ABSTRACT
BACKGROUND
Limited health literacy is associated with poor outcomes in many chronic diseases, but little is known about health literacy in chronic obstructive pulmonary disease (COPD).
OBJECTIVE
To examine the associations between health literacy and both outcomes and health status in COPD.
PARTICIPANTS, DESIGN AND MAIN MEASURES
Structured interviews were administered to 277 subjects with self-report of physician-diagnosed COPD, recruited through US random-digit telephone dialing. Health literacy was measured with a validated three-item battery. Multivariable linear regression, controlling for sociodemographics including income and education, determined the cross-sectional associations between health literacy and COPD-related health status: COPD Severity Score, COPD Helplessness Index, and Airways Questionnaire-20R [measuring respiratory-specific health-related quality of life (HRQoL)]. Multivariable logistic regression estimated associations between health literacy and COPD-related hospitalizations and emergency department (ED) visits.
KEY RESULTS
Taking socioeconomic status into account, poorer health literacy (lowest tertile compared to highest tertile) was associated with: worse COPD severity (+2.3 points; 95 % CI 0.3–4.4); greater COPD helplessness (+3.7 points; 95 % CI 1.6–5.8); and worse respiratory-specific HRQoL (+3.5 points; 95 % CI 1.8–4.9). Poorer health literacy, also controlling for the same covariates, was associated with higher likelihood of COPD-related hospitalizations (OR = 6.6; 95 % CI 1.3–33) and COPD-related ED visits (OR = 4.7; 95 % CI 1.5–15). Analyses for trend across health literacy tertiles were statistically significant (p < 0.05) for all above outcomes.
CONCLUSIONS
Independent of socioeconomic status, poor health literacy is associated with greater COPD severity, greater COPD helplessness, worse respiratory-specific HRQoL, and higher odds of COPD-related emergency health-care utilization. These results underscore that COPD patients with poor health literacy may be at particular risk for poor health-related outcomes.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-012-2177-3) contains supplementary material, which is available to authorized users.
KEY WORDS: chronic obstructive pulmonary disease, health literacy, health status, health outcomes, utilization
INTRODUCTION
Educational attainment is an important predictor of poor outcomes in COPD.1 Higher levels of formal education may have indirect impacts on health by virtue of improved job opportunities and associated improved housing, access to health insurance, and income.2,3 Education may also directly impact health by facilitating improved health knowledge and ability to navigate the healthcare system.2,4 This latter, more direct, factor associated with education may be described as “health literacy,” which has been defined as one’s ability “to obtain, process, and understand basic health-related information needed to make appropriate healthcare decisions.”5 Limited health literacy is common, present in almost half of US adults,6 and is associated with underuse of preventative services, worse self-management skills, and poor outcomes among patients with chronic diseases such as diabetes and congestive heart failure.7–10 Thus, health literacy may be more important to health outcomes than educational attainment more broadly defined. The role of health literacy in COPD, however, has received relatively little attention, and in particular, the impact of health literacy on health status and outcomes in COPD has not been well elucidated.11,12
We explored the associations between poor health literacy and COPD-related health status and outcomes, measuring health literacy with a validated three-item questionnaire that can be incorporated readily into routine clinical practice. Because education and income are known to be associated with poor outcomes in COPD,1 we controlled for these key factors in our analyses. Understanding the role of health literacy in COPD outcomes is critical not only to informing communication strategies in clinical settings, but also to developing COPD self-management support approaches that are appropriate for populations with health literacy limitations.
METHODS
Study Population and Recruitment
This study was conducted on a cohort of COPD subjects from an ongoing population-based study of US adults over the age of 55.13 Survey methods have previously been described in detail, and further detail is available in an online supplement. 13–17 Briefly, subjects were identified from throughout the US by random-digit telephone dialing beginning in 2001, with regional oversampling in Northern California and in geographic “hot spots” with increased COPD mortality.18 The overall study participation rate was 53 % among households meeting initial eligibility screening. Only telephone landlines were sampled; subjects with only cellular mobile phones were not included. Interviews were conducted in English. Subjects were included in longitudinal follow-up if they reported being diagnosed by a physician with an airway disease. This study of health literacy took place in the annual follow-up interview performed in 2009 among the 277 subjects reporting a physician’s diagnosis of emphysema, COPD, or chronic bronchitis, and subjects were classified as having COPD if they reported any of these three physician’s diagnoses. Classification of COPD status as such has been shown to be reasonably accurate as compared with both medical record review and pulmonary function testing.19–21 All study procedures were approved by the University of California San Francisco Committee on Human Research, and all participants provided written informed consent.
