Abstract
Purpose
Varicose veins are a major problem worldwide and improvement in quality of life (QoL) is the ultimate goal after treatment of this benign disease. However QoL is highly dependent on personal and social factors. This study compares high ligation and stripping (HS) and radiofrequency ablation (RFA) in terms of QoL and recurrence in Korea.
Methods
A retrospective analysis of prospectively collected data between August 2006 and October 2008 was performed for patients undergoing HS and RFA at a single institution. QoL was assessed with a questionnaire preoperatively, at 3 months postoperatively and annually thereafter. Recurrence was assessed by Duplex ultrasound annually after surgery.
RESULTS
A total of 272 patients completed the questionnaire at 3 months. Among these patients, 155 patients returned for their annual follow-up. There were no significant differences between HS and RFA in global QoL scores, although RFA showed less pain. However, paresthesia rates were also higher after RFA. Recurrence rates were similar between the two modalities, although technical failures were more common after RFA.
Conclusion
Overall QoL and recurrence rates were similar between the two modalities. The benefits of RFA do not seem to be enough to overcome the higher costs of HS in Korea.
Keywords: Varicose veins, Radiofrequency catheter ablation, Recurrence, Quality of life
INTRODUCTION
Chronic venous disorder is a common problem worldwide with a clinical spectrum ranging from telangiectasias to ulcerations [1,2]. Surgery for varicose veins is very common, with more than 30,000 procedures being performed annually in Korea [3]. Traditionally, high ligation and stripping (HS) has been considered the gold standard of treatment for varicose veins. However, during the past decade, less invasive endovenous methods such as radio-frequency ablation (RFA), endovenous laser treatment (EVLT) or cryosurgery have gained popularity. Endovenous treatments have also shown good results in terms of safety and efficacy [4,5], and many studies have been performed to compare the advantages and limitations of one procedure over the other [6-9]. Comparison in the short-term involves issues such as postoperative complications, pain severity, hospital days and time for return to work [10]. In the long-term parameters such as paresthesia, improvement in quality of life (QoL) and recurrence/reoperation rates have been compared and cost-benefit analyses have been performed based on many of these parameters [11].
Recently the Society for Vascular Surgery (SVS) guideline for treatment of varicose veins recommended the preferential use of endovenous treatment (RFA or EVLT) over open surgery (HS) due to reduced convalescence, pain and morbidity [10]. However, this does not take into account specific issues such as the cost of each procedure or differences in ethnicity and social awareness. Every patient wants the best outcome with less pain and morbidity, with the ultimate goal of improved QoL after surgery. However, the change in QoL perceived by the patient is very subjective and can be influenced by several factors. In Korea, the cost of RFA is at least 4 to 5 times higher than HS, which can affect patient satisfaction after treatment. Furthermore, differences in social awareness as well as expectations in health related issues and cosmesis may differ significantly from one country to another, which can be reflected in QoL. Therefore this study was performed to compare differences in QoL and recurrence after HS and RFA for varicose veins in Korea.
METHODS
Preoperative workup
Under the approval of the Institutional Review Board, a retrospective review of prospectively collected data from patients who underwent treatment for varicose veins at Seoul National University Bundang Hospital between August 2006 and October 2008 was performed. Patients were given the choice of HS or RFA as treatment options (nonrandomization). Preoperative color duplex ultra-sonography was performed in all patients according to standard practice in Seoul National University Bundang Hospital by a single registered vascular technician with high level of expertise. Groin reflux was assessed with both the Valsalva maneuver and manual compression/release method, and other segment refluxes were assessed by manual compression/release method. The criteria used to define pathologic reflux was reverse flow lasting more than 0.5 seconds for the saphenofemoral junction (SFJ), saphenopopliteal junction (SPJ) or other superficial veins, and more than 1 seconds for deep veins. For perforator veins, reflux was diagnosed when reverse flow lasted more than 0.35 seconds.
