ABSTRACT
BACKGROUND
Clinicians have difficulty in identifying patients that are unlikely to adhere to hypertension self-management. Identifying non-adherence is essential to addressing suboptimal blood pressure control and high costs.
OBJECTIVES
1) To identify risk factors associated with non-adherence to three key self-management behaviors in patients with hypertension: proper medication use, diet, and exercise; 2) To evaluate the extent to which an instrument designed to identify the number of risk factors present for non-adherence to each of the three hypertension self-management behaviors would be associated with self-management non-adherence and blood pressure.
DESIGN
Cross-sectional analysis of randomized trial data.
PATIENTS
Six hundred and thirty-six primary care patients with hypertension.
MEASUREMENTS
1) Demographic, socioeconomic, psychosocial, and health belief-related factors; 2) measures of self-reported adherence to recommended medication use, diet recommendations, and exercise recommendations, all collected at baseline assessment; 3) systolic blood pressure (SBP) and diastolic blood pressure (DBP).
RESULTS
We identified patient factors associated with measures of non-adherence to medications, diet, and exercise in hypertension. We then combined risk factors associated with ≥1 adherence measure into an instrument that generated three composite variables (medication, diet, and exercise composites), reflecting the number of risk factors present for non-adherence to the corresponding self-management behavior. These composite variables identified subgroups with higher likelihood of medication non-adherence, difficulty following diet recommendations, and difficulty following exercise recommendations. Composite variable levels representing the highest number of self-management non-adherence risk factors were associated with higher SBP and DBP.
CONCLUSIONS
We identified factors associated with measures of non-adherence to recommended medication use, diet, and exercise in hypertension. We then developed an instrument that was associated with non-adherence to these self-management behaviors, as well as with blood pressure. With further study, this instrument has potential to improve identification of non-adherent patients with hypertension.
KEY WORDS: hypertension, self-management, medication adherence, diet, exercise
BACKGROUND
Patient non-adherence (NA) to chronic disease treatment averages 50 %, exacerbating disease control and increasing costs.1,2 Alhough hypertension (HTN) is a modifiable cardiovascular risk factor, half of hypertensive patients have inadequate control;3 NA to HTN self-management contributes heavily to suboptimal care.4,5
Because HTN self-management NA is modifiable, identifying non-adherent patients is essential. Despite recognizing the influence of demographic, psychosocial, socioeconomic, and health belief-related factors on HTN self-management NA,6–24 physicians have difficulty identifying non-adherent patients. Existing HTN NA prediction instruments are often complex and none are widely accepted.25–30 Moreover, existing instruments focus solely on HTN medication adherence, ignoring important behaviors like diet and exercise. Consequently, clinicians lack convenient tools to help identify patients unlikely to follow HTN self-management recommendations. A simple means to ascertain likelihood of adhering to the three key aspects of HTN self-management—proper medication use, diet, and exercise—would facilitate targeted efforts to combat NA.
The goal of this analysis was to identify risk factors associated with measures of NA to each of the three key HTN self-management behaviors: proper medication use, diet, and exercise. Secondarily, we sought to assess the extent to which an instrument designed to identify the number of risk factors present for NA each of the three HTN self-management behaviors would be associated with self-management NA and blood pressure (BP). This study serves as an initial step in generating a clinically useful tool to facilitate identifying individuals unlikely to adhere to HTN self-management.
METHODS
Patient Population
We analyzed baseline data from the Take Control of Your Blood Pressure (TCYB) trial, which randomized hypertensive patients from two primary care clinics to: 1) behavioral management, 2) home BP monitoring, 3) a combination of 1 and 2, or 4) usual care.31 The study had Duke University Institutional Review Board approval and patients provided written informed consent. Subjects received HTN care at their clinic site for ≥12 months and used ≥1 antihypertensive medication. Poor BP control was not required for enrollment.
Exclusion criteria included: dementia; atrial fibrillation; dialysis dependence; patient of a study investigator; receipt of skilled nursing or home health; hospitalization for stroke, heart attack, revascularization, or metastatic cancer within 3 months; difficulty communicating by telephone; participation in another BP study; arm circumference >17 in. and wrist circumference >8.5 in.; or pregnancy.
Baseline Patient Factors
We examined associations between available patient factors and measures of NA to three HTN self-management behaviors, all assessed at study baseline. Because this project aimed both to identify risk factors associated with self-management NA and also to derive composite variables associated with the adherence measures, we dichotomized some patient factors based on existing data, item responses, or observed distributions to facilitate creating clinically useful composites.
Demographic factors included age, gender, race, education level <12 years, smoking status, diabetes status, employment status, and body mass index (BMI) <30.
