Abstract
Accidental or therapeutic total body exposure to ionizing radiation has profound pathophysiological consequences including acute radiation syndrome. Currently only investigational drugs are available in case of radiological or nuclear accidents or terrorism. Lack of selective radioprotectants for normal tissues also limits the therapeutic doses that can be delivered to treat cancers. CD47 is a receptor for the secreted protein thrombospondin-1. Blockade of thrombospondin-1 or CD47 provides local radioprotection of soft tissues and bone marrow. We now report that suppression of CD47 using an antisense morpholino increases survival of mice exposed to lethal total body irradiation. Increased survival is associated with increased peripheral circulating blood cell counts and increased proliferative capacity of bone marrow derived cells. Moreover, CD47 blockade decreased cell death while inducing a protective autophagy response in radiosensitive gastrointestinal tissues. Thus, CD47 is a new target for radiomitigation that prevents both hematopoietic and gastrointestinal radiation syndromes.
Total body irradiation (TBI) is currently used as a form of therapy for certain blood cancers and to prepare patients for bone marrow transplantation to prevent immune rejection. Furthermore, recent events remind us of the risk for exposure to TBI caused by natural disasters, civilian radiation accidents, terrorism, and warfare. As a therapeutic tool TBI can be effective in the killing of cancer cells. However, a major limitation of TBI is that it also targets essential normal tissues, which causes detrimental side effects to the patients that limit the effectiveness of therapy and increase the risk of death1. At sufficient doses, TBI leads to the onset of acute radiation syndrome (ARS)1,2. ARS includes three syndromes: hematopoietic, gastrointestinal, and neurovascular1,2. The development of these syndromes results from differential tissue radiosensitivities, and the severity depends on the amount of radiation absorbed by radiosensitive tissues. Furthermore, the manifestations and pathology associated with ARS involve interactions between radiosensitive organ systems and thus form a complex disease.
At a cellular level, exposure to Ionizing Radiation (IR) causes double strand breaks in DNA that lead to genomic instability and the generation of reactive oxygen species that activate a myriad of molecular signaling pathways, resulting in tissue damage and cell death. Current medical management of radiation injuries seeks to prevent damage by pretreatment with radioprotectants such as radical scavengers, post-exposure treatment with radiomitigators, such as the steroid 5-androstenediol and growth factors to stimulate tissue regeneration, and antibiotic treatment to prevent sepsis resulting from loss of mucosal barrier function3. Although significant progress has been made toward understanding the severe consequences experienced by exposed individuals, there are currently only five investigational agents and no FDA approved drugs to treat or prevent these harmful side effects of IR and the onset of ARS4.
CD47 is a widely expressed cell surface receptor that serves as a counter-receptor for signal regulatory proteins (SIRPs) and as a receptor for the secreted matricellular protein thrombospondin-15,6. Thrombospondin-1 signaling through CD47 regulates cellular signaling pathways that control cell survival, growth, motility, mitochondrial biogenesis, arterial vasoactive responses to physiologic vasodilators and blood flow, and responsiveness to growth factors7,8,9. Studies employing mice lacking either thrombospondin-1 or CD47 have revealed an important role for this receptor-ligand interaction in tissue responses to injury and stress. These null mice show enhanced recovery from soft tissue fixed ischemic injuries, ischemia reperfusion injuries, and radiation injuries10.
These studies have led to development of antisense strategies to locally or globally suppress CD47 gene expression. A translation-blocking CD47 morpholino improves tissue survival in skin flap and hindlimb fixed ischemia models, full thickness skin grafts, and a liver ischemia/reperfusion model of organ transplantation in mice11,12,13. We previously demonstrated that blockade with antibodies or anti-sense morpholinos to CD47 confers radioresistance to human endothelial cells in vitro and protects mice from the major acute and long term effects of local radiation injury including alopecia, deterioration of muscle function, soft tissue and cutaneous fibrosis, and loss of hematopoietic stem cells in bone marrow in vivo10,14. We recently reported that radioprotection by CD47 blockade requires the activation of autophagy15. CD47 deficient cells show increased autophagosome formation after IR. Treatment with IR increases beclin-1, ATG5, ATG7 and reduces p62/sequestosome expression in cells that lack CD47. Moreover, pharmacological blockade using CD47 morpholinos similarly increased autophagy gene up-regulation while causing a significant reduction in lung tissue apoptosis. This indicates that blockade of CD47 initiates protective autophagy to prevent cell and tissue death.
