Abstract
Given the preferential tax treatment afforded nonprofit firms, policymakers and researchers have been interested in whether the nonprofit sector provides higher nursing home quality relative to its for-profit counterpart. However, differential selection into for-profits and nonprofits can lead to biased estimates of the effect of ownership form. By using “differential distance” to the nearest nonprofit nursing home relative to the nearest for-profit nursing home, we mimic randomization of residents into more or less “exposure” to nonprofit homes when estimating the effects of ownership on quality of care. Using national Minimum Data Set assessments linked with Medicare claims, we use a national cohort of post-acute patients who were newly admitted to nursing homes within an 18-month period spanning January 1, 2004 and June 30, 2005. After instrumenting for ownership status, we found that post-acute patients in nonprofit facilities had fewer 30-day hospitalizations and greater improvement in mobility, pain, and functioning.
Keywords: Ownership, nursing homes, quality, post-acute care
1. Introduction
Two defining features of the nursing home market are the predominance of for-profit facilities and the perception of low quality care in many facilities. The nursing home sector is roughly two-thirds for-profit, while the hospital sector, by comparison, is approximately two-thirds non-profit. Quality of care has been a longstanding concern in the nursing home sector with policymakers, researchers, media and the public all identifying low quality care (Institute of Medicine 1986; U.S. Government Accounting Office 1998). Policymakers and researchers alike have been interested in linking these two ideas by suggesting a causal relationship between ownership status and quality of care.
A large literature examines this issue, but a potential problem with these earlier studies is that unobserved characteristics may be correlated with both an individual’s ownership choice and the quality of their nursing home care. For example, an individual in poorer health may be more likely to choose a nonprofit nursing home and also may have worse outcomes. If so, simple comparisons of quality in for-profits and nonprofits, controlling for observable characteristics, may yield misleading estimates. Moreover, few studies examining ownership and quality have focused on the short-stay (post-acute) nursing home population.
When randomization is not feasible, as in this case, instrumental variables estimation can be used to account for unobserved differences across study populations if a series of assumptions are met. One “instrument” that has been frequently and successfully used in health care is the differential distance from the patient’s home to different providers. By using “differential distance” to the nearest nonprofit nursing home relative to the nearest for-profit nursing home (and assuming that this distance is uncorrelated to unobserved quality), we mimic randomization of residents into more or less “exposure” to nonprofit homes when estimating the effects of ownership on quality of care for the post-acute nursing home population.
Using national Minimum Data Set assessments linked with Medicare claims, we use a national cohort of short-stay residents who were newly admitted to nursing homes within an 18-month period spanning January 1, 2004 and June 30, 2005. Because of the concern that unobservables such as patient health will be correlated with the admission to a nonprofit and the quality of care, we use instrumental variables analysis to examine the effect of ownership on risk-adjusted, person-level short-stay measures of quality. After instrumenting for ownership status, we found that post-acute quality of care was generally poorer in for-profit facilities. Specifically, post-acute patients in nonprofit facilities were less likely to be hospitalized within 30 days and more likely to experience improvement in mobility, pain status, and activities of daily living (ADL) functioning. Importantly, the instrumental variables models generate dramatically different results relative to the standard models that treat ownership as exogenous, with the direction of the bias consistent with the idea that individuals in worse health choose nonprofit nursing homes. As discussed below, this negative selection may relate to both demand and supply factors.
2. Background and Related Research
2.1 U.S. Nursing Home Sector
The most recent National Nursing Home Survey counted 1.5 million Americans living in approximately 16,100 nursing homes nationwide in 2004 (National Center for Health Statistics 2006). It has been projected that in the next twenty years, 46 percent of Americans who survive to age 65 will use a nursing home at some point in their lives (Spillman and Lubitz 2002). Nursing home expenditures totaled $137 billion in 2009, which represented 5.5 percent of national health expenditures (Martin, Lassman et al. 2011). The nursing home market consists of both chronic (long-stay) and post-acute (short-stay) residents. Medicaid is the dominant payer of long-stay nursing home services, accounting for roughly 50% of all nursing home expenditures and 70% of all bed days. Medicare covers post-acute nursing home care, which accounts for 12% of total nursing home expenditures. The remainder of care is financed primarily by private out-of-pocket payments.
For-profit nursing homes, constituting roughly two-thirds of all facilities, may be owned by an individual, partnership or corporation. Nonprofits make up approximately one-fourth of all facilities and are predominantly church-related or a nonprofit corporation. The remaining nursing homes (6%) are government-owned and may be run by the state, county, city, hospital district or federal government, any of which might contract for management services from proprietary firms.
2.2 Nursing Home Objectives
For-profit nursing homes are presumed to maximize profits by setting output, quality, inputs and patient mix at levels to achieve this objective. In most industries, profit-maximizing behavior, given a reasonable level of competition, would be expected to yield desirable outcomes, defined as the delivery of the array and quality of services most valued by consumers given the costs of efficient production. However, if nursing home residents (and prospective residents) cannot readily ascertain the level of quality provided by different nursing homes, the profit motive can lead to lower quality than would be chosen by a hypothetical, fully-informed resident. Unlike their for-profit counterparts, nonprofits cannot distribute accounting profits to individual equity holders. In return, nonprofits enjoy several government-conferred advantages, including exemption from corporate income and property taxes and a lower cost of capital through tax-exempt donations and bonds.
Medicare prices for short-stay nursing home care do not depend on quality of care, but Medicare recipients may still choose nursing homes on the basis of quality. Clearly, certain aspects of quality are observable to patients and their families, while other aspects are unobservable, even with public report cards and regulatory oversight (Zhang and Grabowski 2004; Werner, Konetzka et al. 2009). Aspects of post-acute nursing home quality that are unobservable to consumers include workforce quality (Cawley, Grabowski et al. 2006) and various process and outcome measures unreported on government report card websites such as locomotion, bladder incontinence, and infections (Werner, Konetzka et al. 2009). Given that nonprofit and government providers lack a defined shareholder, these firms may have less incentive to maximize profits and a greater incentive to maximize other objectives such as unobservable aspects of quality and the provision of public goods (Newhouse 1970; Hansmann 1980). Thus, we hypothesize that short-stay nursing home quality will be higher in nonprofit nursing homes.
2.3 Previous Literature
A large health economics literature has considered the role of ownership in health care, with studies focusing on the role of ownership in a number of health care sectors including hospitals (Sloan 2000), health plans (Town, Feldman et al. 2004), dialysis centers (Brooks, Irwin et al. 2006), and home health agencies (Grabowski, Huskamp et al. 2009). In particular, a literature review by Eggleston and colleagues (2008) identified 31 studies of hospital ownership and patient outcomes published over the period 1990 through 2004. The majority of studies included in this review found no statistically significant difference between nonprofit and for-profit hospitals in terms of mortality or other adverse events.
