Abstract
Introduction
Despite the high level of individual and societal burden resulting from headache disorders, the National Institutes of Health (NIH) has funded relatively little research on these disorders.
Objective
The objective of this study was to define current patterns of NIH funding of research on headache disorders.
Methods
The Computer Retrieval of Information on Scientific Projects (CRISP) database was searched using the terms “migraine” or “headache” or “trigeminovascular” and inclusive of the dates 1987 to November 2007. Titles and abstracts of the resulting projects were reviewed to identify headache research projects and to extract data. E-mails were sent to each of the principal investigators to identify investigators experienced in serving on NIH study sections. E-mails and membership directories were used to determine if principal investigators were members of the American Headache Society. Comparisons were made for levels of NIH funding for migraine, headache disorders, and ten other medical disorders relative to three measures of disease burden.
Results
111 headache research projects led by 93 different investigators were identified. Research project grants (R’s) accounted for 61 (55%) of the grants. Migraine was the most common headache type studied, being the focus in 77 (69.4%) of the projects. The National Institute of Neurological Disorders and Stroke (NINDS) was responsible for funding 66 (59.5%) of the projects. At least 30 (32.3%) of the principal investigators were American Headache Society members and 14 (15%) had served on NIH study sections.
Conclusions
A small number of research grants on headache disorders were funded by the NIH over the last two decades. By comparison to NIH funding of research on ten chronic medical conditions relative to disease burden, headache research funding should exceed $103 million annually.
Keywords: Funding, headache disorders, National Institute of Health
Introduction
Headache disorders result in an enormous burden on individuals and societies due to their high prevalence, significant disability, and considerable direct and indirect economic costs. Annual prevalence of any active headache disorder comprises approximately 47% of adults, including 12% with migraine and 4% with chronic daily headache 1. Migraine headaches alone result in more than 1% of the total U.S. disability burden 2. At least 50% of migraine sufferers are severely disabled, many requiring bed rest, during individual migraine attacks lasting hours to days 3. A conservative estimate of total U.S. annual economic costs from headache disorders is $31 billion 4-5.
Despite the significant burden that headache disorders place on individuals and society, federal funding of headache research is minimal. The National Institutes of Health (NIH) is estimated to expend approximately $13 million annually on headache research 2. This accounts for less than 0.05% of the total NIH budget. Headache research is not considered in the NIH estimates of disease-specific grant expenditures or economic costs of illness. There are relatively few request for applications (RFAs) and program announcements (PA’s) related to headache research. There is no NIH institute, center, or standing study section focusing on pain, let alone one focusing specifically on headache disorders. Furthermore, no intramural headache research program exists at the National Institute for Neurological Disorders and Stroke (NINDS).
The aim of this study is to better define the current patterns of NIH funding of research on headache disorders.
Methods
The Computer Retrieval of Information on Scientific Projects (CRISP) database was employed 7. CRISP is a searchable database of federally funded biomedical research projects which is maintained by the NIH. It includes projects funded between 1972 and the present time. Although the majority of projects are funded by the NIH, the database also includes projects funded by other federal institutes including: Substance Abuse and Mental Health Services (SAMHSA), Health Resources and Services Administration (HRSA), Food and Drug Administration (FDA), Centers for Disease Control and Prevention (CDCP), Agency for Health Care Research and Quality (AHRQ), and the Office of Assistant Secretary of Health (OASH).
The CRISP database was searched using the terms “Migraine” or “Headache” or “Trigeminovascular” inclusive of 1987 to November 2007. The titles and abstracts of the resulting projects were reviewed to identify headache related studies. Once these projects were identified, the following information was collected: title of project, principal investigator (PI), study site, grant mechanism, funding institute or center, headache type being studied, duration of funding, research focus (pathophysiology, treatment, diagnosis, novel therapeutics), subject type (human, animal), and peer-review study section. E-mail questionnaires were sent to each of the PIs in order to determine whether they had ever been or currently were a member of the American Headache Society, and whether they have ever served on an NIH study section. The e-mail was sent a second time to all PIs who did not respond to the first email. American Headache Society membership was also determined by reviewing membership directories from the last 5 years.
NIH funding of headache research was compared to the funding of ten other chronic disorders including epilepsy, asthma, diabetes, ovarian cancer, stroke, arthritis, multiple sclerosis (MS), Parkinson’s disease, hepatitis C, and schizophrenia. These ten disorders were among 32 potential comparator disorders or disease categories that were listed on both the “NIH Estimates of Funding for Various Diseases, Conditions, Research Areas” 10 and the World Health Organization estimates of annual United States Disability Adjusted Life Years (DALYs) 16. These ten disorders were selected because published estimates could also be readily obtained for both their population prevalences and their annual US economic costs. Comparisons were made for total 2007 NIH funding, funding per person with the disorder, funding per disability-adjusted life year (DALY), and funding per $1000 costs to society from the disorder. Further methods for determining this information are described in the caption of Table 1.
Table 1. NIH Funding and Disease Burden for Migraine, Headache Disorders and Other Chronic Disorders.
