF) and lef (LF) mutants of B. anthracis Ames are fully virulent in a mouse model for anthrax disease [42]. Further, B. anthracis variants lacking cya or lef, but not pagA mutants, have been tested in a respiratory challenge model in guinea pigs, which revealed a key contribution for edema toxin in this model [46]. We show here that a pagA variant of B. anthracis Ames is defective for multiplication at the SI and displayed reduced dissemination to other organ tissues. Whereas immunization with AVA or PA-vaccines generated significant protection against B. anthracis Ames spore challenge, these vaccines did not protect guinea pigs against pagA mutant spores. Experiments in Fig. 5 suggested that AVA and PA immunized guinea pigs may be more sensitive to challenge with pagA mutant spores than mock-vaccinated animals; the immunological basis for this phenomenon is not known. Preclinical anthrax vaccine studies routinely employ mice, guinea pigs, rabbits and non-human primates [39]. We believe that AVA or PA vaccine efficacy against pagA mutant spore challenge should be examined in any one of these models to ascertain whether the results reported here for guinea pigs represent a general phenomenon. Finally, because capsule mutants are severely attenuated in mice [47] and in guinea pigs [32], these species cannot be used to examine PDGA-D4 vaccine efficacy against variants lacking the corresponding capsule antigen. Future work must assess the contribution of capsule genes towards the pathogenesis of anthrax in rabbits and non-human primate models as well as the role of PDGA-D4 in protecting these species against lethal anthrax spore challenge.
Highlights.
>Sortase forms a single covalent bond between a carrier protein and a capsule antigen. >PDGA-D4 vaccine includes polyglutamate and the D4 domain of protective antigen. >PDGA-D4 elicits immunity against Bacillus anthracis challenge in guinea pigs. >PDGA-D4 elicits immunity against pagA mutant Bacillus anthracis. >Sortase-conjugation may be broadly useful to generate conjugate vaccines.
Acknowledgements
The authors acknowledge membership within and support from the Region V “Great Lakes” Regional Center of Excellence (GLRCE) in Biodefense and Emerging Infectious Diseases Consortium (NIH Award 1-U54-AI-057153). We thank the Animal Research and Immunology Core of the GLRCE for help with animal experiments. This work was supported by the NIH/NIAID Award R01-AI069227. We thank members of our laboratory and Emil C. Gotschlich (Rockefeller University) for discussion and Justin Kern for generating the B. anthracis Sterne pagA mutation. We acknowledge the contributions of the National Science Advisory Board for Biosecurity (NSABB) for review and comments on this manuscript. The following reagent was obtained from the NIH Biodefense and Emerging Infections Research Resources Repository, NIAID, NIH: Bacillus anthracis Protective Antigen (PA).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Dochez AR, Avery OT. The elaboration of specific soluble substance by pneumococcus during growth. J Exp Med. 1917;26:477–93. doi: 10.1084/jem.26.4.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Heidelberger M, Goebel WF, Avery OT. The soluble specific substance of pneumococcus: third paper. J Exp Med. 1925;42:727–45. doi: 10.1084/jem.42.5.727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Goebel WF, Avery OT. Chemo-immunological studies on conjugated carbohydrate-proteins. I. Synthesis of p-aminophenol β-glucoside, p-aminophenol β-galactoside, and their coupling with serum globulin. J Exp Med. 1929;50:521–31. doi: 10.1084/jem.50.4.