ABSTRACT
BACKGROUND
Primary care patients with Panic Disorder (PD) and Generalized Anxiety Disorder (GAD) experience poorer than expected clinical outcomes, despite the availability of efficacious pharmacologic and non-pharmacologic treatments. A barrier to recovery from PD/GAD may be the co-occurrence of pain.
OBJECTIVE
To evaluate whether pain intensity interfered with treatment response for PD and/or GAD in primary care patients who had received collaborative care for anxiety disorders.
DESIGN
A secondary data analysis of a randomized, controlled effectiveness trial comparing a telephone-delivered collaborative care intervention for primary care patients with severe PD and/or GAD to their doctor’s “usual” care.
PARTICIPANTS
Patients had to have a diagnosis of PD and/or GAD and a severe level of anxiety symptoms. The 124 patients randomized at baseline to the collaborative care intervention were analyzed. Participants were divided into two pain intensity groups based on their response to the SF-36 Bodily Pain scale (none or mild pain vs. at least moderate pain).
MAIN MEASURES
Pain was assessed using the Bodily Pain scale of the SF-36. Anxiety symptoms were measured with the Hamilton Anxiety Rating Scale (HRS-A), Panic Disorder Severity Scale (PDSS) and Generalized Anxiety Disorder Severity Scale (GADSS). Measures were collected over 12 months.
KEY RESULTS
At baseline, patients with at least moderate pain were significantly more likely to endorse more anxiety symptoms on the HRS-A than patients with no pain or mild pain (P < .001). Among patients with severe anxiety symptoms, 65 % (80/124) endorsed experiencing at least moderate pain in the previous month. A significantly lesser number of patients achieved a 50 % improvement at 12 months on the HRS-A and GADSS if they had at least moderate pain as compared to patients with little or no pain (P = 0.01 and P = 0.04, respectively).
CONCLUSIONS
Coexisting pain was common in a sample of primary care patients with severe PD/GAD, and appeared to negatively affect response to anxiety treatment.
KEY WORDS: panic disorder, generalized anxiety disorder, pain, collaborative care, clinical trial
INTRODUCTION
Anxiety disorders are highly prevalent in the primary care setting. Approximately 12–22 % of primary care patients present to physicians with symptoms of distress related to anxiety.3–5 Among the anxiety disorders commonly encountered in primary care, panic disorder (PD) and generalized anxiety disorder (GAD) create the largest burden of morbidity and have a similar adverse impact on self-reported quality of life.1,2 They have a median point prevalence of 4–6 %6–9 and 5–19 %9–11 respectively, and are often chronic in nature. Likewise, the prevalence of chronic pain is common in primary care, with estimates that approximately 10 % of Americans have experienced chronic non-cancer pain in the previous 12 months.12 Pain and anxiety disorders often coexist, and in a nationally representative sample, individuals with chronic pain were more likely to have any anxiety disorder than those without pain (35 % vs. 18 %).13 In an international survey, persons with back or neck pain were more than twice as likely to have an anxiety disorder as those without pain.14 These studies did not distinguish between mild and severe anxiety symptoms.
Unfortunately, primary care patients with PD and GAD experience poorer than expected clinical outcomes, despite the availability of efficacious pharmacologic and non-pharmacologic treatments that primary care providers (PCP) can provide.15–20 A variety of explanations for this include PCPs’ unfamiliarity with guideline-based treatments used in specialty care settings,21 patient resistance to a psychiatric diagnosis,22,23 and insufficient patient adherence to treatment recommendations. However, an additional barrier to recovery from PD/GAD may be the co-occurrence of pain. This finding has been well-described in depressed patients, as they are less likely to respond to treatment if they have comorbid pain, but has not been well-studied in patients with PD and/or GAD.24–26 To evaluate whether pain intensity interfered with recovery from comorbid PD and/or GAD, we studied primary care patients who had participated in a trial of collaborative care (CC) for anxiety disorders.27 Our objective was to describe the prevalence of comorbid pain among study participants with PD and/or GAD, and to determine the impact of pain on our CC intervention. Our primary hypothesis was that patients with PD and/or GAD and at least moderate pain were significantly less likely to respond to the CC intervention than patients with PD and/or GAD and mild or no pain.
METHODS
We performed a secondary data analysis on the Reduce Limitations from Anxiety (RELAX) Trial: a randomized, controlled effectiveness trial comparing a telephone-delivered CC intervention for primary care patients with PD and/or GAD to their doctor’s “usual” care.27 Trained care managers delivered an intervention for anxiety. Outcome measures were obtained from January 2005—December 2008. The study was approved by the University of Pittsburgh Institutional Review Board, and all patients provided written informed consent.
Participants
The trial recruited from six primary care practices within the University of Pittsburgh Medical Center.28 If patients had: a Primary Care Evaluation of Mental Disorders (PRIME-MD)1 diagnosis of PD and/or GAD and severe anxiety symptoms, defined as a Panic Disorder Severity Scale (PDSS)29 score ≥ 14 or a Hamilton Anxiety Rating Scale (HRS-A)30 score ≥ 20 respectively; medical stability; life expectancy > 1 year; no active suicidality; no history of bipolar disorder, alcohol dependence or substance abuse; were not in treatment with a mental health specialist (MHS); were English speaking; had no communication barrier, and owned a household telephone, they were randomized to either a telephone-delivered CC intervention or their PCPs’ “usual care” for anxiety.33 These analyses focused on the patients randomized at baseline to the CC intervention (n = 124).