NIH has reported fiscal year 2007 funding for all disorders listed in table except migraine and headache disorders 10. NIH research funding for headache disorders in FY2007 is an estimate of the mean annual migraine funding across FY2003 to FY2006 which has been previously published 2. Annual US economic costs attributable to all headache disorders were derived by adding the indirect costs of all headache disorders ($20 billion) 4 to the direct costs for migraine excluding over-the-counter medication costs ($11 billion) 5 . This is an underestimate of true costs since neither direct costs for non-migraine headache disorders (e.g. chronic daily headache) nor the costs for over-the-counter medications for all headache disorders (which may total $1 billion 6) are included in this total. All other data were derived from sources as cited.
| FY 2007 NIH Funding (US$ millions) |
U.S. population prevalence (millions of patients) |
U.S. annual DALYs attributable to disorder (thousands of DALYs)16 |
U.S. annual economic costs attributable to disorder (US$ billions) |
|
|---|---|---|---|---|
| Migraine | 13 2 | 36 1 | 446 | - |
| Headache Disorders | - | 141 1 | - | 31 4-5 |
| Epilepsy | 105 10 | 3 11 | 142 | 12.5 11 |
| Asthma | 294 10 | 24 14 | 690 | 16 12 |
| Diabetes | 1037 10 | 21 15 | 1280 | 174 13 |
| Ovarian Cancer | 103 10 | 0.17517 | 138 | 318 |
| Stroke | 340 10 | 719 | 1467 | 62.719 |
| Arthritis | 339 10 | 4720 | 1028 | 8621 |
| MS | 98 10 | 0.3522 | 105 | 6.823 |
| Parkinson’s | 186 10 | 0.524 | 226 | 624 |
| Hepatitis C | 108 10 | 5.525 | 76 | 10826 |
| Schizophrenia | 358 10 | 327 | 462 | 62.728 |
To obtain the amounts of NIH awards for grants identified in CRISP searches, the Tracking Accountability in Government Grants System (TAGGS) database (http://taggs.hhs.gov/) was searched. All grants identified by CRISP search for key words “migraine”, “headache”, or “trigeminovascular” were identified as likely awarded in FY2007 and with clear relevance for headache disorders research. TAGGS searches identified awards amounts for these grants.
Results
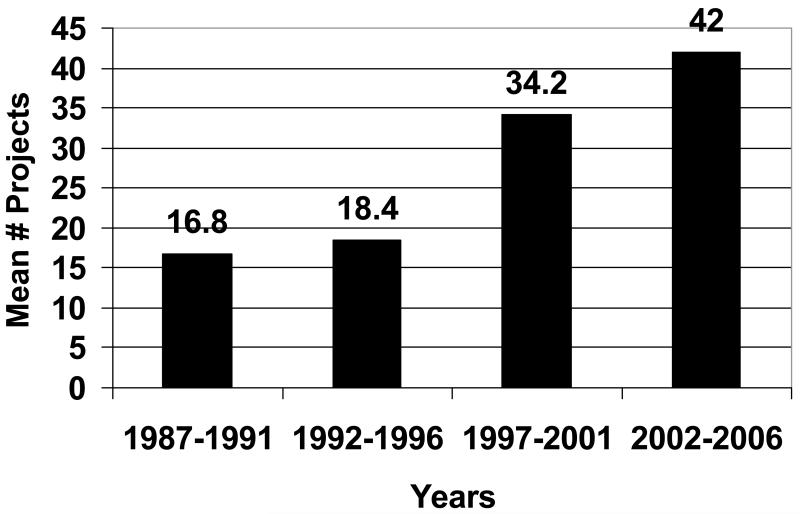
The CRISP search identified 111 different headache research projects funded between 1987 and 2007. These projects accounted for a total of 493 funded headache research years. Ninety-three different PIs were responsible for the 111 projects. The mean duration of funding per project was 5.3 years with a mode of 5 years. Presenting the data in 5 year blocks, the mean number of grants per year increased from 16.8 during 1987-1991 to 42.0 during 2002-2006. [Figure 1]
Figure 1. Annual Mean Number of NIH Funded Headache Research Projects.
Although there has been an increase in the number of projects funded annually from 1987 until 2006, the total number of funded projects remains low.
