Abstract
Objective
To identify trajectories of depressive symptoms in older community residents.
Method
Depressive symptomatology, based on a modified Center for Epidemiological Studies–Depression scale, was obtained at years 0, 3, 6, and 10, in the Duke Established Populations for Epidemiologic Studies of the Elderly (N=4,162). Generalized growth mixture models identified the latent class trajectories present. Baseline demographic, health and social characteristics distinguishing the classes were identified using multinomial logistic regression.
Results
Four latent class trajectories were identified. Class 1-- stable low depressive symptomatology (76.6% of the sample); class 2 – initially low depressive symptomatology, increasing to the subsyndromal level (10.0%); class3 -- stable high depressive symptomatology (5.4%); class 4 –high depressive symptomatology improving over 6 years before reverting somewhat (8.0%). Class 1 was younger, male, with better education, health, and social resources, in contrast to class 3. Class 2 had poorer cognitive functioning and higher death rate. Class 4 had better health and social resources.
Conclusion
Reduction in high depressive symptomatology is associated with more education, better health, fewer stressful events, and a larger social network. Increasing depressive symptomatology is accompanied by poorer physical and cognitive health, more stressful life events, and greater risk of death.
Keywords: depressive symptomatology, trajectories, community sample, longitudinal, elderly
Introduction
Our focus is on a little-studied area -- the natural history of depressive symptomatology in older community residents. There are many studies of the prevalence, but fewer of the incidence, of depression in the elderly. They tend to agree that depression is less prevalent in older than in younger groups, but may increase in the oldest old (1-3). There is inconsistent agreement with respect to the demographic characteristics with which depression is associated (age, gender, education, income, race/ethnicity), and whether depression is a risk factor for or a consequence of certain physical and mental health conditions and functional difficulty (1, 2, 4-14). There is, however, good agreement that social ties and stressful life events are associated with depression (6, 15-19), that comorbid medical conditions may portend a poorer outcome, and that depressive symptoms are costly to the health system and may increase risk of death (20-22).
To date, the history of depression in older adults has focussed primarily on those already depressed, and determining the course of their disease (23-26, 27). The main patterns of the natural history of depressive symptoms – their increase and decline -- have rarely been examined (6), and in an older population are barely known (10, 17).
Cui and colleagues (7) used longitudinal cluster analysis to examine the course of depression over two years in primary care patients present throughout (N=319, 81.4% of the initial sample; noncompleters excluded). They argued that such patients were representative of persons their age, since most older people do seek primary care, but few older persons with significant depression go to a specialist. Diagnosis and severity were based on the Structured Clinical Interview for DSM-III-R (SCID), and the Hamilton Rating Scale for Depression. Importantly, patients ranged from those with no depression to those with major depressive disorder. Six longitudinal clusters best described the findings. Three clusters were constant over the two years: cluster 1, consistently non-depressed (48.6%); cluster 3, consistently at a subsyndromal level (21.6%); and cluster 5, consistently at a depressed level (4.7%). Of the three remaining clusters, two indicated increased depression: cluster 4 (11.9%), started as nondepressed, but became subsyndromal; cluster 6 (5.6%) declining from the subsyndromal level to major depression. One cluster improved from minor depression to subsyndromal/nondepressed (cluster 2, 7.5%). The only characteristics that distinguished the clusters in multivariate analysis were score on the Cumulative Illness Rating Scale, the Hamilton depression rating scale, and functional status.
Lincoln & Takeuchi (10) used data gathered on four occasions over 16 years in the Americans' Changing Lives Study (N = 3,482 African Americans and Whites age 25 and over at baseline, 34% age 65+). Depressive symptomatology was determined by an 11-item Center for Epidemiological Studies-Depression (CES-D) scale (28). Information on subjects who dropped out during the study was included to the extent that it was present. Four trajectories of depressive symptomatology were identified using growth mixture modeling. Two trajectories were stable, one of low symptomatology (68.4% of the sample), and one of high symptomatology (4.8%). Two trajectories showed change: initially high symptoms in which symptoms improved (15.4%), and initially low symptoms, in which symptoms increased (11.4%). While there is good agreement between these two studies, information from additional representative samples of older community residents is desirable.