Socioeconomic factors included:1) self-reported lack of social support (“Do you have someone you feel close to, can trust, and confide in?,” with responses yes/no);32 2) self-reported lack of financial security (“How would you describe your household’s financial situation?,” with responses ranging from 1 (After paying bills, I have money for special things) to 4 (I have difficulty paying bills, no matter what), dichotomized based on response content as lack of financial security present (≥3) or absent (≤2)); 3) Rapid Estimate of Adult Literacy in Medicine Score (REALM, dichotomized as <60 (<9th grade reading level) or ≥61 (>9th grade reading level);33 and 4) Hypertension Knowledge Score (HKS)34 (dichotomized as <7 or 7). The dichotomized REALM and HKS are validated measures, described in detail elsewhere.35
Psychosocial factors included: 1) high stress (“How often in the past month have you felt stressed?,” with responses ranging from 1 (never) to 5 (very often); responses were normally distributed, and we dichotomized as high stress present (≥4) or absent (≤3), which captured approximately the highest-stress tertile); 2) nervous personality (“Do you consider yourself a nervous or tense person?,” with responses ranging from 1 (no) to 4 (all the time); responses were distributed towards the scale extremes, and we dichotomized as yes (≥2) or no (≤1), which captured approximately the top 40 % of subjects with respect to nervousness); 3) depressed mood (“How often during the past month have you felt downhearted and blue?,” with responses ranging from 1 (all the time) to 6 (never); responses were skewed toward no depression, and we dichotomized as depressed mood present (≤4) or absent (≥5) based on response content); 4) lack of accomplishment due to psychosocial issues (“During the past month, have you accomplished less due to any emotional problems, such as depression or anxiety?,” with responses yes/no); 5) and lack of carefulness due to psychosocial issues (“During the past month, did you not do work or other activities as carefully due to any emotional problems, such as depression or anxiety?,” with responses yes/no).36
Health belief-related factors included: 1) belief that HTN is a serious issue (“How serious is it to have high blood pressure?,” with responses ranging from 1 (very serious) to 4 (not at all serious); because 75 % of responses were ‘1,’ we dichotomized as serious (1) or not serious (≥2)); 2) worry about HTN (“How worried are you about your high blood pressure?,” with responses ranging from 1 (definitely not worried) to 10 (extremely worried); responses were skewed towards worry, and we dichotomized as worry present (≥7) or absent (≤6), which divided the population approximately in half); and 3) belief that myocardial infarction (MI) is likely with the patient’s current lifestyle (“How likely are you to have a heart attack if you continue your current lifestyle?,” with responses ranging from 1 (very likely) to 3 (not at all likely); because 80 % of responses were ‘2’ or ‘3,’ we dichotomized as belief present (≤2) or absent (3 or don’t know)).
Baseline Measures of Adherence
We used three measures collected at baseline as indicators of NA to recommended medication use, diet, and exercise. Because dichotomous outcomes are more intuitive for clinicians, we dichotomized measures based on prior data or observed distributions. To evaluate medication adherence, we used the Self-reported Medication-Taking Scale.37,38 This measure was dichotomized as medication NA present (≤2, don’t know, or refused) or absent (≥3); this dichotomized measure is validated, and is described elsewhere.35 To evaluate diet and exercise, we used single-item measures reflecting self-reported difficulty following HTN-related diet (or exercise) recommendations (“Rate how difficult it is to follow diet (or exercise) recommendations to improve your blood pressure,” with responses ranging from 1 (not at all difficult) to 10 (extremely difficult)). We dichotomized these measures as difficulty present (≥7) or absent (≤6); in both cases, responses were normally distributed, and the cutoff captured approximately the most non-adherent tertile.
Statistical Analysis
This analysis consisted of 4 steps: 1) identification of patient factors associated with each of the three self-management NA measures; 2) creation of an instrument designed to generate three composite variables, each corresponding to one self-management NA measure and based on a number of risk factors present for NA to that behavior; 3) assessment of associations between each composite variable and corresponding self-management NA measure; and 4) assessment of associations between each composite variable and mean systolic and diastolic BP (SBP/DBP). All statistical analyses were performed using SAS Enterprise Guide, version 4.3, Cary, NC.
Associations Between Patient Factors and Adherence Measures
To identify factors associated with each self-management NA measure, we used multivariable logistic regression with backward elimination to estimate adjusted odds ratios (OR) and 95 % confidence intervals (CI) reflecting the likelihood of NA based on the presence of a patient factor. For each of the three models, low multicollinearity between baseline patient factors in association with each adherence measure was confirmed by examining the variance inflation factor.39 Prior to backwards elimination, each regression model included all patient factors described above.
Development of Adherence Instrument and Composite Variables
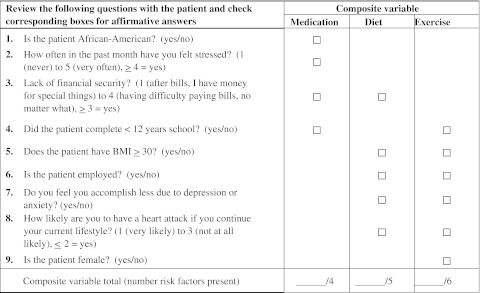
In creating the instrument, we included patient factors significantly associated with ≥1 of the three self-management NA measures. Based on multivariable logistic regression as detailed above, we identified ten factors associated with ≥1 measure of adherence; as we intended the instrument to be suitable for clinical use, we excluded one (REALM) due to unsuitability for clinic assessment. We used the remaining factors to create a 9-item instrument that generated three composite variables (medication, diet, and exercise composites) reflecting the number of risk factors present for NA to the corresponding self-management behavior (Text Box 1).