Nursing home ownership (for-profit vs. nonprofit) has also received particular attention in the literature. In a comprehensive review of 38 studies published over the period 1990 through 2002, Hillmer and colleagues (2005) concluded that quality was lower in for-profit nursing homes. Similarly, a systematic review and meta-analysis of 82 studies published over the period 1962 through 2003 by Comondore and colleagues (2009) suggested nonprofit nursing homes deliver higher quality care than do for-profit nursing homes. However, this previous literature is based entirely on cross-sectional comparisons of nonprofit and for-profit nursing homes that do not account for the possibility that there may be unobservable differences across residents receiving care at different types of facilities. As Konetzka (2009) wrote in an accompanying editorial to the Comondore et al. study, “no review or meta-analysis can overcome the empirical limitations common to all studies reviewed—we still do not know whether not-for-profit status is the reason for higher quality care” (p. 356). Further, the literature on ownership and quality has focused on the long-stay population or on the nursing home population as a whole, with relatively little work differentiating short-stayers (post-acute) and long-stayers. An advantage to studying the short-stay population is that Medicare pays for post-acute nursing home care, thus eliminating price differences for similar patients across ownership types within a common market.
Two previous studies have used alternate methods to examine the role of nursing home ownership. First, Grabowski and Stevenson (2008) exploited approximately 2,100 nursing home conversions that occurred between 1993 and 2004 to examine the effect of ownership on quality of care. Given that hospital conversions have been found to be preceded by financial difficulties (Sloan, Ostermann et al. 2003), the study examined nursing home quality in the periods preceding conversion and how it evolved in the periods following conversion. The results found little evidence to suggest a causal relationship between ownership conversions and nursing home performance. However, the study did find that facilities that have undergone conversion from nonprofit to for-profit status differ from those that did not undergo such a conversion. That is, facilities that converted from nonprofit to for-profit status were generally declining performers, while facilities that converted from for-profit to nonprofit status were generally improving performers. Second, Grabowski and Hirth (2003) considered whether competitive spillovers from nonprofits lead to higher quality in for-profit nursing homes. Using instrumental variables to account for the potential endogeneity of nonprofit market share, the study found that an increase in nonprofit market share improved for-profit and overall nursing home quality. These findings are consistent with the hypothesis that nonprofits serve as a quality signal for uninformed nursing home consumers.
Nursing home ownership remains of substantial policy interest. Ownership status (nonprofit, for-profit, government) is reported on the government’s Nursing Home Compare report card website. Moreover, Section 6101 of the Patient Protection and Affordable Care Act (PPACA) now requires Medicaid/Medicare certified nursing homes to have available for inspection detailed ownership and other disclosable party information. By March 2013, the U.S. Department of Health and Human Services will make detailed ownership information submitted by facilities available to the public. Finally, several states such as New York have enacted rules to oversee (and potentially limit) for-profit nursing home entry.
3. Data and Empirical Strategy
3.1 Data
The study primarily relies upon two types of individual level data: the Minimum Data Set (MDS) for nursing home resident assessment and Medicare Claims and Enrollment records. We also obtained a measure of Medicaid eligibility from the Medicaid Analytic Extract (MAX) data. At the nursing home level, the primary source of data was the Online Survey Certification and Reporting (OSCAR) system. We also included data at the zip-code level. Each of these sources is described briefly below.
The primary data source for this study is the MDS. The MDS resident assessment instrument has nearly 400 data elements, including cognitive function, communication/hearing problems, physical functioning, continence, psychosocial well-being, mood state, activity and recreation, disease diagnoses, health conditions, nutritional status, oral/dental status, skin conditions, special treatments, and medication use. Repeated evaluations of the reliability of the MDS provided at least adequate values on most scales (Morris, Hawes et al. 1990; Phillips, Morris et al. 1997; Mor, Angelelli et al. 2003; Mor, Intrator et al. 2011).
We merged the Medicare Standard Analytic File [inpatient and skilled nursing facility (SNF) files] and eligibility data from the Medicare enrollment record with MDS data using the Health Insurance Claim (HIC) number of Medicare beneficiaries. Match rates between MDS records of residents 65 and older exceed 95%. The Medicare enrollment file contains gender, date of birth, survival status, managed care participation, and Part A and B eligibility and “buy in” status. The record is updated at the end of the calendar year meaning that any change in managed care participation is identified. We also merged in Medicaid eligibility information from the MAX data.
The OSCAR database provides nursing-home level information on topics ranging from ownership and size to staffing and resident mix. The OSCAR data also include results from survey inspections and can be linked to the MDS data through the facility provider number available on the MDS—match rates are close to 100%. Completed on the day of the inspection, data include nursing home ownership, structure (e.g. size, number of beds) and staffing level information (by job category), observed deficiencies, and the availability of various services. A profile of residents in the nursing home on the day of the inspection is provided which includes information on number of residents (by payer category), functional deficits, nursing care needs, and receipt of “high tech” nursing care.
A key issue in the construction of our differential distance instrument (described in detail below) is the geo-coding of both nursing homes and nursing home resident’s prior zip code of residence. We geo-coded all certified nursing homes that currently operate in the U.S. Using this geo-referenced database, we calculated the distance from a particular nursing home to a particular resident’s prior residence as approximated by the centroid of the zip code area from which the resident was admitted.1
We obtained zip code level information from the Census 2000 aggregates and merged these data to individuals in our sample based on their prior zip of residence. Specifically, we included a measure of per capita income and a measure of the percent of elderly individuals living below the federal poverty level.
3.2 Estimation Sample
Using national MDS data, a cohort of 874,143 residents who were newly admitted to 13,980 unique nursing homes within an 18-month period spanning January 1, 2004 and June 30, 2005 were identified. Because of the fundamental interest in whether individuals choose a nonprofit or a for-profit facility contingent upon the geographic proximity of selection options, it is important to identify individuals who have not previously made the choice in the past, which is the rationale for analyzing an “inception” cohort of new admissions. New admission status was determined by tracking all available MDS records for each individual back to 1999 to make sure that no prior nursing home entry has been indicated for that individual. Furthermore, given our interest in examining post-acute patient outcomes, our final analytic file was restricted to those who were newly admitted to nursing homes under the Medicare SNF benefit following a prequalifying hospital stay. Although the goal of SNF care for these newly admitted patients is a discharge back to the community, certain individuals will not achieve this outcome and instead transition to long-stay nursing home residence. These patients are included in the final analytic file, but we consider only the post-acute part of their stay in the construction of our outcomes.
3.3. Empirical Specification
The standard empirical approach to examining the effect of nonprofit ownership on the provision of nursing home quality has been to estimate a reduced form equation that includes a dummy variable measuring ownership type. The basic specification for this approach is:
| (1) |
where Y refers to the quality measure for person i in nursing home j in state s, NFP is a dummy variable for nonprofit ownership status, X includes an intercept and a set of exogenous controls, ν is a state fixed effect, and ε is the residual. The primary variable of interest in this study is a dummy variable coded as 1 for nonprofit ownership and 0 for for-profit ownership. Importantly, when the OSCAR has been compared against other administrative data sources, organizational characteristics such as ownership type have shown strong validity (Straker 1999). A relatively small percentage of facilities (6%) are government-owned. Some of these facilities serve particular populations (e.g., Veterans Affairs beneficiaries) and others serve as safety net providers (e.g., many city or county facilities). Therefore, for many prospective residents, government facilities may not be close substitutes for private facilities. In our primary analyses, we exclude government-owned facilities and their residents, but we present a sensitivity analysis that includes these facilities.
