Abstract
We report a rare complication of iatrogenic spinal intradural following minimally invasive extradural endoscopic procedues in the lumbo-sacral spines. To our knowledge, intradural cyst following epiduroscopy has not been reported in the literature. A 65-year-old woman with back pain related with previous lumbar disc surgery underwent endoscopic epidural neuroplasty and nerve block, but her back pain much aggravated after this procedure. Postoperative magnetic resonance imaging revealed a large intradural cyst from S1-2 to L2-3 displacing the nerve roots anteriorly. On T1 and T2-weighted image, the signal within the cyst had the same intensity as cerebrospinal fluid. The patient underwent partial laminectomy of L5 and intradural exploration, and fenestration of the cystic wall was accomplished. During operation, the communication between the cyst and subarachnoid space was not identified, and the content of the cyst was the same as that of cerebrospinal fluid. Postoperatively, the pain attenuated immediately. Incidental durotomy which occurred during advancing the endoscope through epidural space may be the cause of formation of the intradural cyst. Intrdural cyst should be considered, if a patient complains of new symptoms such as aggravation of back pain after epiduroscopy. Surgical treatment, simple fenestration of the cyst may lead to improved outcome. All the procedures using epiduroscopy should be performed with caution.
Keywords: Intradural lesion, Intradural cyst, Epiduroscopy
INTRODUCTION
Epiduroscopy is a relatively new minimally invasive technique for treatment of chronic low back pain. Recently, some investigators have presented diagnostic role and therapeutic efficacy of epiduroscopy in various kinds of back pain with/without radiculopathy2,3). However, there must be latent risks of dura injury during advancing endoscope from the sacral hiatus to the affected area in the lumbar spine, even if the endoscope is carefully steered and advanced into the epidural space under the guidance of a video-guided catheter and fluoroscopy.
We present a patient that underwent epiduroscopy (Storz Epiduroscope, Karl Storz, Tuttlingen, Germany). After the procedures, back pain was aggravated and newly development of a large intradural lumbosacral cyst was demonstrated in MRI.
CASE REPORT
A 65-year-old lady came to the outpatient department with complaints of low back pain (VAS : 8/10) and stretching discomfort in the left leg since January 2010 when she slipped down on ground. Clinically, she had mild tenderness over L4-L5 and L5-SI regions with paraspinal muscle spasm. Straight leg raising test was normal and she had no neurological deficit. She was managed with pain medications and physiotherapy after checking her X-rays which were normal except findings of left partial laminectomy at L4. She had had a past history of low back pain with left radicular pain, for which two surgeries of microdiscectomy were performed at left L4-5 in May 2008 and November 2008, respectively. She had relief of pain for only 3 months after the first surgery but completely symptom free after the second surgery until the accident on January 2010.
As her pain was not relieved, lumbar spine magnetic resonance imaging (MRI) was done with contrast, which showed no recurrence of disc herniation except for the findings of mild adhesion at L4-5 disc and left partial laminectomy of L4 (Fig. 1). She was referred to the pain clinic on June 24, 2010, and underwent endoscopic epidural neuroplasty and transforaminal epidural steroid injection at L4-5 and L5-S1. In prone position, an epidural catheter was inserted into anterior epidural space of L4-5 and L5-S1 levels through the sacral hiatus (Fig. 2). And, pucaine with triamcinolone was injected and adhesiolysis was done. During the procedure, the pain specialists did not experience any specific incident.