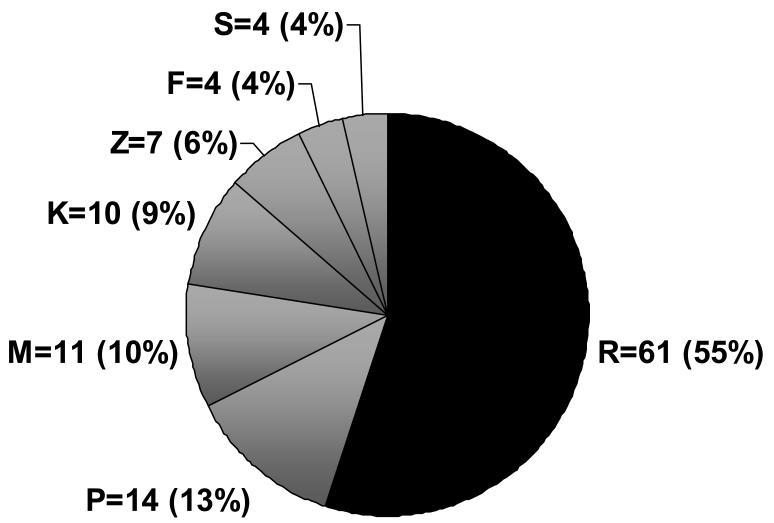
Research project grants (R’s) were the most frequent, accounting for 61 (55%) of the grants. There were 14 (12.6%) program projects and centers grants (P), 11 (9.9%) general clinical research center projects (M), 10 (9%) career development awards (K), 7 (6.3%) intramural research projects (Z), 4 (3.6%) fellowship program awards (F), and 4 (3.6%) research related programs (S). [Figure 2]
Figure 2. Grant Mechanisms.
R = Research Project Grant; P = Program Projects and Centers; M = General Clinical Research Centers; K = Career Development Award; Z = Intramural Research; F = Fellowship Programs; S = Research Related Programs. Numbers and percentages (in parentheses) indicate the total grants of each type funded between 1987 and 2007.
Migraine was studied in 77 (69.4%) of the projects, headache “not otherwise specified” (NOS) in 23 (20.7%), tension-type headache in 4 (3.6%), cluster headache in 2 (1.8%), and other headache types in 5 (4.5%) (1 project each for medication-overuse headache, idiopathic intracranial hypertension, giant cell arteritis, cerebrospinal fluid leak headache, and Chiari malformation headache). Human subjects were studied in 64 (64%) projects, animals in 39 (39%) projects, and 3 projects studied both human subjects and animals. This information was unavailable for 11 studies. Children were included in 6 (5.4%) projects. Pathophysiology of headache was studied in 54 (48.6%) projects, treatment in 37 (33.3%), diagnosis in 19 (17.7%) and novel therapeutics in 9 (8.1%).
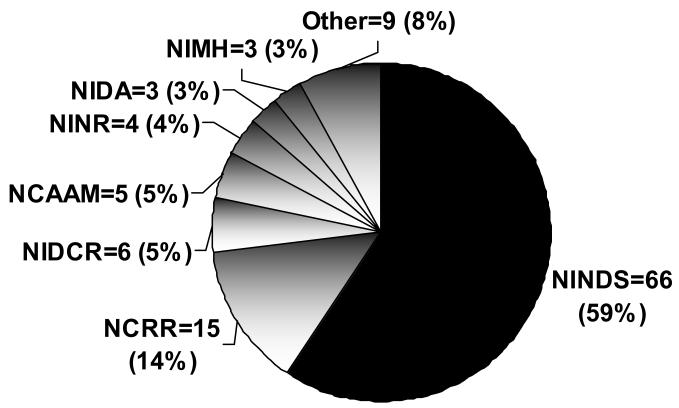
NINDS funded 66 (59.5%) of the identified projects. The NINDS funding proportion has increased slightly since 2002 (mean 64.2% ± 3.5%). The National Center for Research Resources (NCRR) funded 15 (13.5%) projects, the National Institute of Dental and Craniofacial Research (NIDCR) funded 6 (5.4%), and the National Center for Complementary and Alternative Medicine funded 5 (4.5%). Ten other institutes or centers were each responsible for the funding of 4 or fewer projects. [Figure 3] Study sections providing peer-review of grant applications (n=86 projects) included special emphasis panels (44.2%), neurological sciences (10.5%), behavioral medicine (10.5%), somatosensory and chemosensory systems (8.1%), training grant and career development (7.0%), molecular neuropharmacology and signaling (2.3%), and nursing (2.3%).
Figure 3. NIH Funding of Headache Research by Institute and Center.
NINDS = National Institute of Neurological Disorders and Stroke; NCRR = National Center for Research Resources; NIDCR = National Institute of Dental and Craniofacial Research; NCAAM = National Center for Complementary and Alternative Medicine; NINR = National Institute of Nursing Research; NIDA = National Institute on Drug Abuse; NIMH = National Institute of Mental Health. Numbers and percentages (in parentheses) indicate the total grants funded between 1987 and 2007 by each Institute and Center.
The majority of PI’s (n = 72, 77.4%) worked at academic institutions, with an equal split (n=7, 7.5% each) among investigators working at the NIH, at non-academic private institutions, or for industry. E-mail responses were received from 33 (35%) of the PIs. From these responses, as well as from American Headache Society membership directories for the last 5 years, it was determined that at least 28 (30.1%) were currently and at least 30 (32.3%) were at some time members of the American Headache Society. E-mail responses from 14 PIs stated that they had served on a NIH study section at some time.
