Abstract
Objective
To characterize the importance of the vertical angle of the sacral curvature (VASC) in lumbar disc herniations.
Methods
Morphological data derived from lumbar sagittal MRI imaging. The statistical significance of the findings are discussed. The angles of 60 female patients with lumbar disc herniations (LDH) were compared with the 34 female patients without LDH.
Results
128 of the 185 patients met our inclusion criteria. The vertical angle of sacral curvature is statistically significantly bigger in females with lumbar disc herniations when compared to subjects in control group, 28.32 and 25.4, respectively. (p=0.034<0.05). Same difference was not seen in males.
Conclusion
The vertical angle of sagittal sacral curvature may be another risk factor in females with lumbar disc herniations.
Keywords: Risk factor, Lumbar disc herniation, Females, Vertical angle of the sacral curvature
INTRODUCTION
Herniated lumbar disc is one of the most frequent medical problems18), and for decades, lumbar discectomy has been one of the most common surgical practices performed by neurosurgeons22). Today, lumbar spinal fusion surgery has been commonly performed for patients who present with chronic back pain with neurological symptoms23). At present, neurosurgical practice is confronted by an explosion of technology10,11). In the 1990s, the advent of magnetic resonance imaging (MRI) and the progressive increase in definition of this modality of imaging have considerably contributed to the knowledge of the natural evolution of a herniated lumbar disc. Axial loaded MRI can therefore give decisive information in dynamic spinal disorders by allowing simulation of an upright position4). Residual and recurring post-operative symptoms are still quite common in lumbar spinal surgeries12). The reasons some people have this persistent pain after surgery remain unclear, so the surgical treatment of ruptured lumbar inter-vertebral discs is sometimes discouraging to both surgeon and patient. It is important to demonstrate the neurological and radiological correlation while determining clinical status in cases with lumbar complaints5). Any contribution to our knowledge of the cause of these operative failures is always welcome. Since a purely experimental approach cannot provide this information, retrospective studies are called for, and studies focusing on the accurate understanding of appropriate spinal parameters. The development of low back pain can be associated with certain alterations in the sagittal shape of the spine, some studies have analyzed spino-pelvic alignment in patients with lumbar degenerative disease15,16,25), but the significance of the angle of the sacrum in the pathogenesis of low back pain has also received scant attention. Sacral curvature (SC), represented by the angle between the first and the last sacral vertebrae, is a feature that differentiates the human pelvis from that of other animals. In some sacra, the surface of the sacrum can be nearly straight with a very slight curvature affecting the lower end. In the others, the curvature is throughout the entire length of the sacrum, especially toward the middle. Other sacra have a less marked curvature affecting only the lower third of the bone. It is unclear whether the degrees of vertical angle of sacral curvature are the same for all adult patients with disc herniations. We hypothesized that the mechanics of load transfer in the spine and in the intervertebral disc in particular is an important factor in understanding the patterns and mechanics of disc pain. The vertical angle of sacrum may have a pivotal role in etiology and post operative outcome of lumbar disc herniations. There is no publication quantitating human vertical angle of sacrum in lumbar disc herniations, so we analyzed this angle and and compared the results with patients without any lumbar disc disease.
MATERIALS AND METHODS
After informed consent, 185 patients who admitted to the Department of Neurosurgery of Rize Research and Education Hospital with low back pain between 2 April-10 July 2009 were analysed. To provide group homogenity, body mass index (BMI) was calculated. All patients with BMI values less than 20 or more than 40 was excluded from the study as well as patients younger than 20 and older than 50 years of age. The exclusion criteria were as follows : BMI value lesser than 20 or greater than 40, age younger than 20 and older than 50, previous surgery, associated lumbar spine stenosis, foraminal or extraforaminal disc herniations, spondylolisthesis. Of the 185 patients, 128 were met the inclusion criteria. These patients were divided to two groups according to their sex.