These studies led us to examine whether blockade of CD47 is effective for increasing survival of mice exposed to lethal total body doses of IR through an increase in autophagy. Here we examine the ability of CD47 blockade to maintain hematopoietic cell stability and protect the gastrointestinal system.
Results
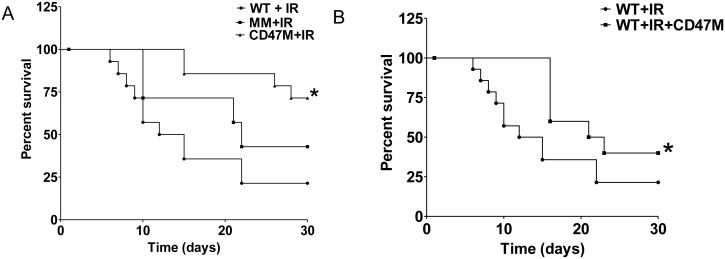
In vivo radioprotection by CD47 blockade
To determine the effect of CD47 blockade on survival of mice exposed to TBI, C57Bl/6 mice were treated with intraperitoneal (IP) injections of saline, 10 µM CD47 morpholino or 10 µM of 4-base mismatched control morpholino in saline. Two days after treatment, mice were exposed to a single dose of 7.6 Gy. Mice received food and water ad libitum. As observed in figure 1A, mice injected with saline started to succumb one week after radiation exposure. On the other hand, blockade of CD47 using anti-sense morpholino increased survival of the mice, with 100% surviving two weeks after radiation and 71.5% surviving at 30 days compared to 21.4% of WT animal injected with saline. To confirm that this effect was specific to CD47 blockade, mice were injected with a mismatched morpholino. Mice in the mismatched morpholino group started to die on day 10 and showed a 40% survival at day 30. Long-rank test statistical analysis revealed that treatment with the CD47 morpholino is beneficial for the survival of mice exposed to irradiation compared to the saline group and the mismatched morpholino treated animals (p<0.01). In a second set of experiments, mice were exposed to the same single dose of radiation and injected immediately after IR with either saline or 10 μM CD47 morpholino in saline. As observed in figure 1B, mice that were injected with CD47 morpholino after exposure to IR showed 40% survival versus 20% in the saline treated control, indicating that blockade of CD47 also increases survival of mice after exposure to IR.
Figure 1. Suppression of CD47 increases survival of mice exposed to total body irradiation (TBI).
(A) C57Bl6 mice were injected I.P. with Saline, 10 µM CD47 morpholino (CD47M), or a mismatched (MM) control morpholino. Two days later mice were exposed to 7.6 Gy TBI. N = 16 *p<0.005. (B) Mice were exposed to the same dose of radiation and were treated with CD47 morpholino after TBI, N = 10 *p<0.05.