Operative procedure
All varicose vein surgeries were performed on a day surgery basis in the operating room under monitored anesthesia care with local anesthetic infiltration. HS was performed with 2 to 4 cm incisions in the groin (great saphenous vein [GSV]) or popliteal area (short saphenous vein [SSV]) to expose the SFJ or SPJ, respectively. After ligating the SFJ or SPJ and all its tributaries, a stripper was inserted and the saphenous vein was stripped in a downward direction down to the proximal or mid-calf level (GSV) or distal calf (SSV). In some cases, the stripper was retrieved at the mid-thigh (GSV) or mid-calf (SSV) through separate stab incisions due to venous tortuosity. Superficial varices were also removed by phlebectomy and significant perforators were ligated using multiple stab incisions. Care was taken not to leave a long stump at the site of high ligation. For RFA, the VNUS Closure system (Covidien, San Jose, CA, USA) was used. By direct puncture or 1 to 2 cm cut down of the distal GSV or SSV, the Closure catheter was inserted into the saphenous vein and placed 1 to 2 cm distal to the SFJ or SPJ under ultrasound guidance. After copious injection of tumescent anesthesia around the entire circumference and length of the vein to be treated, RFA was performed according to the manufacturer's instructions, achieving temperatures of 120℃ for 20 seconds along the length of the vein. For the GSV, ablation was performed down to the proximal or mid calf, while for the SSV, ablation was done down to the distal calf. Superficial varices were also removed by phlebectomy and perforators were ligated through small incisions in the same manner as HS.
Quality of life assessment
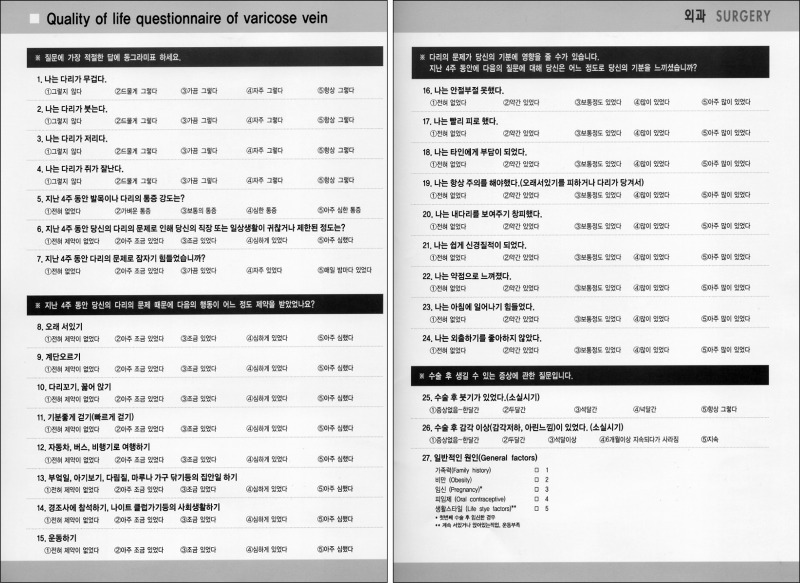
Routine long-term outpatient follow-ups were performed postoperatively at 3 months, 1 year and yearly thereafter. All patients were asked to complete a modified chronic venous insufficiency questionnaire 2 (CIVIQ2) (Appendix) [12] during their preoperative visit and also during their 3 month, 1 year and subsequent annual follow-ups. The original version [12] of this questionnaire was translated into Korean for use in our study. This questionnaire consisted of 24 questions categorized into 5 dimensions: discomfort, pain, physical, psychological and social. Response to each question was rated on a scale of 1 to 5, where 1 represented minimal negative effect on daily activities or well-being and 5 represented maximal negative effect. The scores of the five dimensions were combined to form a single global score. In addition to these five dimensions, we also evaluated postoperative duration of edema and paresthesia. The duration of edema was rated on a scale of 1 to 3, where 1 represented less than 1 month and 3 represented more than 3 months. Likewise, duration of paresthesia was rated on a scale of 1 to 4, where 1 indicated no symptoms and 4 indicated paresthesia for more than 6 months.
Recurrence assessment
Routine postoperative duplex ultrasound follow-up was performed annually and signs for possible recurrence were investigated. Recurrence was defined as visible varicosities or progression of remained varicosities which directly came from the deep vein system, SFJ, SPJ or perforators, regardless of symptoms and when there was a reflux of more than 0.5 seconds on duplex ultrasound. However, mild refluxes around the SFJ or SPJ without distal influence (no connection to the distal thigh or calf) were excluded. Additionally, refluxes in residual segments without aggravation compared to preoperative state or without definite source of origin were excluded. The patterns of recurrence were largely divided as same site recurrence and different (new) site recurrence, and each were classified as: technical failure, neovascularization, uncertain, mixed (same site), and de novo (different site).