Procedures
Collaborative Care Intervention
The intervention lasted for 12 months and consisted of several components.
Patients randomized to CC were initially contacted by a care manager via telephone to review treatment options of guided education (bibliotherapy), pharmacotherapy, referral to a MHS, or some combination thereof. CC was directed toward treatment of anxiety and pain treatment information was not collected (such as participation in physical therapy or injections).
When a patient selected bibliotherapy, a workbook for either managing PD31 or GAD32 (depending on their diagnosis or preference if they had both conditions) was mailed to them. If the patient agreed to pharmacotherapy, the care manager reviewed the patient’s past anxiolytic medications.
At weekly case review meetings with the clinical team (made-up of a general internist, psychiatrist, and psychologist), the care manager presented all newly enrolled patients. For all other patients, they presented the patient’s progress. The clinical team would then make recommendations based on the patient’s treatment response.33 Additionally, if the patient’s symptoms were not improving, they needed additional psychiatric support, or if they voiced interest in seeing a MHS, the care manager facilitated appointments to a MHS. The PCP was informed about the recommended changes via the electronic medical record (EMR). All medications were prescribed by the PCP.
Patients were initially contacted every 2 weeks for the acute phase of treatment, which included assessing for symptom development, medication side effects (if indicated), following up on a recommendation to see a MHS (if made), and review of the workbook. The acute phase usually lasted 4 months.
The acute phase of treatment concluded when the patient’s anxiety symptoms improved to at least mild severity. The patient then entered the continuation phase of treatment, during which the care manager typically contacted the patient once a month. Should the patient’s symptoms relapse, he or she would return to the acute phase of treatment.
Measures
The diagnoses for the clinical trial were abstracted by trained study nurses from the problem list of the EMR, and assigned a category based on a systems approach if the condition had persisted over at least 6 months. NEM reviewed each patient’s list of potentially painful and chronic conditions to confirm the accuracy of the nurse-led chart abstractions, as well as to additionally classify the patient as having a painful condition. The painful conditions fell into the following categories: musculoskeletal, gastrointestinal, genitourinary, neurological/sensory, migraine/chronic headaches, and chronic pain syndrome. In addition to sociodemographic information, the following measures were obtained at baseline, 2, 4, 8, and 12 months by a trained assessor blinded to treatment assignment. The Panic Disorder Severity Scale29 and Generalized Anxiety Disorder Severity Scale34 were only administered to patients with PD or GAD, respectively.
Medical OutcomesStudy 36-ItemShort FormHealth Survey(SF-36): Pain was assessed using the Bodily Pain scale of the widely used SF-36.35 Higher scores indicate better health related quality of life and less bodily pain. The Mental Component Summary (MCS) score was also reported.
Primary CareEvaluation ofMental Disorders(PRIME-MD) PatientHealth Questionnaire(PHQ): The Anxiety and Mood Modules were administered to patients to establish the diagnoses of PD, GAD, and major depression.36 It has a sensitivity of 57 % and a specificity of 97–99 % for both PD and GAD, compared to the “gold standard” of a MHS’s clinical interview (sensitivity 69 %, specificity 82 % for depression).36
Hamilton RatingScale forAnxiety (HRS-A): This scale measures the subjective severity of anxiety symptoms within the preceding 7 days.30 It has long been used as an indicator for anxiolytic efficacy in PD37 and GAD.38 The parent study adopted Bech’s convention, wherein total HRS-A scores of 20+ indicate severe anxiety.37 Lower scores are better.
Panic DisorderSeverity Scale(PDSS): This scale assesses the overall severity of panic symptoms.29,39 It has been used as an outcome measure in other clinical trials of treatments for PD,40 including those in primary care settings.16,27,33 Lower scores are better.
Generalized AnxietyDisorder SeverityScale (GADSS): This scale assesses the severity of GAD symptoms. It has been shown to have high internal consistency, validity, and sensitivity to change.34 Lower scores are better.
Patient HealthQuestionnaire (PHQ-9): This is a brief measure of depressive severity.41 Higher scores are associated with worse functional status and higher levels of health service costs by primary care patients.41 Lower scores are better.
Statistical Analyses
We divided patients into two pain intensity groups by their answer to the following question on the SF-36 Bodily Pain scale at baseline: “How much bodily pain have you had during the past week?” If patients answered none, very mild, or mild, they were considered to be in the “no pain” group, and if they answered moderate, severe, or very severe they were considered to be in the “pain” group.