Data collection
After giving informed consent,, radiographs were obtained. Ergün et al.7) analyzed differences in lumbosacral morphology associated with the tendency to develop intervertebral disc degeneration. Sacral curvature (SC), represented by the angle between the first and the last sacral vertebrae, and the vertical angle of sacral curvature (VASC) was defined as the angle created between the intersection of a line running centrum of sacral curvature and a vertical line (Fig. 1, 2). From sagittal plan of lumber MRI, the vertical angle of sacral curvature. The normal orientation of lumbosacropelvic structure plays an important role in the determination of shear and compressive forces applied on the anterior (corpus vertebrae and intervertebral discs) and posterior (facet joints) elements of lumbar vertebral column19). This finding led us to our interest in VASC values. No publications in the literature were analyzed the relationship between intervertebral disc degeneration and the degree of VASC in females. We measured it by geometrical construct. Patient files and radiological data were reviewed. Data on age and sex, VASC were recorded. To show the uniformity of groups, BMI was also evaluated.
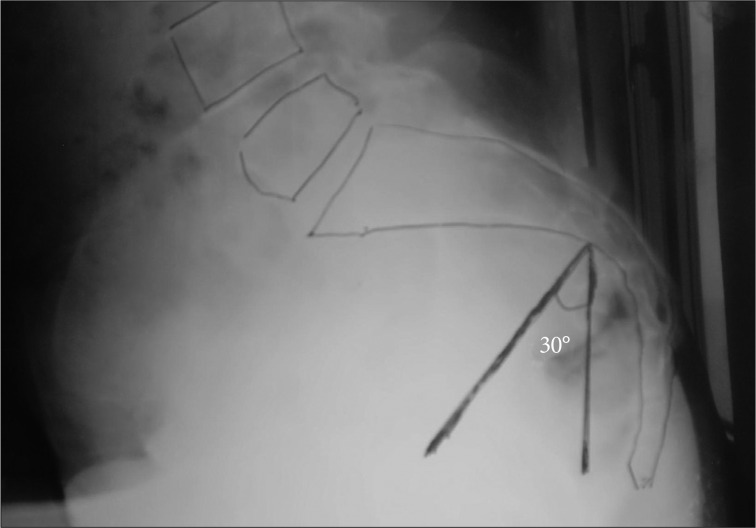
Fig. 1.
The sacral curvature and its vertical angle in conventional X-ray.
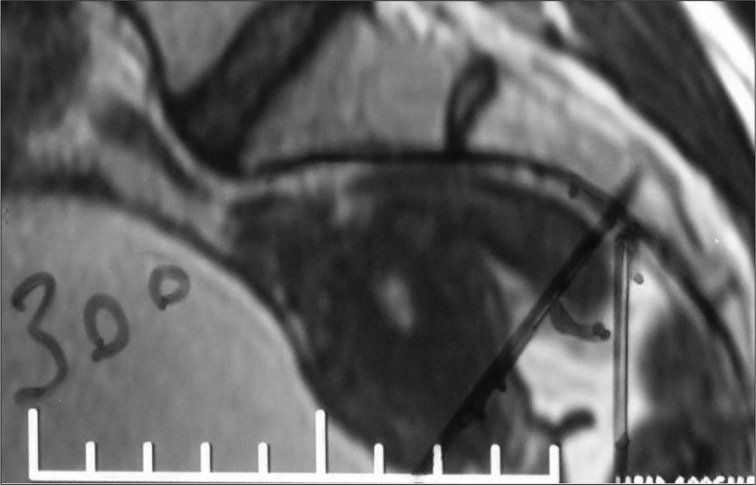
Fig. 2.
VASC in sagittal MRI image. VASC : vertical angle of the sacral curvature, MRI : magnetic resonance imaging.
Statistical analysis
Data were analyzed with the statistical software package SPSS for Windows (SPSS Inc., Chicago, IL, USA). The comparisons between parameters were performed using Wilkonson signed rank test. The level of significance was set at 0.05.