Aims of the study
The present study identifies 10-year latent class trajectories of depressive symptomatology in an older community-representative sample, and determines whether these trajectories can be distinguished at baseline by their demographic characteristics, health status, social factors, and by risk of death. We also examine potential predictors of risk for and improvement from depressive symptoms.
Material and methods
Sample
Data came from sample members of the Duke Established Populations for Epidemiologic Studies of the Elderly (Duke EPESE) residing in one urban, and four rural counties in the north-central Piedmont of North Carolina (29, 30). Of the 5,221 persons age 65 and over who were selected using stratified random household sampling, 4,162 (80%) were successfully interviewed. Of these, 2,261 (54%) were African-American, who were deliberately over-sampled to improve statistical precision for this group. African Americans represent 35% of the older population in the geographical area. Of the remainder, 1,875 (45%) were White, and 26 were of other race/ethnicity; 35% were male. Roughly half came from the urban and half from the rural counties. Sample members were interviewed in person at home at baseline (1986/1987), and 3, 6, and 10 years later, with telephone contact at followup years 1, 2, 4 and 5. Information on depressive symptomatology was obtained only at the in-person interviews. Attrition for reasons other than death was minimal. Annual response rates of survivors ranged from 93.7%-98.7% through the first seven waves, and 92.3% (N = 1,767) at the final wave. For the current study we excluded the sample members of “other race”, and those who provided no information on depressive symptomatology at baseline (162 proxy respondents, 3 others), yielding an analysis sample of 3,973 persons. This study was carried out with permission from the Duke Institutional Review Board. All participants provided signed consent.
Data gathered
Information on depressive symptomatology was obtained using a modified version of the 20-item Center for Epidemiological Studies-Depression (CES-D) scale (28). Response on each item was on a 2-point rather than a 4-point scale, indicating presence or absence of the symptom in the past week. Where relevant, items were reverse coded, so that the sum of the responses indicated the number of depressive symptoms endorsed. A value of 9 or greater on this modified CES-D (from a possible range of 0-20) has been found to be equivalent to a score of 16 or greater on the original scale, indicating clinically relevant depressive symptomatology (29).
Explanatory variables
Since previous reports indicated that at least one latent class was likely to represent a small percent of the sample (e.g., 5%), and analysis required multiple comparisons, we were necessarily parsimonious in selecting variables that, nevertheless, were expected to represent the three areas of primary interest: demographic, health, and social.
Demographic characteristics – the basic demographic information considered included age (continuous), race, sex, and education (continuous, but capped at 17 years). Health -- was assessed by three items. Two items were indicative of physical health: self-rated health (excellent (1), good, fair, poor (4)), and a functional status measure based on the sum of basic activities of daily living (ADL) (5 items (31)), OARS instrumental ADL items (7 items (32)), and abbreviated Rosow-Breslau scale (3 items, primarily mobility (32)), that could not be performed independently (possible range for the sum of the three measures: 0-15) (34). Cognitive status was assessed by number of errors on the 10-item Short Portable Mental Stratus Questionnaire (SPMSQ (35), possible range 0-10). Error scores were not corrected for race or education, since both of these variables were included in the model.
Social characteristics -- were assessed by the sum of stressful life events, e.g., divorce; death of spouse, child or friend; financial decline; relocation (possible range 0-14 (36)); a scale of social interaction with others (summarizing five variables measuring frequency of contact with friends and relatives, and membership in social organizations, possible range 0-39); and network size (summarizing seven variables on number of relatives and close friends, possible range 0-49).
Survival status -- For all participants, survival status through December 31, 1998 (twelve years post baseline) was determined by search of National Death Index records.
Statistical analyses
Initial analyses included basic descriptive statistics. Statistical software, M-plus version 5.1 (37) was used to identify distinct trajectories of CES-D scores using generalized growth mixture models (GGMM). The analyses started with an intercept only model, to which linear and quadratic growth factors were added to determine the forms of the growth model. A piecewise linear model best fit the data. The number of latent classes was determined by sequentially increasing the number of classes, and examining fit statistics including Akaike information criteria (AIC), Bayesian information criteria (BIC), sample size adjusted BIC (SSABIC), entropy and condition number. We also conducted sequential tests to determine if the decrease in likelihood ratio with increase in classes was statistically significant using the Lo-Mendell-Rubin test. Models were tested with a number of start values to ensure that proper solution was obtained. In addition, bootstrap-based testing, and theoretical and other considerations were used to determine the number of classes. The trajectories were identified based on CES-D scores alone. Associations between classes and categorical variables were assessed using chi-square tests, while associations between classes and continuous variables were determined using non-parametric Wilcoxon tests.