Baseline sociodemographics and clinical characteristics were compared between the two pain groups, using t-tests for continuous variables and chi-squared tests for categorical variables. Chi-squared tests were performed to test the proportions of patients achieving a 50 % decline from baseline levels in HRS-A, GADSS and PDSS at 12 months between the intervention patients with pain and the intervention patients without pain. Repeated measures mixed-effect models were run for intervention group subjects to calculate the changes in scores (HRS-A, SF-36 MCS, GADSS and PDSS) from baseline and effect sizes of score changes between the two pain groups. Baseline pain status, time and their interaction were included in the models. Subject intercepts were treated as random effects, and time was treated as categorical fixed effect. Models controlled for age, gender, race, marital status, working status, comorbid conditions (≥2 or <2), and baseline PHQ-9 scores. Inferences were based on restricted maximum likelihood method with missing-at-random and unstructured covariance matrix assumptions. Cohen’s d was used to calculate the effect sizes, based on estimates from mixed models. P-values were 2-tailed with significance level of 0.05. All analyses for the PDSS and GADSS were only for subjects with PD diagnosis and GAD diagnosis at baseline, respectively. Analyses were done using SAS software, version 9.2 (SAS Institute Inc, Cary, North Carolina).
RESULTS
The baseline sociodemographic and clinical characteristics of the sample are presented in Table 1. This sample was predominantly white and well educated. Patients with pain were significantly more likely to be older, single, and unemployed. In addition to a diagnosis of GAD or PD/GAD, a large proportion had comorbid major depression: 93 % (74/80) in the pain group and 84 % (37/44) in the no pain group. At baseline, patients with pain were significantly more likely to endorse more anxiety symptoms on the HRS-A (30.1 vs. 25.4, P < .001). As expected, they were also more likely to endorse significantly more pain on the SF-36 Bodily Pain scale (32.5 vs. 50.4, P < .0001). Patients with pain were significantly more likely to be on a nonsteroidal anti-inflammatory drug (NSAID) or an opioid, and carry a chronic pain diagnosis. The most common pain diagnosis was a musculoskeletal condition (such as chronic low back pain) and occurred in 59 % (47/80) of the intervention patients with pain, but there was no difference between groups in anxiolytic medication use at baseline. Among the patients with severe anxiety symptoms 65 % (80/124) endorsed experiencing at least moderate pain in the previous month.
Table 1.
Baseline Sociodemographic and Clinical Characteristics
| Characteristics | Intervention patients with pain (n = 80) | Intervention patients without pain (n = 44) | Usual care patients with pain (n = 78) | P* |
|---|---|---|---|---|
| Age, mean (SD) | 47.5 (8.3) | 40.3 (12.3) | 45.4 (11.8) | <.001 |
| Female n,(%) | 59 (74) | 32 (73) | 60 (77) | 0.90 |
| Caucasian n,(%) | 59 (74) | 37 (84) | 57 (73) | 0.19 |
| >High school education n,(%) | 55 (69) | 29 (66) | 51 (65) | 0.75 |
| Married n, (%) | 36 (45) | 23 (52) | 33 (42) | 0.44 |
| Working, part-time/full time n,(%) | 37 (46) | 34 (77) | 34 (44) | <.001 |