Technical failure was defined as a failure to carry out technically adequate primary treatment, which in HS manifested as a remnant stump of more than 2 cm from the SFJ or severe reflux of the remaining below-knee segment of the GSV, while for RFA, technical failure mainly consisted of recanalization. Neovascularization was defined as reflux in thin serpentine veins arising from or near previously operated veins, and most cases of neovascularization arose at the stump of the high ligated vein after HS, sometimes with connections to veins going up to the pelvis, or in the remaining below-knee segment of the GSV.
The possible contributory factors were also analyzed not only between the 2 modalities but also between patients with and without recurrence. These factors included deep vein reflux (DVR), perforator vein reflux (PVR), family history and obesity (body mass index > 25).
Statistical analysis
All statistical analyses were performed using SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA). Categorical data were analyzed with the chi-square test and normally distributed continuous data were compared with the t-test/Student's t-test. The results were expressed as mean ± standard deviation, and P < 0.05 was considered statistically significant.
RESULTS
A total of 272 patients underwent varicose vein surgery at Seoul National University Bundang Hospital during the study period, of which 194 patients were treated by HS and 78 patients by RFA. All patients completed the CIVIQ2 preoperatively and at 3 months. After 3 months, patients were lost to follow-up and only 57% (155 patients) returned to the outpatient clinic for their annual follow-up, during which duplex ultrasound was performed. The median follow-up duration was 21 months (range, 8 to 34 months) and the CIVIQ2 data from their last follow-up (n = 112 for HS, n = 43 for RFA) were recorded and analyzed.
The clinical characteristics of patients are described in Table 1. There was no difference in mean age between the two groups, while there was an overall female predominance in the RFA group compared to HS, which was statistically significant. There was no difference in DVR or PVR between the two groups.
Table 1.
Clinical characteristic of patients in HS and RFA group
HS, high ligation and stripping; RFA, radiofrequency ablation; SD, standard deviation; DVR, deep vein reflux; PVR, perforator vein reflux.
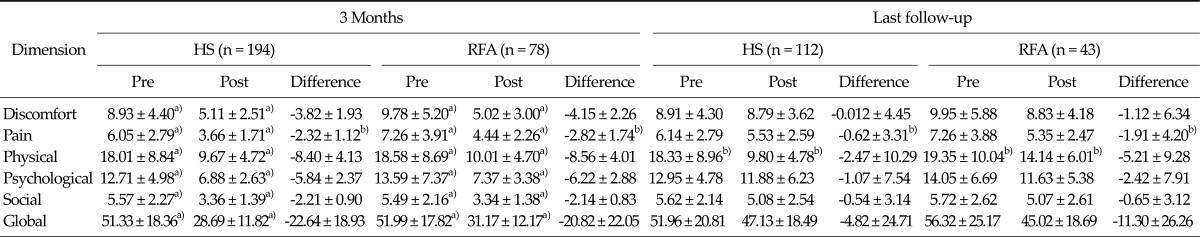
Modified CIVIQ2 scores prior to surgery were comparable in all dimensions between the two groups (P-values not shown). When the scores at 3 months were compared to preoperative scores, there was significant improvement in all dimensions and also in global scores in both groups. However, when the last follow-up scores were analyzed, such significance was lost in most of the dimensions, including global scores (Table 2).
Table 2.
Quality of life scores between HS and RFA
Values are presented as mean ± standard deviation.
HS, high ligation and stripping; RFA, radiofrequency ablation.
a)P < 0.001. b)P < 0.05.
When the differences in scores were compared between the two groups, only pain score was significantly in favor of RFA at both 3 months (-2.32 ± 1.12 in HS group vs. -2.82 ± 1.74 in RFA group, P = 0.015) and at last follow-up (-0.62 ± 3.31 vs. -1.91 ± 4.20, P = 0.046) (Table 2). The differences in scores decreased in the long-term, as shown by the smaller numbers at last follow-up compared to those at 3 months. Additionally, the overall differences in global scores were not statistically significant, and there was a tendency for HS to be better than RFA at 3 months in terms of global score (-22.64 ± 18.93 vs. -20.82 ± 22.05), although this was not so in the long-term.
