Abstract
Background and Objectives
The causal relationship of clinically-significant atrioventricular block (AVB) and coronary artery disease (CAD) is uncertain. We investigated whether CAD is related to irreversible AVB that requires treatment with a permanent pacemaker.
Subjects and Methods
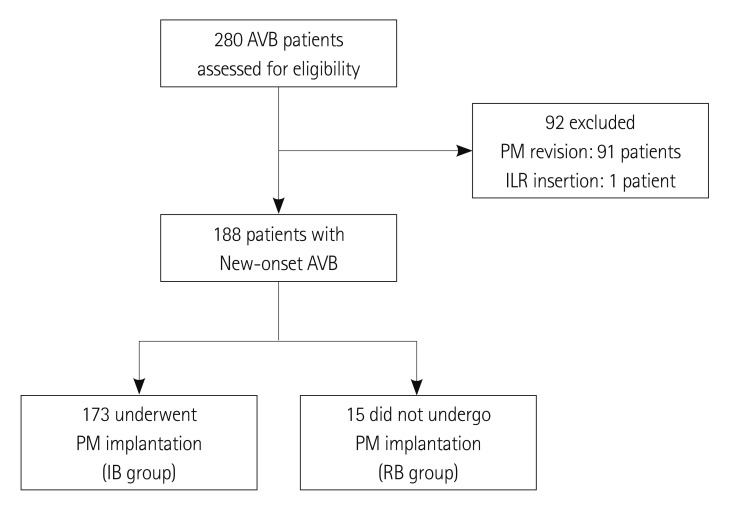
We included 188 consecutive patients with new-onset AVB considering pacemaker, who had undergone invasive or noninvasive coronary evaluation. Patients were divided into one of 2 groups: irreversible AVB who underwent implantation of permanent pacemaker {irreversible block (IB) group, n=173} or reversible AVB {reversible block (RB) group, n=15}.
Results
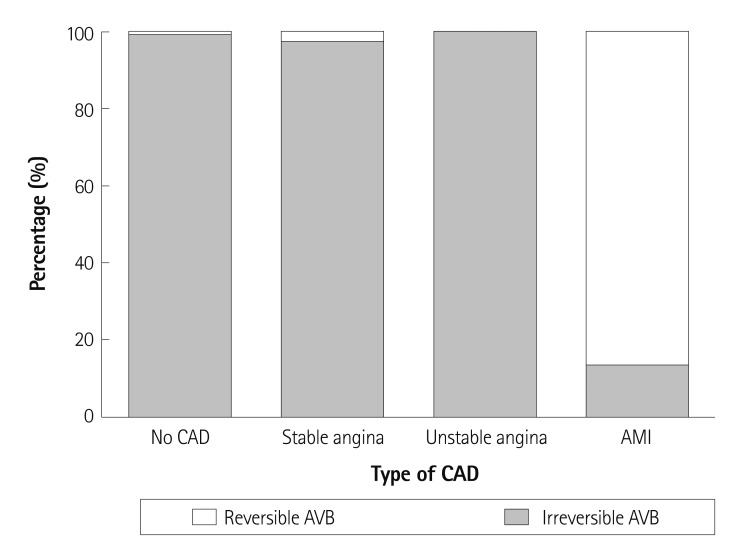
In IB group, significant CAD was observed in 44 patients (25.4%) and there were 2 (1.2%) patients with acute myocardial infarction (AMI). In RB group, 14 patients (93.3%) had CAD (p<0.001) and 13 patients (86.7%) presented with AMI (p<0.001). On the aspect of CAD type and reversibility of AVB, 13/15 (86.7%) patients of AMI, 0/2 (0%) of unstable angina, and 1/41 (2.4%) of stable angina had reversible AVB.
Conclusion
AVB in patients with AMI is usually reversible. Therefore, permanent pacemaker implantation should be delayed in cases of AMI. AVB in patients with CAD other than AMI is usually irreversible.
Keywords: Atrioventricular block; Coronary artery disease; Pacemaker, atrificial
Introduction
Permanent pacemaker implantation is one of the most important treatments for patients with clinically-significant atrioventricular block (AVB), but reversible causes should be evaluated and managed before considering pacemaker implantation.