| Prime-MD diagnosis n,(%) | ||||
| GAD | 37 (46) | 20 (45) | 27 (35) | 0.24 |
| PD | 1 (1) | 3 (7) | 7 (9) | |
| PD/GAD | 42 (53) | 21 (48) | 44 (56) | |
| Major depression n,(%) | 74 (93) | 37 (84) | 75 (96) | 0.14 |
| Anxiety comorbidity, mean n,(SD) | 0.8 (1.1) | 0.8 (0.9) | 0.7 (0.8) | 0.92 |
| †Comorbid conditions ≥ 2 n,(%) | n = 78 | n = 42 | n = 76 | <.001 |
| 41 (53) | 8 (19) | 32 (42) | ||
| ‡Chronic pain diagnoses n,(%) | 55 (69) | 12 (27) | 52 (67) | <.0001 |
| Measures, mean (SD) | ||||
| SF-36 bodily pain | 32.5 (6.1) | 50.4 (6.6) | 33.1 (6.4) | <.0001 |
| HRS-A | 30.1 (6.9) | 25.4 (7.1) | 29.4 (7.0) | <.001 |
| PDSS, N | 16.6 (4.9) 43 | 16.3 (3.7) 24 | 15.9 (4.5) 51 | 0.78 |
| GADSS, N | 16.2 (2.9) 79 | 15.3 (3.4) 41 | 16.7 (2.5) 71 | 0.13 |
| SF-36 MCS | 28.1 (10.1) | 26.1 (11.3) | 27.4 (8.8) | 0.33 |
| PHQ-9 | 16.0 (4.8) | 13.9 (5.5) | 16.4 (4.8) | 0.045 |
| Anxiolytics n,(%) | n = 79 | n = 41 | n = 70 | |
| SSRI | 23 (29) | 6 (15) | 25 (36) | 0.08 |
| SNRI | 8 (10) | 1 (2) | 6 (9) | 0.13 |
| Other anxiolytics | 12 (15) | 4 (10) | 8 (11) | 0.41 |
| Tricyclic | 2 (3) | 0 | 0 | 0.30 |
| Benzodiazepine | 26 (33) | 8 (20) | 15 (21) | 0.12 |
| Pain medications n,(%) | ||||
| NSAIDS | 22 (28) | 1 (2) | 26 (33) | <.001 |
| Opioids | 34 (43) | 4 (9) | 26 (33) | <.001 |
| Acetaminophen | 4 (5) | 0 | 4 (5) | 0.13 |
| Other | 30 (38) | 2 (5) | 21 (27) | <.0001 |
Prime-MD Primary Care Evaluation of Mental Disorders, GAD Generalized Anxiety Disorder, PD Panic Disorder, GADSS Generalized Anxiety Disorder Severity Scale, range 0–24, HRS-A Hamilton Rating Scale for Anxiety, range 0–56, PDSS Panic Disorder Severity Scale, range 0–28, PHQ-9 Patient Health Questionnaire 9, range 0–27; SF-36 BodilyPain range 0–100, SF-36 MCS Short Form-36 Mental Component Summary, range 0–100, SSRI Selective Serotonin Reuptake Inhibitor, SNRI Serotonin Norepinephrine Reuptake Inhibitor, NSAID Nonsteroidal Anti-inflammatory Drug
*Intervention patients with pain vs. intervention patients without pain
†Cardiovascular Disease, Diabetes, Neurologic Disease, Pulmonary Disease, Gastrointestinal Disease
‡Any painful condition in the following areas: musculoskeletal, gastrointestinal, genitourinary, neurological/sensory, migraine/chronic headaches, or chronic pain syndrome
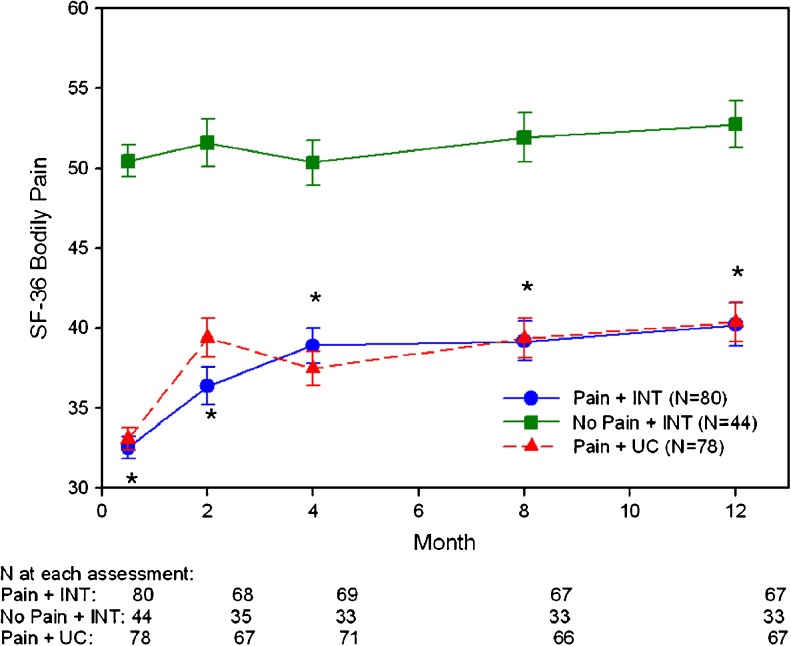
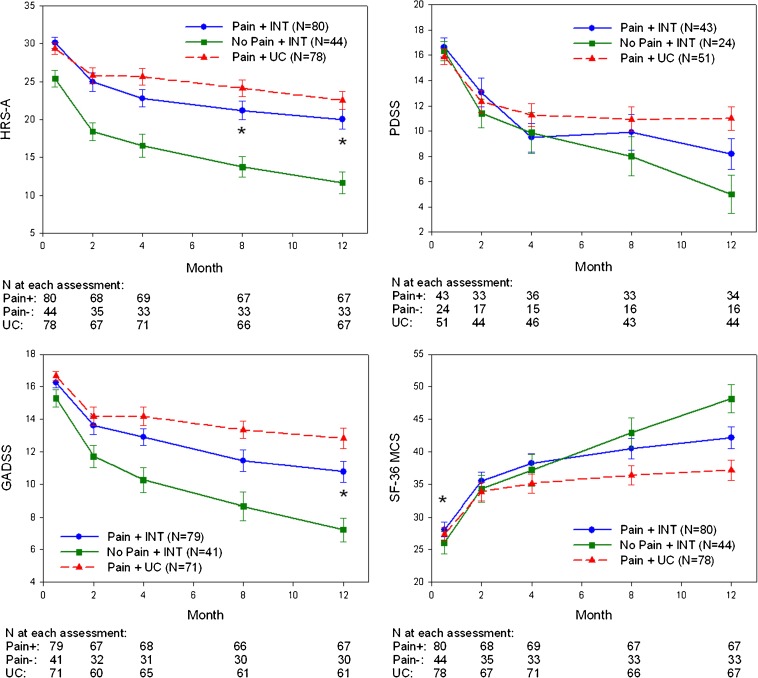
Figure 1 presents the mean scores over time on the SF-36 Bodily Pain scale. The patients with pain assigned to the intervention had significantly more pain at baseline and each subsequent time point on the SF-36 Bodily Pain scale than intervention patients without pain. These results suggest that patients’ pain was chronic in duration, since mean scores on this scale remained low throughout the duration of the study. Figure 2 presents the mean scores for the HRS-A, PDSS, GADSS, and SF-36 MCS for the pain and no pain groups. The differences between mean scores of the two groups for HRS-A were significant at 8 months and 12 months and were also significant at 12 months for the GADSS (P < 0.05). The PDSS and SF-36 MCS were nonsignificant throughout the 12-month follow-up period. The mean scores of the usual care group with pain are included for comparison purposes.
Figure 1.