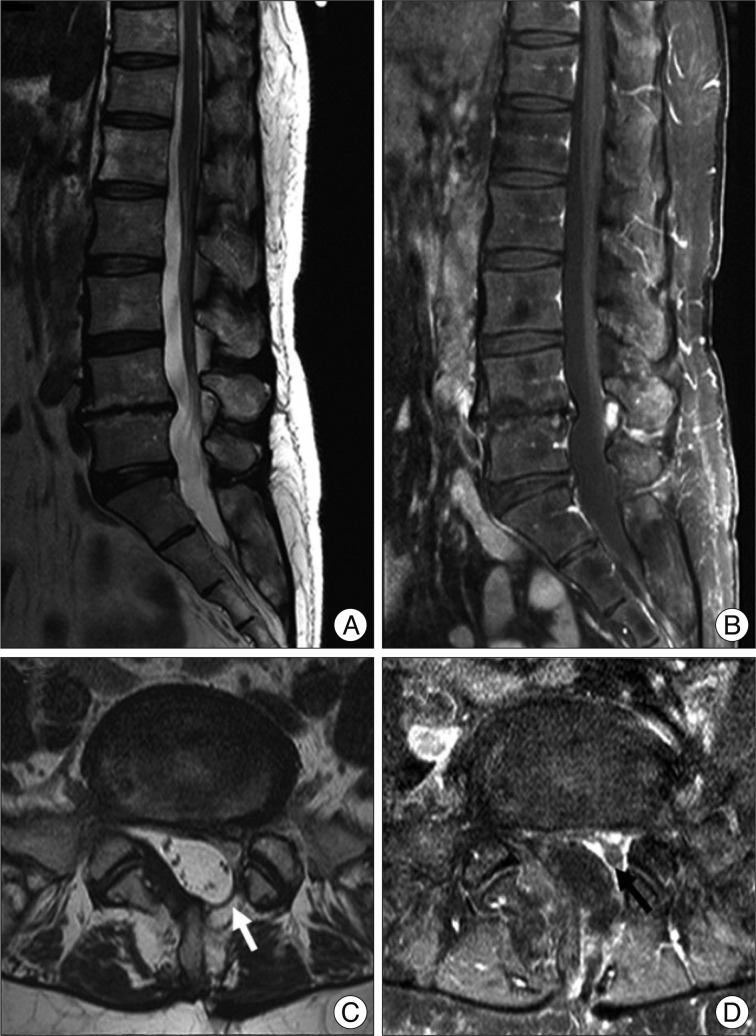
Fig. 1.
Lumbar sagittal T2 weighted (A), Gd-enhanced T1 weighted (B), axial T2 weighted (C), and Gd-enhanced T1 weighted (D) magnetic resonance imaging scans showing the postoperative changes of L4-5 level, which presenting no recurrence of disc herniation except for the findings of mild adhesion and left partial hemilaminectomy of L4 (white and black arrows).
Fig. 2.
A fluoroscopic view showing the endoscopic epidural neuroplasty. An epidural catheter is inserted into the epidural space of L5-S1 levels through the sacral hiatus. The tip of epidural catheter is located just around right L5 root.
After the endoscopic epidural neuroplasty, she complained of increase in the intensity of back pain (VAS : 9/10), over a wide area of low back. She was again put on pain medications for 2 weeks, but not much pain relief and it was decided to take MRI of the lumbosacral spine. MRI showed an intradural cystic lesion, 8 cm in length, spanning from L2-3 to S2-3 level and displacing cauda equina anteriorly, lesion was slightly herniated through the laminectomy defect of left L5. The cyst fluid had the same signal intensity as cerebrospinal fluid, in all the sequences (Fig. 3). She was admitted to our department. Computed tomography myelography confirmed the findings of intradural cyst on the MRI, and contrast media was partially filled up in the cystic cavity of the lower spines (Fig. 4). As conservative treatment did not provide any pain relief, surgery was planned. In operation, the patient was placed in prone position and partial laminectomy of L5 was performed. Opening the dura mater, a large cyst, which presented well demarcated by thin and transparent wall and contained cerebrospinal fluid (CSF), was observed in the dorsal part of the intradural space, compressing and displacing the cauda equina anteriorly. The cauda equina was covered by arachnoid membrane separately (Fig. 5). Fenestration of cystic wall and enlargement of the window were performed. The authors could not find out a connection of the cyst with subarachnoid space intraoperatively. The dura mater was closed water tightly. Before closing the surgical wound, adhesiolysis over the L5 nerve roots was also done. Pathology of cyst wall revealed non-specific fibrous tissue. She had relief of severe back pain postoperatively (VAS : 3/10). Postoperative follow-up MRI disclosed complete disappearance of the intradural cyst (Fig. 6).