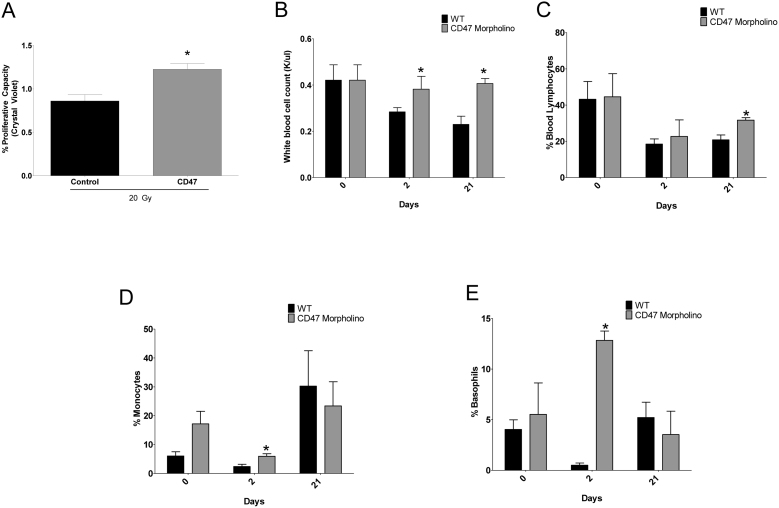
Suppression of CD47 preserves circulating peripheral blood cells
Since bone marrow viability can be a determining factor in survival of TBI16, we pretreated mice with CD47 morpholino, irradiated the mice, and then harvested bone marrow cells from femurs after 24 h and allowed the cells to grow in culture for 14 days. As observed in figure 2A bone marrow derived cells from irradiated mice pretreated with CD47 morpholino had a significant increase in proliferative capacity when compared to untreated irradiated animals. This indicates that the observed increase in survival of mice exposed to TBI with CD47 suppression is associated with preservation of bone marrow cell viability.
Figure 2. Suppression of CD47 preserves circulating peripheral blood cells.
(A) Bone marrow derived cells were collected from femurs of treated mice, and proliferative capacity was measured by a crystal violet assay (n = 3, *p<0.05). Treated mice were sacrificed, and trunk blood was collected at days 0, 2 and 21. Blood samples were submitted for complete blood cell counts to measure (B) white blood cells, (C) lymphocytes, (D) monocytes, and (E) basophils, n = 3–6 *p<0.05.
We pretreated a group of animals with CD47 morpholino in the same manner as our survival experiments and collected blood before and at 2 and 21 days after exposure to IR to quantify peripheral circulating blood cells. The repopulation of circulating blood cells after irradiation is a limiting factor in overcoming the harmful effects to exposure to TBI. Specifically, depletion of white blood cells including lymphocytes and myeloid cells after radiation increases the risk of death from infection16. CD47-null mice have normal white blood cell counts17 and consistent with this we saw no change in WBC counts following 48 h treatment with CD47 morpholino at the time of irradiation (Figure 2B). Control mice exposed to TBI showed the expected reductions in total circulating white blood cells and lymphocytes after IR (Figures 2B & 2C). Pharmacological suppression of CD47 preserved the levels of circulating lymphocytes at 2 days and 21 days after IR, indicating that blockade of CD47 prevents leuckocytopenia associated with IR exposure.
Suppression of CD47 alone resulted in an increased percentage of circulating monocytes but not basophils (Figures 2D & 2E). Irradiation resulted in decreased monocytes in treated and untreated mice at 2 days, which rebounded at 21 days. However, monocytes numbers were closer to basal levels at both time points in the CD47 morpholino-treated group. Basophils fell dramatically 2 days after irradiation in the control mice but were maintained in those pretreated with CD47 morpholino. At 21 days basophil percentages in both groups returned to normal. Preservation of basophils when CD47 was suppressed combined with the lack of elevated monocytes at 21 days may indicate a better ability to prevent or control infection, consistent with their improved survival.