Mean pain scores on the SF-36 Bodily Pain scale over 12 months. *Intervention patients with pain vs. intervention patients without pain, P < .0001. Bars indicate standard error. Higher scores indicate less pain. Controls for age, gender, race, marital status, working status, baseline PHQ-9 score, and comorbid conditions.
Figure 2.
Mean scores on mental health measures over 12 months. *Intervention patients with pain vs. intervention patients without pain, P < .05. Bars indicate standard error. Controls for age, gender, race, marital status, working status, baseline PHQ-9 score, and comorbid conditions. HRS-A = Hamilton Rating scale for Anxiety, lower scores better. PDSS = Panic Disorder Severity Scale, lower scores better. GADSS = Generalized Anxiety Disorder, lower scores better. SF-36 MCS = Short Form-36 Mental Component Summary, higher scores better.
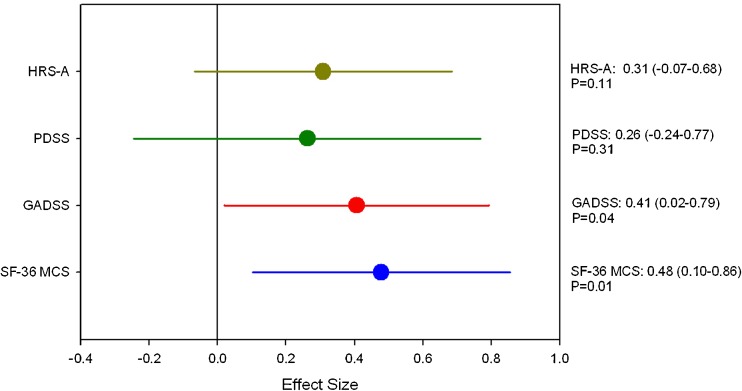
To better understand the effects of the intervention, we determined the proportion of patients who had achieved a significant treatment response. Criteria employed by Barlow40 and Roy-Byrne16 have defined this as a 40 % improvement in the PDSS from baseline. We employed a stricter definition of 50 % improvement, and also applied this to the HRS-A and GADSS. Table 2 presents these results. A significantly lesser number of patients achieved response on the HRS-A and GADSS in the pain group vs. the no pain group (P = 0.01 and P = 0.04, respectively). The PDSS did not show a significant difference between groups, which may partially be due to the small sample size. Effects sizes are also presented as another measure of clinically meaningful change, see Figure 3. All measures had at least a small effect size and the SF-36 MCS had a medium effect size.
Table 2.
Proportions Achieving 50 % Decline from Baseline Levels of Anxiety at 12-Month Follow-up
| Intervention patients with pain (n = 80) | Intervention patients without pain (n = 44) | Usual care patients with pain (n = 78) | P- Value* | |
|---|---|---|---|---|
| HRS-A | 36 % (24) n = 67 | 63 % (20) n = 32 | 23 % (15) n = 66 | 0.01 |
| PDSS | 67 % (22) n = 33 (PD cohort) | 75 % (12) n = 16 (PD cohort) | 21 % (9) n = 43 (PD cohort) | 0.55 |
| GADSS | 34 % (23) n = 67 (GAD cohort) | 57 % (17) n = 30 (GAD cohort) | 18 % (11) n = 60 (GAD cohort) | 0.04 |
*Intervention patients with pain vs. Intervention patients without pain
HRS-A Hamilton Rating Scale for Anxiety, PDSS Panic Disorder Severity, GADSS Generalized Anxiety Disorder Severity Scale
Figure 3.
Effect sizes of change scores from baseline to 12 months between the intervention patients with pain and the intervention patients without pain. Controls for age, gender, race, marital status, working status, baseline PHQ-9 score, and comorbid conditions. Bars indicate standard error. HRS-A = Hamilton Rating scale for Anxiety; PDSS = Panic Disorder Severity Scale; GADSS = Generalized Anxiety Disorder; SF-36 MCS = Short Form-36 Mental Component Summary; PHQ-9 = Patient Health Questionnaire-9.
To determine whether the no pain group may simply have participated more in the CC intervention than the pain group, we looked at the number of calls, medication change recommendations, portions of workbook completed, and MHS visits and found no significant differences between groups (P = 0.21, 0.23, 0.68, 0.20 respectively).
DISCUSSION
This is the first study to investigate the impact of comorbid pain on treatment response to CC for primary care patients with severely symptomatic PD or GAD. We found nearly 2/3 of primary care patients with severely symptomatic PD and GAD were experiencing at least a moderate level of pain, and patients who endorsed at least moderate pain at baseline were less likely to achieve a treatment response as compared to patients without pain, even though both groups received the same CC intervention. This finding was true even after controlling for baseline characteristics, and could not be explained by one group receiving more attention—such as phone calls or medication changes—than the other.