RESULTS
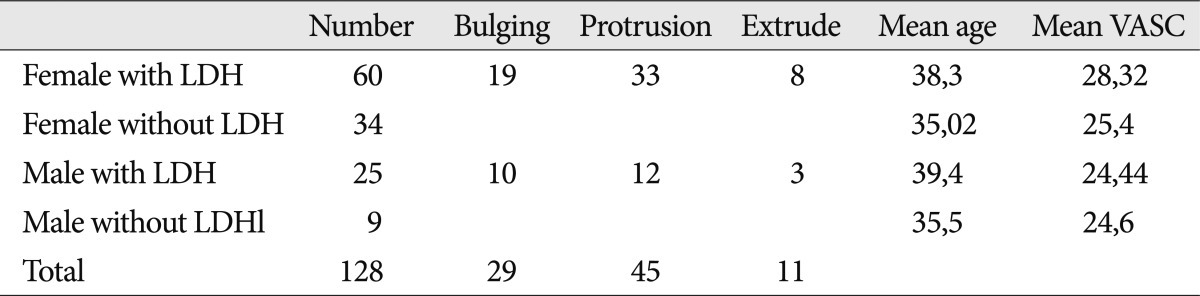
Female patients comprised 60 lumbar disc herniation cases (Disc Herniation Group, DHG); the mean age was of 38.3 years (range 22-50 years). The second group comprised 34 cases without any vertebral disease (Non-Disc Herniation Group), the mean age was of 35.02 years (range 21-50 years). The first group of males comprised 25 subjects with lumbar disc herniation, the mean age was of 39.42 years (range 21-50 years). The second group of male comprised 9 cases with free vertebral disease; the mean age was of 35.5 years (range 21-44 years).
The mean vertical angle of sacral curvature can be seen from the table. Wilkonson signed rank test showed that the vertical angle of sacral curvature was statistically significantly bigger in female with lumbar disc herniations than the angles of control group, 28.32 and 25.4, respectively (p=0.034<0.05).
Table 1.
Shows the means mean vertical angle of both groups
VASC : vertical angle of the sacral curvature, LDH : lumbar disc herniation
DISCUSSION
It is known that the human pelvis reaches its definite form at the age of 20-25 years. This fact is the starting point of our investigation. Complete fusion of the sacrum has been reported to occur between years 25 and 33 of life and is related to the load-bearing aspects of this region. Pathogenesis of the sacral morpho-topography changes could be easily explained by negative effects on human erect position. The sacrum of homo sapiens is not positioned posteriorly at birth and that it is during the first few years that the sacrum, in humans, moves dorsally in relation with the progressive acquisition of erect posture and the ontogeny of bipedal locomotion. The evolution of bipedal posture and ambulation in humans has transformed the horizontal vertebral column of vertebrates into a load-bearing erect spine that is required to efficiently transfer weight, provide stability and permit motion. Due to the erect position, the pelvic bone system is subjected to new static and dynamic relations, which play a very important role in definite formation of this region6,8,14). Through the spinal column, the body load is shifted to the base of the sacrum and then, through the pelvic girdle to inferior extremities. The position of the sacrum relative to the vertical has been frequently mentioned but seldom measured. To express this verticality of the sacrum, Newman drew a line from the posterior superior iliac spine to the symphysis pubis. The angle between this and a vertical line was the sacral inclination. This is also known as "sacral tilt". This refers to the relationship of the sagittal plane of the sacrum to the vertical plane. VASC can be correlated with sacral tilt. In this study, we did not use the sacral inclination (S1 : value of the angle between the posterior side of the body of the first sacral vertebra and the vertical) and sacral slope (SS) parameter. Both parameters are different from VASC. We think that VASC degree is more sufficient in showing the vertical or horizontal sacrum. SS; SI are related to only first sacral vertebra. Orientation of S1 and sacrum itself may not be same degree, because the intervertebral disc between the fifth lumbar and the first sacral vertebrae is subject to more trauma, both acute and chronic, than any other intervertebral disc. This is due to the facts that it carries a heavier load and this disc is found by X-ray to be destroyed more frequently than any other. Sacral biomechanics have an impact on the nerves exiting the spinal cord in the entire spine but particularly in the lower lumbar spine and from the sacrum itself. Sacral curvature is as a characteristic of Homo sapiens as is erect posture1). Lumbar disc surgery is one of the most frequent procedures performed by spine surgeons22). Onset of lumbar disc in human often is associated with bipedal ambulation. Theories propose that this transformation in the mechanics of locomotion is the inciting evolutionary event that made the lumbar spine susceptible to degenerative disease. If the primary sources of disc pathology are these forces/stresses acting on the spine, why did the spine not evolve into a more rigid structure? What is the purpose of having a vertebral column capable of torsion and compression, unless it is somehow linked to the demands of human gait? This study investigates the relationship between lumbar disc herniation and the vertical angle of sacral curvature. This angle was found to be statistically significantly bigger in female with lumbar disc herniations when compared to subjects in control group, 28.32 and 25.4, respectively (p=0.034<0.05). We supposed that there are different factors contributing to the formation of the vertical angle of sacral curvature. These factors include1) the effect of erect posture, which tilts the upper part of the sacrum dorsally and the lower part of the sacrum ventrally2), and the influence of supine posture, which affects the development of the lower part of the sacrum. In addition to supine posture the levator ani, which is well developed in Homo sapiens, also affects the lower part of the sacrum and coccyx and influences its ventral orientation. Variations of the VASC can be result from differences in onset and frequency of supine posture.
