ABSTRACT
BACKGROUND
Although collaborative care is effective for treating depression and other mental disorders in primary care, there have been no randomized trials of collaborative care specifically for patients with Posttraumatic stress disorder (PTSD).
OBJECTIVE
To compare a collaborative approach, the Three Component Model (3CM), with usual care for treating PTSD in primary care.
DESIGN
The study was a two-arm, parallel randomized clinical trial. PTSD patients were recruited from five primary care clinics at four Veterans Affairs healthcare facilities and randomized to receive usual care or usual care plus 3CM. Blinded assessors collected data at baseline and 3-month and 6-month follow-up.
PARTICIPANTS
Participants were 195 Veterans. Their average age was 45 years, 91% were male, 58% were white, 40% served in Iraq or Afghanistan, and 42% served in Vietnam.
INTERVENTION
All participants received usual care. Participants assigned to 3CM also received telephone care management. Care managers received supervision from a psychiatrist.
MAIN MEASURES
PTSD symptom severity was the primary outcome. Depression, functioning, perceived quality of care, utilization, and costs were secondary outcomes.
KEY RESULTS
There were no differences between 3CM and usual care in symptoms or functioning. Participants assigned to 3CM were more likely to have a mental health visit, fill an antidepressant prescription, and have adequate antidepressant refills. 3CM participants also had more mental health visits and higher outpatient pharmacy costs.
CONCLUSIONS
Results suggest the need for careful examination of the way that collaborative care models are implemented for treating PTSD, and for additional supports to encourage primary care providers to manage PTSD.
KEY WORDS: posttraumatic stress disorder, integrated primary care, veterans, randomized clinical trials, treatment
INTRODUCTION
Posttraumatic stress disorder (PTSD) is a severe and often disabling condition resulting from traumatic events such as assault, accidents, and combat.1 It is associated with significant comorbidity, poor health, and impairment.2–4 Lifetime prevalence in US adults is higher in women (9.7%) than in men (3.6%),5 and is especially high among military veterans.6,7
It is important to enhance strategies for managing PTSD in primary care settings. There are effective treatments (particularly cognitive-behavioral therapy and serotonin reuptake inhibitors),8,9 but many individuals with PTSD do not seek mental health care. According to the National Comorbidity Survey-Replication, only 7.1% of individuals with PTSD seek treatment within the first year of onset, versus 37.4% of those with depression and 33.6% of those with panic disorder.10 Instead, many individuals with PTSD present in primary care settings, where it may be underdetected.11 In one study, PTSD had been identified in only 17.8% of veterans with PTSD who were treated in primary care, compared with 78.0% who were treated in mental health settings.3 Gaps in clinician knowledge about PTSD are a significant problem too.11,12 As a result, PTSD patients treated in primary care may not receive adequate treatment. Although the Department of Veterans Affairs (VA) now requires mandatory PTSD screening in primary care clinics, veterans with PTSD who are treated in primary care may have fewer visits for PTSD,13 or be less likely to obtain medication treatment14 relative to veterans who are treated in specialty mental health care. System factors, such as access to mental health specialists and linkages to mental health services, can also present barriers for primary care providers in treating PTSD.12
There have been no published randomized controlled trials (RCTs) of primary care-based treatment specifically for patients with PTSD.15 However, growing evidence suggests that such treatment is feasible. Two RCTs of injured trauma survivors, some of whom developed PTSD, found that collaborative care resulted in better outcomes than usual care.16,17 In Project IMPACT, which used a collaborative stepped-care approach that included antidepressant medication and problem-solving therapy for treating depression, PTSD patients responded more slowly than other patients,18 but had comparable long-term outcomes.19 A study of collaborative care based on the IMPACT model included computer-assisted cognitive-behavioral therapy and medication for patients with anxiety disorders.20 Effects for PTSD outcomes in PTSD patients were similar to effects in patients with other anxiety disorders, but were not statistically significant.
We conducted an RCT of collaborative care for PTSD in veterans treated in a VA medical facility. As a national healthcare system with a high percentage of PTSD patients,3 the VA offers a unique opportunity to study collaborative care. The VA launched a Primary Care-Mental Health Integration (PC-MHI) initiative in 2007 to implement collocated collaborative care or care management for PTSD, alcohol problems, and depression.21
Because collaborative care is effective for treating depression,22,23 we used the Three Component Model (3CM) of collaborative care.24 A prior study, RESPECT-D (Re-engineering Systems for the Primary Care Treatment of Depression),25 found that depressed patients who received 3CM reported greater satisfaction and had improved outcomes relative to patients who received usual care. The model consists of: (1) education and tools for primary care clinicians and staff; (2) telephone care management by a centrally located care manager to answer patient questions and promote treatment adherence; and (3) support from a psychiatrist who supervises care managers by telephone, provides consultation to primary care clinicians, and facilitates mental health referral.
3CM has now been expanded to include content specific to PTSD. An implementation study conducted in the Army (RESPECT-Mil) for soldiers with PTSD and/or depression previously reported that the intervention was feasible and safe, and that patients who participated in follow-up calls had clinically meaningful improvement.26 We hypothesized that 3CM would result in improved symptoms and functioning, higher perceived quality of care, and higher likelihood of receiving medications or psychotherapy.
METHODS
An institutional review board at each site approved the protocol. Participants gave written informed consent prior to enrollment.