Measurements
Health Literacy Assessment
Health literacy was assessed with the validated three-item questionnaire developed by Chew and colleagues: (1) “How often do you have someone like a family member, friend, hospital or clinic worker, or caregiver, help you read hospital materials?” (2) “How often do you have problems learning about your medical condition because of difficulty understanding written information?” (3) “How confident are you filling out medical forms by yourself?”22 Items have a five-option Likert response scale, and scores were summed to yield a total score of 3–15; higher scores indicate better health literacy. These three items correlate strongly with direct tests of literacy, such as the Rapid Estimate of Adult Literacy in Medicine, with areas under the receiver operator curve close to 0.8 in multiple studies in various populations.22–26 This three-item battery has also recently been shown to be predictive of mortality in congestive heart failure.10
Because of the distribution of health literacy scores in our cohort, we divided health literacy scores into tertiles for analysis (approximately 1/3 of subjects had a maximum health literacy score and thus formed a natural cut point for the top tertile). Health literacy has been divided into three levels of capacity in prior literature,6 providing further a priori rationale for dividing the score into tertiles rather than quartiles or some other division. We also conducted sensitivity analyses in which we re-analyzed health literacy scores as a continuous variable; all relationships between health outcomes/status and health literacy that were statistically significant when health literacy was analyzed categorically in tertiles were also statistically significant (p < 0.05) when health literacy was analyzed as a continuous variable (results of sensitivity analyses are not presented).
COPD-Related Health Status Measures
COPD-associated helplessness was assessing using the validated 13-item COPD Helplessness Index (CHI), which measures learned helplessness associated with seemingly unpredictable and uncontrollable COPD-related adverse events.27,28 We have previously shown the CHI to be predictive of COPD-related utilization, independent of its association with COPD severity.27 Scores can range from 0–52; higher scores indicate greater helplessness.
Respiratory-specific health-related quality of life (HRQoL) was assessed using the validated revised Airways Questionnaire-20R (AQ-20R).15,29,30 The 20-item AQ-20R is comparable in performance to the St. George Respiratory Questionnaire for measuring HRQoL in COPD patients.15,29,30 Scores range from 0–20; higher scores reflect poorer respiratory-specific HRQoL.
We assessed COPD severity using the previously validated COPD Severity Score, which is based on survey responses addressing five domains of severity: dyspnea, COPD-related requirement for systemic corticosteroids and antibiotics, regular COPD medication usage, prior COPD-related hospitalizations and intubations, and home oxygen use.14 We and others have previously shown that the COPD Severity Score demonstrates both concurrent and predictive validity, including a prospective association with COPD exacerbations and hospitalizations.14,31–33 Scores range from 0–35, with higher scores representing more severe COPD.
COPD Exacerbations and Healthcare Utilization
Although there is no consensus definition of COPD exacerbations, emergency COPD-related healthcare utilization is often used to define a more severe COPD exacerbation.34–36 Subjects were therefore asked whether they had been admitted to the hospital for an overnight stay or been evaluated in the emergency room or emergency department (ED) in the preceding 12 months. Hospitalizations and ED visits were categorized as COPD-related if subjects further identified the primary cause of such utilization to be worsening of a “lung or breathing problem.”
Separately, to assess worsening symptoms, we asked subjects if they had experienced a worsening of breathing symptoms that lasted a week or more at any point in the previous 12 months. Subjects responding affirmatively to this question were then asked if they had sought medical advice for such worsening symptoms from an “advice nurse” or physician, either by telephone or in-person. The purpose of the latter outcome measure was to determine whether subjects who experienced such worsening symptoms were more or less likely to seek medical advice for these symptoms depending on their level of health literacy.
Sociodemographic Characteristics
Age, gender, marital status (married or cohabitating vs single), self-identified race-ethnicity, educational attainment, and annual household income were assessed in structured telephone interview. Educational attainment was categorized as less than high school, high school graduate, some college but no degree, or college graduate or higher. Annual household income was categorized as <$20,000, ≥$20,000 to <$40,000, ≥$40,000 to <$60,000, ≥$60,000 to $80,000, and ≥$80,000.
Statistical Analysis
Internal consistency of the health literacy scale was evaluated using Cronbach’s α. Because education and income are likely associated with health literacy, we examined the association between these factors and health literacy scores using both graphical analysis and the Kruskal-Wallis test.
We utilized multivariable linear regression to analyze the associations between health literacy as a predictor (independent) variable and, in three separate models, the outcome (dependent) variables of: [1] COPD Severity Score, [2] COPD Helplessness Index, and [3] AQ-20R (respiratory-specific HRQoL). We controlled for age, gender, race, marital status, and both education and annual household income in our multivariable analyses. As detailed below, the vast majority of our sample was non-Latino white, and thus race-ethnicity was categorized as non-Latino white vs non-white.
Similarly, multivariable logistic regression estimated the associations between health literacy and the outcomes of (1) COPD-related hospitalizations, (2) COPD-related ED visits, and (3) a ≥1 week worsening of respiratory symptoms above and beyond baseline. These analyses also controlled for the same sociodemographic covariates, including education and income. Separately, among the subset of subjects reporting a ≥1 week worsening of respiratory symptoms (n = 140), we used multivariable logistic regression, controlling for the same covariates, to test whether health literacy was associated with the likelihood of the subject having sought phone or in-person advice/treatment for such worsening symptoms. We also used the Kruskal-Wallis test to examine the bivariate associations between health literacy score and requirement for either COPD-related ED visit or hospitalization.
Additionally, we performed sensitivity analyses in which we included smoking status (current smoker vs non-current smoker) as a covariate in the above analyses. Smoking could potentially be a confounder in the relationship between health literacy and poor outcomes to the extent that it might independently worsen health literacy and contribute to poor outcomes. Alternatively, it could be a mediator to the extent that low health literacy might make tobacco cessation more difficult. Regardless, including smoking status as a covariate did not substantively impact any of the core findings (data not shown), and results are presented without controlling for this factor.