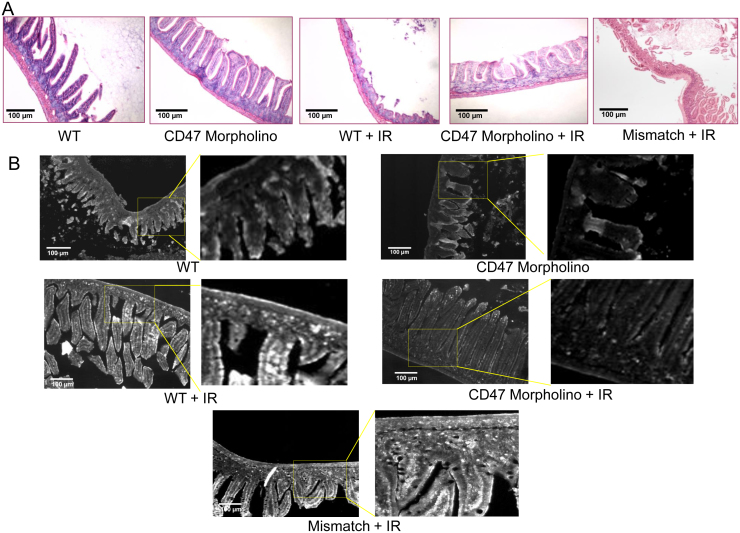
Suppression of CD47 protects intestinal mucosa from TBI
TBI can lead to the onset of the gastrointestinal syndrome, which is characterized by loss of the lining of the intestine and necrosis of tissue in the gastrointestinal tract. Normal villi were observed in the intestines of untreated WT and irradiated mice pretreated with CD47 morpholino (Figure 3A). On the other hand, we observed extensive loss of villi and thinning of the intestinal mucosa two weeks after exposure to TBI in control irradiated animals and those treated with the mismatched control morpholino. To assess programmed cell death, we performed TUNEL staining of tissue sections harvested at 24 h after exposure to TBI. As observed in figure 3B, treatment with CD47 morpholino alone has no effect when compared to intestinal tissue from control treated mice. On the other hand, strong TUNEL staining can be observed in a representative section of saline or mismatch-treated mice exposed to TBI, and a reduction in cell death was observed in mice pre-treated with CD47 morpholino when compared to the control group exposed to TBI. This indicates that blockade of CD47 protects the intestinal lining after TBI.
Figure 3. Suppression of CD47 protects intestinal tissue from IR.
(A) H&E staining of intestinal tissue harvested 14 days post radiation treatment. (B) Representative TUNEL assay of intestinal tissue 24 h post IR.
Blockade of CD47 protects esophageal tissue from death from ionizing radiation
To further explore the protective effects of CD47 blockade in the gastrointestinal system we assessed the structural integrity and tissue viability of esophageal tissue. As illustrated in figure 4A, we observed loss of the esophageal lining after 2 weeks in untreated WT mice exposed to TBI or those treated with mismatched control morpholino and exposed to TBI. On the other hand we observed intact mucosal layer in mice exposed to TBI that were pretreated with CD47 morpholino. We also observed a profound radioprotective effect as measured by the low TUNEL staining at 24 h in sections of CD47 morpholino-treated mice exposed to TBI when compared to saline or mismatch irradiated animals (Figure 4B). This indicates that blockade of CD47 broadly protects gastrointestinal mucosa to improve survival of mice exposed to TBI.
Figure 4. Suppression of CD47 prevents apoptosis and protects esophageal tissue from IR.
(A) H&E staining of tissues harvested 14 days post-exposure to TBI shows structural integrity of esophagus tissue. (B) Representative TUNEL staining showing tissue cell death 24 post-exposure to TBI.
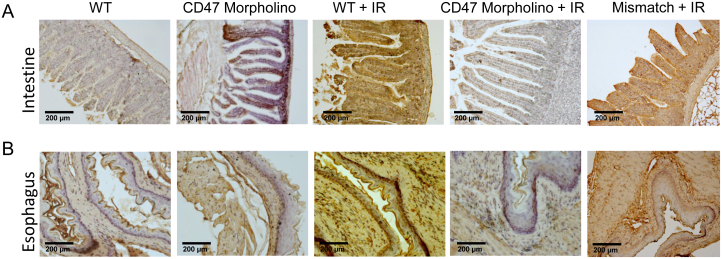
Suppression of CD47 reduces p62 after exposure to TBI
We have previously demonstrated that blockade of CD47 protects endothelial cells, T cells, and lung tissue from death from IR and that this effect is mediated by the activation of autophagy15. Immunohistological staining of intestinal and esophageal tissue indicated that blockade of CD47 and post treatment with IR decreases levels of p62, a molecular adaptor that is degraded upon activation of autophagy (Figure 5). In contrast, the corresponding tissues from control mice treated with saline or with the mismatched control morpholino and exposed to IR showed increased p62 staining, which indicates inhibition of autophagy. This expands on our previous studies and indicates that the increased in survival of radiosensitive tissues in animals exposed to TBI with CD47 blockade is associated with activation of autophagy.