Participants
To be included, participants had to meet diagnostic criteria for PTSD, have regular access to a telephone, and speak English. Exclusion criteria were cognitive impairment, history of psychosis or mania, prominent current suicidal ideation, current substance dependence, and current engagement in mental health treatment (defined as a mental health visit within the prior 3 months or scheduled within the next month).27
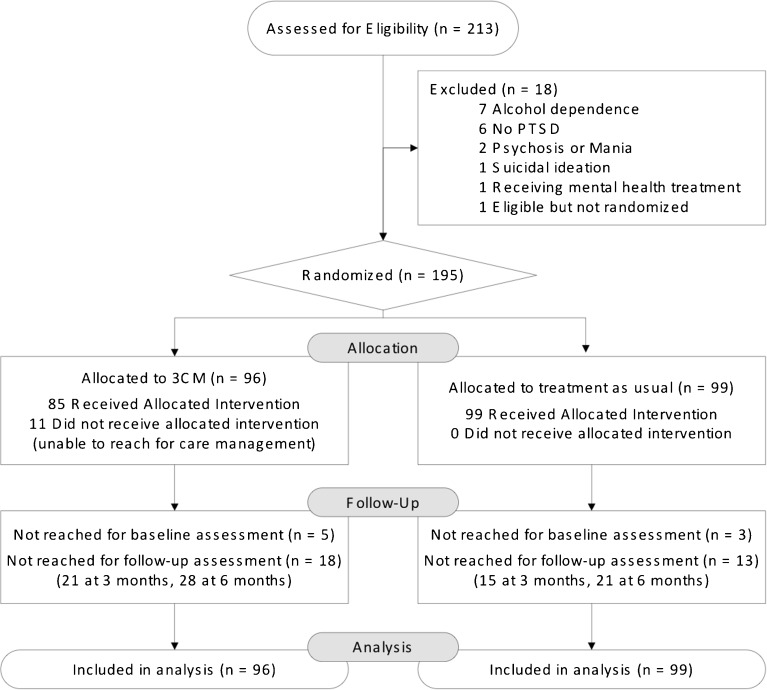
Of 214 veterans referred to the study, 213 were assessed and 195 (91.5%) were randomized, 96 to 3CM and 99 to usual care (Fig. 1). A sample size of 200 was projected to yield .80 power in mixed-model analysis to find a standardized mean difference of .40, assuming α = .05, two-tailed. A data entry error led to enrollment of eight participants meeting only partial PTSD criteria. We retained these participants in our analyses because sensitivity analyses excluding them showed no differences in findings.
Figure 1.
CONSORT flowchart.
Measures
PTSD diagnosis was confirmed by the Composite International Diagnostic Interview (CIDI), which also was used to assess lifetime trauma exposure.28 The PHQ-9 was used to assess comorbid depression.29 As in RESPECT-D, patients were assumed to be cognitively intact unless they did not know their age or address. If not, we administered a brief six-item cognitive impairment screen.30 We used the AUDIT-C31 to assess alcohol problems and the ten-item DAST32 to assess drug problems.
The primary outcome was PTSD symptom severity. Because care managers in 3CM administered the PTSD Checklist (PCL)33 during their calls with patients, we used a different questionnaire, the Posttraumatic Diagnostic Scale (PDS),34 to assess outcome. The PDS consists of brief questions to establish trauma exposure and anchor questions about the 17 DSM-IV symptoms of PTSD (rated on a 0–3 frequency scale). Other patient outcomes included the Hopkins Symptom Checklist-2035 to measure depression (as in RESPECT-D) and the SF-12, to measure physical and mental health functioning.36 Perceived quality of PTSD care and overall care was measured on a 5-point scale, but categorized for analysis as 1 = excellent/very good and 0 = good, fair, or poor.25
We obtained process of care information for all VA-funded utilization that occurred within 6 months after randomization. Because mental health referrals are not captured in VA administrative data, site coordinators abstracted referral data from electronic patient records. For other utilization data, a list of mental health outpatient clinics and inpatient treating specialties, developed in consultation with VA psychologists and clinical managers, was used to classify services as mental health or not. We located outpatient visits with psychotherapy through current procedural technology codes. Antidepressants were identified using a drug-class variable in the VA Decision Support System. We used this information to create the following categorical variables: any filled antidepressant, antidepressant refill for >75% of prescribed days, any mental health visit, any psychotherapy visit, and ≥9 psychotherapy visits in 15 weeks, which has been used as an indicator of frequency necessary for receipt of evidence-based treatment.37 We also used this information to count number of days from study enrollment to first mental health visit, number of psychotherapy visits, and total number of mental health visits.
We determined the cost of VA-funded care for outpatient visits, outpatient pharmacy, inpatient care (including pharmacy), and fee-for-service care provided outside the VA system through the Fee Basis program. The estimated cost of each service was extracted from the VA Decision Support System. Fee Basis records provided the actual payment to non-VA providers for each service. The cost of the 3CM intervention is included in the cost of outpatient visits. We report costs in 2010 dollars following adjustment for inflation using the Consumer Price Index.
Procedure
Recruitment and follow-up occurred from March 2008 through April 2010, at five primary care clinics at four VA Medical Centers in central and north Texas. These sites were selected because they had a high volume of primary care patients and had not implemented a PC-MHI program.
Primary care providers (or other clinical staff who were responsible for routine PTSD screening) referred patients to the study. Patients were considered potentially eligible if they responded “yes” to at least three items on the four-item Primary Care PTSD Screen (PC-PTSD)38 during screening or if they presented with PTSD symptoms. A site coordinator contacted patients who expressed interest in participating and consented them before determining eligibility.