Multinomial logistic regression, with the most prevalent class as the referent, was used to determine the predictors of depressive symptomatology trajectory classes. The three groups of potential predictor variables (demographic, health, and social characteristics) constituted three chunks. To control for type 1 error, the significance of each group of variables was assessed separately in a chunk test. If a chunk was significant, the significant variables in the chunk were included in a final model. All three chunks were significant. Although age was not significant in the demographic chunk, we nevertheless included it because of its relevance in a study of older persons. The final model included sex, race, age and education; self-rated health, functional status, and cognitive status; and stressful life events, social network, and social interaction. All data were run unweighted, since weighting methods were not available for all statistical procedures. SAS version 9.2 was used for the logistic regression and descriptive analyses.
Results
At baseline, the sample ranged in age from 65 to 105 years, 54% were African American, 35% (both African Americans and Whites) were male. Over half had not gone beyond grade school. Health was rated between good and fair. A substantial proportion reported impairment in mobility and instrumental ADL, but few had any basic ADL impairments. On average, cognitive status was in the unimpaired range. At baseline, a majority had experienced one stressful life event (mean (standard deviation) 0.67 (0.95)); mean network size was 13.82 (7.10), and mean social interaction was 13.97 (6.76). The mean CES-D score was 3.2 (3.4), with 9.6% reporting 9 or more depressive symptoms. In the early years approximately 5% of the sample died each year, the percentage dying each year increasing with the age of the study.
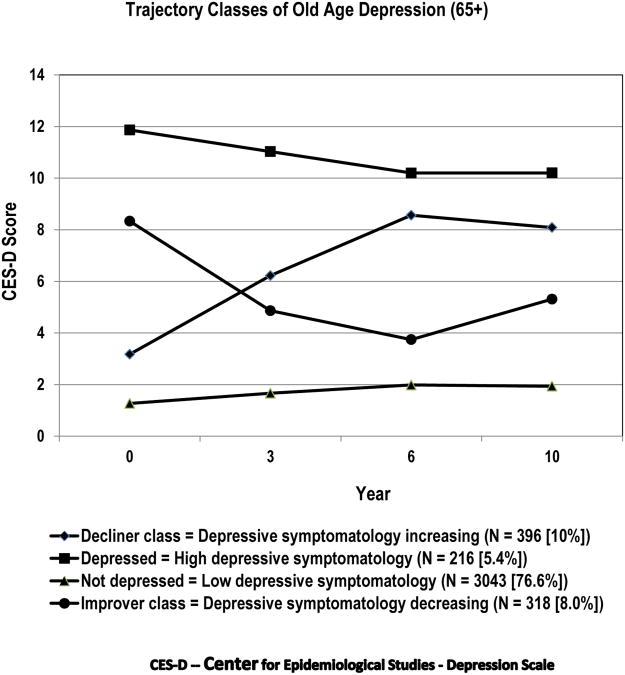
A four class model best fit the data. Participants were assigned to the class to which they had the highest probability of belonging. The four trajectory classes were a stable class with few depressive symptoms (n = 3043; 76.6%); a stable class with many depressive symptoms (n=216; 5.4%), where “stable” indicates consistency in number of depressive symptoms (score on the CES-D) over time; a class with an increasing number of depressive symptoms (labeled “decliners”) (n=396; 10.0%); and a class with a decreasing number of depressive symptoms (“improvers”) (n=318; 8.0%) (Figure 1). At baseline, the stable low symptoms class reported between 1 and 2 depressive symptoms, a level maintained throughout the study. The stable high symptoms class had a mean baseline modified CES-D score of 12, and maintained a score greater than 10 throughout. In the decliner class score increased from a baseline average of around 3 symptoms to approximately 9 symptoms (the cut-point that indicates clinically significant depressive symptoms on this version of the CES-D) 6 years later, before reversing slightly in the tenth year. Finally, the improver class initially had an average score of approximately 8.25, i.e., close to the CES-D cutpoint, improved over the first 6 years (to around 3 symptoms, the same starting point as the improver class), and then deteriorated slightly. Uncontrolled examination of the association of baseline characteristics with trajectory classes showed significant differences for all variables (Table 1) across classes.