TAGGS search of grants identified by CRISP search as research relevant to headache disorders awarded in FY 2007 totaled $6,832,948. Two grants identified in CRISP documentation as likely awarded in FY 2007 could not be identified in the TAGGS database. Therefore, $6,832,948 should be regarded as a minimum estimate of the total NIH funding for headache disorders in FY 2007.
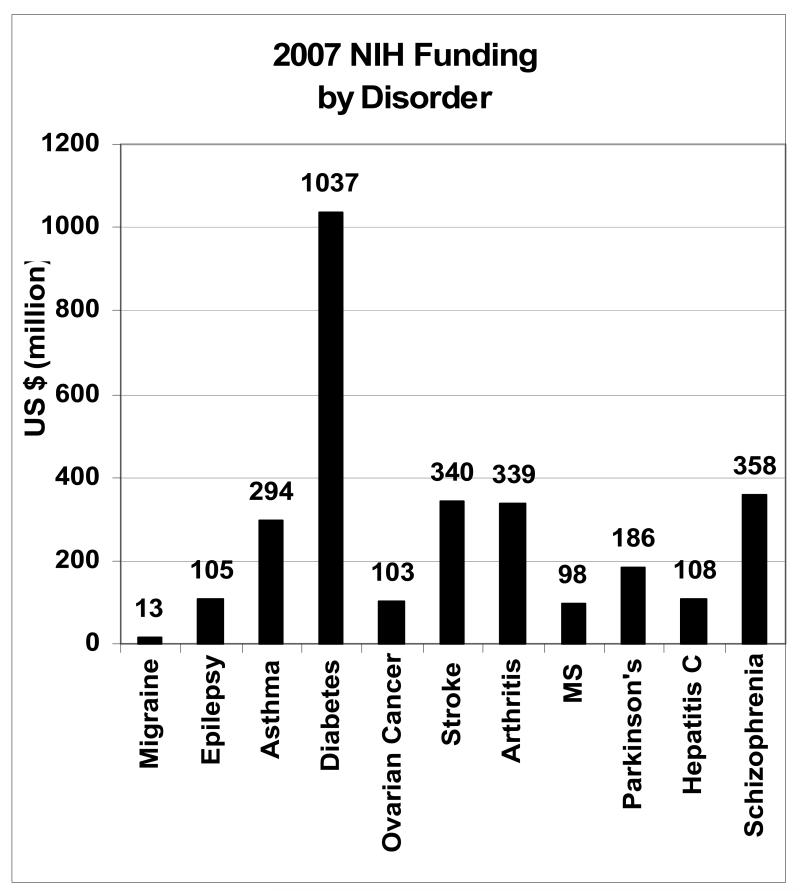
2007 NIH funding for the ten comparator disorders ranged from $98 million to $1.04 billion with a mean funding level of $296.8 million. By comparison, migraine funding is estimated at $13 million for 2007 2. [Table 1; Figure 4]
Figure 4. Total NIH Funding of Headache vs. Other Chronic Disorders.
Total 2007 NIH funding of headache disorders is estimated at $13 million. Total funding for the comparator disorders ranged from $98 million to $1.04 billion. The mean funding for these 10 disorders in 2007 was $296.8 million.
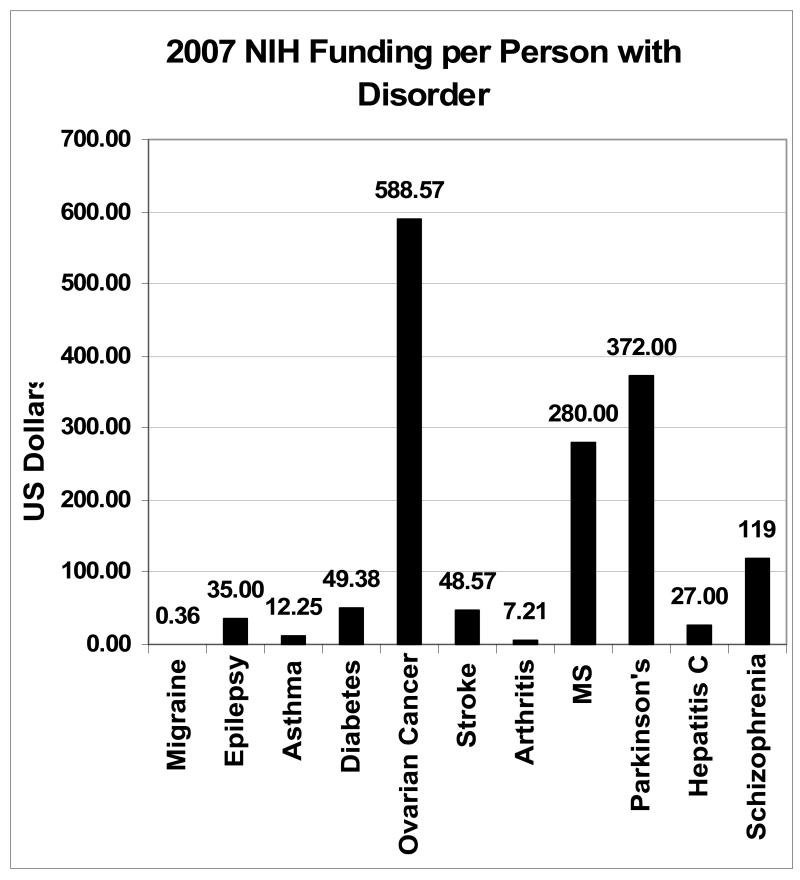
2007 NIH funding per person with the disorder was calculated for migraine and the ten comparator disorders. Funding for the comparator disorders ranged from $7.21 to $588.57 per person with the disorder. [Figure 5] Equivalent annual funding for migraine would range from $259.6 million ($7.21 × 36 million migraineurs) to $21.2 billion ($588.57 × 36 million migraineurs). The mean annual funding level per affected person among the ten comparator disorders was $153.90, with equivalent annual funding for migraine equal to $5.54 billion ($153.90 × 36 million migraineurs).