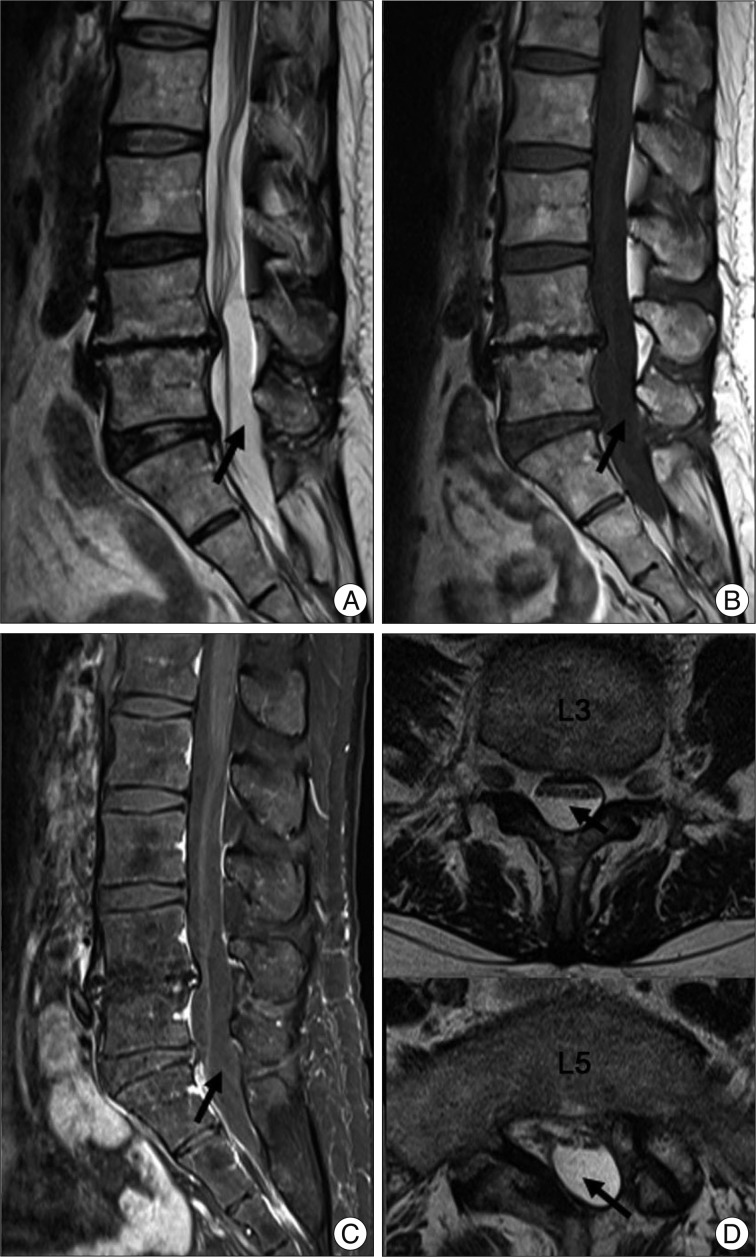
Fig. 3.
Sagittal T2 (A), T1 (B), Gd-enhanced T1 (C) and axial T2 (D) weighted magnetic resonance imaging scans showing an intradural cystic lesion (black arrows), spanning from L2-3 to S2-3 level and displacing cauda equina anteriorly. The cyst fluid having the same signal intensity as cerebrospinal fluid.
Fig. 4.
Myelography-computed tomography images showing an intradural cyst spanning from L4-5 to S2-3 level (black arrow) (A). The contrast media is partially filled up in the cystic cavity of the lower spines (black arrows) (B).