If a patient met eligibility criteria, the site coordinator arranged for a centrally located, blinded independent assessor (a masters-level or doctoral-level clinician) to administer the 15–20 min baseline assessment by telephone. The assessment was administered within 2 weeks of the eligibility interview, and 3 and 6 months following enrollment. The Assessor reached 187 participants (96%) for the baseline assessment; 164 participants (84%) had at least two assessments.
The study was a two-arm, parallel randomized clinical trial. Participants were randomized to 3CM or usual care. Randomization codes were provided to site coordinators by a centralized data-coordinating center through a web portal. Site coordinators called participants or delivered the information in person to those assessed at the initial visit. Randomization was stratified by site. We randomized individual participants (rather than clinicians or clinics), following the approach used in other large studies of collaborative care.39
All primary care providers received an initial one-hour training on PTSD that included information about diagnostic criteria, assessment (including tools such as the PCL), and treatment. Refresher sessions were offered at four of the five participating sites. We did not formally evaluate provider knowledge. Evaluation data available from 42 providers before training and 33 afterward indicated the training led to increased knowledge and confidence, e.g., the percentage of providers who said they were very or mostly confident they could manage PTSD was 11% before training and 40% after training. Educational materials for providers and patient handouts were available at the initial training and during the trial.
Treatment in 3CM and usual care was at the provider’s discretion and could include referral to mental health specialty care. Participants assigned to 3CM received telephone support calls from one of two centrally located care managers, both doctoral-level psychologists. Calls were scheduled to last 15 min and were used to identify barriers to adherence with the primary care provider’s management plan, help the patient to overcome them, and measure treatment response. Calls occurred 1, 4, and 8 weeks after the initial visit, and then every 4 weeks for 6 months or until a participant achieved a 30% reduction in PTSD symptoms on the PCL.33 Participants who did not meet this criterion by 6 months were referred to mental health. Although the study focused on PTSD, care managers also monitored depression using the PHQ-929 for any participant who had depression; for these participants, we used a 30% reduction in PCL scores and 50% reduction in PHQ-9 scores as a target for response. In analyses conducted for this study, a 5-point change on the PCL corresponded to clinically significant change in data from an RCT of PTSD treatment in veterans.40 Five points indicates clinically significant change on the PHQ-9.29
Care managers discussed participant contacts with three centrally located psychiatrists during weekly supervision calls. After each call, care managers informed providers about participants’ progress, including PCL (and PHQ-9) scores and care management actions, by entering information in the electronic medical record system. To ensure that the information was received, providers had to sign off on all notes.
Fidelity to the 3CM protocol was monitored by a measure developed in the RESPECT-D trial41 to reflect 10 essential 3CM process of care components. Because providers did not have to assess PTSD, we adapted the component on patient engagement to measure engagement in care management rather than physician–patient engagement. Fifty-one participants (53.1%) had high-fidelity care (defined as above the median),41 34 (35.4%) had low-fidelity care (defined as below the median and above 0), and 11 (11.5%) had no 3CM care because the care manager could not reach them. Scores ranged from 25.7 to 79.3 in the low fidelity group and 83.5–100.0 in the high fidelity group. Median 6-month fidelity was 79.3 out of a possible 100 among participants with a non-zero score.
Statistical Analysis
The study biostatistician (JG) performed all analyses. Baseline characteristics were compared using χ2 or t-tests. Primary analyses were performed on the intention-to-treat sample, using data from all randomized participants. We used Multivariate Imputation by Chained Equations (MICE)42 to impute missing values for all outcomes except perceived quality of PTSD care and overall care. This method involves specifying a multivariate distribution for the missing data, and drawing imputation from their conditional distributions by Markov chain Monte Carlo techniques. We did not impute ratings of perceived quality of care, because a large number of participants did not provide ratings of PTSD care (67 of 159 respondents at 3 months and 81/147 at 6 months). Over 90% of these participants chose a response option indicating that they did not have any PTSD care, even though examination of their utilization data indicated that that was not the case. For comparability, we did not impute ratings of overall care, although only five participants at 3 months and three participants at 6 months did not rate their overall care.
Outcomes were analyzed using the Generalized Linear Mixed Model (R; available from http://cran.r-project.org/). We estimated the main effect of treatment across the 3-month and 6-month assessments while adjusting for site and the site by treatment interaction as covariates, using identity linkage and the Gaussian family for continuous outcomes and logarithmic linkage and the binomial family for dichotomous outcomes. For longitudinal outcomes, the correlation within participants introduced from repeated measurement at different time points was treated as a random effect in the Mixed Effect model. We used Wald tests to determine the significance of the adjusted treatment effect.
RESULTS
The typical patient was a white man in his mid-40s with some post-secondary education (Table 1). About half were employed full or part-time. Less than 20% were receiving disability compensation for PTSD, and 60% had never applied. Seventy percent had current comorbid depression. Average levels of alcohol and drug problems were low. The 3CM and usual care groups did not differ at baseline, except that 3CM participants were more likely to have witnessed trauma (p < .05).
Table 1.