Figure 5. NIH Funding per Person with Headache vs. Other Chronic Disorders.
NIH funded migraine research received an estimated $0.36 per person with migraine in 2007. NIH funding per person for the comparator disorders ranged from $7.21 to $588.57, with a mean of $153.90. Equivalent headache funding would range from $259.6 million to $21.2 billion. Headache funding equivalent to the mean funding of the 10 comparator disorders ($153.90) would be $5.54 billion annually.
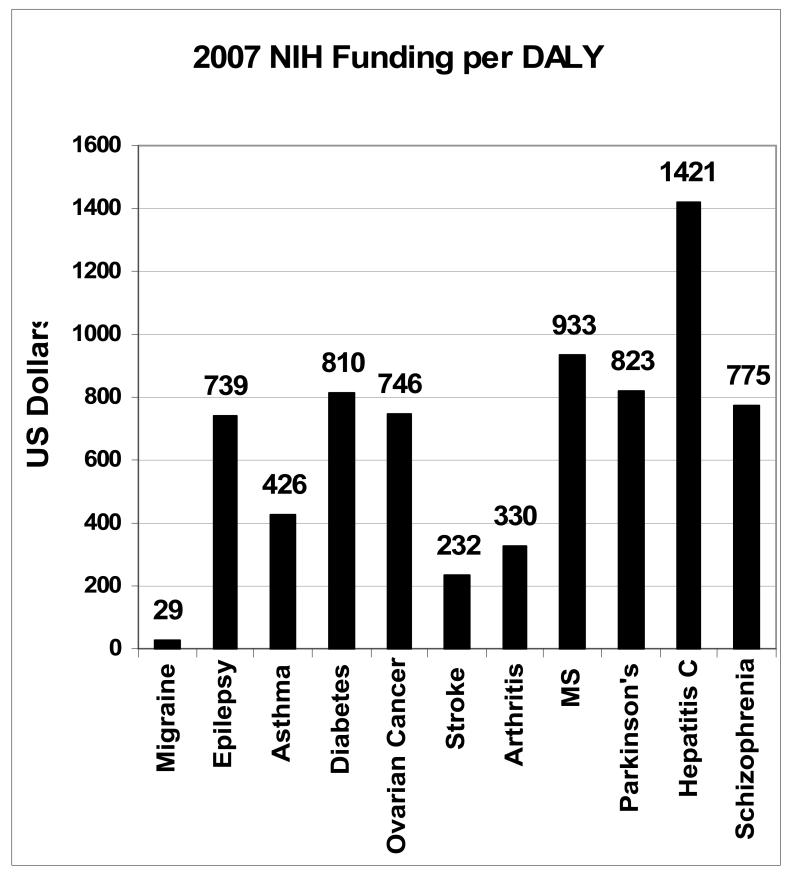
Annual NIH funding of migraine in 2007 per DALY is estimated at $29. Funding per DALY for the ten comparator disorders ranged from $232 to $1421 with a mean of $723.50. Equivalent migraine funding would range from $103.5 million ($232 × 446,000 DALYs) to $633.8 million ($1421 × 446,000 DALYs). Adjusting to the mean funding per DALY for the comparator disorders, migraine would receive $322.7 million annually ($723.50 × 446,000 DALYs). [Figure 6]
Figure 6. NIH Funding per Disability Adjusted Life-Year (DALY) for Headache vs. Other Chronic Disorders.
NIH funded migraine research received an estimated $29 per DALY attributed to migraine in the US in 2007. Annual NIH funding per DALY for the 10 comparator disorders ranges from $232 to $1421, with a mean of $723.50. Equivalent annual headache funding would range from $103.5 million to $633.8 million. Annual headache funding equivalent to the mean of the comparator disorders equals $322.7 million.