There was a high prevalence of severe anxiety and pain in our sample as compared to a general population. Data from the National Comorbidity Survey of the general US population showed 7 % had chronic pain and GAD and 6.5 % had chronic pain and PD with or without agoraphobia.13 Another international survey of mental disorders among persons with chronic back or neck pain found 9 % of Americans had GAD and 6 % had PD.14 Since our sample comprised patients recruited from primary care practices, the large proportion of patients with severe anxiety who reported at least moderate pain (65 %) could reflect how common these conditions are in a primary care setting and underscore how common it is for patients to present to their PCPs with both mental health conditions and pain. Our findings indicate that patients with severe anxiety symptoms have a much higher prevalence of chronic pain than the general population and suggest that they have more painful conditions than patients with mild or moderate anxiety. Patients with anxiety disorders should be evaluated for painful conditions. Our sample also suggests how common severe anxiety is in primary care, as of 1,331 patients referred to the parent study, 19 % (250/1,331) were severely symptomatic.
Patients with at least moderate pain were less likely to have a clinically meaningful response to CC than those with no or mild pain. This could not be explained by a difference in participation in CC since process measures such as number of calls and medication recommendations were not different between the groups. Previous work has shown a decreased response to pain treatment when an anxiety disorder is present,42 but our findings also suggest that the presence of pain interferes with response to anxiety treatment. Earlier work we have done in patients with less severe symptoms of GAD and/or PD found that pain interference was associated with a lower response to anxiety treatment (whether CC or usual care).43 Our current study is distinct from the previous one, as this study is a different cohort of primary care patients with more severe anxiety symptoms, who were identified as having an anxiety disorder by their PCP and then referred to the study instead of waiting-room screened;28 in addition, this study included more men and African Americans, grouped patients by pain intensity, and analysis was restricted to patients randomized to CC.
One possible explanation for our findings is that moderate pain and severe anxiety are mutually exacerbating. For example, fear of both pain and physical activity is thought to play a role in the maintenance of chronic pain,44 but the presence of pain-induced fear may also make anxiety disorders recalcitrant to treatment since fear fuels anxiety.45 Catastrophizing is also another well-described response to chronic pain 46 which may contribute to the maintenance of anxiety symptoms and vice versa. While theoretical models have focused on the role of anxiety as a risk factor for chronic pain,47 less work has focused on the role of pain in maintaining anxiety. There could also be a role of anxiety-induced muscle tension in maintaining chronic musculoskeletal pain.
Our study has several limitations. First, the sample is predominantly made up of well-educated, white women, limiting generalizability. Second, our measure to assess pain, the SF-36 Bodily Pain scale, does not assess for the cognitive and affective dimensions of pain, such as the McGill Pain Questionnaire48 or the Multidimensional Pain Inventory.49 Third, we could not distinguish whether patients had chronic pain, and since the painful conditions were obtained from chart abstraction, it could not be determined how clinically significant the conditions were. However, since the pain group had consistently high pain scores throughout the 12-month period, was more likely to have a pain medication prescribed such as an NSAID or opioid, and was more likely to have a chronic pain diagnosis, the sample likely represents patients with clinically significant chronic pain. Fourth, we did not have information on pain treatments such as physical therapy, as the intent of the CC intervention was directed towards anxiety treatment and not pain treatment.
In conclusion, we found the presence of pain to be common in a sample of primary care patients with severe PD/GAD. Comorbid pain also resulted in fewer patients responding to a CC intervention for anxiety as compared to patients with mild or no pain. It is important for PCPs to remember that these conditions are commonly comorbid, and the response to anxiety treatment may be hampered by the presence of pain. More research is needed to evaluate if treatment of pain in addition to anxiety would improve anxiety outcomes.
Acknowledgments
All work described was supported by a grant from the National Institute of Mental Health (R01 MH59395). The funding source had no role in the design, conduct, or reporting of our study, or in the preparation, review, or decision to submit this manuscript for publication. The contents do not represent the views of the Department of Veterans Affairs or the United States Government.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