Sample Description (N = 195)
| 3CM (N = 96) | Usual Care (N = 99) | |||
|---|---|---|---|---|
| Mean or N | % or 95 % CI | Mean or N | % or 95 % CI | |
| Female gender | 7 | 7.3 % | 10 | 10.1 % |
| Age (years) | 46.1 | 43.1–49.1 | 44.4 | 41.3–47.5 |
| Post-high school education | 66 | 68.8 % | 70 | 70.7 % |
| Employment status: Working | 47 | 49.0 % | 49 | 49.5 % |
| Unemployed | 24 | 25.0 % | 27 | 27.3 % |
| Retired | 25 | 26.0 % | 23 | 23.2 % |
| Married/cohabitating | 53 | 55.2 % | 55 | 55.6 % |
| Race: White, non-Hispanic | 55 | 57.3 % | 55 | 55.6 % |
| Black, non-Hispanic | 21 | 21.9 % | 22 | 22.2 % |
| Hispanic | 15 | 15.6 % | 15 | 15.2 % |
| Other | 5 | 5.2 % | 7 | 7.1 % |
| Era*: Vietnam War | 42 | 43.8 % | 39 | 39.4 % |
| Gulf War | 16 | 16.7 % | 16 | 16.2 % |
| Iraq or Afghanistan Wars | 38 | 39.6 % | 40 | 40.4 % |
| Peacetime only | 7 | 7.3 % | 9 | 9.1 % |
| Number of lifetime traumatic event types (of 10) | 4.7 | 4.4–5.1 | 4.4 | 4.1–4.7 |
| Combat exposure | 73 | 76.0 % | 70 | 70.7 % |
| Rape | 11 | 11.5 % | 6 | 6.1 % |
| Sexual assault | 18 | 18.8 % | 16 | 16.2 % |
| Physical assault | 51 | 51.3 % | 50 | 50.5 % |
| Life-threatening accident | 68 | 70.8 % | 68 | 68.7 % |
| Disaster | 40 | 41.7 % | 29 | 29.3 % |
| PTSD disability: Approved | 17 | 17.7 % | 14 | 14.1 % |
| Pending | 14 | 14.6 % | 21 | 21.2 % |
| Denied | 4 | 4.2 % | 6 | 6.1 % |
| Never applied | 61 | 63.5 % | 58 | 58.6 % |
| Approved PTSD disability % (N = 31) | 60.3 | 44.3–76.3 | 56.0 | 36.2–75.8 |
| Current Major Depression | 64 | 66.7 % | 73 | 73.7 % |
| Patient Health Questionnaire-9 | 15.8 | 14.7–16.9 | 16.3 | 15.2–17.5 |
| Alcohol problems (Alcohol Use Disorders Identification Test-C) | 2.3 | 1.8–2.8 | 2.5 | 2.1–3.0 |
| Drug problems (Drug Abuse Screening Test) | 0.2 | 0.1–0.3 | 0.1 | 0.0–0.3 |
3CM Three Component Model. T-tests were used for continuous variables and χ2 tests for categorical variables. *Percentages may add to >100 % because some veterans served in multiple eras
There were five serious adverse events (SAEs) in 3CM and four in usual care. In 3CM, three of the SAEs were for hospitalizations for unrelated medical problems and two were for psychiatric hospitalizations. Both psychiatric hospitalizations were for the same individual and occurred after the eligibility interview, but before randomization. In usual care, the four SAEs were for unrelated medical hospitalizations. The reasons for medical hospitalizations included previously arranged back surgery, fluid retention, and angioplasty. No events were study-related.
Intention-to-Treat Analyses
PTSD symptoms improved over time (p < .001), although the amount of change was small. There were no differences between 3CM and usual care (Table 2). To understand the lack of difference, we performed exploratory analyses to examine the relationship between symptom change and fidelity to the 3CM model. Fidelity was unrelated to improvement in PTSD from baseline to 6 months (r = −.10). Remission at 6 months occurred in 7.8% of participants who received high fidelity care, 5.9% of who received low fidelity care, and 9.1% who received no 3CM care.
Table 2.
Symptom Outcomes as a Function of Treatment Group (N = 195)
| Pretreatment | 3 Months | 6 Months | Adjusted Mean Difference* (95 % CI) | P | ||||
|---|---|---|---|---|---|---|---|---|
| 3CM | Usual Care | 3CM | Usual Care | 3CM | Usual Care | |||
| PTSD Diagnostic Scale | 33.2 (8.3) | 34.0 (9.7) | 31.4 (10.2) | 31.5 (10.3) | 30.2 (10.3) | 29.9 (10.8) | −0.6 (−4.7, 3.5) | 0.79 |
| Hopkins Symptom Checklist Depression Scale | 1.98 (0.69) | 2.06 (0.78) | 1.80 (0.80) | 1.84 (0.82) | 1.81 (0.84) | 1.83 (0.90) | 0.0 (−0.3, 0.3) | 0.98 |
| SF-36 Mental Component | 33.8 (8.8) | 32.7 (8.1) | 33.9 (8.3) | 33.8 (8.1) | 33.7 (9.4) | 33.4 (8.1) | 0.4 (−2.9, 3.8) | 0.79 |
| SF-36 Physical Component | 42.2 (13.0) | 43.4 (12.6) | 43.8 (13.1) | 43.7 (12.2) | 44.4 (12.6) | 44.8 (11.8) | −1.7 (−7.2, 3.7) | 0.53 |
| Adjusted OR* (95 % CI) | ||||||||
| Perceived quality of PTSD care (N = 102) | – | – | 0.5 (0.51) | 0.59 (0.50) | 0.47 (0.51) | 0.48 (0.51) | 0.11 (0.02, 0.77) | 0.03 |
| Perceived quality of VA care (N = 163) | – | – | 0.68 (0.47) | 0.68 (0.47) | 0.64 (0.48) | 0.64 (0.48) | 0.77 (0.15, 4.05) | 0.76 |
3CM Three Component Model. Means are presented as mean (SD). *Adjusted for time, site, and the treatment X site interaction
Depression symptoms and physical functioning also improved over time (p < .001), but as was the case for PTSD, the magnitude of change was small and there were no differences between 3CM and usual care. There was no improvement in mental functioning or differences between groups. Among participants who provided a numeric rating of PTSD care, half rated it as excellent or very good. However, to our surprise, 3CM was associated with lower perceived quality of PTSD care. Almost two-thirds of participants rated their overall care as excellent or very good, and the groups did not differ.