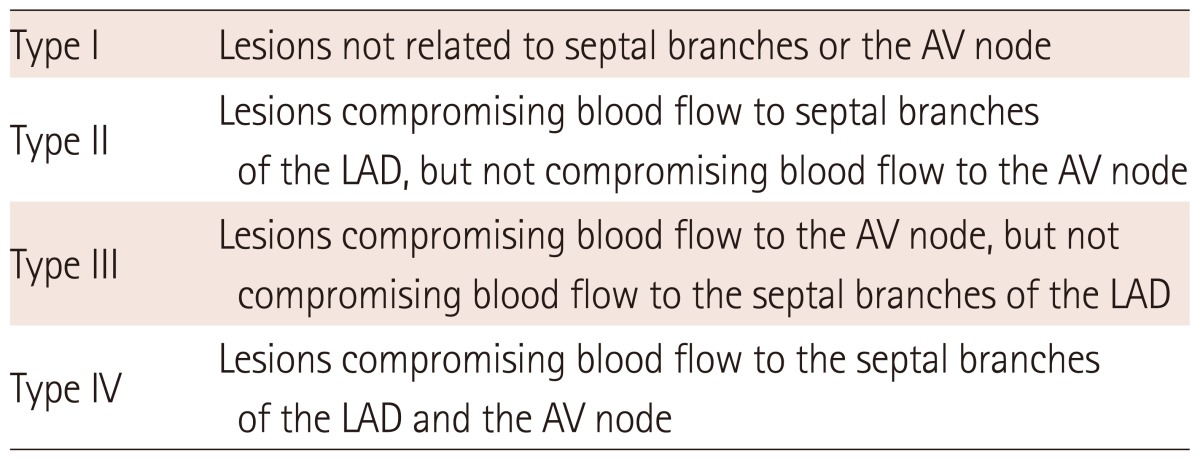
Coronary artery disease (CAD) is one of the possible causes of AVB. Mosseri et al.1) reported that conduction disturbances were more frequent in patients with compromised blood flow of the septal branches after coronary artery bypass grafting (CABG) operation. They analyzed the association of conduction disturbance and the location of CAD in 43 patients, who had permanent pacemaker implantation and coronary angiography (CAG), by classifying coronary pathology into 4 categories (Table 1), and reported that compromised blood flow to septal branch and right coronary artery (RCA, type IV anatomy) was significantly associated with severe conduction disturbances.2) Henceforward, several studies reported the predominance of type II and type IV anatomy in patients with severe conduction disturbance.3),4)
Table 1.
Classification of pathological coronary anatomy supplying the conduction system
Classification of pathological coronary anatomy by Mosseri et al.2) AV: atrioventricular, LAD: left anterior descending coronary artery
Although there are several studies supporting the causal relationship of conduction disturbances and underlying coronary anatomy, this association is not clear, particularly from the view of AVB reversibility. In a study by Omeroglu et al.5) 8 patients with CAD and complete AVB were treated with CABG operation, but none of these patients recovered from complete AVB after revascularization. Yesil et al.6) investigated 53 patients who had third-degree AVB and significant CAD, and the result showed only a small percentage of patients recovered from a third-degree AVB (19% in medical and 27% in interventional treatment) without statistically significant difference. These studies may indicate that revascularization is not helpful in the recovery of conduction disturbances.
In this regards, we evaluated the association of AVB and CAD, to elucidate whether AVB is reversible in patients with CAD.
Subjects and Methods
Study design and data collection
This was an observational retrospective single-center study. This study was approved by the Institutional Review Board of Seoul National University Hospital (IRB No. H-1109-011-376).
From January 2005 to June 2011, 280 consecutive patients with clinically-significant new-onset AVB admitted to Seoul National University Hospital via outpatient clinic or emergency department were enrolled. Clinically-significant AVB requiring pacemaker was defined as follows; complete AVB and advanced AVB including 2 : 1 AVB. Ninety-two patients, who underwent pacemaker revision and implantable loop recorder insertion, were excluded and total 188 patients were analyzed in this study (Fig. 1).
Fig. 1.
Flow diagram of study patients. AVB: atrioventricular block, PM: pacemaker, ILR: implantable loop recorder, IB: irreversible block, RB: reversible block.
Baseline demographic variables of gender, age, height, weight, body mass index (kg/m2), smoking status and amount of smoking in pack-year, history of diabetes mellitus, hypertension, hypercholesterolemia, renal insufficiency, cerebrovascular accident, atrial fibrillation, CAD, prior revascularization therapy (including percutaneous coronary intervention and CABG), other prior open heart surgeries, cardiomyopathies, congenital heart disease, valvular heart disease, a family history of sudden cardiac death, and a family history of premature CAD in first-degree relatives (<55 years in males and <65 years in females) were identified based on the electronic medical records.
Coronary artery disease
Coronary artery disease was determined on the result of CAG, coronary CT angiography, and myocardial single photon emission computerized tomography (SPECT). Significant CAD was defined as >50% stenosis of epicardial coronary artery by CAG and coronary CT angiography, or perfusion decrease of myocardial SPECT.