Figure 5. Suppression of CD47 decreases p62 after IR.
Tissue sections of (A) intestine and (B) esophagus were harvested 24 h after IR. Tissue sections were fixed, paraffin embedded and stained with an antibody specific to p62.
Discussion
Our work shows for the first time that pharmacological inhibition of CD47 increases survival of mice exposed to whole body irradiation. The radioprotection is more effective when mice are pretreated, presumably due to the pharmacokinetics of delivering the morpholino to cells throughout the body and the kinetics of CD47 protein depletion due to normal metabolic turnover. However, we also show that blockade of CD47 confers some radioprotection when administered to mice after exposure to TBI. Additional studies will be required to determine the degree to which CD47 blockade could be utilized as a radiomitigation agent. Faster-acting CD47 blocking agents such as antibodies or small molecules may be more effective for this purpose. Our data also extends previous observations demonstrating that treatment with CD47 protects against local radiation injury and protects normal tissue from lethal doses of IR14,15. The survival of mice that were treated with antisense morpholino to block CD47 is associated with preservation of circulating peripheral blood cells and protection of the gastrointestinal tract. Thus, CD47 blockade is effective against the hematopoietic and gastrointestinal aspects of ARS.
Antisense morpholinos are broadly use in research to efficiently suppress expression of genes in cells and in animal models18. However, these compounds are also emerging as effective therapeutic agents. Antisense morpholino therapy has been demonstrated to be effective as antiviral therapy and showed efficacy in a Phase 2 clinical trial for the treatment of patients with Duchenne muscular dystrophy by targeting human dystrophin pre-mRNA transcript and safety in a Phase 1 trial for prostate cancer patients targeting c-Myc19,20. Administration of these antisense compounds has come without major side effects, which indicates the great potential for an antisense morpholino targeting CD47 to be effective in a clinical setting. In this and our previous studies we did not observe any harmful side effects with CD47 blockade in rodents and pigs21. Other preclinical studies have blocked CD47 using an antibody without reporting any major complications22,23. Therefore targeting CD47 using morpholinos for the protection of accidental or therapeutic exposure to IR has high potential to be translated to the clinic.
In a previous study we demonstrated similar enhancement of tumor responses to local irradiation using local versus intraperitoneal administration of the CD47 morpholino14. In the present data we see additional evidence that systemically administered morpholino reaches a wide variety of cells and tissues. For example, in the esophagus programmed cell death detected by TUNEL staining was suppressed in a majority of cells throughout the mucosal layer and in the smooth muscle wall. Widespread protection of cells was also observed in the villi and wall of the intestine.