All analyses used Stata/SE version 9.2 (StataCorp; College Station, TX). For all multivariable logistic regression models, the Hosmer-Lemeshow test demonstrated adequate goodness-of-fit (p > 0.15 for all models).37 We used the linear contrast method to test for trend in the relationship between health literacy tertile and each outcome examined in multivariable analyses (e.g., to test there was a trend for decreasing health literacy, across tertiles, and poorer outcomes).38
RESULTS
Subject Characteristics
Sociodemographic characteristics are presented in Table 1. Among 277 study participants, 65 % were women and 94 % were non-Latino white. There was a broad range of both educational attainment and reported annual household incomes.
Table 1.
Characteristics of the 277 COPD Subjects Recruited Through Random-Digit Telephone Dialing
| N (%) | |
|---|---|
| Age, years | |
| 55–60 | 21 (8 %) |
| 61–65 | 68 (25 %) |
| 66–70 | 73 (26 %) |
| 71–75 | 65 (23 %) |
| >75 | 50 (18 %) |
| Non-Latino white | 261 (94 %) |
| Female | 181 (65 %) |
| Married/cohabitating | 151 (55 %) |
| Educational attainment | |
| Less than high school | 25 (9 %) |
| High school graduate | 58 (21 %) |
| Some college | 107 (39 %) |
| College graduate | 87 (31 %) |
| Annual household income | |
| Less than $20K | 48 (17 %) |
| $20K–$40K | 79 (29 %) |
| $40K–$60K | 51 (18 %) |
| $60K–$80K | 29 (11 %) |
| More than $80K | 56 (20 %) |
| Refused to provide | 14 (5 %) |
Health Literacy Assessment
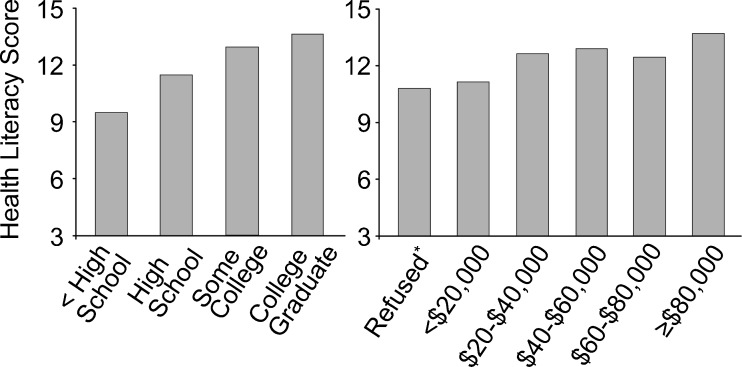
The mean health literacy score was 12.5 (median 14; 25th–75th interquartile range 11–15). Cronbach’s α for the three scale items was 0.75, indicating good internal consistency. As anticipated, better health literacy scores were correlated with greater educational attainment and higher income (p < 0.001 by Kruskal-Wallis test for both; Fig. 1).
Figure 1.
Median health literacy scores by educational attainment and annual household income. p < 0.001 for difference by category, for both education and income (Kruskal-Wallis test). *Refused to provide income (N = 14; 5 % of subjects).
Association Between Health Literacy and COPD-Related Health Status
As shown in Table 2, in multivariable analysis controlling for sociodemographic factors including income and education, poorer health literacy was associated with greater COPD severity, greater learned helplessness, and worse respiratory-specific HRQoL. Comparing the lowest tertile of health literacy to the highest, 95 % confidence intervals (CI) excluded no association for each of these three outcomes. Tests for trend indicated a trend of poorer COPD-related health status with decreasing health literacy across tertiles for each of the three outcomes (p < 0.05 for all).
Table 2.