Scores for edema were not significantly different between the two groups, while for paresthesia, the rates were significantly higher in the RFA group compared to the HS group (67.4% vs. 48.2%, P = 0.032), and most of the paresthesias (47.0%) lasted less than 1 month in the HS group, while in the RFA group, 55.6% lasted more than 6 months (data not shown).
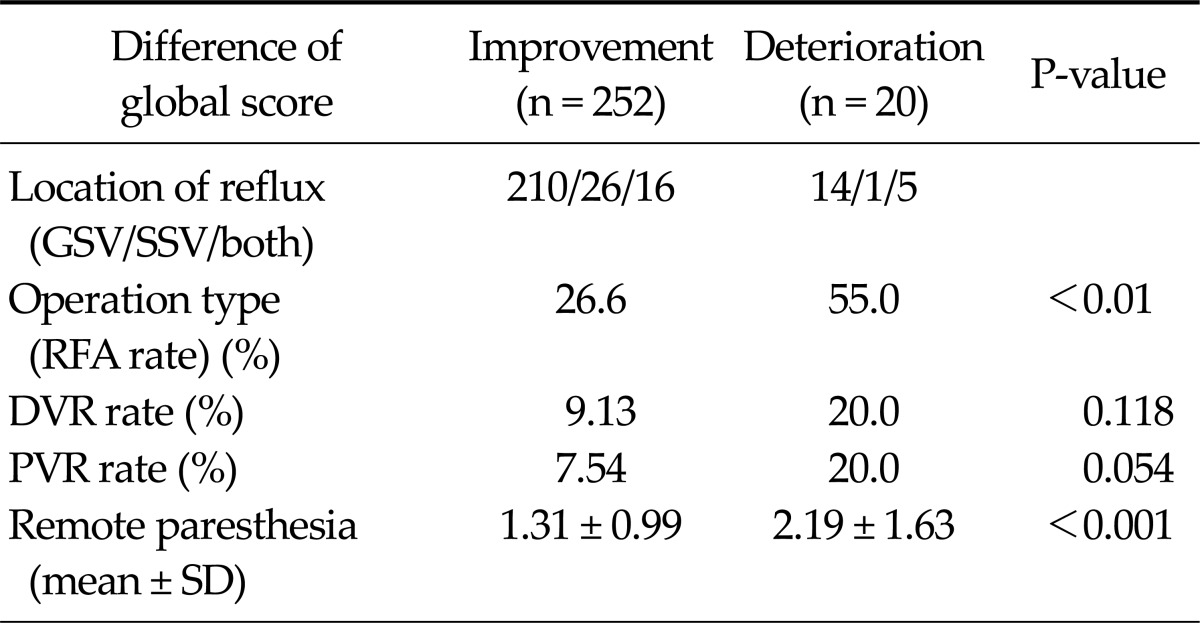
Patients with actual deterioration of global scores at 3 months after treatment were separately analyzed against patients who had improvement of scores. A total of 20 patients (7.4%) had a positive difference in global scores after treatment (deterioration), and factors involved in the deterioration were analyzed and compared against the remaining patients (252 out of 272 patients with improvement of scores after treatment). The results show that the type of operation was a significant factor, with 55.0% of patients having undergone RFA in the deterioration group compared to 26.6% in the improvement group (P = 0.007) (Table 3). The duration of paresthesia was also higher in the deterioration group as shown by the higher scores compared to the improvement group (2.19 ± 1.63 vs 1.31 ± 0.99, P < 0.001). However, DVR or PVR rates were not significantly different between the two groups.
Table 3.
Variables affecting quality of life score
GSV, great saphenous vein; SSV, short saphenous vein; RFA, radiofrequency ablation; DVR, deep vein reflux; PVR, perforator vein reflux; SD, standard deviation.