Table 3 presents information about the process of mental health care. Participants assigned to 3CM were more likely to fill an antidepressant prescription (p = .05) or have a refill for 75% of prescribed days. 3CM participants also were more likely to have a mental health visit and to have a higher number of mental health visits. The groups did not differ on other measures of process of care. Almost 40% of participants were referred to mental health and 75% had a mental health visit, on average, within 2–3 weeks of enrollment. (The percentage of use is greater than the percentage of referral, because participants did not need a referral from primary care to access mental health treatment.) Costs were similar for both groups, except participants assigned to 3CM had higher outpatient pharmacy costs (Table 4).
Table 3.
Process of Care Outcomes as a Function of Treatment Group (N = 194)
| 3CM | Usual Care | Adjusted OR* (95 % CI) | P | |||
|---|---|---|---|---|---|---|
| N | % | N | % | |||
| Any filled antidepressant | 80 | 83.3 % | 65 | 65.7 % | 3.2 (1.0, 10.2) | 0.05 |
| Antidepressant refill for 75 % of prescribed days | 55 | 57.3 % | 47 | 49.0 % | 3.0 (1.1, 8.2) | 0.03 |
| Referred to mental health | 38 | 39.6 % | 37 | 37.4 % | 2.4 (0.9, 6.5) | 0.09 |
| Any mental health visit | 73 | 76.0 % | 73 | 73.7 % | 9.1 (1.1, 77.7) | 0.04 |
| Any psychotherapy visit | 53 | 55.2 % | 53 | 53.5 % | 2.4 (0.9, 6.5) | 0.09 |
| ≥9 psychotherapy visits in 15 weeks | 8 | 8.3 % | 6 | 6.1 % | 2.3 (0.2, 26.1) | 0.51 |
| M | SD | M | SD | Adjusted Mean Difference* (95 % CI) | P | |
| Days to first mental health visit | 13.14 | 21.40 | 24.10 | 41.80 | −9.5 (−24.8, 5.8) | 0.23 |
| Total number of psychotherapy visits | 4.26 | 4.49 | 4.23 | 6.77 | 0.9 (−2.6, 4.4) | 0.62 |
| Total number of mental health visits | 8.26 | 6.62 | 4.70 | 8.30 | 4.5 (0.8, 8.3) | 0.02 |
3CM Three Component Model. *Adjusted for site and the treatment X site interaction
Table 4.
Average Cost of Care Per Patient as a Function of Treatment Group (N = 194)
| 3CM | Usual Care | Adjusted Mean Difference* | 95 % CI | P | |||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | ||||
| Outpatient visits | 3,984.8 | 3,277.6 | 2,620.3 | 2,997.8 | 1,152.0 | −293.4, 2,957.5 | 0.12 |
| Outpatient pharmacy | 439.7 | 547.4 | 304.3 | 394.2 | 386.4 | 168.3, 604.5 | <0.001 |
| Inpatient stays | 1,420.4 | 11,096.6 | 316.5 | 2,234.8 | −822.3 | −4,616.5, 2971.9 | 0.67 |
| VA-funded FFS | 156.8 | 686.0 | 271.8 | 1,547.0 | 236.8 | −335.9, 809.5 | 0.42 |
| Total cost | 6,001.7 | 12,357.4 | 3,512.9 | 4,583.5 | 953.0 | −3.449.2, 5,355.2 | 0.67 |
3CM Three Component Model. N = 194 because utilization data for one participant would not be identified definitively. FFS fee-for-service (Fee Basis program). Costs are reported in 2010 dollars following adjustment for inflation using the Consumer Price Index. *Adjusted for site and the treatment X site interaction
DISCUSSION
Our study demonstrates the difficulty of translating successful collaborative care for primary care depression to treating PTSD in primary care. Over a 6-month period, primary care patients with PTSD in both 3CM and usual care groups did not show clinically significant improvement in PTSD, depression, or functioning. We did not find any additional benefit for participants assigned to 3CM, despite the fact that they were more likely to receive an antidepressant and had more mental health care. The lack of difference in symptoms and functioning may be because of difficulty in establishing the treatment of PTSD as part of a primary care clinician’s job, as well as the chronicity and severity of PTSD in VA patients.
Several findings suggest that convincing primary care providers to treat PTSD is difficult. The baseline confidence in treating PTSD by primary care clinicians was much lower than that reported for treating depression.23 Thus, it is not surprising that the rate of referral to specialty mental health in 3CM was much higher than that usually seen in collaborative care for depression.25 Because providers did not have to identify or diagnose PTSD, we had to adapt the fidelity scale41 to measure patient engagement in care management rather than physician-patient engagement. Even with this change (and good fidelity to care management), fidelity scores were lower than those reported for depression. Median fidelity at 6 months was only 79.3 versus 87.1 in RESPECT-D.41 3CM might have been more effective if fidelity had included greater primary care clinician involvement in assessment and diagnosis, one of the key elements in 3CM.