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Avery OT, Goebel WF. Chemo-immunological studies on conjugated carbohydrate-protein. V. The immunological specificity of an antigen prepared by combining the capsular polysaccharide of type III pneumococcus with foreign protein. J Exp Med. 1931;54:437–47. doi: 10.1084/jem.54.3.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Robbins JB, Schneerson R. Polysaccharide-protein conjugates: a new generation of vaccines. J Infect Dis. 1990;161:821–32. doi: 10.1093/infdis/161.5.821. [DOI] [PubMed] [Google Scholar]
- [6].Siber GR. Pneumococcal disease: prospects for a new generation of vaccines. Science. 1994;265:1385–7. doi: 10.1126/science.8073278. [DOI] [PubMed] [Google Scholar]
- [7].Robbins JB, Schneerson R. Haemophilus influenzae type b: the search for a vaccine. Pediatr Infect Dis J. 1987;6:791–4. doi: 10.1097/00006454-198708000-00039. [DOI] [PubMed] [Google Scholar]
- [8].Gotschlich EC, Liu TY, Artenstein MS. Human immunity to the meningococcus. IV. Immunogenicity of group A and group C meningococcal polysaccharides in human volunteers. J Exp Med. 1969;129:1367–84. doi: 10.1084/jem.129.6.1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].MacLeod CM, Hodges RG, Heidelberger M, Bernhard WG. Prevention of pneumococcal pneumonia by immunization with specific capsular polysaccharides. J Exp Med. 1945;82:445–65. [PMC free article] [PubMed] [Google Scholar]
- [10].Hermanson GT. Bioconjugate techniques. Academic Press; New York: 2008. [Google Scholar]
- [11].Schneewind O, Model P, Fischetti VA. Sorting of protein A to the staphylococcal cell wall. Cell. 1992;70:267–81. doi: 10.1016/0092-8674(92)90101-h. [DOI] [PubMed] [Google Scholar]
- [12].Ton-That H, Liu G, Mazmanian SK, Faull KF, Schneewind O. Purification and characterization of sortase, the transpeptidase that cleaves surface proteins of Staphylococcus aureus at the LPXTG motif. Proc Natl Acad Sci USA. 1999;96:12424–9. doi: 10.1073/pnas.96.22.12424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Koch R. Die Ätiologie der Milzbrand-Krankheit, begründet auf die Entwicklungsgeschichte des Bacillus anthracis. Beiträge zur Biologie der Pflanzen. 1876;2:277–310. [Google Scholar]
- [14].Preisz H. Experimentelle Studien über Virulenz, Empfänglichkeit und Immunität beim Milzbrand. Zeitschrift für Immunitäts-Forschung. 1909;5:341–452. [Google Scholar]
- [15].Bruckner V, Kovacs J, Denes G. Structure of poly-D-glutamic acid isolated from capsulated strains of B. anthracis. Nature. 1953;172:508. doi: 10.1038/172508a0. [DOI] [PubMed] [Google Scholar]
- [16].Smith H, Keppie J, Stanley JL. The chemical basis of the virulence of Bacillus anthracis. V. The specific toxin produced by Bacillus anthracis in vivo. Br J Exp Pathol. 1955;36:460–72. [PMC free article] [PubMed] [Google Scholar]
- [17].Collier RJ, Young JA. Anthrax toxin. Annu Rev Cell Dev Biol. 2003;19:45–70. doi: 10.1146/annurev.cellbio.19.111301.140655. [DOI] [PubMed] [Google Scholar]
- [18].Bradley KA, Mogridge J, Mourez M, Collier RJ, Young JA. Identification of the cellular receptor for anthrax toxin. Nature. 2001;414:225–9. doi: 10.1038/n35101999. [DOI] [PubMed] [Google Scholar]
- [19].Duesbery NS, Webb CP, Leppla SH, Gordon VM, Klimpel KR, Copeland TD, et al. Proteolytic inactivation of Map-kinase-kinase by anthrax lethal factor. Science. 1998;280:734–7. doi: 10.1126/science.280.5364.734. [DOI] [PubMed] [Google Scholar]