Text Box 1. Nine-item instrument comprising risk factors associated with non-adherence to 3 self-management behaviors in hypertension (proper medication use, diet, and exercise)
Associations Between Adherence Instrument and Adherence Measures
We structured each composite variable to divide the cohort into levels based on the number of risk factors present for NA to the corresponding self-management behavior. Using each composite variable as an independent variable, we performed simple logistic regression to determine associations between the levels of each composite variable and the corresponding NA measure. We then used multivariable logistic regression with backward elimination to determine adjusted OR and 95 % CI. Before elimination, each multivariable regression model also included all patient factors except for those included in the composite variable, and also adjusted for clinic site. To further evaluate site effects, we tested a site-by-composite interaction term; for each model, these were non-significant and ultimately not included. To better characterize each model, we determined c-statistics and Hosmer–Lemeshow goodness-of-fit tests.
Associations Between Adherence Instrument and Baseline Blood Pressure
To better understand how the instrument related to clinical outcomes, we examined associations between the levels of each composite variable and SBP/DBP. For each patient, we used the mean of two measurements made by digital sphygmomanometer to calculate baseline SBP/DBP. We ran six separate one-way ANOVA models, where the outcome variable was SBP or DBP and the main predictor was the medication, diet, or exercise composite variable. Tukey’s test was used to control for experiment-wise Type I error.
RESULTS
Baseline Characteristics
The 636 patients had a mean age of 61, were 49 % African-American, and 34 % male (Table 1); 73 % had well-controlled BP (<130/80 mmHg in diabetes, <140/90 mmHg otherwise).
Table 1.
Baseline Data for Patients in the Take Control of Your Blood Pressure Study
| Baseline Characteristics | Measure |
|---|---|
| Demographic | |
| Mean age (SD) | 61 (12) |
| Male | 34 % |
| Race | |
| African-American | 49 % |
| Caucasian | 48 % |
| Other | 3 % |
| Completed < 12 years school | 36 % |
| Current smoker | 16 % |
| Diabetes | 36 % |
| Employed | 39 % |
| Socioeconomic | |
| Endorsed lack of social support | 6 % |
| Lack of financial security | 19 % |
| Low health literacy (REALM ≤ 60) | 28 % |
| Low HTN knowledge (HKS < 7) | 65 % |
| Psychosocial | |
| High stress level | 38 % |
| Nervous or tense personality | 42 % |
| Depressed mood | 31 % |
| Lack of accomplishment due to psychosocial issues | 27 % |
| Lack of carefulness due to psychosocial issues | 19 % |
| Health Belief-Related | |
| Belief that HTN is a serious issue | 75 % |
| Worried about HTN | 50 % |
| Belief that MI is likely with the current lifestyle | 45 % |
| Adherence Measures | |
| Self-reported medication non-adherence | 36 % |
| Difficulty following diet recommendations | 34 % |
| Difficulty following exercise recommendations | 36 % |
| Clinical Measures | |
| BP controlled† | 73 % |
| Mean systolic BP (SD) ‡ | 125 (17) |
| Mean diastolic BP (SD) ‡ | 71 (11) |
| Mean BMI (SD) | 32.1 (8.2) |
Abbreviations: BP blood pressure, REALM Rapid Estimate of Adult Literacy in Medicine, HTN hypertension, HKS Hypertension Knowledge Score, MI myocardial infarction, BMI body mass index
*All data except blood pressure, and weight used in body mass index were patient-reported. When missing values existed, they were included in the calculation of percentages
†According to the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure guidelines: <130/80 mmHg for patients with diabetes and <140/90 mmHg for other patients
‡Patient blood pressure is based on average of two values obtained during study enrollment visit
Associations between Patient Factors and Adherence Measures
Multivariable logistic regression analysis identified patient factors that were significantly associated with each of the HTN self-management NA measures (Table 2). For medication NA, these risk factors included African-American race, low education level, lack of financial security, poor health literacy (REALM ≤60), and high stress level. For diet, risk factors included BMI ≥30, being employed, lack of financial security, lack of accomplishment due to psychosocial issues, and belief that MI is likely with current lifestyle. For exercise, risk factors included BMI ≥30, female gender, low education level, being employed, lack of accomplishment due to psychosocial issues, and belief that MI is likely with current lifestyle.
Table 2.