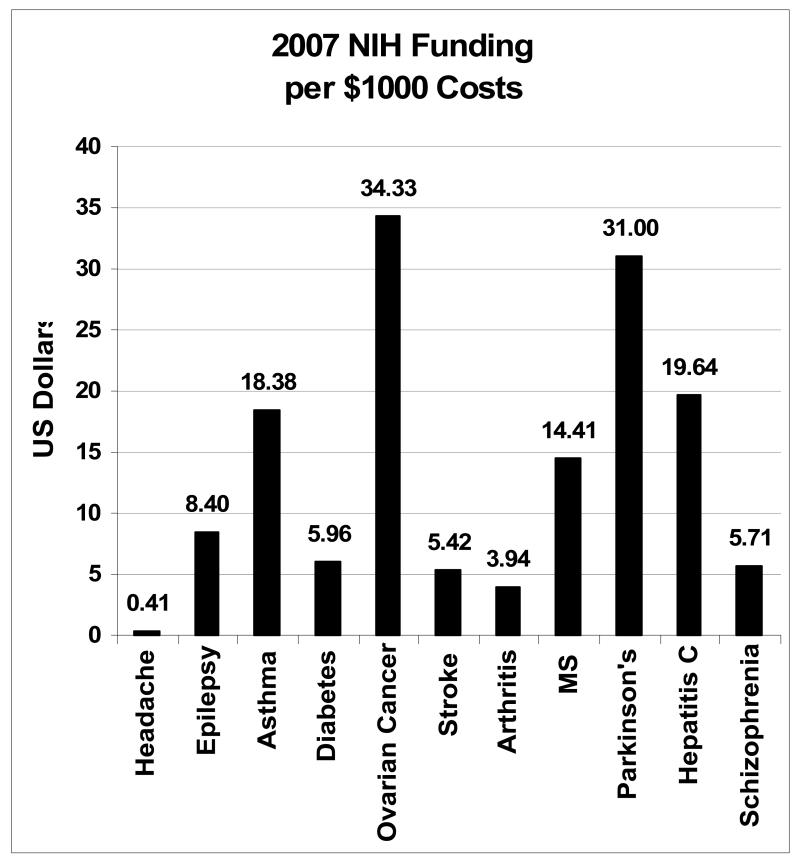
Research on headache disorders received approximately $0.41 of NIH funding per $1000 U.S. direct and indirect economic costs attributable to headache disorders in 2007. Funding for the ten comparator diseases ranged from $3.94 to $34.33 per $1000 U.S. costs, with a mean of $14.72. Equivalent annual headache funding would range from $126 million (($3.94 × $32 billion) / $1000) to $1.1 billion (($34.33 × $32 billion)/ $1000). Adjusting headache funding to the mean funding level of the comparator disorders suggests that headache would receive $471 million (($14.72 × $32 billion)/ $1000) annually. [Figure 7]
Figure 7. NIH Funding per Economic Costs from Headache vs. Other Chronic Disorders.
NIH funded headache disorders research received an estimated $0.41 per $1000 costs due to headache disorders in 2007. Annual NIH funding per $1000 costs from the ten comparator disorders ranges from $3.94 to $34.33, with a mean of $14.72. Equivalent annual headache funding would range from $126 million to $1.1 billion. Annual headache funding equivalent to the mean of the comparator disorders would be $471 million.
Discussion
Headache disorders are highly prevalent and result in significant individual and societal burden. However, governmental funding of headache research is minimal in the United States and Europe 8-9.
The NIH has not disclosed an estimate of the total funding allocations for migraine or headache disorders. We previously reported a rough estimate of recent annual NIH funding for headache research as approximately $13 million dollars 2. This estimate was obtained by identifying the mean annual number of CRISP documents obtained for the keyword “migraine” over the period FY 2003 – FY2006 and multiplying this number by the estimated mean funding per document calculated over that same time period for other disorders. The $13 million figure assumes that all “migraine” documents are truly relevant to headache research and that the estimated mean funding per “migraine” document is similar for other disorders. Inspection of the documents retrieved for “migraine” indicate that a sizeable number are in fact marginally related to headache research, and we have no data on the average dollar amounts of grants for migraine research compared to other disorders. Use of the $13 million figure as indicative of funding for all headache research also assumes that NIH funds very little non-migraine headache research. Our data indicate that approximately 69% of NIH headache research grants studied migraine, and an additional 21% of these grants did not specify the headache type studied, many of which could have been migraine-related as well 29.
The $13 million total headache funding figure is likely an overestimation of total NIH funding for headache research. Our TAGGS database analysis indicates a minimum level of FY 2007 NIH funding of headache research of $6,832,948. This number is likely an underestimation of the total funding since (1) the funding amounts for some grants identified by CRISP search could not be found in the TAGGS database, and (2) we excluded from our overall analysis some grants that included any of the keywords “migraine”, “headache” or “trigeminovascular”, but were judged to be marginally related to headache research on close reading of the grant abstracts. The NINDS estimates their FY 2007 funding for all headache research to have been $6.206 million (personal communication, Dr. Linda Porter, NINDS). Since our analysis indicates that NINDS accounts for approximately 64% of all NIH headache research grants, $9.7 million may be a closer estimate of the total NIH FY 2007 research funding for headache disorders.