Association Between Poorer Health Literacy and COPD-Related Health Status Measures Among 277 COPD Subjects
| COPD-related health status measure* | Mean ± SD | Difference associated with health literacy tertile (95 % CI)† | Analysis for trend across health literacy tertiles‡ |
|---|---|---|---|
| COPD severity score | 8.0 ± 6.6 | Highest: 0 [referent] | p = 0.025 |
| Middle: 1.2 (−0.5–3.0) | |||
| Lowest: 2.3 (0.3–4.4) | |||
| COPD helplessness index | 17.3 ± 6.6 | Highest: 0 [referent] | p < 0.001 |
| Middle: 1.9 (0.1–3.7) | |||
| Lowest: 3.7 (1.6–5.8) | |||
| Respiratory-specific HRQoL (AQ-20R) | 7.4 ± 5.2 | Highest: 0 [referent] | p < 0.001 |
| Middle: 1.4 (0.1–2.7) | |||
| Lowest: 3.4 (1.8–4.9) |
*Each COPD-related health status measure was used as the dependent (outcome) variable in a separate multivariable linear regression in which health literacy was the independent (predictor) variable of interest, and covariates were: age, gender, race, marital status, educational attainment, and income
†Results indicate that poorer health literacy is associated with poorer health status in each of the three COPD-related measures examined
‡Test for trend using the linear contrast method indicated a trend of poorer COPD-related health status with decreasing health literacy across tertiles
Association Between Health Literacy and COPD-Related Health Outcomes
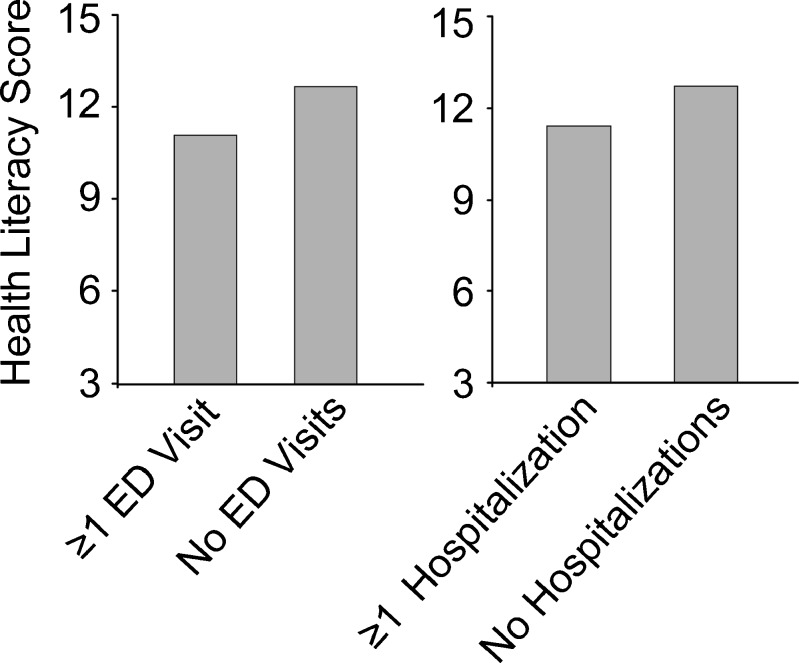
Poorer health literacy was associated with greater odds of both COPD-related ED visits and hospitalizations in bivariate analyses (Fig. 2). As shown in Table 3, after controlling for sociodemographic factors, poorer health literacy was not statistically associated with having experienced a worsening of respiratory symptoms lasting at least 1 week. However, among those who did experience such a worsening in respiratory symptoms (N = 140; 50.1 % of sample), poorer health literacy, comparing the lowest tertile to the highest tertile of health literacy, was associated with a greater likelihood of seeking medical advice and/or treatment for such worsening symptoms. Comparing the lowest tertile to the highest tertile, poorer health literacy was also associated with greater likelihood of a COPD-related ED visit and COPD-related hospitalization. Tests for trend indicated a trend of increasing odds of COPD-related hospitalizations, ED visits, and likelihood of seeking medical advice/treatment for worsening symptoms with decreasing health literacy across tertiles (p < 0.05).
Figure 2.
Median health literacy scores associated with COPD-related emergency utilization. p < 0.01 for difference, for both ED visits and hospitalizations (Kruskal-Wallis test).
Table 3.
Association Between Poorer Health Literacy and COPD-Related Outcomes Among 277 COPD Subjects
| COPD-related outcome* | Events/N† | OR associated with health literacy tertile (95 % CI) | Analysis for trend across health literacy tertiles‡ |
|---|---|---|---|
| ≥1 week period of worsening respiratory symptoms | 140/277 (50.5 %) | Highest: 1.0 [referent] | p = 0.59 |
| Middle: 1.0 (0.6–1.9) | |||
| Lowest: 1.2 (0.6–2.5) | |||
| Sought advice and/or treatment for worsening symptoms§ | 109/140 (77.9 %) | Highest: 1.0 [referent] | p = 0.003 |
| Middle: 2.2 (0.8–6.3) | |||
| Lowest: 8.8 (2.1–37) | |||
| COPD-related ED Visits | 38/277 (13.7 %) | Highest: 1.0 [referent] | p = 0.009 |
| Middle: 3.0 (1.1–8.5) | |||
| Lowest: 4.7 (1.5–15) | |||
| COPD-related hospitalizations | 22/277 (7.9 %) | Highest: 1.0 [referent] | p = 0.02 |
| Middle: 2.7 (0.6–11.8) | |||
| Lowest: 6.6 (1.3–33) |
*Each COPD-related outcome above was used as the dependent (outcome) variable in a separate multivariable logistic regression in which health literacy was the independent (predictor) variable of interest and covariates were: age, gender, race, marital status, educational attainment, and income
†Number of subjects with events (e.g., there were 22 subjects with ≥1 COPD-related hospitalization) and sample size (N) for each analysis
‡Tests for trend indicated a trend of increasing odds of COPD-related hospitalizations, ED visits, and likelihood of seeking medical advice/treatment for worsening symptoms with decreasing health literacy across tertiles
§The analysis of the association between poorer health literacy and likelihood of seeking medical advice/treatment for worsening symptoms, either via phone or in-person, was conducted only on the subset of subjects who reported a ≥1 week period of worsening respiratory symptoms (N = 140)
DISCUSSION
In this population-based cohort, poorer health literacy was associated with worse COPD-related health status and adverse COPD-related outcomes. Importantly, poorer health literacy was associated with such outcomes even after controlling for poor health literacy’s well-known relationship with sociodemographic factors, including education and income. These findings suggest both a potential target for intervention in COPD as well as a potential screening tool that might be used to identify patients at risk for poor outcomes.