This is the first time that vertical angle of sacral curvature has been shown to play a role in female with lumbar disc herniation. The purpose of this study is to determine the reliability and validity of a goniometric measurement of the vertical angle of sacrum, found statistically significant difference in female with lumbar disc herniation and without intervertebral disc disease. If indeed one is the first to report something and that something is of value. We assumed that that this finding result in a higher gravitational compressive force which may, in turn, lead to progressive degeneration of the discs in female high VASC degree. Men in their fourth to fifth decade appear to be the most prone to disc herniation with subsequent cauda equina and conus medullaris syndromes17,24). Because of insufficient number of males in this study, their angle was not analyzed. Our study was performed in the eastern Black Sea Region of Turkey, and in this area women are exposed to more environmental and life issues than men. This is the reason the high number of female in this study. It was shown , that the VASC degree of females with lumbar disc herniations (LDH) is statistically significantly bigger than from the females without LDH. "More vertical sacrum" means increased the VASC degree. This study is the first time this has been documented. The increased VASC in female found in the disc herniation group suggest that the spatial orientation of the sacrum is more vertical than in the normal group. Even if it is difficult to determine the part of structural loss of lordosis and the postural part, we observed that increased VASC induces LDH in female, probably with anterior displacement of C7 plumbline and center of gravity, resulting in an increased flexion moment applied to the spine, here, increased VASC may be predisposed LDH in female. This sagittal unbalance is partially corrected by the pelvis back tilt. The gravity line of the body passes through many vertebrae and "leaves" the spine at the sacral promontory.
We conducted this study with sacrum, because the sagittal sacral morphology is a constant anatomic variable specific to each individual and unaffected by the position of the patient in space and, found VASC was increased in female with LDH.
Discectomy is often used in the treatment of prolapsed intervertebral disc to relieve the associated leg pain. Surgical treatment of symptomatic lumbar disc herniations has been well established. But conservative treatment should be considered when cauda equina syndrome or progressive motor weakness are absent in the acute stage of the lumbar herniated disc21). Although lumbar disc surgery is known to be able to relieve pain we have to make sure it improves the quality of life3,9). The outcomes reported after both traditional techniques and microsurgery for lumbar disc herniation have generally been shown to be equal13,17). However, between 10% and 40% of patients do not have a satisfactory outcome13), and many in whom surgery is deemed successful continue to have some degree of low back pain. The reasons some people have persistent pain after surgery remain unclear, so the surgical treatment of ruptured lumbar intervertebral discs is sometimes discouraging to both surgeon and patient, because the operation fails to relieve the symptoms of back pain and/or sciatica, and the treatment of discogenic pain is always problematic for spine surgeons. There is an incessant search for the causes and the action mechanisms of operative failures of the lumbar disc herniation. Any contribution to our knowledge of the cause of these operative failures is always welcome. Increased VASC in females may also be one of the reasons of unsatisfactory outcome after discectomy. Some authors also report that the female gender is a risk factor for failed back surgery2,20). This may be associated with the increased VASC degrees of female gender. We copiously stress the fact that we are the first ones to report that such an increased VASC degrees in females with LDH. The recognition of this fact is of importance because it has to do with degenerative changes in the spine. If indeed one is the first to report something and that something is of value. More data is needed on this subject.
Why preferred sagittal MRI image to measure sacral curvature rate and vertical angle?