For the purposes of our comparative analyses, we used the estimate of $13 million since we believed this would avoid overstating the relative degree of underfunding of headache research. $13 million in research funding represents approximately $0.36 per person with migraine, $29 per DALY attributable to migraine, and $0.41 per $1000 of economic costs from all headache disorders. This level of NIH research funding pales in comparison to funding for ten other chronic diseases, both in terms of total dollars allocated, as well as in proportion to the annual attributable disease burden assessed by population prevalence, economic costs and death and disability (DALYs).
A conservative estimate of equitable reseach funding relative to disease burden can be obtained by comparing the funding levels for the lowest of the ten comparator disorders after adjusting for each measure of disease burden. For example, arthritis received the lowest amount of NIH funding per person among the comparator disorders ($7.21). If migraine research received $7.21 per migraineur, then it would receive $259.6 million in NIH funding annually. Accordingly, minimum estimates of parity for annual migraine research funding would range from $103.5 million (i.e. comparable to $232 per DALY attributable to stroke) to $259.6 million (i.e. comparable to $7.21 per affected person with arthritis).
Investigator-initiated research is the core activity supported by NIH; the peer-review system is intended to ensure that only the most promising of these projects receive funding. However, the NIH is also structured to encourage research into particular areas where it is most needed. Priorities for funding are expressed by NIH through programmatic vehicles such as RFAs and PAs, or by establishment of Branches, Institutes, or Centers. Important factors taken into consideration when prioritizing NIH research programs include the need to counter emerging public health threats and the desire to capitalize on unique opportunities such as the development of novel research techniques or breakthroughs which can accelerate the advancement of particular fields.
Relative burden of disease is another important consideration in prioritizing research. We calculated NIH funded headache research relative to three commonly recognized measures of disease burden: population prevalence, disability adjusted life years (DALYs), and economic costs. By each of these measures, headache research is grossly underfunded relative to other chronic disorders. While the DALY metric takes into account “lost years” due to disability, some have argued that the most meaningful measure of disease burden is mortality and that headache disorders are not fatal illnesses. In fact, migraine with aura is a significant risk factor for suicide attempts 30 and may also account for more than 1400 excess cardiovascular deaths in the US annually 31.
Burden of illness is a central concern of the NINDS; the stated primary mission of the institute is to “…reduce the burden of neurological disease…” 32. In light of this mission, the inattention to headache research by NINDS is particularly striking.
Conclusions
Search of the CRISP database indicates that 111 headache research projects from 93 different PIs were funded by the NIH during 1987 to 2007. The majority (55%) of projects is comprised of research project grants (R’s) and at least 69% of grants were related to migraine. NINDS funded a mean of 64% of all NIH research grants on headache disorders since 2002. A comparison of headache disorders to ten other chronic diseases, relative to three measures of disease burden, suggests that current NIH funding of headache research should exceed $103 million annually.
Footnotes
Conflict of Interest:
Dr Schwedt: Research Funding: National Institutes of Health, National Headache Foundation. Consulting: VerusMed. Participation in Industry-Sponsored Research: Allergan, GSK, AGA Medical
Dr Shapiro (since 1/1/07): Research Funding: National Institutes of Health. Scientific Advisory Boards: NuPathe, MAP Pharma, Merck. Participation in Industry-Sponsored Research: Merck
References
- 1.Jensen R, Stovner LJ. Epidemiology and comorbidity of headache. Lancet Neurol. 2008;7:354–361. doi: 10.1016/S1474-4422(08)70062-0. [DOI] [PubMed] [Google Scholar]
- 2.Shapiro RE, Goadsby PJ. The long drought: the dearth of public funding for headache research. Cephalalgia. 2007;27:991–994. doi: 10.1111/j.1468-2982.2007.01396.x. [DOI] [PubMed] [Google Scholar]
- 3.Lipton RB, Stewart WF, Diamond S, Diamond ML, Reed M. Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache. 2001;41:646–657. doi: 10.1046/j.1526-4610.2001.041007646.x. [DOI] [PubMed] [Google Scholar]
- 4.Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R. Lost productive time and cost due to common pain in the US workforce. JAMA. 2003;290:2443–2454. doi: 10.1001/jama.290.18.2443. [DOI] [PubMed] [Google Scholar]
- 5.Hawkins K, Wang S, Rupnow M. Direct cost burden among insured US employees with migraine. Headache. 2008;48:553–563. doi: 10.1111/j.1526-4610.2007.00990.x. [DOI] [PubMed] [Google Scholar]
- 6.Lipton RB. Personal communication. Estimated U.S.annual cost of non-prescription medications for headache. [Google Scholar]
- 7.Computer Retrieval of Information on Scientific Projects Available at: http://crisp.cit.nih.gov/
- 8.Olesen J, Lekander I, Andlin-Sobocki P, Jonsson B. Funding of headache research in Europe. Cephalalgia. 2007;27:995–999. doi: 10.1111/j.1468-2982.2007.01397.x. [DOI] [PubMed] [Google Scholar]
- 9.Shapiro RE. NIH funding for research on headache disorders: does it matter? Headache. 2007;47:993–995. doi: 10.1111/j.1526-4610.2007.00875.x. [DOI] [PubMed] [Google Scholar]
- 10.NIH Estimates of Funding for Various Diseases, Conditions, Research Areas. Available at: http://www.nih.gov/news/fundingresearchareas.htm.