Adjusted Odds Ratios and 95 % Confidence Intervals for Associations Between Patient Factors and Hypertension Self-Management Adherence Measures, Determined Using Multivariable Logistic Regression Analysis With Backward Elimination
| Associated Patient Factors by Adherence Measure | Adjusted OR* [95 % CI] |
|---|---|
| Self-reported medication non-adherence: | |
| African-American race | 2.26 [1.53 to 3.34] |
| Completed < 12 years school | 1.58 [1.04 to 2.40] |
| Lack of financial security | 1.79 [1.11 to 2.89] |
| REALM ≤ 60 | 1.77 [1.12 to 2.80] |
| High stress level | 1.63 [1.12 to 2.38] |
| Difficulty following diet recommendations: | |
| BMI ≥ 30 | 2.11 [1.43 to 3.10] |
| Employed | 1.63 [1.13 to 2.37] |
| Lack of financial security | 1.63 [1.03 to 2.60] |
| Lack of accomplishment due to psychosocial issues | 1.64 [1.10 to 2.46] |
| Belief that MI is likely with current lifestyle | 1.49 [1.03 to 2.16] |
| Difficulty following exercise recommendations: | |
| BMI ≥ 30 | 1.53 [1.04 to 2.25] |
| Female gender | 1.68 [1.13 to 2.51] |
| Completed < 12 years school | 1.50 [1.01 to 2.23] |
| Employed | 1.84 [1.24 to 2.71] |
| Lack of accomplishment due to psychosocial issues | 2.09 [1.39 to 3.12] |
| Belief that MI is likely with current lifestyle | 2.05 [1.41 to 2.99] |
Abbreviations: OR odds ratio, CI confidence interval, REALM Rapid Estimate of Adult Literacy in Medicine, MI myocardial infarction, BMI body mass index
*Initial self-reported independent variables included in multivariable logistic regression analysis: age, gender, race, education level, smoking status, diabetes status, employment status, BMI ≥ 30, lack of social support, lack of financial security, Rapid Estimate of Adult Literacy in Medicine, Hypertension Knowledge Score, high stress level, depressed mood, lack of accomplishment due to psychosocial issues, lack of carefulness due to psychosocial issues, belief that hypertension is a serious issue, worry about hypertension, and presence of belief that a myocardial infarction is likely with the patient’s current lifestyle
Development of Adherence Instrument and Composite Variables
As described, in constructing this instrument, we included easily assessable demographic, socioeconomic, psychosocial, and health belief-related factors associated with ≥1 adherence measure. These included nine of the ten factors from Table 1, excluding only REALM (unsuitable for clinic assessment). The instrument (Text Box 1) generated three composite variables (medication, diet, and exercise composites) that indicated the number of risk factors present for NA to the corresponding self-management behavior. At the higher levels of each composite variable, cell sizes were small, so multiple levels were collapsed into one (levels 3–4 for medication composite, 3–5 for diet, and 4–6 for exercise); the lowest two exercise composite levels were collapsed for the same reason. Ultimately, each of the three composite variables yielded four categories, which we labeled “low,” “moderate,” “high,” and “very high” (Table 3) with respect to likelihood of NA. Seven of 636 subjects had insufficient data to determine the medication composite variable, 35 had insufficient data for the diet composite, and 32 had insufficient data for the exercise composite (more subjects were missing for diet/exercise due to missing BMI data).
Table 3.
Unadjusted and Adjusted Odds Ratios and 95 % Confidence Intervals for Associations Between Medication, Diet, and Exercise Composite Variable Levels and Corresponding Hypertension Self-Management Adherence Measures (Medication Non-Adherence, Difficulty Following Diet Recommendations, and Difficulty Following Exercise Recommendations, Respectively)
| Number of risk factors present | N | Unadjusted OR [95 % CI] | Adjusted OR§ [95 % CI] |
|---|---|---|---|
| Medication Composite* | |||
| Low (0 factors) | 157 | 1.0 | 1.0 |
| Moderate (1) | 198 | 1.9 [1.1 to 3.2] | 1.8 [1.1 to 3.2] |
| High (2) | 157 | 5.1 [3.0 to 8.6] | 3.6 [2.0 to 6.6] |
| Very High (≥3) | 117 | 8.1 [4.6 to 14.4] | 4.8 [2.4 to 9.7] |
| Diet Composite† | |||
| Low (0 factors) | 106 | 1.0 | 1.0 |
| Moderate (1) | 145 | 1.9 [0.9 to 3.7] | 1.8 [0.9 to 3.6] |
| High (2) | 155 | 3.9 [2.0 to 7.5] | 4.1 [2.1 to 7.8] |
| Very High (≥3) | 195 | 6.3 [3.3 to 11.8] | 6.1 [3.2 to 11.4] |
| Exercise Composite‡ | |||
| Low (≤1 factors) | 135 | 1.0 | 1.0 |
| Moderate (2) | 131 | 1.9 [1.0 to 3.6] | 1.9 [1.0 to 3.7] |
| High (3) | 160 | 3.9 [2.2 to 6.9] | 4.0 [2.2 to 7.3] |
| Very High (≥4) | 178 | 6.8 [3.9 to 12.1] | 7.4 [4.1 to 13.2] |
Abbreviations: OR odds ratio, CI confidence interval
*Medication composite is a categorical variable reflecting how many of the following self-reported factors are present for a patient: African-American race, completion of < 12 years school, lack of financial security, high stress level
†Diet composite is a categorical variable reflecting how many of the following self-reported factors are present for a patient: BMI ≥ 30, employed, lack of financial security, lack of accomplishment due to psychosocial issues, belief that MI is likely with current lifestyle
‡Exercise composite is a categorical variable reflecting how many of the following self-reported factors are present for a patient: BMI ≥ 30, female gender, completion of < 12 years school, employed, lack of accomplishment due to psychosocial issues, belief that MI is likely with current lifestyle
§Medication composite model adjusted for REALM score < 60 and clinic site. For diet and exercise composite models, no additional effects were included in adjusted model after backward elimination; slight differences in unadjusted vs. adjusted ORs for diet and exercise due to a small reduction in number of observations used in adjusted models
Association Between Adherence Instrument and Adherence Measures
Table 3 presents OR for associations between composite variable levels and corresponding NA measures. As expected, odds for NA were greater for patients with increasing numbers of risk factors. OR were stronger for the composite variables than for any individual factor. Compared to the respective “low” likelihood levels, each “high” and “very high” level was associated with significantly higher odds of NA for each self-management behavior. C-statistics for the three adjusted models ranged from acceptable to good (medication 0.73, diet 0.67, exercise 0.69), and Hosmer–Lemeshow tests were non-significant (p = 0.93 for medication, 1.0 for exercise, 1.0 for diet).