A question can be asked for this subject. There are two reasons; 1-We measured the angle of sacral curvature. This angle will not be changed in sagittal MRI image or direct conventional radiographic X-rays (Fig. 1, 2). In the beginning of study, we measured the VAS both in MRI images and direct conventional lumbo-sacral lateral X-rays, and noted the VAS degree is correlated with each other. It was bigger in conventional X-rays than MRI. In lying down, or standing X-Rays, we found it was two times greater degree than sagittal MR images. We wanted to omit to give patient unnecessary radiation to by conventional X-Ray, used MRI images. The problem, here, may be important with regard with the VASC which is calculated on MRI imaging in prone position and then referenced with a vertical line. This reference line may not correspond with the standing position. This should not be problem, because sacral curve is the undistorted part of the spinal curves. Regarding the second line which is the radius of the sacrum, it is positioning the centre of the sacral curvature. This curvature is assimilated to a circle.
CONCLUSION
The sacral bone is an integral a part of the pelvis and constitutes the undistorted part of the spinal curves. We think that the development of the vertical angle of sacral curvature is related to the progressive acquisition of erect posture and the ontogeny of bipedal locomotion. As lumbosacral angle, this angle is almost nil in the nonprimate mammals, who only infrequently stand erect. Organization of sagittal curves during growth can be followed up by looking at the sacrum and its vertical angle. VASC may be parameter showing sacrum orientation, its vertical or horizontal position. This study suggested the impact of the sagittal sacral profile in pathogenesis of LDH in female. In this situation the compressive force component of gravity increases and these greater compressive forces accelerate the degeneration of the disc. This increase of the compressive forces is probably one of the many pathognomic conditions that lead to herniation. Therefore, this pathology generally occurs after 20-25 years of age and rarely earlier in life. We suggest that the sacrum and also spine supported by the legs are balanced in the sagittal plane. The vertical angle of sacral curvature in female with LDH is bigger than the angle of female without LDH. The greater VASC or, anteriorly shifted the gravity line with increased VASC in females may be a risk factor for LDH. We think that increased VASC may have a direct influence on the development of lumbar disc herniation in females, but a thorough knowledge of the vertical angle of sacral curvature are needed to aid in understanding the mechanisms that lead to lumbar disc herniations in female and to provide rationale of management. Further study is needed in this subject.
References
- 1.Abitbol MM. Sacral curvature and supine posture. Am J Phys Anthropol. 1989;80:379–389. doi: 10.1002/ajpa.1330800311. [DOI] [PubMed] [Google Scholar]
- 2.Akgun B, Kaplan M, Arici L, Pusat S, Erol FS. Low back pain and sciatica related with the premenstrual period in patients with lumbar disc herniation. Turk Neurosurg. 2010;20:437–441. doi: 10.5137/1019-5149.JTN.2898-10.1. [DOI] [PubMed] [Google Scholar]
- 3.Aydin V, Aydin S. Outcome measurement after lumbar disc surgery. Turk Neurosurg. 2005;15:4–11. [Google Scholar]
- 4.Choi KC, Kim JS, Jung B, Lee SH. Dynamic lumbar spinal stenosis : the usefulness of axial loaded MRI in preoperative evaluation. J Korean Neurosurg Soc. 2009;46:265–268. doi: 10.3340/jkns.2009.46.3.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cosan TE, Adapinar B, Aslantas A, Tel E, Sahin F. Is Lumbar Spinal Reserve Capacity on CT-Myelography Significant? Turk Neurosurg. 1998;8:114–118. [Google Scholar]
- 6.Davies JW. Man's assumption of the erect posture, its effect on the position of the pelvis. Am J Obstet Gynecol. 1955;70:1012–1021. doi: 10.1016/0002-9378(55)90008-9. [DOI] [PubMed] [Google Scholar]