Substantial improvement in the usual care group does not explain the findings. Change over time in both groups was statistically, but not clinically, significant—despite the fact that almost 40% of participants were referred to mental health and 75% had a mental health visit, typically within 2–3 weeks of entering the trial. Although half of the participants had an antidepressant refill for more than 75% of prescribed days, less than 10% had enough psychotherapy visits to have received an evidence-based treatment.37 The lower perceived quality of PTSD care in 3CM may have been due to greater exposure of 3CM patients to care that was not helping them improve. 3CM might have been more effective if care coordination had been able to help more patients receive an adequate course of medication or more psychotherapy visits. Also, lack of clinical benefit for patients assigned to 3CM, despite their greater likelihood of receiving adequate antidepressant refills, may be due to the fact that the effects of medication on PTSD are relatively modest when compared with the effects of psychotherapy.9,43
It would be premature to conclude from our study that 3CM is not effective for treating PTSD in primary care patients. Findings from RESPECT-Mil, a large implementation study of 3CM in Army soldiers, suggest that those who participated in the program benefitted substantially.26 Although RESPECT-Mil does not have a comparison group, the magnitude of change among its participants is much greater than we observed. The greater improvement may be due to the fact that they were treated at an earlier stage of PTSD, before it became as chronic as it is in many VA patients. For example, a study of collaborative depression care conducted in the VA found that comorbid PTSD was associated with more severe depression, additional comorbidity, lower social support, and greater use of specialty mental health care and antidepressants—all indications that PTSD patients in VA primary care settings may be challenging to treat relative to other primary care patients with mental disorders.44,45 The severity and comorbidity in VA PTSD patients have been cited as reasons for smaller effects of evidence based PTSD treatment in this population.43,46
It also would be premature to conclude from our study or from existing evidence that collaborative care is not effective for managing PTSD. Research is at an early stage, e.g., a randomized trial of stepped care for acute PTSD is underway.47 One challenge is the feasibility of delivering evidence-based psychotherapy for PTSD.8,9 Care management and mental health support can facilitate medication management and referral to specialty mental health, but the effective psychotherapies require 10–12 weekly sessions of 60–90 min each, which is lengthy for a primary care setting. However, evidence suggesting the effectiveness of briefer cognitive-behavioral treatments delivered by co-located behavioral health specialists is emerging.15,48 Blended models that combine care management, mental health support, and co-located behavioral health specialists who interact with primary care providers and care managers in-person may be required to treat severe and chronic PTSD in order to offer both psychotherapy and medication management. Although a recent trial of a blended model for treating anxiety disorders failed to find benefits for PTSD patients, the effect size for PTSD was comparable to the effect sizes for patients with other disorders.19
Several limitations should be considered when evaluating our results. Findings may not generalize to active duty or nonmilitary populations, or to women (because most participants were men). Also, information about utilization and costs may be generalized to VA sources only. The high rate of referral and mental health utilization is another limitation. Findings may not generalize to settings where access to mental health care is lower. Lastly, outcomes may have differed if we had continued the intervention longer, e.g., 12 months as in IMPACT27 and other studies of collaborative care for depression.22,23
Our results suggest the need for careful examination of how collaborative care models for PTSD are implemented, and for additional supports to encourage primary care providers to manage PTSD. Whereas many providers feel responsible for managing depression49 and have confidence in their skills to do so,50 there are gaps in knowledge and confidence about PTSD.10–12 More than provider education will be needed to address these gaps. As with depression,49 providers probably need to have successful experiences in treating PTSD with back-up from mental health specialists encouraging use of evidence-based treatments. Ultimately, the optimal strategy for managing PTSD in primary care settings is likely to depend on patient, provider, and system factors.12
Acknowledgments
This study was funded by the VA Health Services Research and Development Service. However, the views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs or any US government agency.
We wish to thank the Site Principal Investigators Dzung V. Le, DO, Praveen Mehta, MD, Guna Raj, MD, Immanuel Thamban, MD, and Edwin Woo, MD and research staff (David S. Greenawalt, PhD, Kathy McNair, RN, Lisa D. Jones, Reed J. Robinson, PhD, Jack Y. Tsan, PhD, and Elizabeth S. Wiley, PhD). We also wish to thank Shelia Barry, Allison Brandt, MBA, Shuo Chen, PhD, Suzy B. Gulliver, PhD, Kathryn Kotrla, MD, Carol S. North, MD, Jeffrey Smith, PhD, John Williams, MD, Keith A. Young, PhD, and Yinong Young-Xu, DSc, for valuable assistance in planning or in implementing the study, and Charles C. Engel, MD for helpful discussions about the study findings.
Conflict of Interest
Dr. Schnurr has provided consultation and content development on PTSD for Medscape. Oxman & Dietrich are partners in 3CM, LLC, a consultant group based on their work for the MacArthur Foundation in order to disseminate their work on integrating mental health in primary care. They primarily work with the U.S. Army, but have also worked with Aetna, the University of Miami and the New York City Dept. of Health and Mental Hygiene. Dr. Smith is employed by Thomson Reuters. All other authors have no conflicts to declare.
Footnotes
Trial Registration
Clinicaltrials.gov Identifier NCT00373698
REFERENCES
- 1.Diagnostic and statistical manual of mental disorders. Washington: American Psychiatric Association; 1994. [Google Scholar]
- 2.Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Magruder KM, Frueh BC, Knapp RG, et al. Prevalence of posttraumatic stress disorder in Veterans Affairs primary care clinics. Gen Hosp Psychiatry. 2005;27:169–179. doi: 10.1016/j.genhosppsych.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 4.Schnurr PP, Green BL, editors. Trauma and Health: Physical Health Consequences of Exposure to Extreme Stress. Washington: American Psychological Association; 2004. [Google Scholar]
- 5.National Comorbidity Survey-Replication. Lifetime prevalence of DSM-IV/WMH-CIDI disorders by sex and cohort. Available at: http://www.hcp.med.harvard.edu/ncs/ftpdir/NCS-R_Lifetime_Prevalence_Estimates.pdf. Accessed June 22, 2012.