Coronary pathologies were classified into 4 types according to classification of Mosseri et al.2); type I, lesions not related to septal branches or the atrioventricular (AV) node; type II, lesions compromising blood supply to septal branches emerging from the left anterior descending artery (LAD); type III, lesions compromising blood supply to the AV node; and type IV, lesions compromising blood supply both to septal branches emerging from the LAD and to the AV node (Table 1). Pathologic coronary anatomy was determined on the result of CAG or coronary CT angiography. When determining coronary pathologies, results of myocardial SPECT were not counted, as it could not designate the specific location.
Statistical analysis
Results are presented as mean±standard deviation or absolute numbers with percentages (%). Group comparisons were performed with Student t-test or crosstabs. The χ2 test or the Fisher exact test was used for categorical variables. To evaluate the association of CAD and conduction disturbance which require implantation of permanent pacemaker, univariate and multivariate logistic regression analysis was performed. All statistical analyses were performed with software, Statistical Package for the Social Sciences (SPSS) 18.0 (SPSS Inc., Chicago, IL, USA) and a p<0.05 was considered statistically significant.
Results
Patient characteristics
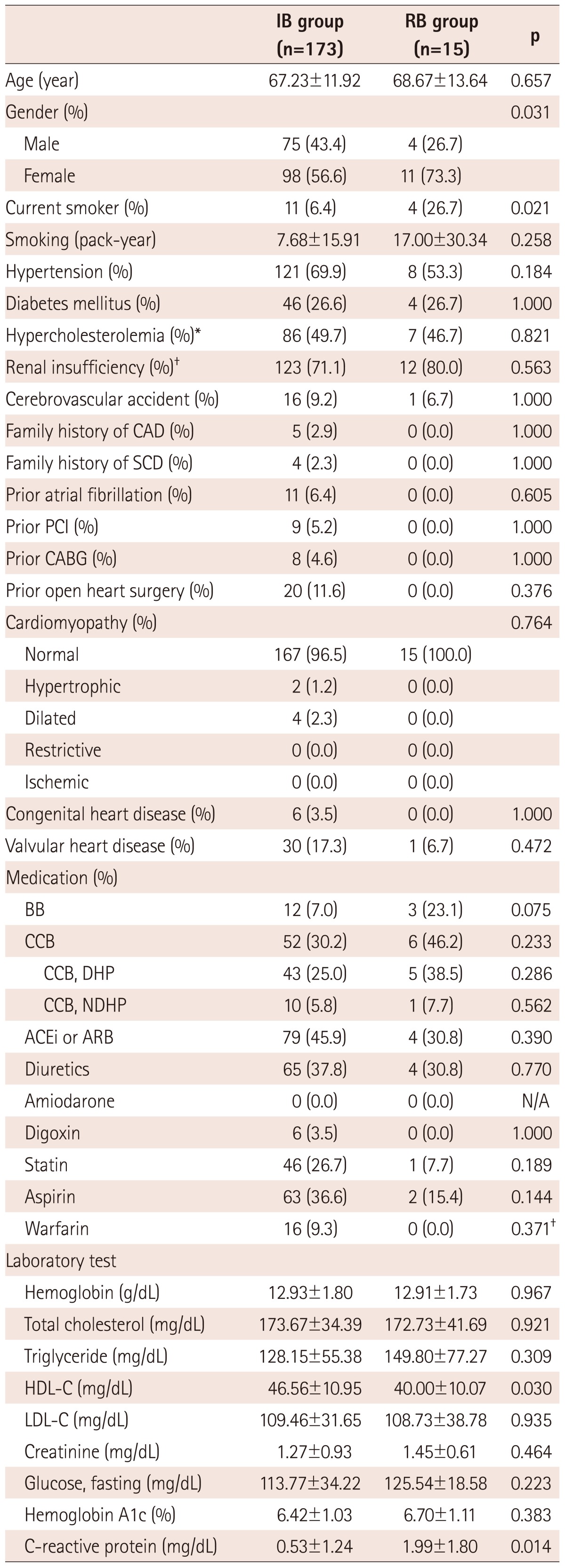
Baseline characteristics of 188 patients are summarized in Table 2. Irreversible AVB was observed in 173 patients (IB group) who had undergone implantation of a permanent pacemaker. Reversible AVB was observed in 15 patients (RB group). There were significant differences in gender, smoking status, and serum level of high density lipoprotein-cholesterol (HDL-C) and C-reactive protein (CRP) between the 2 groups. In the IB group, 75 (43.4%) were male and 11 (6.4%) were current smokers, while RB group had 11 (73.3%) males and 4 (26.7%) current smokers (p=0.031 for gender, p=0.021 for smoking status). Serum level of HDL-C was higher in IB group (46.56±10.95 mg/dL vs. 40.00±10.07 mg/dL, p=0.030), whereas CRP was higher in RB group (0.53±1.24 mg/dL vs. 1.99±1.80 mg/dL, p=0.014). There was no difference in other characteristics between the two groups.