Association Between Adherence Instrument and Baseline Blood Pressure
Mean SBP and DBP were estimated for the levels of each of the three composite variables (Table 4). Patients in the composite variable level representing the highest number of self-management NA risk factors (“very high”) had higher estimated mean SBP and DBP as compared to patients with fewer risk factors.
Table 4.
Systolic and Diastolic Blood Pressure at Baseline Study Assessment According to Medication, Diet, and Exercise Composite Variable Levels
| Number of risk factors present | Mean SBP (SD) | Mean DBP (SD) |
|---|---|---|
| Medication Composite* | ||
| Low (0 factors) | 121.3 (16.2) | 68.4 (10.6) |
| Moderate (1) | 123.5 (14.9) | 70.4 (10.3) |
| High (2) | 127.0 (19.2)§ | 72.3 (10.3)§ |
| Very High (≥3) | 129.4 (18.0)‖ | 75.1 (10.4)‖ |
| Diet Composite† | ||
| Low (0 factors) | 122.9 (17.5) | 67.4 (10.6) |
| Moderate (1) | 124.3 (15.6) | 71.3 (10.3)§ |
| High (2) | 123.2 (15.2) | 70.7 (10.6) |
| Very High (≥3) | 126.9 (19.3) | 73.7 (10.3)¶ |
| Exercise Composite‡ | ||
| Low (≤1 factors) | 124.3 (16.8) | 70.1 (11.0) |
| Moderate (2) | 121.9 (17.1) | 68.6 (10.3) |
| High (3) | 123.9 (15.2) | 72.0 (10.4)# |
| Very High (≥4) | 127.5 (19.3)# | 73.3 (10.7)‖ |
Abbreviations: SBP systolic blood pressure, DBP diastolic blood pressure
*Medication composite is a categorical variable reflecting how many of the following self-reported factors are present for a patient: African-American race, completion of < 12 years school, lack of financial security, high stress level
†Diet composite is a categorical variable reflecting how many of the following self-reported factors are present for a patient: BMI ≥ 30, employed, lack of financial security, lack of accomplishment due to psychosocial issues, belief that MI is likely with current lifestyle
‡Exercise composite is a categorical variable reflecting how many of the following self-reported factors are present for a patient: BMI ≥ 30, female gender, completion of < 12 years school, employed, lack of accomplishment due to psychosocial issues, belief that MI is likely with current lifestyle
§p < 0.05 for comparison with Low (determined by ANOVA, corrected for multiple comparisons using Tukey method)
‖p < 0.05 for comparison with Low and Moderate (determined by ANOVA, corrected for multiple comparisons using Tukey method)
¶p < 0.05 for comparison with Low and High (determined by ANOVA, corrected for multiple comparisons using Tukey method)
#p < 0.05 for comparison with Moderate (determined by ANOVA, corrected for multiple comparisons using Tukey method)
DISCUSSION
Using baseline data from a HTN trial, we identified patient factors associated with measures of NA to medication, diet, and exercise, the three key self-management behaviors in HTN. We also created an instrument that generated three composite variables (medication, diet, and exercise composites), each reflecting the number of risk factors present for NA to the corresponding HTN self-management behavior; these three composites identified subgroups with higher likelihood of medication NA, difficulty following diet recommendations, and difficulty following exercise recommendations, respectively. Composite variable levels representing the highest number of self-management NA risk factors were also associated with higher SBP/DBP. With further study, this instrument could facilitate identification of patients less likely to adhere to HTN self-management.
This study is unique in its identification of factors associated with measures of NA to all of the three key self-management behaviors in HTN. By identifying distinct factors associated with likelihood of NA to recommended medication use, diet, and exercise, this study suggests that adhering to each of these behaviors poses different challenges for patients. For example, lack of financial security and high stress had associations with medication NA. By contrast, a sense of lack of accomplishment due to psychosocial issues and the belief that MI is likely with current lifestyle were not associated with reported medication NA, but each was associated with difficulty following diet and exercise recommendations. Lack of financial security was associated with difficulty following diet recommendations, but not difficulty following exercise recommendations. While there are intriguing possible interpretations for these associations, the cross-sectional design of this study precludes conclusions regarding causation between the patient factors and NA measures examined.
As interventions exist to improve NA to self-management behaviors in HTN, identification of non-adherent individuals is essential to improving BP control and reducing costs. Physicians have difficulty identifying patients with self-management NA,40,41 so a single instrument capable of identifying individuals likely to have NA to different HTN self-management behaviors would be valuable, particularly in light of our findings that distinct factors are associated with NA to each self-management behavior. This instrument could be utilized by clinicians to evaluate one, two, or three of the HTN self-management behaviors for a given patient, and would facilitate appropriate targeting of patient counseling or referral based on the results. While prospective validation will be needed in order to confirm this instrument’s clinical utility, its ability to identify subgroups with high likelihood of NA to single or multiple self-management behaviors distinguishes it from other NA identification aids. Further, this instrument includes only easily assessed factors, making it convenient for clinical use. The apparent positive relationship between this instrument and BP further supports its potential clinical utility.