REFERENCES
- 1.Spitzer RL, Kroenke K, Linzer M, et al. Health-related quality of life in primary care patients with mental disorders. Results from the PRIME-MD 1000 Study. JAMA. 1995;274(19):1511–7. doi: 10.1001/jama.1995.03530190025030. [DOI] [PubMed] [Google Scholar]
- 2.Massion AO, Warshaw MG, Keller MB. Quality of life and psychiatric morbidity in panic disorder and generalized anxiety disorder. Am J Psychiatry. 1993;150(4):600–7. doi: 10.1176/ajp.150.4.600. [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Demler O, Frank RG, et al. Prevalence and treatment of mental disorders, 1990 to 2003. N Engl J Med. 2005;352(24):2515–23. doi: 10.1056/NEJMsa043266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Regier DA, Boyd JH, Burke JD, Jr, et al. One-month prevalence of mental disorders in the United States. Based on five epidemiologic catchment area sites. Arch Gen Psychiatry. 1988;45(11):977–86. doi: 10.1001/archpsyc.1988.01800350011002. [DOI] [PubMed] [Google Scholar]
- 5.Leon AC, Portera L, Weissman MM. The social costs of anxiety disorders. Br J Psychiatry Suppl. 1995;27:19–22. [PubMed] [Google Scholar]
- 6.Leon AC, Olfson M, Broadhead WE, et al. Prevalence of mental disorders in primary care. Implications for screening. Arch Fam Med. 1995;4(10):857–61. doi: 10.1001/archfami.4.10.857. [DOI] [PubMed] [Google Scholar]
- 7.Shear MK, Schulberg HC. Anxiety disorders in primary care. Bull Menninger Clin. 1995;59(2 Suppl A):A73–85. [PubMed] [Google Scholar]
- 8.Tiemens BG, Ormel J, Simon GE. Occurrence, recognition, and outcome of psychological disorders in primary care. Am J Psychiatry. 1996;153(5):636–44. doi: 10.1176/ajp.153.5.636. [DOI] [PubMed] [Google Scholar]
- 9.Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 10.Wittchen HU, Zhao S, Kessler RC, Eaton WW. DSM-III-R generalized anxiety disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(5):355–64. doi: 10.1001/archpsyc.1994.03950050015002. [DOI] [PubMed] [Google Scholar]
- 11.Sherbourne CD, Jackson CA, Meredith LS, Camp P, Wells KB. Prevalence of comorbid anxiety disorders in primary care outpatients. Arch Fam Med. 1996;5(1):27–34. doi: 10.1001/archfami.5.1.27. [DOI] [PubMed] [Google Scholar]
- 12.Verhaak PF, Kerssens JJ, Dekker J, Sorbi MJ, Bensing JM. Prevalence of chronic benign pain disorder among adults: a review of the literature. Pain. 1998;77(3):231–9. doi: 10.1016/S0304-3959(98)00117-1. [DOI] [PubMed] [Google Scholar]
- 13.McWilliams LA, Cox BJ, Enns MW. Mood and anxiety disorders associated with chronic pain: an examination in a nationally representative sample. Pain. 2003;106(1–2):127–33. doi: 10.1016/S0304-3959(03)00301-4. [DOI] [PubMed] [Google Scholar]
- 14.Demyttenaere K, Bruffaerts R, Lee S, et al. Mental disorders among persons with chronic back or neck pain: results from the World Mental Health Surveys. Pain. 2007;129(3):332–42. doi: 10.1016/j.pain.2007.01.022. [DOI] [PubMed] [Google Scholar]
- 15.Gorman JM. Treatment of generalized anxiety disorder. J Clin Psychiatry. 2002;63(Suppl 8):17–23. [PubMed] [Google Scholar]
- 16.Roy-Byrne PP, Katon W, Cowley DS, Russo J. A randomized effectiveness trial of collaborative care for patients with panic disorder in primary care. Arch Gen Psychiatry. 2001;58(9):869–76. doi: 10.1001/archpsyc.58.9.869. [DOI] [PubMed] [Google Scholar]
- 17.Katz IR, Reynolds CF, Alexopoulos GS, Hackett D. Venlafaxine ER as a treatment for generalized anxiety disorder in older adults: pooled analysis of five randomized placebo-controlled clinical trials. J Am Geriatr Soc. 2002;50(1):18–25. doi: 10.1046/j.1532-5415.2002.50003.x. [DOI] [PubMed] [Google Scholar]
- 18.Barlow DH, Gorman JM, Shear MK, Woods SW. Cognitive-behavioral therapy, imipramine, or their combination for panic disorder—a randomized controlled trial. JAMA. 2000;283(19):2529–36. doi: 10.1001/jama.283.19.2529. [DOI] [PubMed] [Google Scholar]
- 19.Schweizer E, Rickels K, Lydiard, et al. Strategies for treatment of generalized anxiety in the primary care setting. J Clin Psychiatry. 1997;58:27–33. [PubMed] [Google Scholar]
- 20.American Psychiatric Association. Practice Guideline for the Treatment of Patients with Panic Disorders, Second Edition. Washington, D.C.: American Psychiatric Association; 2009.
- 21.Schulberg HC, McClelland M, Coulehan JL, Block M, Werner G. Psychiatric decision making in family practice. Future research directions. Gen Hosp Psychiatry. 1986;8(1):1–6. doi: 10.1016/0163-8343(86)90056-3. [DOI] [PubMed] [Google Scholar]
- 22.Goldstein MZ. Depression and anxiety in older women. Primary Care. 2002;29(1):69–80. doi: 10.1016/S0095-4543(03)00074-5. [DOI] [PubMed] [Google Scholar]
- 23.Rost K, Smith R, Matthews DB, Guise B. The deliberate misdiagnosis of major depression in primary care. Arch Fam Med. 1994;3(4):333–7. doi: 10.1001/archfami.3.4.333. [DOI] [PubMed] [Google Scholar]
- 24.Karp JF, Weiner D, Seligman K, et al. Body pain and treatment response in late-life depression. Am J Geriatr Psychiatr. 2005;13(3):188–94. doi: 10.1176/appi.ajgp.13.3.188. [DOI] [PubMed] [Google Scholar]