This is the first systematic analysis, to our knowledge, to demonstrate an association between poor health literacy and poor outcomes in COPD.12 Prior research has suggested that limited health literacy contributes to adverse outcomes in other chronic diseases.9,10 Such studies, however, have not yielded uniform results, with a recent study by Peterson and colleagues showing no independent association between health literacy, measured with the same 3-item instrument, and hospitalizations in heart failure.10 Moreover, because chronic diseases vary in both the complexity of the required self-management as well as the efficacy of associated treatments, demonstrating a relationship between poorer health literacy and worse outcomes specifically in COPD is an important step for disease-specific interventions.39
This was a cross-sectional analysis of health status, with COPD-related outcomes reported retrospectively for the year preceding the interview. This precludes a definitive assessment of causality between poor health literacy and worse outcomes. Nonetheless, unlike factors such as depression that might worsen as a result of a hospitalization,40 health literacy is less likely to be affected by events such as hospitalizations or ED visits.11 For example, having been hospitalized for COPD would be relatively unlikely to negatively affect “learning about [one’s] medical condition because of difficulty understanding written information,” as assessed in one of the three health literacy items. Although it is possible that severe COPD exacerbations requiring intubation might impair cognitive function, any such declines may largely resolve with the exacerbation.41 Certainly, there is reason to believe that poorer health literacy may be causally related to worse outcomes in COPD. Patients with limited health literacy are more likely to have impaired self-management skills, including difficulty understanding their medication regimens.42,43 Although a recent study by Press and colleagues did not find an association between limited health literacy and COPD medication knowledge,44 other studies have found a relationship between poor health literacy and medication knowledge in asthma patients.45,46 Alternatively, it is possible that poor health literacy may be operating within a vicious cycle, whereby factors such as hypoxemia contribute to impaired cognition and thus worse health literacy, which in turn leads to poorer COPD outcomes.
Poor health literacy was not only associated statistically with poor outcomes but also worse COPD-related health status, in particular the COPD severity, learned helplessness, and respiratory-specific HRQoL. Although minimum clinically important differences (MCIDs) are not explicitly determined for the instruments with which these constructs were measured, MCIDs for health status measures are generally approximated by a ½ standard deviation change in a scale.47,48 By this standard, our results suggest that subjects in the lowest tertile of health literacy had meaningfully worse learned helplessness and respiratory-specific HRQoL than subjects in the highest tertile of health literacy, but differences in COPD severity did not meet this criterion for MCID.
Our finding with respect to learned helplessness does suggest another potential mechanism by which limited health literacy may contribute to poorer outcomes. Learned helplessness theory posits that feelings of passive resignation brought on by seemingly uncontrollable adverse events may lead to decreased problem-solving,27,28 and limited health literacy could contribute to a sense of helplessness by exacerbating a perceived lack of control. Learned helplessness is closely related to the construct of self-efficacy,27,28 and it is interesting that Mancuso and colleagues did not find a relationship in asthma patients between limited health literacy and poor self-efficacy.49 It is possible that these contrasting findings are due to differences in the constructs assessed or potentially due to differences between asthma and COPD; relative to asthma, COPD is a more progressive and chronically deteriorating disease.28,50
Health literacy was not statistically associated with the likelihood of experiencing a ≥1 week worsening of respiratory symptoms but was associated with the likelihood of seeking advice or treatment for such worsening symptoms. This may have been because symptoms were simply worse among subjects with poorer health literacy. However, this may also suggest that subjects with poorer health literacy are more likely to utilize healthcare resources, potentially because of inability or lack of confidence in their ability to self-manage their symptoms without medical assistance. Some studies have indeed found that patients with limited health literacy are more likely to utilize emergency medical care.51,52 On the other hand, patients with poor health literacy may also be reluctant to interact with the medical system, because of feelings of shame or distrust, and thus be less likely to seek advice or treatment for worsening symptoms.11,53 This finding regarding the likelihood of seeking medical attention is by no means obvious and may suggest that improvements in self-management skills are one route to decreasing utilization among patients with limited health literacy.
Our study has additional limitations beyond those already addressed above. Although recruited through random-digit telephone dialing, our study was conducted in English and our cohort was largely white, which may limit generalizability to more racially and ethnically diverse populations. Nonetheless, the fact that we did find an association between health literacy and poor outcomes despite the relative racial homogeneity of the cohort suggests that the role of health literacy may be distinct from that of cultural perceptions associated with ethnicity. That is, even in this largely white cohort, health literacy appears to have played an important role in health status and outcomes. Second, we relied upon self-report to identify healthcare utilization. This approach has been shown to be valid and accurate, especially for emergency utilization (as compared to routine outpatient care).54–56,57 We utilized a time frame of 12 months for recall of such events, and while a shorter duration of recall may improve accuracy, the relatively infrequent nature of events such as hospitalizations made a shorter recall period impractical. Nonetheless, longitudinal studies with objective verification of events will be an important future avenue of research. Third, our health literacy scale was not normally distributed, with a ceiling effect for approximately a third of the cohort. Because we took this distribution into account, analyzing the scale as an ordinal categorical variable, this ceiling effect should not have driven our findings. Fourth, we assessed health literacy through indirect measurement rather than with direct tests such as reading comprehension evaluation. Although it is possible that our measurement assessed other constructs, such as visual or cognitive impairments, this brief instrument correlates strongly with direct measurements and is more practical for incorporating into clinical practice or for identifying patients at higher risk.10,22–25 Additionally, factors such as visual and cognitive impairments are considered by many to be an integral part of health literacy, and it may therefore be appropriate that our survey battery captured such related constructs.11
This analysis has important implications. First and foremost, our findings suggest that poor health literacy may play an important and independent role in health status and outcomes among COPD patients. Developing both patient-clinician level as well as system-based strategies to improve communication and understanding in COPD patients with limited health literacy may therefore have the potential to improve outcomes.11 Similar approaches have achieved some success in diabetes and heart failure.58,59 Further research is required to elucidate causal pathways and potential interventions. These results both establish a basis for such work as well as highlight to healthcare professionals the importance of considering health literacy in their communications with COPD patients.