- 7.Ergün T, Lakadamyalı H, Sahin MS. The relation between sagittal morphology of the lumbosacral spine and the degree of lumbar intervertebral disc degeneration. Acta Orthop Traumatol Turc. 2010;44:293–299. doi: 10.3944/AOTT.2010.2375. [DOI] [PubMed] [Google Scholar]
- 8.Gregory WK. The upright posture of man : a review of its origin and evolution. Proc Am Phylos Soc. 1928;67:339–377. [Google Scholar]
- 9.Hutchinson PJ, Laing RJ, Waran V, Hutchinson E, Hollingworth W. Assessing outcome in lumbar disc surgery using patient completed measures. Br J Neurosurg. 2000;14:195–199. doi: 10.1080/026886900408351. [DOI] [PubMed] [Google Scholar]
- 10.Kanat A, Epstein CR. Challenges to neurosurgical professionalism. Clin Neurol Neurosurg. 2010;112:839–843. doi: 10.1016/j.clineuro.2010.07.012. [DOI] [PubMed] [Google Scholar]
- 11.Kanat A, Yazar U, Kazdal H, Yilmaz A, Musluman M. Neurosurgery is a profession. Neurol Neurochir Pol. 2009;43:286–288. [PubMed] [Google Scholar]
- 12.Kaner T, Tutkan I. Monoradiculopathy and secondary segmental instability caused by postoperative pars interarticularis fracture : a case report. Turk Neurosurg. 2009;19:177–181. [PubMed] [Google Scholar]
- 13.Kara B, Başkurt Z, Acar U. One year outcome after surgery for lumbar disc herniation : a comparison of reoperated and not reoperated patients. Turk Neurosurg. 2007;17:1–6. [PubMed] [Google Scholar]
- 14.Keith A. Men's posture : its evolution and disorders. Theories concerning the evolution of men's posture. Br Med J. 1923;1:451–455. doi: 10.1136/bmj.1.3246.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lazennec JY, Ramaré S, Arafati N, Laudet CG, Gorin M, Roger B, et al. Sagittal alignment in lumbosacral fusion : relations between radiological parameters and pain. Eur Spine J. 2000;9:47–55. doi: 10.1007/s005860050008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Legaye J, Duval-Beaupère G, Hecquet J, Marty C. Pelvic incidence : a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99–103. doi: 10.1007/s005860050038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nachemson A, Zdeblick TA, O'Brien JP. Lumbar disc disease with discogenic pain. What surgical treatment is most effective? Spine (Phila Pa 1976) 1996;21:1835–1838. doi: 10.1097/00007632-199608010-00023. [DOI] [PubMed] [Google Scholar]
- 18.Naderi S, Egemen N, Gokalp H, Cu1cuoglu A, Erdogan A, Baskaya M. The value of dermatomal somatosensory-evoked potantial in evaluation of herniated lumbar disc. Turk Neurosurg. 1992;2:139–143. [Google Scholar]
- 19.Roaf R. Vertebral growth and its mechanical control. J Bone Joint Surg Br. 1960;42:40–59. doi: 10.1302/0301-620X.42B1.40. [DOI] [PubMed] [Google Scholar]
- 20.Rosenfeld R, Livne D, Nevo O, Dayan L, Milloul V, Lavi S, et al. Hormonal and volume dysregulation in women with premenstrual syndrome. Hypertension. 2008;51:1225–1230. doi: 10.1161/HYPERTENSIONAHA.107.107136. [DOI] [PubMed] [Google Scholar]
- 21.Ryu SJ, Kim IS. Spontaneous regression of a large lumbar disc extrusion. J Korean Neurosurg Soc. 2010;48:285–287. doi: 10.3340/jkns.2010.48.3.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sasani M, Oktenoğlu T, Tuncay K, Canbulat N, Carilli S, Ozer FA. Total disc replacement in the treatment of lumbar discogenic pain with disc herniation : a prospective clinical study. Turk Neurosurg. 2009;19:127–134. [PubMed] [Google Scholar]
- 23.Seong JH, Lee JW, Kwon KY, Rhee JJ, Hur JW, Lee HK. Comparative study of posterior lumbar interbody fusion via unilateral and bilateral approaches in patients with unilateral leg symptoms. J Korean Neurosurg Soc. 2011;50:363–369. doi: 10.3340/jkns.2011.50.4.363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shapiro S. Cauda equina syndrome secondary to lumbar disc herniation. Neurosurgery. 1993;32:743–746. doi: 10.1227/00006123-199305000-00007. discussion 746-747. [DOI] [PubMed] [Google Scholar]
- 25.Wiltse LL, Winter RB. Terminology and measurement of spondylolisthesis. J Bone Joint Surg Am. 1983;65:768–772. [PubMed] [Google Scholar]