Table 2.
Baseline characteristics
Values are mean±SD, or absolute number (%). *Hypercholesterolemia: known dyslipidemia or use of statin or total cholesterol >200 mg/dL, †Renal insufficiency: known chronic kidney disease or glomerular filtration rate <60 mL/min per 1.73 m2. IB: irreversible block, RB: reversible block, CAD: coronary artery disease, SCD: sudden cardiac death, PCI: percutaneous coronary intervention, CABG: coronary artery bypass graft, BB: beta blocker, CCB: calcium channel blocker, DHP: dihydropyridine, NDHP: non-dihydropyridine, ACEi: angiotensin converting enzyme inhibitor, ARB: angiotensin receptor blocker, HDL-C: high density lipoprotein-cholesterol, LDL-C: low density lipoprotein-cholesterol
Coronary artery disease and reversibility of atrioventricular block
In the IB group, 129 (74.6%) had no CAD on admission, 40 (23.1%) had stable angina, 2 (1.2%) presented with unstable angina, and 2 (1.2%) presented with acute myocardial infarction (AMI). In contrast, the RB group had 13 (86.7%) with AMI, one (6.7%) with stable angina, and one (6.7%) without CAD on admission (p<0.001). On the aspect of CAD type and reversibility of AVB, 13/15 (86.7%) patients had AMI, 0/2 (0%) had unstable angina, and 1/41 (2.4%) with stable angina had reversible AVB (Fig. 2). In 130 patients without CAD, only one (0.8%) had reversible AVB. The proportion of reversible AVB in patients with AMI was significantly higher than other groups; patients without CAD, with stable angina, and with unstable angina.
Fig. 2.
Reversibility of AVB and CAD type. Reversibility of AVB was assessed on the aspect of CAD type. The proportion of reversible AVB was significantly higher in patients presented with AMI. AVB: atrioventricular block, CAD: coronary artery disease, AMI: acute myocardial infarction.
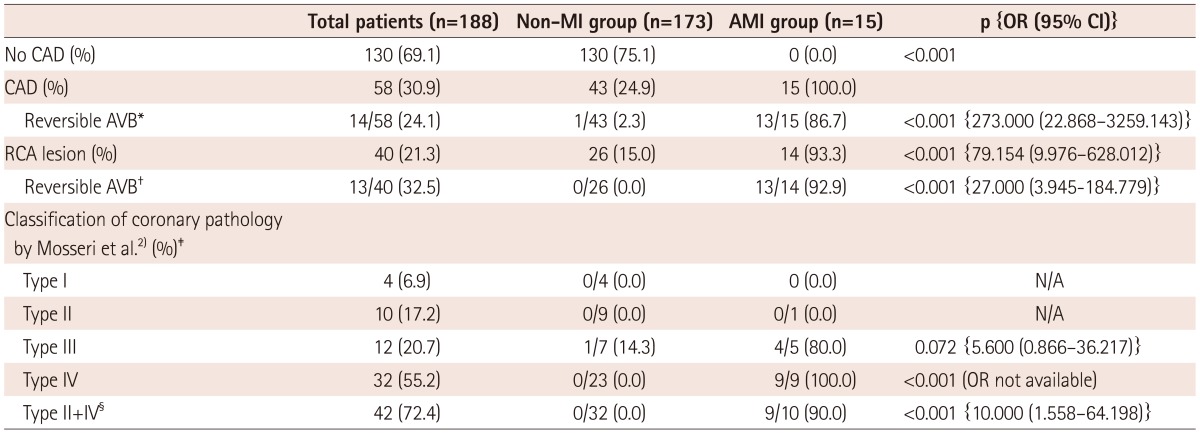
The reversibility of AVB was analyzed according to the distribution of coronary pathology (Table 3). CAD was found in 58 (30.9%) of 188 patients. 43 (24.9%) of 173 patients in the non-AMI group and 15 (100.0%) of 15 patients in the AMI group had CAD. Overall, 14 (24.1%) of 58 CAD patients had reversible AVB. AVB was rarely reversible in the non-AMI group as only one of 43 patients (2.3%) showed reversible AVB. In contrast, 13 of 15 patients with AMI (86.7%) had reversible AVB and there were significant difference between non-AMI group and AMI group (p<0.001). Among 15 patients with AMI, 11 patients had inferior wall ST-segment elevation myocardial infarction (STEMI) and 1 patient had anterior wall STEMI. There were 2 patients with AMI in IB group, showing inferior and anterior wall STEMI for each. RCA lesions were found in 25 (15.0%) in the non-AMI group and 14 (93.3%) in the AMI group (p<0.001) by CAG. The proportion of reversible AVB among patients with RCA lesion was also significantly higher in AMI group (p<0.001).