- 6.Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New Engl J Med. 2004;351:13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- 7.Prigerson HG, Maciejewski PK, Rosenheck RA. Combat trauma: trauma with highest risk of delayed onset and unresolved posttraumatic stress disorder symptoms, unemployment, and abuse among men. J Nerv Ment Dis. 2001;189:99–108. doi: 10.1097/00005053-200102000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Department of Veterans Affairs and Department of Defense. VA/DoD Clinical Practice Guideline for Management of Posttraumatic Stress. http://www.healthquality.va.gov/Post_Traumatic_Stress_Disorder_PTSD.asp. Accessed June 22, 2012.
- 9.Foa EB, Keane TM, Friedman MJ, Cohen JA. Effective treatments for PTSD. 2. New York: Guilford; 2008. [Google Scholar]
- 10.Wang PS, Berglund P, Olfson M, et al. Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:603–613. doi: 10.1001/archpsyc.62.6.603. [DOI] [PubMed] [Google Scholar]
- 11.Liebschutz J, Saitz R, Brower V, et al. PTSD in urban primary care: high prevalence and low physician recognition. J Gen Intern Med. 2007;22:719–726. doi: 10.1007/s11606-007-0161-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meredith LS, Eisenmann DP, Green BL, et al. System factors affect the recognition and management of posttraumatic stress disorder by primary care clinicians. Med Care. 2009;47:686–694. doi: 10.1097/MLR.0b013e318190db5d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Possemato K, Ouimette P, Lantinga LA, et al. Treatment of Department of Veterans Affairs primary care patients with posttraumatic stress disorder. Psychol Serv. 2011;8:82–93. doi: 10.1037/a0022704. [DOI] [Google Scholar]
- 14.Mohammed S, Rosenheck R. Pharmacotherapy for older veterans diagnosed with posttraumatic stress disorder in Veterans Administration. Am J Geriatr Psychiatry. 2008;16:804–812. doi: 10.1097/JGP.0b013e318173f617. [DOI] [PubMed] [Google Scholar]
- 15.Possemato K. The current state of intervention research for posttraumatic stress disorder within the primary care setting. J Clin Psychol Med Settings. 2011;18:268–280. doi: 10.1007/s10880-011-9237-4. [DOI] [PubMed] [Google Scholar]
- 16.Zatzick D, Roy-Byrne P, Russo J, et al. Collaborative interventions for physically injured trauma survivors: a pilot randomized effectiveness trial. Gen Hosp Psychiatry. 2001;23:114–123. doi: 10.1016/S0163-8343(01)00140-2. [DOI] [PubMed] [Google Scholar]
- 17.Zatzick D, Roy-Byrne P, Russo J, et al. A randomized effectiveness trial of stepped collaborative care for acutely injured trauma survivors. Arch Gen Psychiatry. 2004;61:498–506. doi: 10.1001/archpsyc.61.5.498. [DOI] [PubMed] [Google Scholar]
- 18.Hegel M, Unützer J, Tang L, et al. Impact of comorbid panic and posttraumatic stress disorder on outcomes of collaborative care for late-life depression in primary care. Am J Geriatr Psychiatry. 2005;13:48–58. doi: 10.1176/appi.ajgp.13.1.48. [DOI] [PubMed] [Google Scholar]
- 19.Chan D, Fan M-Y, Unützer J. Long-term effectiveness of collaborative depression care in older primary care patients with and without PTSD symptoms. Int J Geriatr Psychiatry. 2011;26:758–764. doi: 10.1002/gps.2606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Craske MG, Stein MB, Sullivan G, et al. Disorder-specific impact of coordinated anxiety learning and management treatment for anxiety disorder in primary care. Arch Gen Psychiatry. 2011;68:378–388. doi: 10.1001/archgenpsychiatry.2011.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Post EP, Metzger M, Dumas P, et al. Integrating mental health into primary care within the Veterans Health Administration. Fam Syst Health. 2010;28:83–90. doi: 10.1037/a0020130. [DOI] [PubMed] [Google Scholar]
- 22.Bower P, Gilbody S, Richard D, et al. Collaborative care for depression in primary care: making sense of a complex intervention: systematic review and meta-regression. Br J Psychiatry. 2006;189:484–493. doi: 10.1192/bjp.bp.106.023655. [DOI] [PubMed] [Google Scholar]
- 23.Williams J, Gerrity M, Holsinger T, et al. Systematic review of multifaceted interventions to improve depression care. Gen Hosp Psychiatry. 2007;29:91–116. doi: 10.1016/j.genhosppsych.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 24.Oxman TE, Dietrich AJ, Williams JW, et al. A three-component model for reengineering systems for the treatment of depression in primary care. Psychosomatics. 2002;43:441–450. doi: 10.1176/appi.psy.43.6.441. [DOI] [PubMed] [Google Scholar]
- 25.Dietrich AJ, Oxman TE, Williams JW, et al. Re-engineering systems for the treatment of depression in primary care: cluster randomized controlled trial. Br Med J. 2004;329:602–605. doi: 10.1136/bmj.38219.481250.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Engel CC, Oxman T, Yamamoto C, et al. RESPECT-Mil: feasibility of a systems-level collaborative care approach to depression and posttraumatic stress disorder in military primary care. Mil Med. 2008;173:935–940. doi: 10.7205/milmed.173.10.935. [DOI] [PubMed] [Google Scholar]
- 27.Unützer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting. A randomized controlled trial. JAMA. 2002;288:2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 28.Kessler RC, Ustun TB. The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Meth Psychiatr Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Callahan CM, Unverzagt FW, Hui SL, et al. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40:771–781. doi: 10.1097/00005650-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 31.Bradley KA, Kivlahan DR, Zhou XH, et al. Using alcohol screening results and treatment history to assess the severity of at-risk drinking in Veterans Affairs primary care patients. Alc Clin Exp Res. 2004;28:448–455. doi: 10.1097/01.ALC.0000117836.38108.38. [DOI] [PubMed] [Google Scholar]
- 32.Skinner H. The drug abuse screening test. Add Beh. 1982;7:363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- 33.Weathers FW, Litz BT, Herman DS, et al. PTSD Checklist: reliability, validity, and diagnostic utility. In: Proceedings of the 9th Annual Meeting of the International Society for Traumatic Stress Studies (ISTSS). Chicago, Ill: ISTSS; 1993:8.