- 25.Karp JF, Scott J, Houck P, Reynolds CF, 3rd, Kupfer DJ, Frank E. Pain predicts longer time to remission during treatment of recurrent depression. J Clin Psychiatry. 2005;66(5):591–7. doi: 10.4088/JCP.v66n0508. [DOI] [PubMed] [Google Scholar]
- 26.Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003;163(20):2433–45. doi: 10.1001/archinte.163.20.2433. [DOI] [PubMed] [Google Scholar]
- 27.Rollman B, Mazumdar S, Belnap BH, Houck P, Lenze E, Schulberg H. Main outcomes from the RELAX Trial of telephone-delivered collaborative care for panic and generalized anxiety disorder. J Gen Intern Med. 2010;25(Suppl 3):S326. [Google Scholar]
- 28.Rollman BL, Fischer GS, Zhu F, Belnap BH. Comparison of electronic physician prompts versus waitroom case-finding on clinical trial enrollment. J Gen Intern Med. 2008;23(4):447–50. doi: 10.1007/s11606-007-0449-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shear MK, Brown TA, Barlow DH, et al. Multicenter collaborative panic disorder severity scale. Am J Psychiatry. 1997;154(11):1571–5. doi: 10.1176/ajp.154.11.1571. [DOI] [PubMed] [Google Scholar]
- 30.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32(1):50–5. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 31.Olfson M, Shea S, Feder A, et al. Prevalence of anxiety, depression, and substance use disorders in an urban general medicine practice. Arch Fam Med. 2000;9(9):876–83. doi: 10.1001/archfami.9.9.876. [DOI] [PubMed] [Google Scholar]
- 32.Young AS, Klap R, Sherbourne CD, Wells KB. The quality of care for depressive and anxiety disorders in the United States. Arch Gen Psychiatry. 2001;58(1):55–61. doi: 10.1001/archpsyc.58.1.55. [DOI] [PubMed] [Google Scholar]
- 33.Rollman BL, Belnap BH, Mazumdar S, et al. A randomized trial to improve the quality of treatment for panic and generalized anxiety disorders in primary care. Arch Gen Psychiatry. 2005;62(12):1332–41. doi: 10.1001/archpsyc.62.12.1332. [DOI] [PubMed] [Google Scholar]
- 34.Shear K, Belnap BH, Mazumdar S, Houck P, Rollman BL. Generalized anxiety disorder severity scale (GADSS): a preliminary validation study. Depress Anxiety. 2006;23(2):77–82. doi: 10.1002/da.20149. [DOI] [PubMed] [Google Scholar]
- 35.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–83. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 36.Spitzer RL, Williams JB, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA. 1994;272(22):1749–56. doi: 10.1001/jama.1994.03520220043029. [DOI] [PubMed] [Google Scholar]
- 37.Bech P, Kastrup M, Rafaelsen OJ. Mini-compendium of rating scales for states of anxiety depression mania schizophrenia with corresponding DSM-III syndromes. Acta Psychiatr Scand Suppl. 1986;326:1–37. [PubMed] [Google Scholar]
- 38.Rickels K, Downing R, Schweizer E, Hassman H. Antidepressants for the treatment of generalized anxiety disorder. A placebo-controlled comparison of imipramine, trazodone, and diazepam. Arch Gen Psychiatry. 1993;50(11):884–95. doi: 10.1001/archpsyc.1993.01820230054005. [DOI] [PubMed] [Google Scholar]
- 39.Rollman BL, Belnap BH, Mazumdar S, et al. Symptomatic severity of PRIME-MD diagnosed episodes of panic and generalized anxiety disorder in primary care. J Gen Intern Med. 2005;20(7):623–8. doi: 10.1007/s11606-005-0108-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barlow DH, Gorman JM, Shear MK, Woods SW. Cognitive-behavioral therapy, imipramine, or their combination for panic disorder—a randomized controlled trial. JAMA. 2000;283(19):2529–36. doi: 10.1001/jama.283.19.2529. [DOI] [PubMed] [Google Scholar]
- 41.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Burton K, Polatin PB, Gatchel RJ. Psychosocial factors and the rehabilitation of patients with chronic work-related upper extremity disorders. J Occup Rehabil. 1997;7(3):139–53. doi: 10.1007/BF02767360. [DOI] [Google Scholar]
- 43.Teh CF, Morone NE, Karp JF, et al. Pain interference impacts response to treatment for anxiety disorders. Depress Anxiety. 2009;26(3):222–8. doi: 10.1002/da.20514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Asmundson GJ, Norton PJ, Norton GR. Beyond pain: the role of fear and avoidance in chronicity. Clin Psychol Rev. 1999;19(1):97–119. doi: 10.1016/S0272-7358(98)00034-8. [DOI] [PubMed] [Google Scholar]
- 45.Graham BM, Milad MR. The study of fear extinction: implications for anxiety disorders. Am J Psychiatry. 2011;168(12):1255–65. doi: 10.1176/appi.ajp.2011.11040557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Keefe FJ, Rumble ME, Scipio CD, Giordano LA, Perri LM. Psychological aspects of persistent pain: current state of the science. J Pain. 2004;5(4):195–211. doi: 10.1016/j.jpain.2004.02.576. [DOI] [PubMed] [Google Scholar]
- 47.Dersh J, Polatin PB, Gatchel RJ. Chronic pain and psychopathology: research findings and theoretical considerations. Psychosom Med. 2002;64(5):773–86. doi: 10.1097/01.PSY.0000024232.11538.54. [DOI] [PubMed] [Google Scholar]
- 48.Melzack R. The short-form McGill Pain Questionnaire. Pain. 1987;30(2):191–7. doi: 10.1016/0304-3959(87)91074-8. [DOI] [PubMed] [Google Scholar]
- 49.Kerns RD, Turk DC, Rudy TE. The West Haven-Yale Multidimensional Pain Inventory (WHYMPI) Pain. 1985;23(4):345–56. doi: 10.1016/0304-3959(85)90004-1. [DOI] [PubMed] [Google Scholar]