In this study, quality Y is represented by several measures specific to the short-stay patient population. The quality measures are change in ADL functioning, change in mobility status, change in pain status, and re-hospitalization within 30 days. Across the measures, the possibility of informative censoring due to death or loss to follow-up exists. For the hospitalization outcome, some residents may die in the nursing home without hospitalization within 30 days. For the MDS based outcomes, Medicare post-acute patients are assessed at time of admission, day 5, day 14 and day 30 of their stay. In order to evaluate improvement over time in the outcomes, we compare performance across two assessments. For time 1, we use the first assessment collected (typically the admission assessment). For time 2, we use the assessment closest to the 30th day. For individuals with a follow-up assessment in our sample, the average time between assessments was 11.96 days (SD = 8.2). However, some individuals die or are discharged without a follow-up assessment. Among all post-acute patients in our study sample, 8.1% died without a follow-up MDS assessment within the 30-day window and 33.6% were discharged alive without a follow-up assessment. If we ignored this censoring, it could introduce bias into the measurement of the outcomes. To account for this, we estimate multinomial models that incorporate censoring. Thus, we model pain, mobility, and ADL functioning based on four outcomes: improvement, worsening, missing, and death. For the hospitalization measure, we model three 30-day outcomes: hospitalization, death, and neither hospitalization nor death.
A series of exogenous variables at the person, facility, zip code and state level were included as controls in this study. In particular, at the person level, we control for age, gender, race, education, marital status, Medicaid eligibility, diabetes, congestive heart failure, hip fracture, Alzheimer’s, other dementia, stroke, manic depression, schizophrenia, emphysema/COPD, cancer, shortness of breath, number of medications in prior 7 days, and a cognitive performance scale (CPS). Importantly, the person-level health measures were obtained from the MDS admission assessment and thus cannot be influenced by the care of the facility directly. At the facility level, we controlled for the occupancy rate, the number of beds, urban/rural status, hospital-based facility and chain membership. At the zip-code level, we controlled for per capita income and the elderly poverty rate. We also controlled for state fixed effects.
We first estimate equation 1 using a multinomial logit model. However, this approach may suffer from bias due to the suspected endogeneity of ownership status and nursing home quality. The error term in equation 1 is likely to include unobserved health status that may be correlated with ownership status. As such, we next estimate an instrumental variables model. Assume that nonprofit status NFP has the following reduced form:
| (2) |
where DD is the differential distance between the nearest nonprofit and for-profit nursing homes, X is the same set of variables that appeared in the quality equation, ν is a state fixed effect, and μ is the residual.
A key econometric issue is that nonprofit status NFP may be correlated with the error term in the quality equation (Sloan 2000). Unobserved factors may be correlated with both an individual’s ownership choice and the quality of their nursing home care. For example, an individual in poorer health may be more likely to choose a nonprofit nursing home and also experience worse outcomes on the measures used to reflect quality. Indeed, observable measures of health such as the Changes in Health, End-stage disease and Symptoms and Signs (CHESS) score, the number of drugs taken, the Resource Utilization Groups (RUGS) score, and other medical conditions are correlated with the choice of nonprofit ownership among post-acute patients and worse quality outcomes.
The differential selection of less healthy individuals into nonprofit nursing homes may reflect both demand and supply side factors. On the demand side, this negative selection may relate to the higher value that sicker individuals place on nonprofit status as a signal that the promised level of quality will be delivered. In other words, patients in worse health have the most to gain from higher quality nonprofit care. On the supply side, nonprofits may be more willing to admit sicker, more costly patients. Although Medicare SNF payment is case-mix adjusted, the system uses a relatively narrow set of patient conditions in adjusting payments.
If unobserved health is similarly correlated with ownership choice and quality, the error terms ε and μ will be correlated, which violates the assumptions underlying the linear regression model. However, we can still generate a consistent estimate of the effect of nonprofit status on quality if we can identify a variable DD that is correlated with nonprofit status but not ε, the error term in the quality equation. Given DD, we can calculate an IV estimate of the effect of nonprofit status on quality.
We assume that differential distance between the nearest nonprofit and for-profit will strongly predict entry into a nonprofit nursing home. A large health services literature establishes the importance of distance in the choice of provider (e.g., McClellan, McNeil et al. 1994; Hirth, Chernew et al. 2003; Brooks, Irwin et al. 2006) and research also suggests that distance matters in the choice of nursing home (e.g., Zwanziger, Mukamel et al. 2002; Shugarman and Brown 2006). Indeed, in our study, the median distance traveled to a SNF for post-acute care was 9.75 kilometers. In the study that most closely mirrors the distance-based instrument used in this study, Brooks and colleagues (2006) found the relative proximity to for-profit and nonprofit dialysis facilities to be the strongest predictor of the type of facility chosen, and that use of this measure as an IV eliminated the relationship between ownership and patient survival that existed in the observational data.
We also expect differential distance to be uncorrelated with unobserved factors that may influence outcomes. We assert that individuals choose a place of residence without regard to the proximity of nonprofit and for-profit nursing homes. The relatively low rate of elderly migration supports this assumption (U.S. Census Bureau 2003). Moreover, although Norton and Staiger (1994) found that hospitals chose organization type endogenously with characteristics of the local population, the wide and historical variability of nonprofit prevalence geographically helps support the validity of our instrument in the nursing home context. That is, the relative proportions of nonprofit and for-profit nursing homes have been relatively static within-markets over time (Grabowski and Stevenson, 2008). The relative share of nonprofits in different parts of the country is rooted in historical factors such as the age of the city and different patterns of voluntarism and charitable provision that have little to do with the advanced technology and prevalence of third party payment that characterize the current health care environment (Stevens 1989). The conversions across for-profit and nonprofit ownership (roughly 75 in each direction per year) and the limited entry and exit over time do not create major changes in the presence of ownership types in the majority of local markets. As such, we hypothesize that the differential distance measure is predetermined for potential nursing home residents and unrelated to unobserved quality of care. In the next section, we report a falsification test to validate this assumption.
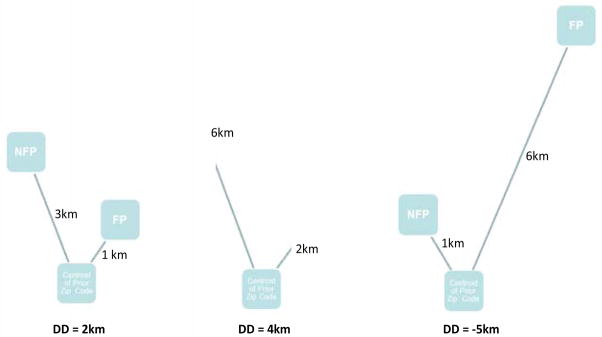
To construct a differential distance (DD) measure for nursing home residents, we calculated the distance using the great circle formula from the centroid of the resident’s zip code prior to nursing home admission, as reported in the MDS admission assessment, to the exact geo-address of the nearest nonprofit and for-profit facilities based on the latitude and longitude of the respective facilities. The differential measure was then calculated as the distance to the nearest nonprofit minus the distance to the nearest for-profit. In other words, the measure’s interpretation is how much farther the resident would have to re-locate to be admitted to the nearest nonprofit facility (see Figure 1 for examples). A negative value on this measure indicates that the nearest facility is a nonprofit.