The increase in survival with CD47 blockade has several therapeutic implications. Blockade of CD47 protects circulating peripheral circulating blood cell counts including leukocytes and myeloid cells. Low white blood cell count or leucopenia is major side effect of exposure to high doses of irradiation and one of the several symptoms associated with ARS2. Leucopenia compromises the ability of the immune system to fight infections and can lead to death from secondary infections if sustained. Treatment with granulocyte colony-stimulating factor (G-CSF) is the only experimental therapy to address leucopenia that has emergency use IND approval, but its efficacy in lethally irradiated humans has not been established. Cell based therapies employing hematopoietic precursors to repopulate bone marrow are also under investigation for radiomitigation. Our results indicate that pretreatment with a CD47 morpholino maintains white blood cell counts and prevents the depletion of myeloid cells after TBI, indicating that pharmacological inhibition of CD47 can prevent symptoms of the hematopoietic radiation syndrome and increase survival after exposure to IR and increase the quality of life of patients undergoing radiotherapy for cancer. The immunocompromised state of individuals exposed to IR can also lead to proliferation and unbalanced growth of bacteria located along the gastrointestinal (GI) tract leading to infections24. The onset of gastrointestinal syndrome occurs as a consequence of cells dying along the lining of the digestive tract, this leads to severe anorexia, dehydration, electrolyte imbalance and compromises the barrier function that prevents systemic infection2. Radiation-induced esophagitis is a major dose-limiting side effect of thoracic radiation as widely employed for treatment of lung and breast cancers25. Only palliative treatments are currently available for clinical management of radiation-induced esophagitis26. Our data indicates that blockade of CD47 broadly prevents death of cells along the intestine and esophageal lining. This is associated with a reduction in intestinal crypt loss and cell death of the digestive tract lining. The mortality from gastrointestinal syndrome is high, and inadequate therapeutic interventions are available to treat it. Current treatments are limited to antibiotic support. Patients undergoing thoracic radiotherapy often experience radiation enteritis, which limits radiation dosage and is detrimental to patient quality of life. Therefore treatment to block CD47 could be a therapeutic option for preventing these gastrointestinal- associated pathologies.
Our previous studies show that the mechanism of radioprotection by CD47 is mediated by an increase in autophagy. Blockade of CD47 increased the autophagic flux in T-cells and endothelial cells that were protected from IR. Moreover, pharmacological inhibition or siRNA inhibition of autophagy related genes ATG5 and ATG7 or re-expression of CD47 in CD47 deficient cells sensitized cells to death by IR, indicating that the radioprotective effect is directly related to the absence of CD47. Moreover, the increased cell death in lung tissue of WT mice exposed to TBI could be prevented by blockade of CD47 and was associated also with an increase in the activation of autophagy in vivo. Therefore, activators of autophagy should be more broadly considered as potential therapeutic radioprotectants.
One concern about blocking CD47 in combination with radiotherapy of cancer is that it could also protect tumor cells from radiation. However, we have previously shown in both melanoma and squamous carcinoma models that blockade of CD47 does not protect solid tumors from IR14. Rather, CD47 blockade sensitizes tumors to radiation treatment. The mechanism is at present unknown but may involve selective radioprotection of tumor-associated immune cells.
Overall this work confirms that pharmacological inhibition of CD47 is radioprotective. Our results showing that CD47 treatment extends the life of mice exposed to TBI before and after treatment indicates that CD47 blockade is a feasible alternative in the search for countermeasure actions in the case of mass exposure to IR by accident or warfare. Also our data suggest that the radioprotective effects of CD47 blockade could reduce the hematological and gastrointestinal side effects associated with radiotherapy of cancer.
Methods
Animals
C57BL/6 mice were housed in a specific pathogen-free environment and had ad libitum access to standard rat chow and water. Care and handling of animals was under approved protocol LP-012 and was in compliance with standards established by the Animal Care and Use Committee of the National Cancer Institute.
Animal model of Total Body Irradiation
Mice were acclimated to the vivarium for 14 days before use to minimize differences in microflora that influence survival rates after TBI. Age and sex matched C57BL/6 wild type mice were injected IP with a 750 μl volume of 10 µM CD47 morpholino or a 4 base-mismatched control morpholino in saline or a saline control and were exposed to IR 48 h after treatment. To determine if blockade would protect mice after exposure to IR, the animals were treated with CD47 morpholino in the same manner after exposure to IR. A single radiation dose of 7.6 Gy was delivered by a Therapax DXT300 X-ray irradiator (Pantak, Inc., East Haven, CT) using 2.0-mm Al filtration (300 kVp) at a dose rate of 2.53 Gy/min. After irradiation, the animals were placed in cages as indicated above and observed daily.