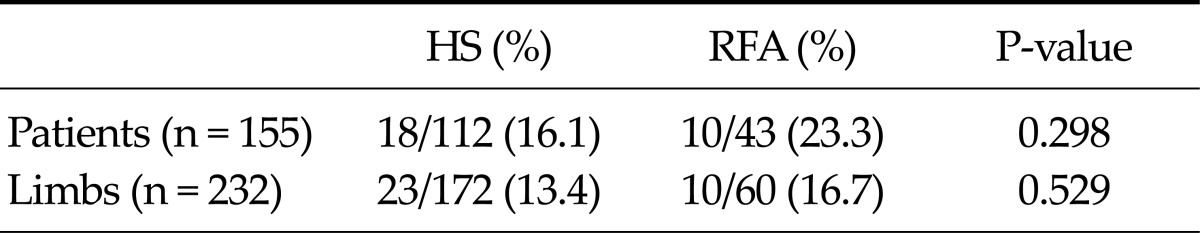
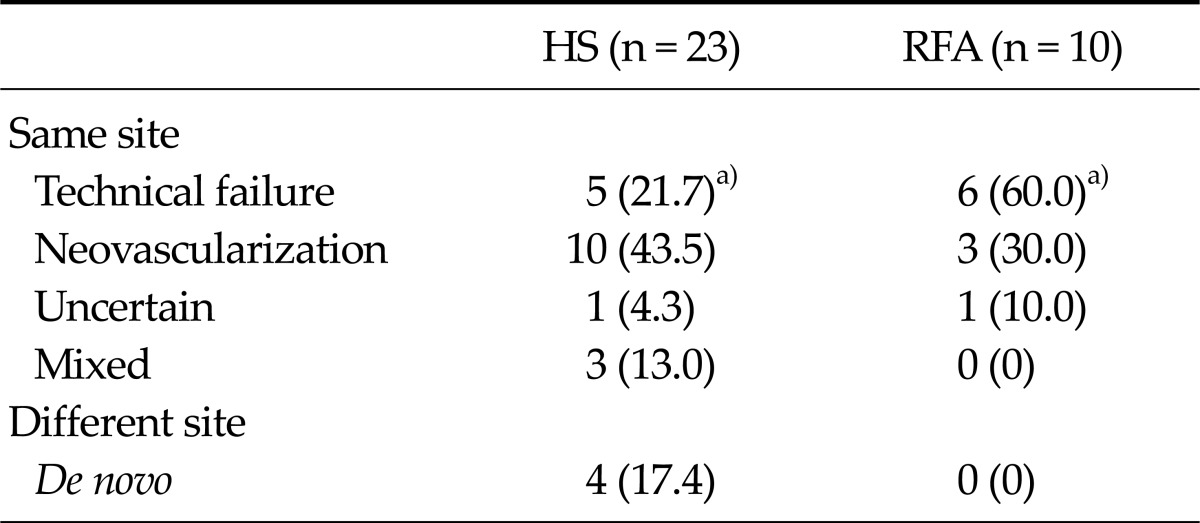
For analysis of recurrence, a total of 155 patients who underwent duplex ultrasound during their annual follow-up were included. A total of 232 limbs were included, of which 172 limbs from 112 patients were treated by HS, and 60 limbs from 43 patients were treated by RFA. During the follow-up period, recurrence was observed in 23 limbs from 18 patients in the HS group, and 10 limbs from 10 patients in the RFA group. Recurrence rates were not statistically significant between the two groups (Table 4). Analysis of the patterns of recurrence between the two groups showed that there was a higher rate of technical failure in the RFA compared with HS, with statistical significance (P = 0.014) (Table 5). There were 2 cases of full recanalization and 4 cases of partial recanalization (3 cases in the distal GSV and 1 case in the SFJ) in the RFA group. Recurrence due to neovascularization was not significantly different between the two groups, although there was a higher tendency for neovascularization to occur after HS. There was also a higher rate of mixed recurrence and new recurrences occurring at a site different from that of treatment after HS. Also analysis of the possible contributory factors for recurrence, such as DVR, PVR, family history and obesity, showed that none of these factors were significantly different between the two modalities or between patients with recurrence compared to those without recurrence (data not shown).
Table 4.
Recurrence rates after HS and RFA
HS, high ligation and stripping; RFA, radiofrequency ablation.
Table 5.
Patterns of recurrence after HS and RFA
Values are presented as number (%).
HS, high ligation and stripping; RFA, radiofrequency ablation.
a)P < 0.05.
DISCUSSION
The main findings of this Korean, single-center study comparing HS and RFA can be summarized as follows: firstly, improvement in QoL after treatment was similar between the two treatment modalities, as shown by the similar changes in global score, although pain was significantly in favor of RFA. Secondly, there was a significantly higher rate of patients with deterioration of QoL after RFA, and the incidence and duration of paresthesia was higher after RFA. Thirdly, there were no significant differences in recurrence between the two modalities, with recurrence rates being in the range of 13% to 17%. Finally, technical failures were more common after RFA, and there was a tendency for higher neovascularization after HS (without statistical significance).