Figure 1.
Examples of differential distance (DD) calculation between nearest nonprofit (NFP) and for-profit (FP) nursing homes
In the estimation of our IV models, we account for the fact that both our endogenous regressor (ownership status) and our outcomes of interest (e.g., hospitalization, death or neither) are binary or multinomial measures. Recent methodological papers have stressed the potential for bias when standard two-stage least squares IV methods are employed (e.g., Bhattacharya, Goldman et al. 2006; Terza, Bradford et al. 2008). Even in cases such as ours with large sample size, this bias is not attenuated. Assuming a valid instrument, the two-stage residual inclusion (2SRI) method has been shown to provide unbiased estimates (Terza, Basu et al. 2008). In 2SRI, the endogenous variables are not replaced by first-stage predictors but rather the first-stage residuals are included as an additional regressor in the second stage. In our application, we estimate the first stage using least squares and the second stage using a multinomial logit. In the results section, we present marginal effects at the mean for the key outcomes. The full multinomial results are available upon request.
In grouped data such as ours, a concern involves the likely presence of heteroskedasticity. When the true specification of the residual variance-covariance matrix follows such a structure, Moulton (1990) has shown that estimates of the standard errors will be biased downwards. A straightforward and unrestrictive approach to addressing this issue is to adjust the standard errors using the Huber-White robust estimator clustered at the zip-code level.
Tables 1 and 2 summarize the variables used in our analysis. Roughly 37% of the post-acute patients are admitted to nonprofit facilities. The average age of the sample is 80.8 years old, roughly two-thirds are female, 89% are white, 35% are married, and 20% are Medicaid-eligible. In terms of outcomes, 18.2% of the sample is hospitalized within 30 days and 5.2% dies (without hospitalization). Improvement in ADL functioning (34.3%), pain status (7.4%), and mobility (29.7%) all occurred to varying degrees. As expected, we observed significant missing outcomes and loss to follow-up with all three measures due to the rapid discharge prior to a scheduled assessment. Once again, we estimate multinomial models that incorporate censoring to guard against measurement bias. The average differential distance was 5.59 kilometers (or 3.47 miles), suggesting the typical patient in our sample had to travel 5.59 additional kilometers to the nearest nonprofit facility relative to the nearest for-profit.
Table 1.
Descriptive statistics: Post-acute residents (N=874,143)
| Mean | Std. Dev. | |
|---|---|---|
| Nonprofit status | 0.370 | 0.483 |
| Age | 80.810 | 7.618 |
| Female | 0.654 | 0.476 |
| White | 0.888 | 0.316 |
| High school graduate | 0.366 | 0.482 |
| More than high school | 0.398 | 0.489 |
| Missing education | 0.167 | 0.373 |
| Married | 0.354 | 0.478 |
| Diabetes | 0.270 | 0.444 |
| Congestive heart failure | 0.215 | 0.411 |
| Hip fracture | 0.093 | 0.291 |
| Alzheimer’s disease | 0.052 | 0.223 |
| Stroke | 0.125 | 0.331 |
| Dementia (non-Alzheimer’s) | 0.130 | 0.336 |
| Manic depression | 0.006 | 0.079 |
| Schizophrenia | 0.005 | 0.073 |
| Emphysema/Chronic obstructive pulmonary disease | 0.193 | 0.394 |
| Cancer | 0.095 | 0.294 |
| Shortness of breath | 10.445 | 4.441 |
| Number of medications in last 7 days | 1.339 | 1.605 |
| Cognitive Performance Scale | 0.174 | 0.379 |
| Medicaid eligible | 0.203 | 0.403 |
| Occupancy rate | 0.851 | 0.137 |
| Total number of beds | 120.558 | 80.362 |
| Urban facility | 0.826 | 0.379 |
| Hospital-based facility | 0.190 | 0.393 |
| Chain-owned facility | 0.561 | 0.496 |
| Per capita income in origin zip code | 22,345.440 | 9,214.681 |
| Poverty rate in origin zip code | 9.427 | 6.303 |
| Differential distance in km (nearest nonprofit minus nearest for-profit) | 5.587 | 15.590 |
Table 2.
Summary of post-acute outcomes (N=874,143)
| Mean | Std. Dev. | |
|---|---|---|
| Hospitalized (before death) in 30 days | 0.183 | 0.387 |
| Died in 30 days | 0.051 | 0.220 |
| Neither hospitalized, nor died in 30 days | 0.766 | 0.423 |
| ADL functioning improved | 0.343 | 0.475 |
| ADL functioning stable/worsened | 0.240 | 0.427 |
| Missing ADL functioning/no follow-up | 0.336 | 0.472 |
| Died | 0.081 | 0.273 |
| Pain improved | 0.074 | 0.261 |
| Pain stable/worsened | 0.509 | 0.500 |
| Missing pain/no follow-up | 0.336 | 0.472 |
| Died | 0.081 | 0.273 |
| Mobility improved | 0.297 | 0.457 |
| Mobility stable/worsened | 0.286 | 0.452 |
| Missing mobility/no follow-up | 0.336 | 0.472 |
| Died | 0.081 | 0.273 |
Notes:
ADL = Activities of daily living
3.4 Effect of Differential Distance: Specification Tests
Problems with weak instruments are well-known (Staiger and Stock 1997; Stock and Yogo 2005) and Bound and colleagues (1995) have argued that the use of instruments that jointly explain little variation in the endogenous regressors can do more harm than good. The differential distance instrument meets the standard of Staiger and Stock, with the F-statistics far exceeding the threshold of 10. The first-stage estimates suggest that a one kilometer increase in the differential distance between the nearest nonprofit and for-profit led to a 0.5 percentage point decrease in the likelihood of choosing a nonprofit (see first column of Table 3).
Table 3.
First-stage results, regression of nonprofit ownership on differential distance
| All | Entered NH 100km+ | Entered NH 200km+ | Entered NH 500km+ | |
|---|---|---|---|---|
| Differential Distance (nearest nonprofit – nearest for-profit) | −0.0048 (31.40) | −0.000182 (1.54) | −0.000184 (1.57) | −0.00005 (0.32) |
| R-squared | 0.3449 | 0.295 | 0.272 | 0.267 |
| Observations | 874,143 | 44,484 | 30,253 | 20,843 |
Notes: Regression includes all the covariates reported in Table 1 and state fixed effects.