The current study focuses on self-management NA in HTN, which is highly prevalent in primary care. Because medication, diet, and exercise adherence are also essential to diabetes and hyperlipidemia self-management, it is possible that this instrument could be used to assess medication, diet, and exercise NA in these conditions, as well.
Limitations
Several factors may affect the generalizability of our results, including: 1) the multiple exclusion criteria for the TCYB trial; 2) the particular demographics of our population (mostly female, high unemployment); and particularly, 3) the good baseline BP control in our population. In general, our results generalize to individuals under treatment for hypertension in primary care setting, but should be confirmed in patients with poorer BP control.
Though our results suggest ways in which the identified risk factors may underlie NA to HTN self-management behaviors, prospective study is needed to establish causation and confirm the clinical utility of this instrument. Though the composite variable levels we defined appear to be positively associated with odds of NA to self-management behaviors, the fact that there is overlap between the OR CI for these associations leaves some uncertainty as to whether the “moderate,” “high,” and “very high” levels truly represent different likelihood of NA. Additionally, it should be noted that the patient factors examined were not an exhaustive list of factors known to impact NA, but rather were measures available through the TCYB trial database. Likewise, an item known to impact medication NA, health literacy, was excluded given our focus on clinical usability.
There is no perfect strategy for measuring medication NA. For this analysis, we used a validated self-reported medication adherence measure.36,37 While the degree to which self-report correlates with objective medication adherence is questioned,42,43 it remains the most common strategy for assessing medication NA because it is simple, reliable, and convenient.44–46 For diet and exercise, we used single-item measures assessing patient-reported difficulty in following diet and exercise recommendations. Although the optimal means for assessing diet and exercise adherence is unclear, there is evidence that direct questioning regarding self-management behaviors yields unreliable information.47 Thus, while our use of single-item, self-reported diet and exercise adherence measures remains a limitation, the structure of these measures likely minimizes any social desirability bias that would cause respondents to endorse better diet or exercise than they actually follow, while still capturing the extent to which patients adhere to recommended diet and exercise.
Despite these limitations, we identified risk factors for NA to the three key self-management behaviors in HTN: proper medication use, diet, and exercise. We also explored development of an instrument strongly associated with NA to these behaviors and BP. With further prospective study, this instrument has the potential to improve identification of hypertensive individuals that are less likely to follow medication, diet, and exercise recommendations.
Acknowledgements
The Take Control of Your Blood Pressure study is supported by a NHLBI grant R01 HL070713, a Pfizer Foundation Health Communication Initiative award, and Established Investigator Award from the American Heart Association to the last author, who was also supported by a research career scientist award from the VA Health service research and development (VA HSR&D 08-027). The first author is supported in part by a NIDDK grant R01 DK074672 and HHSA290-2007-10066-I-TO6. The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs or the Agency for Healthcare Research and Quality.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
REFERENCES
- 1.World Health Organization. Adherence to long-term therapies: evidence for action. Noncommunicable Diseases and Mental Health Adherence to long-term therapies project. 2003. http://www.who.int/chp/knowledge/publications/adherence_introduction.pdf. Accessed July 31, 2012.
- 2.Peterson AM, Takiya L, Finley R. Meta-analysis of trials of interventions to improve medication adherence. Am J Health Syst Pharm. 2003;60:657–665. doi: 10.1093/ajhp/60.7.657. [DOI] [PubMed] [Google Scholar]
- 3.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 4.Borzecki AM, Oliveria SA, Berlowitz DR. Barriers to hypertension control. Am Heart J. 2005;149:785–794. doi: 10.1016/j.ahj.2005.01.047. [DOI] [PubMed] [Google Scholar]
- 5.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 6.Siegel D, Lopez J, Meier J. Antihypertensive medication adherence in the Department of Veterans Affairs. Am J Med. 2007;120:26–32. doi: 10.1016/j.amjmed.2006.06.028. [DOI] [PubMed] [Google Scholar]
- 7.Ren XS, Kazis LE, Lee A, Zhang H, Miller DR. Identifying patient and physician characteristics that affect compliance with antihypertensive medications. J Clin Pharm Ther. 2002;27:47–56. doi: 10.1046/j.1365-2710.2002.00387.x. [DOI] [PubMed] [Google Scholar]