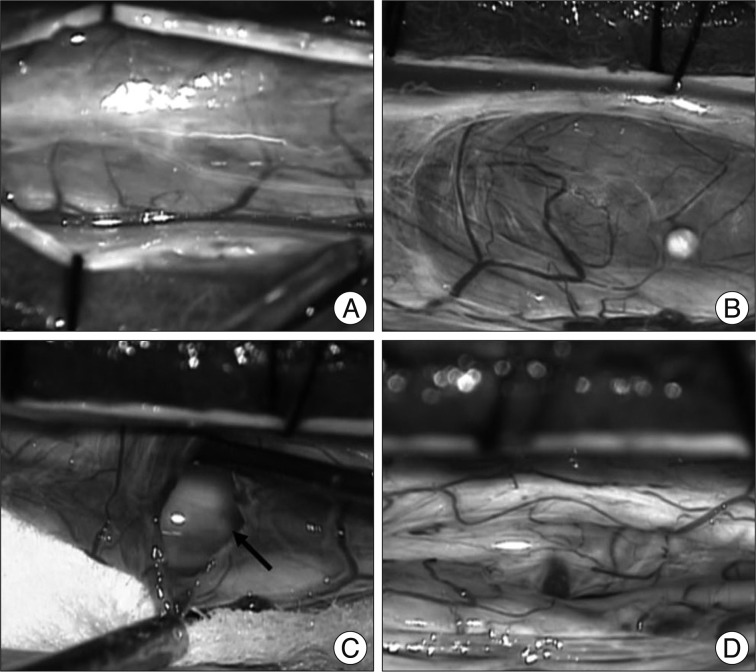
Fig. 5.
Intraoperative photographs. A : After hemilaminectomy, the dura mater is opened. B : A large arachnoid cyst, which presents well demarcated by thin and transparent wall and contains cerebrospinal fluid, is observed in the dorsal part of the intradural space, compressing and displacing the cauda equina anteriorly. C : Cystic wall and enlargement of the window were performed. No connection of the cyst with subarachnoid space is noticed. D : After partial removal of cyst wall, nerve roots are exposed and decompressed.
Fig. 6.
Sagittal (A) and axial (B) postoperative magnetic resonance imaging scans showing complete disappearance of the intradural cyst.
DISCUSSION
Epiduroscopy has several synonyms such as periduroscopy, epiduraloscopy, extraduroscopy, and spinal endoscopy. This minimally invasive technique can offer diagnostic and therapeutic advantages to patients with chronic low back pain and radiculopathy. The advantages of epiduroscopy are : confirming diagnosis by detection of nerve root pathology, fibrosis and adhesions not visible on MRI scan; minimally invasive procedure for treating radiculopathy; and allowing targeted drug therapy2). On the other hand, the most frequent complication of epiduroscopy must be perforation of the dural sac1,5,9). Although the mechanism of development of intradural syst in our case is not clear, in our case, after the dura mater and arachnoid would be violated concurrently by endoscopy during the procedures, and it could cause a ball-valve type phenomenon which led to entrapment of CSF followed by formation of arachnoid cyst.
Acquired spinal intradural cysts, which can be formed by trauma, infection, inflammation and haemorrhage, are uncommon spinal lesions. Only a few cases of iatrogenic spinal intradural cyst have been reported. Iatrogenic causes of acquired spinal arachnoid cyst have been presented following spinal injections, lumbar puncture, percutaneous vertebroplasty and lumbar spine surgery4,5,7,8) Mao et al.5), reported spinal extradural arachnoid cyst following percutaneous vertebroplasty. They suggested that the causes of arachnoid cyst formation might be extradural outpouchings of arachnoid that communicate with the intraspinal subarachnoid space via a small dural defect. Timothy et al., noted a case which showing symptomatic spinal intradural arachnoid cyst after lumbar myelography. In their case, arachnoid cyst was developed within 5 months after myelography. They proposed mechanical disruption of dura and arachnoid could make a symptomatic cyst. However, most of these arachnoid cysts are extradural, and none of iatrogenic spinal cyst following epidurography has been reported yet, although epidurography appears to have a high potentiality of incidental durotomy during the procedure.