Table 3.
Reversible AVB and distribution of coronary pathology
Values are absolute number (%), or proportion of reversible AVB of each CAD types (%). *Proportion of reversible AVB among patients with CAD, †Proportion of reversible AVB among patients with RCA lesion, ‡Classification of coronary pathology by Mosseri et al.2) Values of this cell are absolute number (%), or proportion of reversible AVB of each CAD types (%), among patients with CAD, §Type II or IV vs. Type I or III. AVB: atrioventricular block, AMI: acute myocardial infarction, OR: odds ratio, CI: confidence interval, CAD: coronary artery disease, RCA: right coronary artery, N/A: not applicable, MI: myocardial infarction
According to Mosseri et al's2) classification, the number of patients with CAD in the non-AMI group were: 4 (9.3%) type I anatomy, 9 (20.9%) type II anatomy, 7 (16.3%) type III anatomy, and 23 (53.5%) type IV anatomy. One patient whose AVB was reversible had type III anatomy. In the AMI group, according to this same classification system, no patients had type I anatomy, 1 (6.7%) patient had type II, 5 (33.3%) patients had type III, and 9 (60.0%) patients had type IV. The proportions of reversible AVB in type III and type IV were higher in the AMI group (p=0.072 for type III and p<0.001 for type IV). The composite of type II and IV, in which septal blood flow of LAD is compromised in common, was found in 32 (74.4%) patients from the non-AMI group and AVB was irreversible in all patients, while the composite was found in 10 (66.6%) patients of AMI group and 9 (90.0%) patients had reversible AVB (p<0.001).
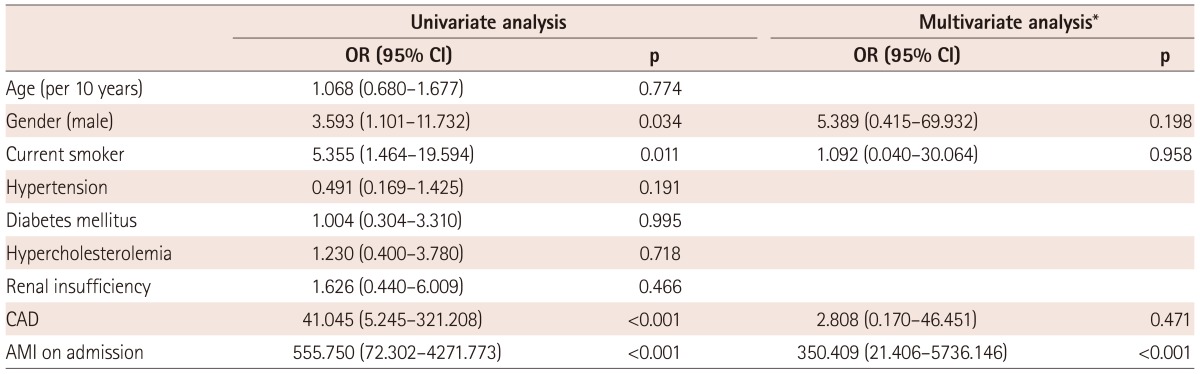
Factors associated with reversibility of atrioventricular block
Among demographic variables and the status of CAD on admission, we identified factors that showed significant association with reversibility of AVB by univariate and multivariate logistic regression analysis (Table 4). Univariate analysis revealed several significant factors; male gender {odds ratio (OR) 3.593, 95% confidence interval (CI) 1.101-11.732, p=0.034}, current smoker (OR 5.355, 95% CI 1.464-19.594, p=0.011), CAD (OR 41.045, 95% CI 5.245-321.208, p<0.001), and AMI on admission (OR 555.750, 95% CI 72.302-4271.773, p<0.001). Multivariate analysis was used to clarify these uncertainties and showed an obvious result; AMI on admission was the only associated factor (OR 350.409, 95% CI 21.406-5736.146, p<0.001).
Table 4.
Factors associated with reversibility of AVB
*Multivariate logistic regression analysis to define factors associated with reversible AVB. All univariate variables of p<0.10 were entered for multivariate analysis. AVB: atrioventricular block, OR: odds ratio, CI: confidence interval, CAD: coronary artery disease, AMI: acute myocardial infarction
Discussion
The main finding of this study is that AVB in patients with AMI is usually reversible, while AVB in patients with CAD other than AMI is usually irreversible. This result indicates that permanent pacemaker implantation should be delayed in cases of AMI. To our knowledge, the present study is the first to describe the reversibility of AVB in each type of CAD. Although we could not provide the optimal timing to confirm the reversibility of AVB in each type of CAD, the results of this study deserve special consideration.