- 8.Shea S, Misra D, Ehrlich MH, Field L, Francis CK. Predisposing factors for severe, uncontrolled hypertension in an inner-city minority population. N Engl J Med. 1992;327:776–781. doi: 10.1056/NEJM199209103271107. [DOI] [PubMed] [Google Scholar]
- 9.Francis CK. Hypertension, cardiac disease, and compliance in minority patients. Am J Med. 1991;91:29S–36. doi: 10.1016/0002-9343(91)90060-B. [DOI] [PubMed] [Google Scholar]
- 10.Nabi H, Vahtera J, Singh-Manoux A, Pentti J, Oksanen T, Gimeno D, Elovainio M, Virtanen M, Klaukka T, Kivimaki M. Do psychological attributes matter for adherence to antihypertensive medication? The Finnish Public Sector Cohort Study. J Hypertens. 2008;26:2236–2243. doi: 10.1097/HJH.0b013e32830dfe5f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hassan NB, Hasanah CI, Foong K, Naing L, Awang R, Ismail SB, Ishak A, Yaacob LH, Harmy MY, Daud AH, Shaharom MH, Conroy R, Rahman AR. Identification of psychosocial factors of noncompliance in hypertensive patients. J Hum Hypertens. 2006;20:23–29. doi: 10.1038/sj.jhh.1001930. [DOI] [PubMed] [Google Scholar]
- 12.Wang PS, Bohn RL, Knight E, Glynn RJ, Mogun H, Avorn J. Noncompliance with antihypertensive medications: the impact of depressive symptoms and psychosocial factors. J Gen Intern Med. 2002;17:504–511. doi: 10.1046/j.1525-1497.2002.00406.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Patel RP, Taylor SD. Factors affecting medication adherence in hypertensive patients. Ann Pharmacother. 2002;36:40–45. doi: 10.1345/aph.1A046. [DOI] [PubMed] [Google Scholar]
- 14.Gerber BS, Cho YI, Arozullah AM, Lee SY. Racial differences in medication adherence: A cross-sectional study of Medicare enrollees. Am J Geriatr Pharmacother. 2010;8:136–145. doi: 10.1016/j.amjopharm.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bosworth HB, Powers B, Grubber JM, Thorpe CT, Olsen MK, Orr M, Oddone EZ. Racial differences in blood pressure control: potential explanatory factors. J Gen Intern Med. 2008;23:692–698. doi: 10.1007/s11606-008-0547-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morris AB, Li J, Kroenke K, Bruner-England TE, Young JM, Murray MD. Factors associated with drug adherence and blood pressure control in patients with hypertension. Pharmacotherapy. 2006;26:483–492. doi: 10.1592/phco.26.4.483. [DOI] [PubMed] [Google Scholar]
- 17.Hill MN, Bone LR, Kim MT, Miller DJ, Dennison CR, Levine DM. Barriers to hypertension care and control in young urban black men. Am J Hypertens. 1999;12:951–958. doi: 10.1016/S0895-7061(99)00121-1. [DOI] [PubMed] [Google Scholar]
- 18.Kaplan S, Greenfield S, Ware JE. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. 1989;27:S110–S127. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- 19.Krousel-Wood M, Islam T, Muntner P, Holt E, Joyce C, Morisky DE, Webber LS, Frohlich ED. Association of depression with antihypertensive medication adherence in older adults: cross-sectional and longitudinal findings from CoSMO. Ann Behav Med. 2010;40:248–257. doi: 10.1007/s12160-010-9217-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aggarwal B, Mosca L. Lifestyle and psychosocial risk factors predict non-adherence to medication. Ann Behav Med. 2010;40:228–233. doi: 10.1007/s12160-010-9212-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krousel-Wood MA, Frohlich ED. Hypertension and depression: coexisting barriers to medication adherence. J Clin Hypertens (Greenwich) 2010;12:481–486. doi: 10.1111/j.1751-7176.2010.00302.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eze-Nliam CM, Thombs BD, Lima BB, Smith CG, Ziegelstein RC. The association of depression with adherence to antihypertensive medications: a systematic review. J Hypertens. 2010;28:1785–1795. doi: 10.1097/HJH.0b013e32833b4a6f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bosworth H, Oddone E. A model of psychosocial and cultural antecedents of blood pressure control. J Natl Med Assoc. 2002;94:236–248. [PMC free article] [PubMed] [Google Scholar]
- 24.Kressin NR, Orner MB, Manze M, Glickman ME, Berlowitz D. Understanding contributors to racial disparities in blood pressure control. Circ Cardiovasc Qual Outcomes. 2010;3:173–180. doi: 10.1161/CIRCOUTCOMES.109.860841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zeller A, Taegtmeyer A, Martina B, Battegay E, Tschudi P. Physicians’ ability to predict patients’ adherence to antihypertensive medication in primary care. Hypertens Res. 2008;31:1765–1771. doi: 10.1291/hypres.31.1765. [DOI] [PubMed] [Google Scholar]
- 26.McHorney CA. The Adherence Estimator: A brief, proximal screener for patient propensity to adhere to prescription medications for chronic disease. Curr Med Res Opin. 2009;25:215–238. doi: 10.1185/03007990802619425. [DOI] [PubMed] [Google Scholar]