- [20].Leppla SH. Anthrax toxin edema factor: a bacterial adenylate cyclase that increases cyclin AMP concentrations in eukaryotic cells. Proc Natl Acad Sci USA. 1982;79:3162–6. doi: 10.1073/pnas.79.10.3162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Green BD, Battisti L, Koehler TM, Thorne CB, Ivins BE. Demonstration of a capsule plasmid in Bacillus anthracis. Infect Immun. 1985;49:291–7. doi: 10.1128/iai.49.2.291-297.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Ivins BE, Ezzell JWJ, Jemski J, Hedlund KW, Ristroph JD, Leppla SH. Immunization studies with attenuated strains of Bacillus anthracis. Infect Immun. 1986;52:454–8. doi: 10.1128/iai.52.2.454-458.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Pasteur L. Le vaccin du charbon. Comptes Rendus Hebdomadaires des Scéances de l’Académie des Sciences. 1881;92:666–8. [Google Scholar]
- [24].Sterne M. Anthrax vaccines. J Am Vet Med Assoc. 1988;192:141. [PubMed] [Google Scholar]
- [25].Chabot DJ, Scorpio A, Tobery SA, Little SF, Norris SL, Friedlander AM. Anthrax capsule vaccine protects against experimental infection. Vaccine. 2004;23:43–7. doi: 10.1016/j.vaccine.2004.05.029. [DOI] [PubMed] [Google Scholar]
- [26].Schneerson R, Kubler-Kielb J, Liu TY, Dai ZD, Leppla SH, Yergey A, et al. Poly(gamma-D-glutamic acid) protein conjugates induce IgG antibodies in mice to the capsule of Bacillus anthracis: a potential addition to the anthrax vaccine. Proc Nat Acad Sci USA. 2003;100:8945–50. doi: 10.1073/pnas.1633512100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Wang TT, Fellows PF, Leighton TJ, Lucas AH. Induction of opsonic antibodies to the gamma-D-glutamic acid capsule of Bacillus anthracis by immunization with a synthetic peptide-carrier protein conjugate. FEMS Immunol Med Microbiol. 2004;40:231–7. doi: 10.1016/S0928-8244(03)00366-3. [DOI] [PubMed] [Google Scholar]
- [28].Rhie GE, Roehrl MH, Mourez M, Collier RJ, Mekalanos JJ, Wang JY. A dually active anthrax vaccine that confers protection against both bacilli and toxins. Proc Natl Acad Sci USA. 2003;100:10925–30. doi: 10.1073/pnas.1834478100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Joyce J, Cook J, Chabot D, Hepler R, Shoop W, Xu Q, et al. Immunogenicity and protective efficacy of Bacillus anthracis poly-gamma-D-glutamic acid capsule covalently coupled to a protein carrier using a novel triazine-based conjugation strategy. J Biol Chem. 2006;281:4831–43. doi: 10.1074/jbc.M509432200. [DOI] [PubMed] [Google Scholar]
- [30].Kubler-Kielb J, Liu TY, Mocca C, Majadly F, Robbins JB, Schneerson R. Additional conjugation methods and immunogenicity of Bacillus anthracis poly-gamma-D-glutamic acid-protein conjugates. Infect Immun. 2006;74:4744–9. doi: 10.1128/IAI.00315-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Kim HU, Goepfert JM. A sporulation medium for Bacillus anthracis. J Appl Bacteriol. 1974 Jun;37:265–7. doi: 10.1111/j.1365-2672.1974.tb00438.x. [DOI] [PubMed] [Google Scholar]
- [32].Richter GS, Anderson VJ, Garufi G, Lu L, Joachimiak A, He C, et al. Capsule anchoring in Bacillus anthracis occurs by a transpeptidation mechanism that is inhibited by capsidin. Mol Microbiol. 2009;71:404–20. doi: 10.1111/j.1365-2958.2008.06533.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Gaspar AH, Marraffini LA, Glass EM, DeBord KL, Ton-That H, Schneewind O. Bacillus anthracis sortase A (SrtA) anchors LPXTG motif-containing surface proteins to the cell wall envelope. J Bacteriol. 2005;187:4646–55. doi: 10.1128/JB.187.13.4646-4655.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Marraffini LA, Schneewind O. Targeting proteins to the cell wall of sporulating Bacillus anthracis. Mol Microbiol. 2006 Dec;62:1402–17. doi: 10.1111/j.1365-2958.2006.05469.x. [DOI] [PubMed] [Google Scholar]