Bone marrow derived cells proliferative capacity
Twelve week old C57BL/6 mice, were exposed to 7.6 Gy of irradiation to the hindlimb as described above. Mice were injected IP with equal volumes of saline or 10 μM CD47 morpholino in 750 μl of saline 48 h prior to irradiation. Twenty-four hours after irradiation, the mice were euthanized, and femurs were extracted from the irradiated hindlimbs under aseptic conditions. The femoral bone was cut at both joint ends, and a single cell suspension of bone marrow cells from each individual mouse was obtained by flushing the femoral cavity with 5 mL of cold RPMI containing 2% fetal calf serum using a 22-gauge needle. The suspension of bone marrow cells was filtered through a 40 μm nylon mesh cell strainer (Falcon, Becton Dickson Franklin Lakes, NJ USA) and centrifuged at 400 g for 10 min at 4°C. Cells were plated in triplicate from each mouse into 24 well plates. Cells were maintained for 14 days in a humidified 37°C incubator with 5% CO2 in air, and cell viability was measured using a crystal violet assay.
Immunohistochemistry
Tissue was harvested, paraffin embedded, and stained with an antibody specific for SQSTM1/p62 as reported previously15.
Tissue Apoptosis
The In Situ Cell Death Detection Kit, (Roche, Indianapolis, IN) was used following the manufacturer's recommendations and performed as described previously15. In brief, animals were sacrificed 24 h post irradiation (7.6 Gy), and tissue was embedded in paraffin blocks (American HistoLabs, Gaithersburg, MD). Tissue sections were examined for apoptosis employing 3′-hydroxy DNA strand breaks enzymatically labeled with fluorescein-dUTP.
Blood cell counts
Animals were exposed to TBI as explained above, and trunk blood was collected into EDTA containing tubes. Samples were processed for complete blood cell count by the Department of Laboratory Medicine, Clinical Center, NIH, Bethesda, Maryland.
Author Contributions
D.R.S.-P. and D.D.R. conceived and designed the experiments. D.R.S.-P. and L.A.R. performed experiments and analyzed data. D.R.S.-P., D.A.W. and D.D.R. wrote the manuscript.
Acknowledgments
This work was supported by the Intramural Research Program of the NIH/NCI (D.D.R., D.A.W.) and by a by a NCI Director's Career Development Innovation Award (D.R.S.-P.).
References
- Heslet L., Bay C. & Nepper-Christensen S. Acute radiation syndrome (ARS) - treatment of the reduced host defense. Int J Gen Med 5, 105–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorr H. & Meineke V. Acute radiation syndrome caused by accidental radiation exposure - therapeutic principles. BMC Med 9, 126 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao M., Inal C. E., Parekh V. I., Li X. H. & Whitnall M. H. Role of NF-kappaB in hematopoietic niche function of osteoblasts after radiation injury. Exp Hematol 37, 52–64 (2009). [DOI] [PubMed] [Google Scholar]
- Singh V. K., Ducey E. J., Brown D. S. & Whitnall M. H. A review of radiation countermeasure work ongoing at the Armed Forces Radiobiology Research Institute. Int J Radiat Biol 88, 296–310 (2012). [DOI] [PubMed] [Google Scholar]
- Soto-Pantoja D. R., Isenberg J. S. & Roberts D. D. Therapeutic Targeting of CD47 to Modulate Tissue Responses to Ischemia and Radiation. J Genet Syndr Gene Ther 2 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts D. D., Miller T. W., Rogers N. M., Yao M. & Isenberg J. S. The matricellular protein thrombospondin-1 globally regulates cardiovascular function and responses to stress via CD47. Matrix Biol 31, 162–169 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frazier E. P. et al. Age-dependent regulation of skeletal muscle mitochondria by the thrombospondin-1 receptor CD47. Matrix Biol 30, 154–161 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isenberg J. S. et al. CD47 is necessary for inhibition of nitric oxide-stimulated vascular cell responses by thrombospondin-1. J Biol Chem 281, 26069–26080 (2006). [DOI] [PubMed] [Google Scholar]