- 27.Zeller A, Schroeder K, Peters TJ. An adherence self-report questionnaire facilitated the differentiation between non-adherence and nonresponse to antihypertensive treatment. J Clin Epidemiol. 2008;61:282–288. doi: 10.1016/j.jclinepi.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 28.Schoberberger R, Janda M, Pescosta W, Sonneck G. The COMpliance Praxis Survey (COMPASS): A multidimensional instrument to monitor compliance for patients on antihypertensive medication. J Hum Hypertens. 2002;16:779–787. doi: 10.1038/sj.jhh.1001479. [DOI] [PubMed] [Google Scholar]
- 29.Girerd X, Hanon O, Anagnostopoulos K, Ciupek C, Mourad JJ, Consoli S. Assessment of antihypertensive compliance using a self-administered questionnaire: Development and use in a hypertension clinic [in French] Presse Med. 2001;30:1044–1048. [PubMed] [Google Scholar]
- 30.Kim MT, Hill MN, Bone LR, Levine DM. Development and testing of the Hill-Bone Compliance to High Blood Pressure Therapy Scale. Prog Cardiovasc Nurs. 2000;15:90–96. doi: 10.1111/j.1751-7117.2000.tb00211.x. [DOI] [PubMed] [Google Scholar]
- 31.Bosworth HB, Olsen MK, Grubber JM, Neary AM, Orr MM, Powers BJ, Adams MB, Svetkey LP, Reed SD, Li Y, Dolor RJ, Oddone EZ. Two Self-management Interventions to Improve Hypertension Control: A Randomized Trial. Ann Intern Med. 2009;151:687–695. doi: 10.1059/0003-4819-151-10-200911170-00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Williams RB, Barefoot JC, Califf RM, Haney TL, Saunders WB, Pryor DB, Hlatky MA, Siegler IC, Mark DB. Prognostic importance of social and economic resources among medically treated patients with angiographically documented coronary artery disease. JAMA. 1992;267:520–524. doi: 10.1001/jama.1992.03480040068032. [DOI] [PubMed] [Google Scholar]
- 33.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: A new instrument for measuring patients’ literacy skills. J Gen Intern Med. 1995;10:537–541. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 34.Jette AM, Cummings KM, Brock BM, Phelps MC, Naessens J. The structure and reliability of health belief indices. Health Serv Res. 1981;16:81–98. [PMC free article] [PubMed] [Google Scholar]
- 35.Bosworth HB, Olsen MK, Neary A, Orr M, Grubber J, Svetkey L, Adams M, Oddone EZ. Take Control of Your Blood pressure (TCYB) study: A multifactorial tailored behavioral and educational intervention for achieving blood pressure control. Patient Educ Couns. 2008;70:338–347. doi: 10.1016/j.pec.2007.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, Bullinger M, Kaasa S, Leplege A, Prieto L, Sullivan M. Cross-validation of item selection and scoring for the SF-12 health survey in nine countries: Results from the IQOLA project. J Clin Epidemiol. 1998;51:1171–1178. doi: 10.1016/S0895-4356(98)00109-7. [DOI] [PubMed] [Google Scholar]
- 37.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 38.Lowry KP, Dudley TK, Oddone EZ, Bosworth HB. Intentional and unintentional non-adherence to antihypertensive medication. Ann Pharmacother. 2005;39:1198–1203. doi: 10.1345/aph.1E594. [DOI] [PubMed] [Google Scholar]
- 39.Allison PD. Logistic Regression Using the SAS System: Theory and Application. Cary, NC: SAS Institute Inc; 1999. pp. 49–50. [Google Scholar]
- 40.Svarstad BL, Chewning BA, Sleath BL, Claesson C. The Brief Medication Questionnaire: A tool for screening patient adherence and barriers to adherence. Patient Educ Couns. 1999;37:113–124. doi: 10.1016/S0738-3991(98)00107-4. [DOI] [PubMed] [Google Scholar]
- 41.Copher R, Buzinec P, Zarotsky V, Kazis L, Iqbal SU, Macarios D. Physician perception of patient adherence compared to patient adherence of osteoporosis medications from pharmacy claims. Curr Med Res Opin. 2010;26:777–785. doi: 10.1185/03007990903579171. [DOI] [PubMed] [Google Scholar]
- 42.Voils CI, Hoyle RH, Thorpe CT, Maciejewski ML, Yancy WS., Jr Improving the measurement of self-reported medication non-adherence. J Clin Epidemiol. 2011;64:250–254. doi: 10.1016/j.jclinepi.2010.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang PS, Benner JS, Glynn RJ, Winkelmayer WC, Mogun H, Avorn J. How well do patients report noncompliance with antihypertensive medications?: a comparison of self-report versus filled prescriptions. Pharmacoepidemiol Drug Saf. 2004;13:11–19. doi: 10.1002/pds.819. [DOI] [PubMed] [Google Scholar]
- 44.Feinstein A. Compliance bias and the interpretation of therapeutic trials. In: Haynes RB, Taylor DW, Sackeets DL, editors. Compliance in health care. Baltimore, M.D: The Johns Hopkins University Press; 1979. pp. 309–322. [Google Scholar]
- 45.Schroeder K, Fahey T, Hay AD, Montgomery A, Peters TJ. Adherence to antihypertensive medication assessed by self-report was associated with electronic monitoring compliance. J Clin Epidemiol. 2006;59:650–651. doi: 10.1016/j.jclinepi.2005.10.013. [DOI] [PubMed] [Google Scholar]
- 46.Morisky DE, DiMatteo MR. Improving the measurement of self-reported medication non-adherence: response to authors. J Clin Epidemiol. 2011;64:255–257. doi: 10.1016/j.jclinepi.2010.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cramer JA. Microelectronic systems for monitoring and enhancing patient compliance with medication regimens. Drugs. 1995;49:321–327. doi: 10.2165/00003495-199549030-00001. [DOI] [PubMed] [Google Scholar]