The causal relationship between AVB and inferior wall AMI is relatively well-established. AVB complicates inferior wall AMI in 10% to 15% of cases,7-9) and most of these patients can be recovered from AVB by revascularization.10-12) However, the association of CAD other than AMI and reversibility of AVB is still unclear and is rarely studied. In this context, we tried to evaluate the association of AVB and CAD, in order to elucidate whether AVB is reversible in patients with CAD.
The blood supply of the AV node is from the posterior interventricular artery, which is a branch of RCA in right-dominant individuals. In the remainder of individuals, the AV node is still supplied by the posterior interventricular artery, but that artery is a branch of the left circumflex artery; the coronary circulation of these individuals is considered left-dominant. Intraventricular conduction system is supplied by septal branches from LAD, especially the first septal perforator branch from proximal LAD.13) This physiologic background has been supported by several studies. Mosseri et al.2) reported that a compromised blood flow of the septal branch and the RCA were associated with conduction disturbances. Tandoğan et al.,3) Yesil et al.,14) and Wei et al.4) reported similar results; stenoses of septal branch from LAD or RCA are associated with AVB. However, revascularization of the stenosed coronary artery could not reverse conduction disturbances.5),6)
In the present study, status of CAD on admission showed significant difference between the IB group and the RB group. The majority of the IB group had no evidence of CAD, while the RB group was mainly consisted of AMI patients. Patients with AMI recovered from AVB after revascularization therapy in most of cases, which is concordant with previous reports.10-12) In contrast, almost all patients without AMI eventually underwent implantation of a pacemaker, as they did not recover to sinus rhythm. With this result, we can postulate that patients with AVB and AMI have a higher chance to return to sinus rhythm by coronary revascularization, and it is not applied to the patients without AMI.
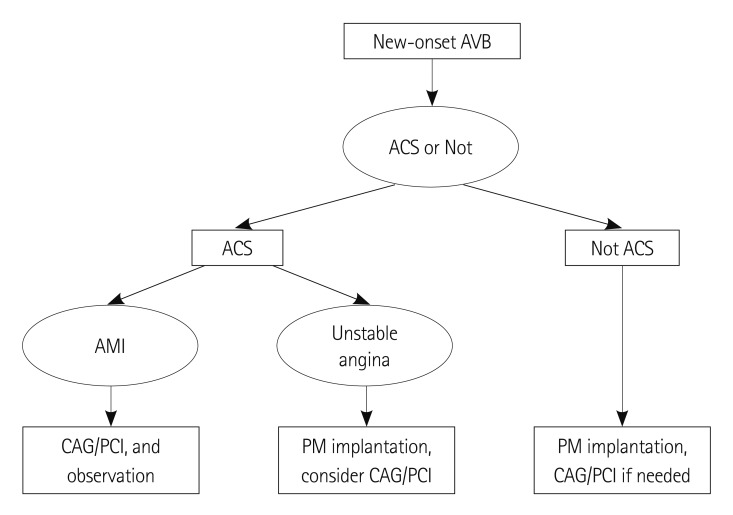
Patients with new-onset AVB might present with AMI, unstable angina, or stable angina. When planning implantation of pacemaker in these patients, it should be noted that dual-antiplatelet therapy is usually required after PCI in the era of drug-eluting stent.15) On the other hand, dual-antiplatelet therapy at the time of pacemaker implantation might increase the risk of bleeding complication and extend procedure time.16-18) Considering this clinical aspect and our study results, we recommend application of different therapeutic strategies for each entity (Fig. 3). If a patient of new-onset AVB presents with AMI, revascularization therapy is definitely required for treatment of AMI. But for the treatment of AVB which is a resultant feature of AMI, pacemaker implantation should be delayed as this type of AVB has very high probability to return to sinus rhythm after appropriate revascularization. If a patient with AVB presents with unstable angina, we recommend that the patient undergo pacemaker implantation first, and then revascularization therapy. In the present study, 2 AVB patients of unstable angina had to undergo pacemaker implantation. Considering the necessity of dual-antiplatelet therapy after coronary interventions,15) it would be rational to undergo pacemaker implantation prior to revascularization. If patients of new-onset AVB have no evidence of AMI or unstable angina, then pacemaker implantation would be the most important treatment, because the reversibility of AVB in these patients is hardly expected.
Fig. 3.