Electronic supplementary material
(DOCX 31 kb)
Acknowledgments
Dr. Omachi was supported by K23 HL102159 from the National Heart, Lung, and Blood Institute, National Institutes of Health. Dr. Katz, Dr. Blanc, and recruitment of the cohort were supported by R01 HL067438 from the National Heart, Lung, and Blood Institute, National Institutes of Health.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Abbreviations
- AQ-20R
Airways Questionnaire-20R
- CHI
COPD Helplessness Index
- CI
confidence interval
- COPD
chronic obstructive pulmonary disease
- ED
emergency department
- HRQoL
health-related quality of life
- OR
odds ratio
- MCID
minimum clinically important difference
- SD
standard deviation
Contributor Information
Theodore A. Omachi, Phone: +1-415-4768058, FAX: +1-415-8853650, Email: omachi@ucsf.edu.
Urmimala Sarkar, Email: usarkar@medsfgh.ucsf.edu.
Edward H. Yelin, Email: ed.yelin@ucsf.edu.
Paul D. Blanc, Email: paul.blanc@ucsf.edu.
Patricia P. Katz, Email: patti.katz@ucsf.edu.
REFERENCES
- 1.Eisner MD, Blanc PD, Omachi TA, et al. Socioeconomic status, race and COPD health outcomes. J Epidemiol Community Health. 2011;65:26–34. doi: 10.1136/jech.2009.089722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian JA, Huang J. Health literacy and mortality among elderly persons. Arch Intern Med. 2007;167:1503–9. doi: 10.1001/archinte.167.14.1503. [DOI] [PubMed] [Google Scholar]
- 3.Davey Smith G, Hart C, Hole D, et al. Education and occupational social class: which is the more important indicator of mortality risk? J Epidemiol Community Health. 1998;52:153–60. doi: 10.1136/jech.52.3.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blane D. Commentary: explanations of the difference in mortality risk between different educational groups. Int J Epidemiol. 2003;32:355–6. doi: 10.1093/ije/dyg078. [DOI] [PubMed] [Google Scholar]
- 5.Health literacy: A prescription to end confusion. Washington, DC: National Academy Press, Institute of Medicine Committee on Health Literacy; 2004. [Google Scholar]
- 6.Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielsen-Bohlman LT, Rudd RR. The prevalence of limited health literacy. J Gen Intern Med. 2005;20:175–84. doi: 10.1111/j.1525-1497.2005.40245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient Educ Couns. 2003;51:267–75. doi: 10.1016/S0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- 8.Scott TL, Gazmararian JA, Williams MV, Baker DW. Health literacy and preventive health care use among Medicare enrollees in a managed care organization. Med Care. 2002;40:395–404. doi: 10.1097/00005650-200205000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Schillinger D, Grumbach K, Piette J, et al. Association of health literacy with diabetes outcomes. Jama. 2002;288:475–82. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 10.Peterson PN, Shetterly SM, Clarke CL, et al. Health literacy and outcomes among patients with heart failure. Jama. 2011;305:1695–701. doi: 10.1001/jama.2011.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Paasche-Orlow MK, Wolf MS. The causal pathways linking health literacy to health outcomes. Am J Health Behav. 2007;31(Suppl 1):S19–26. doi: 10.5993/AJHB.31.s1.4. [DOI] [PubMed] [Google Scholar]
- 12.Roberts NJ, Ghiassi R, Partridge MR. Health literacy in COPD. Int J Chron Obstruct Pulmon Dis. 2008;3:499–507. doi: 10.2147/copd.s1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Trupin L, Earnest G, San Pedro M, et al. The occupational burden of chronic obstructive pulmonary disease. Eur Respir J. 2003;22:462–9. doi: 10.1183/09031936.03.00094203. [DOI] [PubMed] [Google Scholar]
- 14.Eisner MD, Trupin L, Katz PP, et al. Development and validation of a survey-based COPD severity score. Chest. 2005;127:1890–7. doi: 10.1378/chest.127.6.1890. [DOI] [PubMed] [Google Scholar]
- 15.Chen H, Eisner MD, Katz PP, Yelin EH, Blanc PD. Measuring disease-specific quality of life in obstructive airway disease: validation of a modified version of the airways questionnaire 20. Chest. 2006;129:1644–52. doi: 10.1378/chest.129.6.1644. [DOI] [PubMed] [Google Scholar]
- 16.Blanc PD, Eisner MD, Trupin L, Yelin EH, Katz PP, Balmes JR. The association between occupational factors and adverse health outcomes in chronic obstructive pulmonary disease. Occup Environ Med. 2004;61:661–7. doi: 10.1136/oem.2003.010058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Katz PP, Gregorich S, Eisner M, et al. Disability in valued life activities among individuals with COPD and other respiratory conditions. J Cardiopulm Rehabil Prev. 2010;30:126–36. doi: 10.1097/HCR.0b013e3181be7e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim J. Atlas of respiratory disease mortality, United States: 1982–1993. Cincinnati, OH: Department of Health and Human Services, National Institute for Occupational Safety and Health; 1998. [Google Scholar]