- [35].Little SF, Novak JM, Lowe JR, Leppla SH, Singh Y, Klimpel KR, et al. Characterization of lethal factor binding and cell receptor binding domains of protective antigen of Bacillus anthracis using monoclonal antibodies. Microbiology. 1996;142:707–15. doi: 10.1099/13500872-142-3-707. [DOI] [PubMed] [Google Scholar]
- [36].Brossier F, Levy M, Landier A, Lafaye P, Mock M. Functional analysis of Bacillus anthracis protective antigen by using neutralizing monoclonal antibodies. Infect Immun. 2004;72:6313–7. doi: 10.1128/IAI.72.11.6313-6317.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Mazmanian SK, Liu G, Ton-That H, Schneewind O. Staphylococcus aureus sortase, an enzyme that anchors surface proteins to the cell wall. Science. 1999;285:760–3. doi: 10.1126/science.285.5428.760. [DOI] [PubMed] [Google Scholar]
- [38].Ivins BE, Fellows P, Pitt L, Estep J, Farchaus J, Friedlander AM, et al. Experimental anthrax vaccines: efficacy of adjuvants combined with protective antigen against an aerosol Bacillus anthracis spore challenge in guinea pigs. Vaccine. 1995;18:1779–84. doi: 10.1016/0264-410x(95)00139-r. [DOI] [PubMed] [Google Scholar]
- [39].Grabenstein JD. Vaccines: countering anthrax: vaccines and immunoglobulins. Clin Infect Dis. 2008;46:129–36. doi: 10.1086/523578. [DOI] [PubMed] [Google Scholar]
- [40].Singer DE, Schneerson R, Bautista CT, Rubertone MV, Robbins JB, Taylor DN. Serum IgG antibody response to the protective antigen (PA) of Bacillus anthracis induced by anthrax vaccine adsorbed (AVA) among U.S. military personnel. Vaccine. 2008;26:869–73. doi: 10.1016/j.vaccine.2007.11.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Kern JW, Schneewind O. BslA, a pXO1-encoded adhesin of Bacillus anthracis. Mol Microbiol. 2008;68:504–15. doi: 10.1111/j.1365-2958.2008.06169.x. [DOI] [PubMed] [Google Scholar]
- [42].Chand HS, Drysdale M, Lovchik J, Koehler TM, Lipscomb MF, Lyons CR. Discriminating virulence mechanisms among Bacillus anthracis strains by using a murine subcutaneous infection model. Infect Immun. 2009;77:429–35. doi: 10.1128/IAI.00647-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Marraffini LA, DeDent AC, Schneewind O. Sortases and the art of anchoring proteins to the envelopes of gram-positive bacteria. Microbiol Mol Biol Rev. 2006;70:192–221. doi: 10.1128/MMBR.70.1.192-221.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Schneewind O, Fowler A, Faull KF. Structure of the cell wall anchor of surface proteins in Staphylococcus aureus. Science. 1995;268:103–6. doi: 10.1126/science.7701329. [DOI] [PubMed] [Google Scholar]
- [45].Bentley ML, Lamb EC, McCafferty DG. Mutagenesis studies of substrate recognition and catalysis in the sortase A transpeptidase from Staphylococcus aureus. J Biol Chem. 2008;283:14762–71. doi: 10.1074/jbc.M800974200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Dumetz F, Jouvoin G, Khun H, Glomski IJ, Corre JP, Rougeaux C, et al. Noninvasive imaging technologies reveal edema toxin as a key virulence factor in anthrax. Am J Pathol. 2011;178:2523–35. doi: 10.1016/j.ajpath.2011.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Drysdale M, Heninger S, Hutt J, Chen Y, Lyons CR, Koehler TM. Capsule synthesis by Bacillus anthracis is required for dissemination in murine inhalation anthrax. EMBO J. 2005;24:221–7. doi: 10.1038/sj.emboj.7600495. [DOI] [PMC free article] [PubMed] [Google Scholar]