- Isenberg J. S., Martin-Manso G., Maxhimer J. B. & Roberts D. D. Regulation of nitric oxide signalling by thrombospondin 1: implications for anti-angiogenic therapies. Nat Rev Cancer 9, 182–194 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isenberg J. S. et al. Thrombospondin-1 and CD47 limit cell and tissue survival of radiation injury. Am J Pathol 173, 1100–1112 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isenberg J. S. et al. Increasing survival of ischemic tissue by targeting CD47. Circ Res 100, 712–720 (2007). [DOI] [PubMed] [Google Scholar]
- Isenberg J. S. et al. Treatment of liver ischemia-reperfusion injury by limiting thrombospondin-1/CD47 signaling. Surgery 144, 752–761 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isenberg J. S. et al. Blockade of thrombospondin-1-CD47 interactions prevents necrosis of full thickness skin grafts. Ann Surg 247, 180–190 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxhimer J. B. et al. Radioprotection in normal tissue and delayed tumor growth by blockade of CD47 signaling. Sci Transl Med 1, 3ra7 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soto Pantoja D. R. et al. CD47 deficiency confers cell and tissue radioprotection by activation of autophagy. Autophagy 8, 0–1 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulkarni S., Ghosh S. P., Hauer-Jensen M. & Kumar K. S. Hematological targets of radiation damage. Curr Drug Targets 11, 1375–1385 (2010). [DOI] [PubMed] [Google Scholar]
- Reinhold M. I., Green J. M., Lindberg F. P., Ticchioni M. & Brown E. J. Cell spreading distinguishes the mechanism of augmentation of T cell activation by integrin-associated protein/CD47 and CD28. Int Immunol 11, 707–718 (1999). [DOI] [PubMed] [Google Scholar]
- Bill B. R., Petzold A. M., Clark K. J., Schimmenti L. A. & Ekker S. C. A primer for morpholino use in zebrafish. Zebrafish 6, 69–77 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sazani P., Weller D. L. & Shrewsbury S. B. Safety pharmacology and genotoxicity evaluation of AVI-4658. Int J Toxicol 29, 143–156 (2010). [DOI] [PubMed] [Google Scholar]
- Iversen P. L., Arora V., Acker A. J., Mason D. H. & Devi G. R. Efficacy of antisense morpholino oligomer targeted to c-myc in prostate cancer xenograft murine model and a Phase I safety study in humans. Clin Cancer Res 9, 2510–2519 (2003). [PubMed] [Google Scholar]
- Isenberg J. S. et al. Gene silencing of CD47 and antibody ligation of thrombospondin-1 enhance ischemic tissue survival in a porcine model: implications for human disease. Ann Surg 247, 860–868 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim D. et al. Anti-CD47 antibodies promote phagocytosis and inhibit the growth of human myeloma cells. Leukemia (2012). [DOI] [PubMed] [Google Scholar]
- Rogers N. M., Thomson A. W. & Isenberg J. S. Activation of Parenchymal CD47 Promotes Renal Ischemia-Reperfusion Injury. J Am Soc Nephrol 23, 1538–1550 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahraus C. D. et al. Rifaximin diminishes neutropenia following potentially lethal whole-body radiation. Exp Biol Med (Maywood) 235, 900–905 (2010). [DOI] [PubMed] [Google Scholar]
- Rose J., Rodrigues G., Yaremko B., Lock M. & D'Souza D. Systematic review of dose-volume parameters in the prediction of esophagitis in thoracic radiotherapy. Radiother Oncol 91, 282–287 (2009). [DOI] [PubMed] [Google Scholar]
- Berkey F. J. Managing the adverse effects of radiation therapy. Am Fam Physician 82, 381–388, 394 (2010). [PubMed] [Google Scholar]