- 19.Radeos MS, Cydulka RK, Rowe BH, Barr RG, Clark S, Camargo CA., Jr Validation of self-reported chronic obstructive pulmonary disease among patients in the ED. American J Emerg Med. 2009;27:191–6. doi: 10.1016/j.ajem.2008.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tisnado DM, Adams JL, Liu H, et al. What is the concordance between the medical record and patient self-report as data sources for ambulatory care? Med Care. 2006;44:132–40. doi: 10.1097/01.mlr.0000196952.15921.bf. [DOI] [PubMed] [Google Scholar]
- 21.Straus SE, McAlister FA, Sackett DL, Deeks JJ. Accuracy of history, wheezing, and forced expiratory time in the diagnosis of chronic obstructive pulmonary disease. J Gen Intern Med. 2002;17:684–8. doi: 10.1046/j.1525-1497.2002.20102.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36:588–94. [PubMed] [Google Scholar]
- 23.Chew LD, Griffin JM, Partin MR, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008;23:561–6. doi: 10.1007/s11606-008-0520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wallace LS, Rogers ES, Roskos SE, Holiday DB, Weiss BD. Brief report: screening items to identify patients with limited health literacy skills. J Gen Intern Med. 2006;21:874–7. doi: 10.1111/j.1525-1497.2006.00532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sarkar U, Schillinger D, Lopez A, Sudore R. Validation of self-reported health literacy questions among diverse English and Spanish-speaking populations. J Gen Intern Med. 2011;26:265–71. doi: 10.1007/s11606-010-1552-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Davis TC, Long SW, Jackson RH, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25:391–5. [PubMed] [Google Scholar]
- 27.Omachi TA, Katz PP, Yelin EH, et al. The COPD Helplessness Index: A new tool to measure factors affecting patient self-management. Chest 2010;137(4):823–30. [DOI] [PMC free article] [PubMed]
- 28.Peterson C. Learned helplessness and health psychology. Health Psychol. 1982;1:153–68. doi: 10.1037/0278-6133.1.2.153. [DOI] [Google Scholar]
- 29.Hajiro T, Nishimura K, Jones PW, et al. A novel, short, and simple questionnaire to measure health-related quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1999;159:1874–8. doi: 10.1164/ajrccm.159.6.9807097. [DOI] [PubMed] [Google Scholar]
- 30.Alemayehu B, Aubert RE, Feifer RA, Paul LD. Comparative analysis of two quality-of-life instruments for patients with chronic obstructive pulmonary disease. Value Health. 2002;5:437–42. doi: 10.1046/J.1524-4733.2002.55151.x. [DOI] [PubMed] [Google Scholar]
- 31.Omachi TA, Yelin EH, Katz PP, Blanc PD, Eisner MD. The COPD severity score: a dynamic prediction tool for health-care utilization. Copd. 2008;5:339–46. doi: 10.1080/15412550802522700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Eisner MD, Omachi TA, Katz PP, Yelin EH, Iribarren C, Blanc PD. Measurement of COPD severity using a survey-based score: validation in a clinically and physiologically characterized cohort. Chest. 2010;137:846–51. doi: 10.1378/chest.09-1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Miravitlles M, Llor C, de Castellar R, Izquierdo I, Baro E, Donado E. Validation of the COPD severity score for use in primary care: the NEREA study. Eur Respir J. 2009;33:519–27. doi: 10.1183/09031936.00087208. [DOI] [PubMed] [Google Scholar]
- 34.Burge S, Wedzicha JA. COPD exacerbations: definitions and classifications. Eur Respir J Suppl. 2003;41:46s–53s. doi: 10.1183/09031936.03.00078002. [DOI] [PubMed] [Google Scholar]
- 35.Pauwels R, Calverley P, Buist AS, et al. COPD exacerbations: the importance of a standard definition. Respir Med. 2004;98:99–107. doi: 10.1016/j.rmed.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 36.Rodriguez-Roisin R. Toward a consensus definition for COPD exacerbations. Chest. 2000;117:398S–401S. doi: 10.1378/chest.117.5_suppl_2.398S. [DOI] [PubMed] [Google Scholar]
- 37.Hosmer DW, Lemeshow S. Applied logistic regression. 2. Hoboken, NJ: John Wiley & Sons, Inc.; 2000. [Google Scholar]
- 38.Vittinghoff E, Glidden DV, Shiboski SC, McCulloch CE. Regression Methods in Biostatistics: Linear, Logistic, Survivial, and Repeated Measures Models. New York: Springer Science & Business Media, Inc.; 2005. [Google Scholar]
- 39.Bourbeau J, Julien M, Maltais F, et al. Reduction of hospital utilization in patients with chronic obstructive pulmonary disease: a disease-specific self-management intervention. Arch Intern Med. 2003;163:585–91. doi: 10.1001/archinte.163.5.585. [DOI] [PubMed] [Google Scholar]