Three randomized control trials [13-15] and one meta-analysis [8] have compared RFA with HS, with mixed results. In terms of QoL, Subramonia and Lees [14] showed an overall better improvement in QoL after RFA in the short-term, although different types of questionnaires showed different results. The EVOLVeS study reported a progressive decrease in QoL score change between 1 week and 4 months, but the differences reappeared at 1 year and remained significant at 2 years after treatment, showing long-term advantages of RFA [15,16]. On the other hand, Rautio et al. [13] showed that there was no difference in QoL scores between the two groups, with thermal injuries and symptomatic thrombophlebitis occurring in up to 20% of patients after RFA. In terms of recurrence, none of these randomized control trials showed significant difference in recurrence rates between HS and RFA. There was a tendency for higher neovascularization to occur after HS and technical failure or recanalization to occur after RFA, which is very similar to the results of our study.
Our study showed that both treatment modalities significantly improved QoL scores at 3 months after treatment, which justifies treatment in these patients, at least in the short-term, since there have been previous studies comparing treatment of varicose veins against conservative management [17-19]. In the long-term, these significant differences were lost, which may be due to recall bias, since patients have a tendency to forget or underestimate their preoperative symptoms. However, poor patient selection, procedure-related complications such as persistent paresthesias and recurrences may also account for these long-term results. When comparing HS and RFA, pain scores were better after RFA but overall global scores were not significantly different, and deterioration of QoL after treatment was significantly higher after RFA. Paresthesia rates were also higher after RFA, and the duration tended to be longer after RFA, with a significant number of patients showing deterioration of QoL after treatment due to paresthesia. Higher paresthesia rates after RFA may partly be explained by technical factors, since this study was performed not so long after the introduction of RFA at our institution (and also in Korea). Therefore, learning curve issues may have affected the results during the early periods of the study. Also the results may have been influenced by the use of the older version of the RFA system (Closure Plus, Covidien, San Jose, CA, USA) during the earlier stages of the study, with the introduction of the newer version (Closure Fast, Covidien) during the later periods. The newer version has the advantage of using a larger (7 cm) heating element that emits heat in all directions at higher temperatures compared to the older version, and studies that used the newer version have shown better occlusion rates than studies with the older version [20,21]. Such technical issues correlate with the significantly higher technical failure rates after RFA in terms of recurrence. In fact, most of our recurrences occurred in patients during the earlier phases of the study, which supports our suggestion. However, the mechanism of RFA itself involves thermal ablation of the vein, which may reach the skin or the nearby cutaneous nerves, leading to cutaneous neurosensory loss. There may be an unavoidable margin of thermal damage by the procedure itself no matter how technically well the procedure may have been performed. Also our recurrence rates were lower than those reported by other studies, demonstrating that not everything can be attributed to technical inexperience. Yet, it seems that the outcomes after RFA may be more sensitive to the skills of the surgeon and therefore may be technically more demanding.
The results of our study must be interpreted with caution. The major drawback is that the costs of the two modalities are different in Korea, with patients having to pay 4 to 5 times more for RFA than for HS. Other studies have shown that higher RFA costs are not always associated with higher overall costs since lower pain and earlier return to work can bring about lower societal costs [11-14]. However, QoL scores are usually not influenced by this since patients do not have perception on societal costs, and factors associated with societal costs or time in returning to work are usually different for each country, depending on social awareness. On the other hand, patient expectations are usually higher if the cost is higher, which influence satisfaction and therefore QoL scores after treatment [22,23]. This may explain for the nonsignificant difference in QoL scores between RFA and HS, since the degree of symptomatic improvement after RFA may be counteracted by the higher cost and expectation from the patient. Considering the similar QoL scores and recurrence rates in our study, the possible benefits reported by other studies may not be enough to overcome the higher costs, although a cost-benefit analysis may be needed to further clarify this issue.