- 34.Foa EB, Cashman L, Jaycox L, et al. The validation of a self-report measure of posttraumatic stress disorder: the Posttraumatic Diagnostic Scale. Psychol Assess. 1997;9:445–451. doi: 10.1037/1040-3590.9.4.445. [DOI] [Google Scholar]
- 35.Derogatis LR, Lipman RS, Covi L. SCL-90: an outpatient psychiatric rating scale – preliminary report. Psychopharm Bull. 1973;9:13–28. [PubMed] [Google Scholar]
- 36.Seal KH, Maguen S, Cohen B, et al. VA mental health services utilization in Iraq and Afghanistan veterans in the first year of receiving new mental health diagnoses. J Trauma Stress. 2010;23:5–16. doi: 10.1002/jts.20493. [DOI] [PubMed] [Google Scholar]
- 37.Gandek B, Ware JE, Aaronson NK, et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. J Clin Epidemiol. 1998;51:1171–1178. doi: 10.1016/S0895-4356(98)00109-7. [DOI] [PubMed] [Google Scholar]
- 38.Prins A, Ouimette P, Kimerling R, et al. The Primary Care PTSD Screen (PC-PTSD): development and operating characteristics. Prim Care Phys. 2003;9:9–14. doi: 10.1185/135525703125002360. [DOI] [Google Scholar]
- 39.Gilbody S, Bower P, Torgerson D, et al. Cluster randomized trials produced similar results to individually randomized trials in a meta-analysis of enhanced care for depression. J Clin Epidemiol. 2008;61:160–168. doi: 10.1016/j.jclinepi.2007.04.015. [DOI] [PubMed] [Google Scholar]
- 40.Schnurr PP, Friedman MJ, Foy DW, et al. A randomized trial of trauma focus group therapy for posttraumatic stress disorder: results from a Department of Veterans Affairs Cooperative Study. Arch Gen Psychiatry. 2003;60:481–489. doi: 10.1001/archpsyc.60.5.481. [DOI] [PubMed] [Google Scholar]
- 41.Oxman TE, Schulberg HC, Greenberg RL, et al. A fidelity measure for integrated management of depression in primary care. Med Care. 2006;44:1030–1037. doi: 10.1097/01.mlr.0000233683.82254.63. [DOI] [PubMed] [Google Scholar]
- 42.van Buuren S, Oudshoorn K. MICE: Multivariate imputation by chained equations in R. J Statistical Software, in press.
- 43.Bradley RG, Greene J, Russ E, et al. A multidimensional meta-analysis of psychotherapy for PTSD. Am J Psychiatry. 2005;162:214–227. doi: 10.1176/appi.ajp.162.2.214. [DOI] [PubMed] [Google Scholar]
- 44.Campbell DG, Felker BL, Liu C-F, et al. Prevalence of depression-PTSD comorbidity: implications for clinical practice guidelines and primary care-based interventions. J Gen Intern Med. 2007;22:711–718. doi: 10.1007/s11606-006-0101-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chan D, Cheadle AD, Reiber G, et al. Health care utilization and its costs for depressed veterans with and without comorbid PTSD Symptoms. Psychiatr Serv. 2009;60:1612–1617. doi: 10.1176/appi.ps.60.12.1612. [DOI] [PubMed] [Google Scholar]
- 46.Friedman MJ, Marmar CR, Baker DG, et al. Randomized, double-blind comparison of sertraline and placebo for posttraumatic stress disorder in a Department of Veterans Affairs setting. J Clin Psychiatry. 2007;68:711–720. doi: 10.4088/JCP.v68n0508. [DOI] [PubMed] [Google Scholar]
- 47.Zatzick D, Rivara F, Jurkovich G, et al. Enhancing the population impact of collaborative care interventions: mixed method development and implementation of stepped care targeting posttraumatic stress disorder and related comorbidities after acute trauma. Gen Hosp Psychiatry. 2011;33:123–134. doi: 10.1016/j.genhosppsych.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cigrang JA, Rauch SAM, Avila LL, et al. Treatment of active-duty military with PTSD in primary care: early findings. Psychol Serv. 2011;8:104–13.
- 49.Nutting PA, Gallacher KM, Riley K, et al. Implementing a depression improvement intervention in five health care organizations: experience from the RESPECT-Depression trial. Adm Policy Ment Health. 2007;34:127–137. doi: 10.1007/s10488-006-0090-y. [DOI] [PubMed] [Google Scholar]
- 50.Gerrity MS, Williams JW, Dietrich AJ, et al. Identifying physicians likely to benefit for depression education: a challenge for health care organizations. Med Care. 2001;39:856–866. doi: 10.1097/00005650-200108000-00011. [DOI] [PubMed] [Google Scholar]