Robust t-statistics clustered at the zip code level are reported in parentheses.
NH = Nursing home
In addition to the assumption regarding the instruments being strongly associated with the endogenous variable, IV also assumes the instrument must not be correlated with the error term in the second stage of IV estimation. If it is still correlated, then the instrumented variable will still be endogenous. Although it is impossible to confirm the null hypothesis that the instrument is uncorrelated with the error term in the quality equation, a standard practice within the literature is to report whether the instrument is correlated with those observed factors that affect the second-stage error term. Thus, we divide the variables used within this study by those observations that are above or below the median in differential distance (see Table 4). As expected (and shown in the first-stage above), nonprofit status is 23.41 percentage points higher for those patients with distances below the median. The other patient-level measures are remarkably similar across the two groups, suggesting the samples are balanced and mitigating concerns that large unobserved differences exist between populations located relatively close to facilities of different ownership types.
Table 4.
Person-level characteristics by differential distance (DD) between nearest nonprofit and nearest for-profit (N=874,143)
| DD<median | DD>median | |
|---|---|---|
| Nonprofit status | 0.486 | 0.255 |
| Age | 80.967 | 80.653 |
| Female | 0.657 | 0.650 |
| White | 0.887 | 0.888 |
| High school graduate | 0.366 | 0.365 |
| More than high school | 0.406 | 0.390 |
| Missing education | 0.174 | 0.160 |
| Married | 0.347 | 0.360 |
| Diabetes | 0.268 | 0.272 |
| Congestive heart failure | 0.213 | 0.217 |
| Hip fracture | 0.092 | 0.095 |
| Alzheimer’s disease | 0.050 | 0.055 |
| Stroke | 0.122 | 0.129 |
| Dementia (non-Alzheimer’s) | 0.128 | 0.132 |
| Manic depression | 0.006 | 0.006 |
| Schizophrenia | 0.006 | 0.005 |
| Emphysema/Chronic obstructive pulmonary disease | 0.189 | 0.197 |
| Cancer | 0.096 | 0.094 |
| Shortness of breath | 10.478 | 10.413 |
| Number of medications in last 7 days | 1.309 | 1.369 |
| Cognitive performance scale | 0.171 | 0.178 |
| Medicaid eligible | 0.198 | 0.209 |
As a final specification check, we conducted a falsification test of our instrument, which we draw from the identification strategy of an unrelated recent study. Doyle (2011) used people treated in Florida that did not reside there (“vacationers”) as a means of addressing selection of individuals into high and low cost areas in studying the relationship between spending and health care outcomes. We borrow from this idea by examining individuals who enter a nursing home far away from their primary residence. The concentration of non-profit nursing homes around their primary residence should not affect entry into a NFP for those individuals who enter a nursing home near a family member living elsewhere or get sick or need surgery while on vacation. For this sub-sample of “vacationers,” the first stage should be small and insignificant. If it is negative and significant, it suggests that where individuals live relative to the nearest NFP and FP is correlated with unmeasured quality (which would violate the assumption underlying a valid instrument).
In conducting this falsification test, we alternately define this vacationer sub-sample as individuals entering a nursing home over 100 km (N=44,484 or 5.1% of full sample), 200 km (N=30,253 or 3.5% of full sample) or 500 km (N=20,843 or 2.4% of full sample) away from their primary residence. The results suggest a weak first-stage estimate of the DD instrument for the vacationer sub-samples (see columns 2–4 in Table 3). When we use cutoffs of 100 or 200 kilometers to define the vacationer sub-sample, the first-stage estimate is roughly 4% as large as the result from the full sample. When we use a cutoff of 500 kilometers, the effect is about 1% as large as the full sample. The results are not statistically meaningful in any of these sub-samples. Thus, this falsification check does not support the idea that an individual’s place of residence relative to the nearest NFP and FP is correlated with other (unmeasured) factors that predict quality of care.
4. Results
4.1 Primary Findings
The estimates of the effect of profit status on quality of care are presented in Table 5. In the table, we present both the standard model that treats profit status as exogenous, and the IV model that treats profit status as endogenous (N=874,143). Results are presented as marginal effects at the mean. For the majority of outcomes, the results are quite different across the two models.
Table 5.
Marginal effects of being treated in a nonprofit home instead of a for-profit home (N=874,143)
| Outcome | Multinomial Logit | 2SRI |
|---|---|---|
| Hospitalized within 30 days | −0.0189*** (16.07) | −0.0174** (2.293) |
| Mobility improved | −0.011*** (5.40) | 0.0283** (2.331) |
| Pain improved | −0.000469 (0.54) | 0.0147*** (2.654) |
| ADL functioning improved | −0.017*** (7.61) | 0.0380*** (2.838) |
Notes: Results are presented as marginal effects at the mean. Full multinomial results available upon request. Models include all the covariates reported in table 1 and state fixed effects. Robust t-statistics clustered at the zip code-level are reported in parentheses.
ADL = activities of daily living
In the multinomial logit model results, short-stay patients in nonprofit facilities are 1.9 percentage points less likely to be hospitalized within 30 days. Improvement in mobility was 1.1 percentage points lower in nonprofit facilities, while improvement in ADL functioning was 1.7 percentage points lower. The multinomial logit approach did not suggest a statistically meaningful difference in the improvement of pain by ownership status. Thus, when we fail to account for the endogeneity of ownership status, our results suggest a very mixed story with patients in nonprofits faring better in terms of hospitalizations but worse in terms of mobility and ADL improvement. Across all three MDS outcomes, the multinomial logit findings suggest a negative correlation between (endogenous) nonprofit ownership and nursing home quality, which is consistent with the idea that poorer health is correlated with both nonprofit ownership and the outcomes of care used to assess quality.
When we account for endogenous ownership in the IV models, we obtain a much more consistent story regarding ownership and short-stay quality. Specifically, patients admitted to nonprofit facilities are 1.74 percentage points less likely to be re-admitted to the hospital within 30-days. They are also 2.83 percentage points more likely to experience mobility improvement, 1.47 percentage points more likely to experience improvement in pain status, and 3.80 percentage points more likely to experience improvement in ADL functioning. As a percentage of the dependent variable mean, admission to a nonprofit is associated with between 9.5% and 19.9% better quality relative to admission to a for-profit. Thus, unlike the uninstrumented multinomial logit model, a remarkably consistent picture of the relationship between ownership and short-stay quality emerges when we instrument for endogenous ownership.
4.2 Specification Checks
In order to examine the robustness of our primary model specification, we ran a series of alternate models (see Table 6). As a first check, we excluded those discharges to hospital-based nursing homes from our dataset. The concern is that hospital-based nursing homes might selectively attract patients from the hospital to which they are affiliated (Stearns, Dalton et al. 2006). When we re-ran the model excluding the hospital-based discharges, the 30-day hospitalization and ADL functioning results were robust, but the pain and mobility estimates were smaller and no longer statistically meaningful.
Table 6.