Pain is the most common symptom followed by sensory changes, urinary dysfuction, and weakness4). Clinical symptoms are strongly dependent on the location of the intradural cyst, presumambly due to the difference in the diameter of the spinal canal6). Symptoms can be intermittent or slowly progressive and can be aggravated by increasing intraspinal pressure. In our case, the patient had only diffuse back pain even though large size of the cyst compressed the cauda equina. This can be explained by two reasons, firstly the large diameter of the spinal canal in the lumbar spine and secondly, there was a defect in the spinal column, partial laminectomy site of the previous disc surgeries at L5, through which part of arachnoid cyst herniated out. This defect might increase the room for the cyst to expand, and induce decrease of intra-cystic pressure (Fig. 3).
CONCLUSION
Intradural cyst should be considered, if patient complains of new symptoms such as aggravation of back pain after epiduroscopy procedures in the lumbo-sacral spine. Surgery in the form of simple fenestration of the cyst may lead to improved outcome. All the procedures using epiduroscopy should be performed with caution especially in patients who have a history of previous lumbar operations.
References
- 1.Avellanal M, Diaz-Reganon G. Interlaminar approach for epiduroscopy in patients with failed back surgery syndrome. Br J Anaesth. 2008;101:244–249. doi: 10.1093/bja/aen165. [DOI] [PubMed] [Google Scholar]
- 2.Gillespie G, MacKenzie P. Epiduroscopy--a review. Scott Med J. 2004;49:79–81. doi: 10.1177/003693300404900301. [DOI] [PubMed] [Google Scholar]
- 3.Igarashi T, Hirabayashi Y, Seo N, Saitoh K, Fukuda H, Suzuki H. Lysis of adhesions and epidural injection of steroid/local anaesthetic during epiduroscopy potentially alleviate low back and leg pain in elderly patients with lumbar spinal stenosis. Br J Anaesth. 2004;93:181–187. doi: 10.1093/bja/aeh201. [DOI] [PubMed] [Google Scholar]
- 4.Kriss TC, Kriss VM. Symptomatic spinal intradural arachnoid cyst development after lumbar myelography. Case report and review of the literature. Spine (Phila Pa 1976) 1997;22:568–572. doi: 10.1097/00007632-199703010-00023. [DOI] [PubMed] [Google Scholar]
- 5.Mao HQ, Yang HL, Geng DC, Bao ZH, Tang TS. Spinal extradural arachnoid cyst following percutaneous vertebroplasty. Eur Spine J. 2011;20(Suppl 2):S206–S210. doi: 10.1007/s00586-010-1569-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nabors MW, Pait TG, Byrd EB, Karim NO, Davis DO, Kobrine AI, et al. Updated assessment and current classification of spinal meningeal cysts. J Neurosurg. 1988;68:366–377. doi: 10.3171/jns.1988.68.3.0366. [DOI] [PubMed] [Google Scholar]
- 7.Nottmeier EW, Wharen RE, Patel NP. Iatrogenic intradural spinal arachnoid cyst as a complication of lumbar spine surgery. J Neurosurg Spine. 2009;11:344–346. doi: 10.3171/2009.3.SPINE08844. [DOI] [PubMed] [Google Scholar]
- 8.Rincon F, Mocco J, Komotar RJ, Khandji AG, McCormick PC, Olarte M. Chronic myelopathy due to a giant spinal arachnoid cyst: a complication of the intrathecal injection of phenol. Case report. J Neurosurg Spine. 2008;8:390–393. doi: 10.3171/SPI/2008/8/4/390. [DOI] [PubMed] [Google Scholar]
- 9.Shah RV, Heavner JE. Recognition of the subarachnoid and subdural compartments during epiduroscopy : two cases. Pain Pract. 2003;3:321–325. doi: 10.1111/j.1530-7085.2003.03036.x. [DOI] [PubMed] [Google Scholar]