- 11.Epilepsy Foundation Epilepsy and Seizure Statistics. Available at: http://www.epilepsyfoundation.org/about/statistics.cfm.
- 12.National Heart, Lung and Blood Institute Chartbook, U.S. Department of Health and Human Services. National Institutes of Health; 2004. [Google Scholar]
- 13.American Diabetes Association Direct and Indirect Costs of Diabetes in the United States. Available at: http://www.diabetes.org/diabetes-statistics/cost-of-diabetes-in-us.jsp.
- 14.Centers for Disease Control and Prevention Asthma episodes and current asthma. Available at: http://www.cdc.gov/nchs/data/nhis/earlyrelease/200709_15.pdf.
- 15.American Diabetes Association Total prevalence of diabetes and pre-diabetes. Available at: http://www.diabetes.org/diabetes-statistics/prevalence.jsp.
- 16.World Health Organization Estimated total DALYs (’000), by cause and WHO member state. 2002 Available at: http://www.who.int/healthinfo/statistics/bodgbddeathdalyestimates.xls.
- 17.American Society of Clinical Oncology Cancer.Net. Available at: http://www.ascocancerfoundation.org/
- 18.Chang S, Long SR, Kutikova L, Bowman L, Finley D, Crown WH, Bennett CL. Estimating the cost of cancer: results on the basis of claims data analyses for cancer patients diagnosed with seven types of cancer during 1999 to 2000. Journal of Clinical Oncology. 2004;22:3524–3530. doi: 10.1200/JCO.2004.10.170. [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control Prevalence of Stroke – United States, 2005. Morbidity and Mortality Weekly Report. 2007;56:469–474. Available at: http://www.cdc.gov/MMWR/preview/mmwrhtml/mm5619a2.htm. [PubMed] [Google Scholar]
- 20.National Center for Chronic Disease Prevention and Health Promotion Arthritis Data and Statistics. Available at: http://www.cdc.gov/arthritis/data_statistics/index.htm.
- 21.Centers for Disease Control Update: direct and indirect costs of arthritis and other rheumatic conditions – United States, 1997. JAMA. 2004;291:2935–2936. [Google Scholar]
- 22.Frohman EM. Med Clin N Amer. 2003;87:887–97. doi: 10.1016/s0025-7125(03)00008-7. [DOI] [PubMed] [Google Scholar]
- 23.Whetten-Goldstein K, Sloan FA, Goldstein LB, Kulas ED. A comprehensive assessment of the cost of multiple sclerosis in the United States. Mult Scler. 1998;4:419–425. doi: 10.1177/135245859800400504. [DOI] [PubMed] [Google Scholar]
- 24.Parkinson’s prevalence and cost – NINDS. Parkinson’s Disease: Hope Through Research. Available at: http://www.ninds.nih.gov/disorders/parkisnons_disease/detail_parkinsons_disease.htm.
- 25.National Institute of Allergy and Infectious Diseases Overview of Hepatitis C. Available at: http://www3.niaid.nih.gov/healthscience/healthtopics/HepatitisC/overview.htm.
- 26.C. Leigh JP, Bowlus CL, Leistikow BN, Schenker M. Cost of hepatitis C. Arch Int Med. 2001;161:2231–2237. doi: 10.1001/archinte.161.18.2231. [DOI] [PubMed] [Google Scholar]
- 27.American Psychiatric Association Let’s Talk Facts About Schizophrenia. Available at: http://healthyminds.org/factsheets/LTF-Schizophrenia.pdf.
- 28.Wu EQ, Birnbaum HG, Shi L, Ball DE, Kessler RC, Moulis M, Aggarwal J. The economic burden of schizophrenia in the United States in 2002. J Clin Psychiatry. 2005;66:1122–1129. doi: 10.4088/jcp.v66n0906. [DOI] [PubMed] [Google Scholar]
- 29.Hasse LA, Ritchey PN, Smith R. Quantifying headache symptoms and other headache features from chart notes. Headache. 2004;44:873–84. doi: 10.1111/j.1526-4610.2004.04169.x. [DOI] [PubMed] [Google Scholar]
- 30.Breslau N. Migraine, suicidal ideation, and suicide attempts. Neurology. 1992;42:392–5. doi: 10.1212/wnl.42.2.392. [DOI] [PubMed] [Google Scholar]
- 31.Kurth T, Gaziano JM, Cook NR, Logroscino G, Diener HC, Buring JE. Migraine and risk of cardiovascular disease in women. JAMA. 2006;296:283–91. doi: 10.1001/jama.296.3.283. [DOI] [PubMed] [Google Scholar]
- 32.NINDS website. Available at: http://www.ninds.nih.gov/about_ninds/mission.htm.