Specification checks (N=874,143 unless otherwise noted)
| Hospitalized within 30 days | Mobility improved | Pain improved | ADL functioning improved | |
|---|---|---|---|---|
| Baseline model | −0.0174** (2.293) | 0.0283** (2.331) | 0.0147*** (2.654) | 0.0380*** (2.838) |
| Exclude Hospital-based NHs (N=707,737) | −0.0172** (2.152) | 0.0209 (1.521) | 0.00901 (1.44) | 0.0295** (2.001) |
| Urban NHs only (N=722,466) | −0.0247** (2.277) | 0.0341** (1.975) | 0.0206** (2.555) | 0.0401** (2.144) |
| Rural NHs only (N=151,677) | −0.0137 (1.386) | 0.0111 (0.699) | 0.00354 (0.463) | 0.0168 (0.951) |
| Most competitive markets (N=448,514) | −0.0534*** (3.55) | 0.0816*** (3.09) | 0.0052 (0.47) | 0.0772*** (2.75) |
| Include health referral region fixed effects | −0.0194** (2.428) | 0.0151 (1.248) | 0.00355 (0.61) | 0.0251* (1.88) |
| Supply of NH beds included in the model (N=855,612) | −0.0248*** (3.118) | 0.0318** (2.397) | 0.0165*** (2.771) | 0.0437*** (3.022) |
| Include government facilities (N=912,970) | −0.0151** (1.988) | 0.0216* (1.721) | 0.0147** (2.566) | 0.0304** (2.182) |
| Binary DD measure (above/below) median | −0.0395*** (6.165) | −0.0047 (0.417) | 0.00344 (0.711) | −0.00493 (0.403) |
| Logged values of DD measure | −0.0430*** (7.307) | −0.00303 (0.295) | 0.000612 (0.138) | 0.00218 (0.193) |
| Exclude NHs in same zip code as resident prior address (N=635,786) | −0.0249** (1.961) | 0.0350* (1.828) | 0.0230** (2.519) | 0.0425** (2.057) |
Notes: Results are presented as marginal effects at the mean. Full multinomial results available upon request. Models include all the covariates reported in table 1 and state fixed effects unless otherwise noted. Robust t-statistics clustered at the zip code-level are reported in parentheses.
DD = Differential distance; NH = nursing home; ADL = activities of daily living.
Another potential concern is that the exclusion of discharges to government nursing homes may have biased the results. When we added discharges to government facilities and included a corresponding instrument for differential distance to a government provider relative to the next nearest facility, the nonprofit findings were robust across all the outcomes. Interestingly, the quality of post-acute care in government facilities was relatively poor compared to for-profit facilities. Patients in government facilities had significantly less improvement in ADL functioning and mobility, while the hospitalization and pain results were not statistically meaningful at conventional levels of significance.
Another potential issue is that the effects we observed might be predominantly concentrated in certain markets. When we estimated our models conditional on urban and rural markets, our primary findings were still present. However, given the loss in precision due to smaller sample sizes, the results were not statistically meaningful in rural markets. We also investigated whether the magnitude of our result varied based on the competitiveness of the local market (Duggan 2002). Using the country to approximate the market, we split the sample based on the median Herfindahl value. We found that nonprofit nursing homes located in the most competitive (i.e., least concentrated) markets were less likely to hospitalize patients and more likely to exhibit ADL functioning and mobility improvement. Thus, across three of the measures, the nonprofit effect was stronger in more competitive markets.
The primary models include state fixed effects. However, one concern is that unobserved factors at the market level may be correlated with both ownership and quality of care. For example, more concentrated nursing home markets might have less access to nonprofit nursing homes and lower quality of care due to reduced competition. In order to address this concern, we substituted health referral region (HRR) fixed effects for state fixed effects in our model. With HRR fixed effects, the 30-day hospitalization and ADL functioning results both suggested higher quality in nonprofit nursing homes. Mobility and pain improvement still had positive coefficients for nonprofit ownership but were no longer statistically significant. We also ran another check in which we included a term in the model measuring the local supply of nursing home beds. The inclusion of this measure did not alter our primary conclusions.
We also experimented with different forms of the DD instrument including a binary measure (above/below median) and logged values (log of distance to nearest nonprofit minus log distance to nearest for-profit) to take account of skewed values. The results were relatively robust for the hospitalization outcome but less so for the other outcomes. Given that both the binary and logged versions of the instrument tend to suppress the role of large absolute values, the primary IV results for the MDS outcomes may be driven by larger values of the DD instrument. The reason as to why this occurs for the MDS based outcomes but not the hospitalization outcome is unclear. However, one possible explanation is that nearly one-third of our sample did not have a follow-up MDS assessment, while the hospitalization measure had no loss to follow-up. Although we attempt to account for this censoring in our estimation, the MDS based outcomes are bound to yield less robust estimates relative to the hospitalization outcome.
Finally, because we approximated the resident’s prior residence by the centroid of the zip code area from which the resident was admitted, the DD instrument will have the greatest measurement error when a nursing home is located in that same zip code. When we exclude those cases in which a nursing home was located in their zip code of prior residence, all our results have the same sign and significance but slightly larger effect magnitudes than our baseline estimates.
In summary, the specification checks suggest the hospitalization results are very robust across all the checks, and the results for ADL function are robust across most of the checks. The results based on the other MDS outcomes are less robust, but in several cases, the point estimates were relatively similar but the smaller sample caused a loss in precision.
5. Conclusion
A large health economics literature has investigated the relationship between ownership status and quality of care. The majority of these studies treat ownership as exogenous, although there are reasons to suspect that firms jointly choose their ownership form and quality of care (Sloan 2000). Our results suggest that—after instrumenting for endogenous ownership—nonprofits nursing homes provide better quality for short-stay patients relative to their for-profit counterparts. Unlike the multinomial logit (uninstrumented) models, the instrumented result is consistent across distinct measures of short-stay quality. Therefore, failure to account for the endogeneity of ownership would lead to an errant conclusion that ownership does not have a systematic relationship to quality of care, which could lead to unjustified policy prescriptions.
Rough calculations based on our estimates suggest that nonprofit ownership status had a large and policy-relevant effect on short-stay nursing home quality. More specifically, over our 18-month period of study, 56,752 30-day readmissions occurred among the 323,604 nonprofit nursing home residents in our sample. Our baseline 2SRI estimate implies that 5,631 additional readmissions would have occurred if these facilities were for-profit owned. If we assume Medicare paid $10,000 per readmission (Mor, Intrator et al. 2010), nonprofit ownership saved over $56 million dollars in Medicare expenditures over our period of study. Furthermore, the 550,539 individuals in our sample admitted to for-profit nursing homes had 103,053 30-day readmissions. Our results imply that nonprofit ownership would have prevented 9,579 readmissions, saving nearly $96 million dollars over the sample period.