This study has the limitation of being a nonrandomized study performed in a single institution and therefore selection bias may have affected the results, which makes direct comparison with previously published randomized control trials inadequate. Patient or doctor preference may have influenced the choice of treatment, however the baseline characteristics were only different for sex, with the female predominance for RFA reflecting their willingness for better cosmetic results. However the difference in cost makes a randomized control trial difficult to be performed. Also randomized control trials have the disadvantage of having smaller numbers overall, thus our study has the advantage of involving more subjects with long-term follow-up results.
In conclusion, HS and RFA for varicose vein treatment showed similar differences in QoL and recurrence rates. Pain was lower after RFA, but the incidence of paresthesia and technical failure rates were higher after RFA. In terms of QoL and recurrence, it seems that the possible benefits of RFA are not enough to justify for the higher costs in Korea.
ACKNOWLEDGEMENTS
This study was supported by a clinical research grant funded by the 1st Lee Yong Kak-Astellas Scholar Fund from the Korean Society for Vascular Surgery.
We thank Hanmi, Yun, RVT and Minjung Woo, RN for their technical assistance with duplex ultrasound imaging and data collection.
Appendix
Korean translation of the Chronic Venous Insufficiency Questionnaire 2
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Eklof B, Perrin M, Delis KT, Rutherford RB, Gloviczki P, et al. American Venous Forum. Updated terminology of chronic venous disorders: the VEIN-TERM transatlantic interdisciplinary consensus document. J Vasc Surg. 2009;49:498–501. doi: 10.1016/j.jvs.2008.09.014. [DOI] [PubMed] [Google Scholar]
- 2.Porter JM, Moneta GL International Consensus Committee on Chronic Venous Disease. Reporting standards in venous disease: an update. J Vasc Surg. 1995;21:635–645. doi: 10.1016/s0741-5214(95)70195-8. [DOI] [PubMed] [Google Scholar]
- 3.Ai L, Yu H, Takabe W, Paraboschi A, Yu F, Kim ES, et al. Optimization of intravascular shear stress assessment in vivo. J Biomech. 2009;42:1429–1437. doi: 10.1016/j.jbiomech.2009.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Darwood RJ, Gough MJ. Endovenous laser treatment for uncomplicated varicose veins. Phlebology. 2009;24(Suppl 1):50–61. doi: 10.1258/phleb.2009.09s006. [DOI] [PubMed] [Google Scholar]
- 5.Gohel MS, Davies AH. Radiofrequency ablation for uncomplicated varicose veins. Phlebology. 2009;24(Suppl 1):42–49. doi: 10.1258/phleb.2009.09s005. [DOI] [PubMed] [Google Scholar]
- 6.Rasmussen LH, Lawaetz M, Bjoern L, Vennits B, Blemings A, Eklof B. Randomized clinical trial comparing endovenous laser ablation, radiofrequency ablation, foam sclerotherapy and surgical stripping for great saphenous varicose veins. Br J Surg. 2011;98:1079–1087. doi: 10.1002/bjs.7555. [DOI] [PubMed] [Google Scholar]
- 7.Almeida JI, Kaufman J, Gockeritz O, Chopra P, Evans MT, Hoheim DF, et al. Radiofrequency endovenous ClosureFAST versus laser ablation for the treatment of great saphenous reflux: a multicenter, single-blinded, randomized study (RECOVERY study) J Vasc Interv Radiol. 2009;20:752–759. doi: 10.1016/j.jvir.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 8.Nesbitt C, Eifell RK, Coyne P, Badri H, Bhattacharya V, Stansby G. Endovenous ablation (radiofrequency and laser) and foam sclerotherapy versus conventional surgery for great saphenous vein varices. Cochrane Database Syst Rev. 2011;(10):CD005624. doi: 10.1002/14651858.CD005624.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Jung IM, Oh EM, Chung JK. Comparative study of postoperative complications of high ligation and stripping with endovenous laser treatment for varicose veins. J Korean Soc Vasc Surg. 2010;26:36–42. [Google Scholar]