- 40.Covinsky KE, Fortinsky RH, Palmer RM, Kresevic DM, Landefeld CS. Relation between symptoms of depression and health status outcomes in acutely ill hospitalized older persons. Ann Intern Med. 1997;126:417–25. doi: 10.7326/0003-4819-126-6-199703150-00001. [DOI] [PubMed] [Google Scholar]
- 41.Ambrosino N, Bruletti G, Scala V, Porta R, Vitacca M. Cognitive and perceived health status in patient with chronic obstructive pulmonary disease surviving acute on chronic respiratory failure: a controlled study. Intensive Care Med. 2002;28:170–7. doi: 10.1007/s00134-001-1165-6. [DOI] [PubMed] [Google Scholar]
- 42.Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients’ knowledge of their chronic disease. A study of patients with hypertension and diabetes. Arch Intern Med. 1998;158:166–72. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- 43.Williams MV, Parker RM, Baker DW, Coates W, Nurss J. The impact of inadequate functional health literacy on patients’ understanding of diagnosis, prescribed medications, and compliance. Acad Emerg Med. 1995;2:386. doi: 10.1111/j.1553-2712.1995.tb03088.x. [DOI] [Google Scholar]
- 44.Press VG, Arora VM, Shah LM. Misuse of respiratory inhalers in hospitalized patients with asthma or COPD. J Gen Intern Med. 2011;26:635–42. doi: 10.1007/s11606-010-1624-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Paasche-Orlow MK, Riekert KA, Bilderback A. Tailorededucation may reduce health literacy disparities in asthma self-management. Am J Respir Crit Care Med. 2005;172:980–6. doi: 10.1164/rccm.200409-1291OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Williams MV, Baker DW, Honig EG, Lee TM, Nowlan A. Inadequate literacy is a barrer to asthma knowledge and self-care. Chest. 1998;114:1008–15. doi: 10.1378/chest.114.4.1008. [DOI] [PubMed] [Google Scholar]
- 47.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41:582–92. doi: 10.1097/01.MLR.0000062554.74615.4C. [DOI] [PubMed] [Google Scholar]
- 48.Kazis LE, Anderson JJ, Meenan RF. Effect sizes for interpreting changes in health status. Med Care. 1989;27:S178–89. doi: 10.1097/00005650-198903001-00015. [DOI] [PubMed] [Google Scholar]
- 49.Mancuso CA, Rincon M. Impact of health literacy on longitudinal asthma outcomes. J Gen Intern Med. 2006;21:813–7. doi: 10.1111/j.1525-1497.2006.00528.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bleecker ER. Similarities and differences in asthma and COPD. The Dutch hypothesis. Chest. 2004;126:93S–5S. doi: 10.1378/chest.126.2_suppl_1.93S. [DOI] [PubMed] [Google Scholar]
- 51.Baker DW, Gazmararian JA, Williams MV, et al. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. Am J Public Health. 2002;92:1278–83. doi: 10.2105/AJPH.92.8.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Baker DW, Parker RM, Williams MV, Clark WS. Health literacy and the risk of hospital admission. J Gen Intern Med. 1998;13:791–8. doi: 10.1046/j.1525-1497.1998.00242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Baker DW, Parker RM, Williams MV, et al. The health care experience of patients with low literacy. Arch Fam Med. 1996;5:329–34. doi: 10.1001/archfami.5.6.329. [DOI] [PubMed] [Google Scholar]
- 54.Quint JK, Donaldson GC, Hurst JR, Goldring JJ, Seemungal TR, Wedzicha JA. Predictive accuracy of patient-reported exacerbation frequency in COPD. Eur Respir J. 2011;37:501–7. doi: 10.1183/09031936.00035909. [DOI] [PubMed] [Google Scholar]
- 55.Raina P, Torrance-Rynard V, Wong M, Woodward C. Agreement between self-reported and routinely collected health-care utilization data among seniors. Health Serv Res. 2002;37:751–74. doi: 10.1111/1475-6773.00047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cleary PD, Jette AM. The validity of self-reported physician utilization measures. Med Care. 1984;22:796–803. doi: 10.1097/00005650-198409000-00003. [DOI] [PubMed] [Google Scholar]
- 57.Roberts RO, Bergstralh EJ, Schmidt L, Jacobsen SJ. Comparison of self-reported and medical record health care utilization measures. J Clin Epidemiol. 1996;49:989–95. doi: 10.1016/0895-4356(96)00143-6. [DOI] [PubMed] [Google Scholar]
- 58.Rothman RL, DeWalt DA, Malone R, et al. Influence of patient literacy on the effectiveness of a primary care-based diabetes disease management program. Jama. 2004;292:1711–6. doi: 10.1001/jama.292.14.1711. [DOI] [PubMed] [Google Scholar]
- 59.DeWalt DA, Malone RM, Bryant ME, et al. A heart failure self-management program for patients of all literacy levels: a randomized, controlled trial [ISRCTN11535170] BMC Health Serv Res. 2006;6:30. doi: 10.1186/1472-6963-6-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 31 kb)