Flow chart of management of new-onset AVB. AVB: atrioventricular block, ACS: acute coronary syndrome, AMI: acute myocardial infarction, CAG: coronary angiography, PCI: percutaneous coronary intervention, PM: pacemaker.
The result of multivariate analysis in Table 4 confirmed the strong causal relationship between AMI and new-onset AVB. Male gender, smoking status, and existence of CAD were significantly associated factors on univariate analyses, but not on multivariate analysis. As male gender and smoking status are distinct risk factors of CAD, it seems that gender and smoking status are not major components in the reversibility of AVB. The most important aspect of this result is the strong association of AMI and reversibility of AVB, but not CAD itself. This result also poses a question of whether CAG as a routine procedure prior to implantation of permanent pacemaker is mandatory.
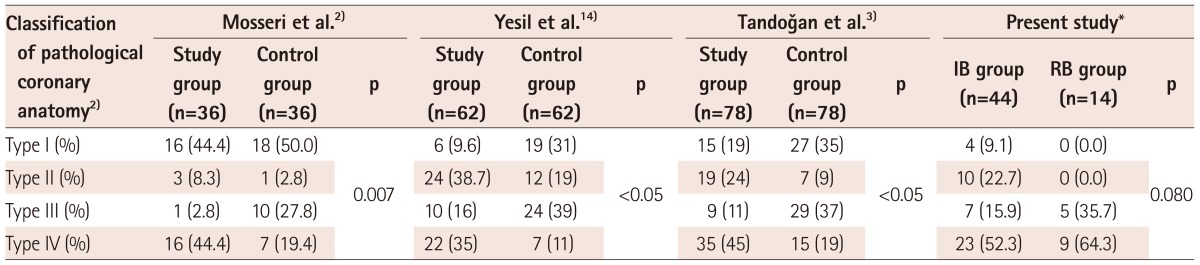
The location of pathologic coronary artery among patients with irreversible AVB showed similar distribution, compare to the results of previous several studies (Table 5).2-6),14) In the present study, type IV was the most common type of coronary pathology and type II was the second most common type in IB group; type I anatomy observed in 9.1% of patients with CAD, type II in 22.7%, type III in 15.9%, and type IV in 52.3%. In the study by Yesil et al.14) the distribution of coronary pathology was 9.6% type I, 38.7% type II, 16.0% type III, and 35.0% type IV. Tandoğan et al.3) studied 78 patients who had pacemaker implantation and angiographically proven CAD, and the distribution was 19% type I, 24% type II, 11% type III, and 45% type IV. In the study by Mosseri et al.2) type I and IV were the most frequently observed types (44.4% for each type) among 36 matched patients with permanent pacemaker. Generously, type II and type IV were much more frequently observed in patients with irreversible AVB which required implantation of permanent pacemaker. Thus, our study result supports the association of AVB and underlying CAD, which compromise the blood flow to septal branch or the RCA. The similarity shared by our result and previous studies not only supports the validity of our study, but also increases the potential for generalization. By screening all patients with new-onset AVB who visited our hospital, this study reflects medical practice in the real world.
Table 5.
Distribution of pathological coronary anatomy
Values are absolute number (%). *Patients who had significant CAD were counted. IB: irreversible block, RB: reversible block, CAD: coronary artery disease
Limitations
This study had several limitations. First, study population was not evenly distributed to each CAD types. Majority of patients had no evidence of CAD, while only 2 patients presented with unstable angina. This is primarily because this study reflected real practice. Second, this was an observational retrospective study, based on the electronic medical records. No standardized protocol was used to indicate tests in advance, although attending physicians referred to guidelines for managing AVB. Third, a further prospective study is required to investigate the effect of revascularization on the reversibility of AVB.