- 10.Gloviczki P, Comerota AJ, Dalsing MC, Eklof BG, Gillespie DL, Gloviczki ML, et al. The care of patients with varicose veins and associated chronic venous diseases: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2011;53(5 Suppl):2S–48S. doi: 10.1016/j.jvs.2011.01.079. [DOI] [PubMed] [Google Scholar]
- 11.Subramonia S, Lees T. Radiofrequency ablation vs conventional surgery for varicose veins: a comparison of treatment costs in a randomised trial. Eur J Vasc Endovasc Surg. 2010;39:104–111. doi: 10.1016/j.ejvs.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 12.Launois R, Mansilha A, Jantet G. International psychometric validation of the Chronic Venous Disease quality of life Questionnaire (CIVIQ-20) Eur J Vasc Endovasc Surg. 2010;40:783–789. doi: 10.1016/j.ejvs.2010.03.034. [DOI] [PubMed] [Google Scholar]
- 13.Rautio T, Ohinmaa A, Perala J, Ohtonen P, Heikkinen T, Wiik H, et al. Endovenous obliteration versus conventional stripping operation in the treatment of primary varicose veins: a randomized controlled trial with comparison of the costs. J Vasc Surg. 2002;35:958–965. doi: 10.1067/mva.2002.123096. [DOI] [PubMed] [Google Scholar]
- 14.Subramonia S, Lees T. Randomized clinical trial of radio-frequency ablation or conventional high ligation and stripping for great saphenous varicose veins. Br J Surg. 2010;97:328–336. doi: 10.1002/bjs.6867. [DOI] [PubMed] [Google Scholar]
- 15.Lurie F, Creton D, Eklof B, Kabnick LS, Kistner RL, Pichot O, et al. Prospective randomized study of endovenous radiofrequency obliteration (closure procedure) versus ligation and stripping in a selected patient population (EVOLVeS Study) J Vasc Surg. 2003;38:207–214. doi: 10.1016/s0741-5214(03)00228-3. [DOI] [PubMed] [Google Scholar]
- 16.Lurie F, Creton D, Eklof B, Kabnick LS, Kistner RL, Pichot O, et al. Prospective randomised study of endovenous radiofrequency obliteration (closure) versus ligation and vein stripping (EVOLVeS): two-year follow-up. Eur J Vasc Endovasc Surg. 2005;29:67–73. doi: 10.1016/j.ejvs.2004.09.019. [DOI] [PubMed] [Google Scholar]
- 17.Barwell JR, Davies CE, Deacon J, Harvey K, Minor J, Sassano A, et al. Comparison of surgery and compression with compression alone in chronic venous ulceration (ESCHAR study): randomised controlled trial. Lancet. 2004;363:1854–1859. doi: 10.1016/S0140-6736(04)16353-8. [DOI] [PubMed] [Google Scholar]
- 18.Gohel MS, Barwell JR, Taylor M, Chant T, Foy C, Earnshaw JJ, et al. Long term results of compression therapy alone versus compression plus surgery in chronic venous ulceration (ESCHAR): randomised controlled trial. BMJ. 2007;335:83. doi: 10.1136/bmj.39216.542442.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Howard DP, Howard A, Kothari A, Wales L, Guest M, Davies AH. The role of superficial venous surgery in the management of venous ulcers: a systematic review. Eur J Vasc Endovasc Surg. 2008;36:458–465. doi: 10.1016/j.ejvs.2008.06.013. [DOI] [PubMed] [Google Scholar]
- 20.Zuniga JM, Hingorani A, Ascher E, Shiferson A, Jung D, Jimenez R, et al. Short-term outcome analysis of radio-frequency ablation using ClosurePlus vs ClosureFast catheters in the treatment of incompetent great saphenous vein. J Vasc Surg. 2012;55:1048–1051. doi: 10.1016/j.jvs.2011.11.050. [DOI] [PubMed] [Google Scholar]
- 21.Perrin M. Endovenous radiofrequency ablation of saphenous vein reflux. The VNUS Closure procedure with Closurefast. An updated review. Int Angiol. 2010;29:303–307. [PubMed] [Google Scholar]
- 22.Baker DM, Turnbull NB, Pearson JC, Makin GS. How successful is varicose vein surgery? A patient outcome study following varicose vein surgery using the SF-36 Health Assessment Questionnaire. Eur J Vasc Endovasc Surg. 1995;9:299–304. doi: 10.1016/s1078-5884(05)80134-0. [DOI] [PubMed] [Google Scholar]
- 23.O'Leary DP, Chester JF, Jones SM. Management of varicose veins according to reason for presentation. Ann R Coll Surg Engl. 1996;78(3 Pt 1):214–216. [PMC free article] [PubMed] [Google Scholar]