From a policy perspective, we can use this $96 million figure to conduct a “back-of-the-envelope” cost-benefit analysis of the nonprofit tax exemption. On the cost side, we need to calculate the dollar value of the tax exemption for nonprofit nursing homes. We are not aware of a published estimate of this value from the nursing home nonprofit literature. However, Kane and Wubbenhorst (2000) estimate that value of the tax exemption for nonprofit hospitals is 3.2% of revenues. Applying this figure to SNF Medicare revenues using the 2004–5 Medicare SNF cost reports, nonprofit nursing homes received a total tax exemption of $391 million over the 18-month study period.2 Although this rough calculation suggests that the nonprofit tax exemption generates costs in excess of the savings in hospital spending, at least one caveat is worth bearing in mind. This exercise ignored any other potential benefits from nonprofit status such as improved quality (and the associated Medicare/Medicaid savings), charity care, or increased access for underserved populations.
Although we cannot directly identify the mechanism underlying our result, the likely pathway towards higher nonprofit post-acute quality is via the level and quality of nurse staffing. Labor is the dominant input in skilled nursing facility care, accounting for roughly two-thirds of expenses. Our data suggest nonprofits staff at a level above for-profit facilities, even after adjusting for their higher acuity. We cannot measure it directly in our data but it also may be the case that nonprofits hire and retain better skilled nurse staff and therapists.
Future research might better tease out how exactly nonprofits generate better outcomes, but our results can still be useful for resident care planning. First and foremost, our estimates of the causal effect of ownership on quality can aide prospective residents and their public and private advocates in making better care decisions. For example, the ownership status of facilities is currently reported on Nursing Home Compare (www.medicare.gov/NHCompare), the government’s nursing home report card effort. In addition to the quality measures reported on the website (e.g., survey deficiencies, staffing, pressure ulcers), the results of this study provide salience to ownership status as a signal of quality. Second, an improved understanding of the effects of ownership also contributes to the assessment of an area’s long-term care resources, even if direct policy measures to change the environment cannot be implemented quickly.
From a methodological perspective, this study provides long-term care researchers with a potential new approach to analyzing for-profit and nonprofit differences which accounts for unobserved patient differences across ownership types, and which could also be applied to study the impact of other facility characteristics such as chain ownership. Moreover, this IV strategy provides information on the implications of ownership for the increasingly important short-stay population that has received far less attention than the “traditional” long-stay nursing home population.
Acknowledgments
We gratefully acknowledge funding from the National Institute on Aging (R01 AG034179; P01 AG027296).
Footnotes
We examined the reliability and consistency of the resident’s prior primary residence zip code information as reported on the admission minimum data set (MDS) assessment as compared to the zip code data contained in the Medicare enrollment file for the same person. Specifically, we first identified all new nursing home admissions in 2000. Next, we matched these individuals to their enrollment records covering a three-year period: 1999, 2000, and 2001. We compared the resident’s 1999 enrollment zip code (before ever entering a nursing home) with his/her prior residence zip code according to the 2000 admission MDS. As expected, a high percentage (83%) of short-stay residents had common zip codes across the two data sources, presumably because most short-stayers return to their prior-admission residence within a short period of time. This reasonably high level of congruence indicates the reliability of the prior residence zip code information as reported in the MDS. We also assessed the stability of the resident’s enrollment zip codes one year before and one year after the year of nursing home admission. Among short-stayers, 84% reported the same enrollment zip in 1999 and 2001.
We calculate this number using the following steps: 1) from the 2004–5 Medicare cost reports, the average nonprofit SNF had roughly $15 millon in revenue over the 18 month study period. 2) We assumed that 20% of this revenue (i.e., $3 million) came from the care of post-acute SNF patients. 3) Using the Kane and Wubbenhorst (2000) estimate of the tax exemption relative to revenues (3.2%) from the hospital literature, the value of the tax exemption for each nonprofit facility (for their SNF care) over the study period was $96,000 (= 3.2% times $3 million). 4) We had 4,074 nonprofits in our dataset, suggesting the total value of the nonprofit tax exemption for Medicare nonprofit SNF care was $391 million (= 4,074 times $96,000).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
David C. Grabowski, Harvard University.
Zhanlian Feng, Brown University.
Richard Hirth, University of Michigan.
Momotazur Rahman, Brown University.
Vincent Mor, Brown University.
References
- Bhattacharya J, Goldman D, et al. Estimating probit models with self-selected treatments. Stat Med. 2006;25(3):389–413. doi: 10.1002/sim.2226. [DOI] [PubMed] [Google Scholar]
- Bound J, Jaeger DA, et al. Problems with instrumental variables estimation when the correlation between the instruments and the endogenous explanatory variable is weak. Journal of the American Statistical Association. 1995;90(430):443–450. [Google Scholar]
- Brooks JM, Irwin CP, et al. Effect of dialysis center profit-status on patient survival: a comparison of risk-adjustment and instrumental variable approaches. Health Serv Res. 2006;41(6):2267–89. doi: 10.1111/j.1475-6773.2006.00581.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cawley J, Grabowski DC, et al. Factor substitution in nursing homes. Journal of Health Economics. 2006;25(2):234–47. doi: 10.1016/j.jhealeco.2005.06.004. [DOI] [PubMed] [Google Scholar]
- Comondore VR, Devereaux PJ, et al. Quality of care in for-profit and not-for-profit nursing homes: systematic review and meta-analysis. Bmj. 2009;339:b2732. doi: 10.1136/bmj.b2732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doyle JJ. Returns to Local-Area Healthcare Spending: Evidence from Health Shocks to Patients Far From Home. American Economic Journal: Applied Economics. 2011;3(3):221–243. doi: 10.1257/app.3.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duggan M. Hospital market structure and the behavior of not-for-profit hospitals. Rand J Econ. 2002;33(3):433–46. [PubMed] [Google Scholar]
- Eggleston K, Shen YC, et al. Hospital ownership and quality of care: what explains the different results in the literature? Health Economics. 2008;17(12):1345–62. doi: 10.1002/hec.1333. [DOI] [PubMed] [Google Scholar]
- Grabowski DC, Hirth RA. Competitive spillovers across non-profit and for-profit nursing homes. Journal of Health Economics. 2003;22(1):1–22. doi: 10.1016/s0167-6296(02)00093-0. [DOI] [PubMed] [Google Scholar]