Conclusion
Our results show that AVB in patients with AMI is usually reversible after revascularization treatment, while patients with AVB (without AMI) usually required implantation of a permanent pacemaker, irrespective of the presence of CAD. Permanent pacemaker implantation should be delayed in cases of AMI. AVB in patients with CAD other than AMI is usually irreversible, therefore implantation of a pacemaker should be considered on a preferential basis.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Mosseri M, Meir G, Lotan C, et al. Coronary pathology predicts conduction disturbances after coronary artery bypass grafting. Ann Thorac Surg. 1991;51:248–252. doi: 10.1016/0003-4975(91)90796-s. [DOI] [PubMed] [Google Scholar]
- 2.Mosseri M, Izak T, Rosenheck S, et al. Coronary angiographic characteristics of patients with permanent artificial pacemakers. Circulation. 1997;96:809–815. doi: 10.1161/01.cir.96.3.809. [DOI] [PubMed] [Google Scholar]
- 3.Tandoğan I, Yetkin E, Güray Y, et al. Distribution of coronary artery lesions in patients with permanent pacemakers. Anadolu Kardiyol Derg. 2002;2:279–283. [PubMed] [Google Scholar]
- 4.Wei S, Zhong L, Chen S, Li X. The status of coronary artery lesions in patients with conduction disturbance. J Cardiovasc Med (Hagerstown) 2011;12:709–713. doi: 10.2459/JCM.0b013e328349187c. [DOI] [PubMed] [Google Scholar]
- 5.Omeroglu SN, Ardal H, Erdogan HB, et al. Can revascularization restore sinus rhythm in patients with acute onset atrioventricular block? J Card Surg. 2005;20:136–141. doi: 10.1111/j.0886-0440.2005.200369pl.x. [DOI] [PubMed] [Google Scholar]
- 6.Yesil M, Bayata S, Arikan E, Yilmaz R, Postaci N. Should we revascularize before implanting a pacemaker? Clin Cardiol. 2008;31:498–501. doi: 10.1002/clc.20280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gupta MC, Singh MM, Wahal PK, Mehrotra MP, Gupta SK. Complete heart block complicating acute myocardial infarction. Angiology. 1978;29:749–757. doi: 10.1177/000331977802901005. [DOI] [PubMed] [Google Scholar]
- 8.Tans AC, Lie KI, Durrer D. Clinical setting and prognostic significance of high degree atrioventricular block in acute inferior myocardial infarction: a study of 144 patients. Am Heart J. 1980;99:4–8. doi: 10.1016/0002-8703(80)90308-7. [DOI] [PubMed] [Google Scholar]
- 9.Nicod P, Gilpin E, Dittrich H, Polikar R, Henning H, Ross J., Jr Long-term outcome in patients with inferior myocardial infarction and complete atrioventricular block. J Am Coll Cardiol. 1988;12:589–594. doi: 10.1016/s0735-1097(88)80042-1. [DOI] [PubMed] [Google Scholar]
- 10.Feigl D, Ashkenazy J, Kishon Y. Early and late atrioventricular block in acute inferior myocardial infarction. J Am Coll Cardiol. 1984;4:35–38. doi: 10.1016/s0735-1097(84)80315-0. [DOI] [PubMed] [Google Scholar]
- 11.Tjandrawidjaja MC, Fu Y, Kim DH, et al. Compromised atrial coronary anatomy is associated with atrial arrhythmias and atrioventricular block complicating acute myocardial infarction. J Electrocardiol. 2005;38:271–278. doi: 10.1016/j.jelectrocard.2005.01.013. [DOI] [PubMed] [Google Scholar]
- 12.Giglioli C, Margheri M, Valente S, et al. Timing, setting and incidence of cardiovascular complications in patients with acute myocardial infarction submitted to primary percutaneous coronary intervention. Can J Cardiol. 2006;22:1047–1052. doi: 10.1016/s0828-282x(06)70320-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van der Hauwaert LG, Stroobandt R, Verhaeghe L. Arterial blood supply of the atrioventricular node and main bundle. Br Heart J. 1972;34:1045–1051. doi: 10.1136/hrt.34.10.1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yesil M, Arikan E, Postaci N, Bayata S, Yilmaz R. Locations of coronary artery lesions in patients with severe conduction disturbance. Int Heart J. 2008;49:525–531. doi: 10.1536/ihj.49.525. [DOI] [PubMed] [Google Scholar]
- 15.Iakovou I, Schmidt T, Bonizzoni E, et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA. 2005;293:2126–2130. doi: 10.1001/jama.293.17.2126. [DOI] [PubMed] [Google Scholar]
- 16.Tompkins C, Cheng A, Dalal D, et al. Dual antiplatelet therapy and heparin "bridging" significantly increase the risk of bleeding complications after pacemaker or implantable cardioverter-defibrillator device implantation. J Am Coll Cardiol. 2010;55:2376–2382. doi: 10.1016/j.jacc.2009.12.056. [DOI] [PubMed] [Google Scholar]
- 17.Cano O, Osca J, Sancho-Tello MJ, Olagüe J, Castro JE, Salvador A. Morbidity associated with three different antiplatelet regimens in patients undergoing implantation of cardiac rhythm management devices. Europace. 2011;13:395–401. doi: 10.1093/europace/euq431. [DOI] [PubMed] [Google Scholar]
- 18.Dreger H, Grohmann A, Bondke H, Gast B, Baumann G, Melzer C. Is antiarrhythmia device implantation safe under dual antiplatelet therapy? Pacing Clin Electrophysiol. 2010;33:394–399. doi: 10.1111/j.1540-8159.2009.02645.x. [DOI] [PubMed] [Google Scholar]