- Grabowski DC, Huskamp HA, et al. Ownership status and home health care performance. Journal of Aging and Social Policy. 2009;21(2):130–43. doi: 10.1080/08959420902728751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabowski DC, Stevenson DG. Ownership conversions and nursing home performance. Health Services Research. 2008;43(4):1184–203. doi: 10.1111/j.1475-6773.2008.00841.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansmann HB. The Role of Nonprofit Enterprise. The Yale Law Journal. 1980;89(5):835–901. [Google Scholar]
- Hillmer MP, Wodchis WP, et al. Nursing home profit status and quality of care: is there any evidence of an association? Medical Care Research and Review. 2005;62(2):139–66. doi: 10.1177/1077558704273769. [DOI] [PubMed] [Google Scholar]
- Hirth RA, Chernew ME, et al. Chronic illness, treatment choice and workforce participation. Int J Health Care Finance Econ. 2003;3(3):167–81. doi: 10.1023/a:1025332802736. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Improving the quality of care in nursing homes. Washington, D.C: National Academy Press; 1986. [Google Scholar]
- Kane NM, Wubbenhorst WH. Alternative funding policies for the uninsured: exploring the value of hospital tax exemption. Milbank Q. 2000;78(2):185–212. 150. doi: 10.1111/1468-0009.00168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konetzka RT. Do not-for-profit nursing homes provide better quality? Bmj. 2009;339:b2683. doi: 10.1136/bmj.b2683. [DOI] [PubMed] [Google Scholar]
- Martin A, Lassman D, et al. Recession contributes to slowest annual rate of increase in health spending in five decades. Health Aff (Millwood) 2011;30(1):11–22. doi: 10.1377/hlthaff.2010.1032. [DOI] [PubMed] [Google Scholar]
- McClellan M, McNeil BJ, et al. Does more intensive treatment of acute myocardial infarction in the elderly reduce mortality? Analysis using instrumental variables. Jama. 1994;272(11):859–66. [PubMed] [Google Scholar]
- Mor V, Angelelli J, et al. Inter-rater reliability of nursing home quality indicators in the U.S. BMC Health Serv Res. 2003;3(1):20. doi: 10.1186/1472-6963-3-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor V, Intrator O, et al. The revolving door of rehospitalization from skilled nursing facilities. Health Affairs (Millwood) 2010;29(1):57–64. doi: 10.1377/hlthaff.2009.0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor V, Intrator O, et al. Temporal and Geographic variation in the validity and internal consistency of the Nursing Home Resident Assessment Minimum Data Set 2.0. BMC Health Serv Res. 2011;11:78. doi: 10.1186/1472-6963-11-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris JN, Hawes C, et al. Designing the national resident assessment instrument for nursing homes. Gerontologist. 1990;30(3):293–307. doi: 10.1093/geront/30.3.293. [DOI] [PubMed] [Google Scholar]
- Moulton BR. An illustration of a pitfall in estimating the effects of aggregate variables on micro units. The Review of Economics and Statistics. 1990;72(2):334–338. [Google Scholar]
- National Center for Health Statistics. 2004 Facility Tables. 2006 Retrieved December 26, 2006, from http://www.cdc.gov/nchs/data/nnhsd/nursinghomefacilities2006.pdf#01.
- Newhouse JP. Toward a Theory of Nonprofit Institutions: An Economic Model of a Hospital. American Economic Review. 1970;60(1):64–74. [Google Scholar]
- Norton EC, Staiger DO. How Hospital Ownership Affects Access to Care of the Uninsured. Rand Journal of Economics. 1994;25(1):171–185. [PubMed] [Google Scholar]
- Phillips CD, Morris JN, et al. Association of the Resident Assessment Instrument (RAI) with changes in function, cognition, and psychosocial status. J Am Geriatr Soc. 1997;45(8):986–93. doi: 10.1111/j.1532-5415.1997.tb02971.x. [DOI] [PubMed] [Google Scholar]
- Shugarman LR, Brown JA. Nursing Home Selection: How Do Consumers Choose? Volume I: Findings from Focus Groups of Consumers and Information Intermediaries. Washington, DC: Prepared for Office of Disability, Aging and Long-Term Care Policy, Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services; 2006. Contract #HHS-100-03-0023. [Google Scholar]
- Sloan FA. Not-For-Profit Ownership and Hospital Behavior. In: Cuyler AJ, Newhouse JP, editors. Handbook of Health Economics. Vol. 1. Amsterdam: Elsevier Science, North-Holland; 2000. pp. 1141–1174. [Google Scholar]
- Sloan FA, Ostermann J, et al. Antecedents of hospital ownership conversions, mergers, and closures. Inquiry. 2003;40(1):39–56. doi: 10.5034/inquiryjrnl_40.1.39. [DOI] [PubMed] [Google Scholar]
- Spillman BC, Lubitz J. New estimates of lifetime nursing home use: have patterns of use changed? Medical Care. 2002;40(10):965–75. doi: 10.1097/00005650-200210000-00013. [DOI] [PubMed] [Google Scholar]
- Staiger D, Stock JH. Instrumental Variables Regression with Weak Instruments Econometrica. 1997;65(3):557–86. [Google Scholar]
- Stearns SC, Dalton K, et al. Using propensity stratification to compare patient outcomes in hospital-based versus freestanding skilled-nursing facilities. Med Care Res Rev. 2006;63(5):599–622. doi: 10.1177/1077558706290944. [DOI] [PubMed] [Google Scholar]
- Stevens R. Sickness and in Wealth. New York: Basic Books; 1989. [Google Scholar]
- Stock JH, Yogo M. Testing for Weak Instruments in Linear IV Regression. In: Andrews DWK, Stock JH, editors. Identification and Inference for Econometric Models: Essays in Honor of Thomas Rothenberg. Cambridge: Cambridge University Press; 2005. pp. 80–108. [Google Scholar]
- Straker JK. Technical Report 3–01. Oxford, OH: Scripps Gerontology Center; 1999. Reliability of OSCAR Occupancy, Census and Staff Data: A Comparison with the Ohio Department of Health Annual Survey of Long-Term Care Facilities. [Google Scholar]
- Terza JV, Basu A, et al. Two-stage residual inclusion estimation: addressing endogeneity in health econometric modeling. Journal of Health Economics. 2008;27(3):531–43. doi: 10.1016/j.jhealeco.2007.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terza JV, Bradford WD, et al. The use of linear instrumental variables methods in health services research and health economics: a cautionary note. Health Serv Res. 2008;43(3):1102–20. doi: 10.1111/j.1475-6773.2007.00807.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Town R, Feldman R, et al. The impact of ownership conversions on HMO performance. International Journal of Health Care Finance and Economics. 2004;4(4):327–42. doi: 10.1023/B:IHFE.0000043761.95636.96. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. Census 2000 Special Reports. U.S. Department of Commerce; 2003. Internal Migration of the Older Population: 1995–2000. [Google Scholar]
- U.S. Government Accounting Office. California Nursing Homes: Care Problems Persist Despite Federal and State Oversight. U. G. A. Office; Washington, DC: 1998. [Google Scholar]
- Werner RM, Konetzka RT, et al. Impact of public reporting on unreported quality of care. Health Serv Res. 2009;44(2 Pt 1):379–98. doi: 10.1111/j.1475-6773.2008.00915.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner RM, Konetzka RT, et al. Impact of public reporting on quality of postacute care. Health Serv Res. 2009;44(4):1169–87. doi: 10.1111/j.1475-6773.2009.00967.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X, Grabowski DC. Nursing home staffing and quality under the nursing home reform act. Gerontologist. 2004;44(1):13–23. doi: 10.1093/geront/44.1.13. [DOI] [PubMed] [Google Scholar]
- Zwanziger J, Mukamel DB, et al. Use of Resident-Origin Data to Define Nursing Home Market Boundaries. Inquiry. 2002;39(1):56–66. doi: 10.5034/inquiryjrnl_39.1.56. [DOI] [PubMed] [Google Scholar]