Figure 1. Trajectory classes of depressive symptomatology.
The four trajectories are based on generalized growth mixture models of scores on the modified CES-D obtained at baseline, 3, 6, and 10 years later.
Table 1. Baseline Characteristics of the Trajectory Classes (mean (standard deviation), or N (%)) (n=3973).
| Low depressive symptomatology N=3043 (76.6%) | Depressive symptomatology decreasing (Improvers) N=318 (8.0%) | Depressive symptomatology increasing (Decliners) N=396 (10.0%) | Stable high symptomatology N=216 (5.4%) | P | |
|---|---|---|---|---|---|
| Demographic characteristics | |||||
|
| |||||
| Age (years) | 73.1 (6.4) | 73.4 (6.3) | 74.8 (7.1) | 73.5 (6.4) | .0001 |
| Race (White) | 1429 (47.0%) | 135 (42.4%) | 142 (35.9%) | 113 (52.3%) | .0001 |
| Female | 1908 (62.7%) | 239 (75.2%) | 278 (70.2%) | 164 (75.9%) | .0001 |
| Education | .0001 | ||||
| 0-8 years | 1472 (53.5%) | 198 (66.4%) | 270 (71.2%) | 140 (68.0%) | |
| 9-11 years | 788 (28.6%) | 69 (23.2%) | 78 (20.6%) | 47 (22.8%) | |
| ≥12 years | 493 (17.9%) | 31 (10.4%) | 31 (8.2%) | 19 (9.2%) | |
|
| |||||
| Health Status | |||||
|
| |||||
| Self-rated health1 | 2.3 (0.9) | 2.7 (0.9) | 3.1 (0.8) | 3.3 (0.8) | .0001 |
| Functional Status – | 1.42 (2.46) | 2.09 (2.82) | 3.43 (3.53) | 3.60 (3.38) | .0001 |
| Cognitive status2 | 1.55 (1.51) | 1.74 (1.33) | 2.27 (1.74) | 2.16 (1.81) | .0001 |
|
| |||||
| Social Factors | |||||
|
| |||||
| Stressful life events | 0.55 (0.84) | 0.82 (0.99) | 1.06 (1.16) | 1.44 (1.29) | .0001 |
| Social network | 14.06 (7.08) | 14.35 (7.51) | 12.54 (6.84) | 11.81 (6.66) | .0001 |
| Social interaction | 14.27 (6.81) | 13.97 (6.58) | 12.39 (6.55) | 12.45 (6.09) | .0001 |
|
| |||||
| Survival status 12 years after baseline | |||||
|
| |||||
| Number dead | 1833 (60.24%) | 192 (60.38%) | 289 (72.98%) | 143 (66.20%) | .0001 |
P values based on chi square tests (for categorical variables), and non-parametric Wilcoxon tests (for continuous variables).
Self-rated health is coded as excellent (1), good (2), fair (3), poor (4)
Cognitive status assessed by Short Portable Mental Status Questionnaire (Pfeiffer, 1975)
The stable low symptomatology class was younger, included a larger proportion of men, had more education, the best health status on each of the health measures, the fewest stressors, the highest social support, and (as with the improver class), the lowest death rate over 12 years (60%). The stable high symptomatology class was more likely to be White, reported the poorest health status, the largest number of stressors, the poorest social support, and two thirds died within 12 years. Compared to the improvers, the decliners were over a year older, included a larger proportion of African Americans, men, and people with less education. Their self-rated health, functional status, stressful life events and social support was comparable to that of the stable high symptomatology class; they had the poorest cognitive status of all the classes. At 73%, they had the highest rate of death.
Controlled analyses (multinomial logistic regression) included demographic (age, race, sex, education), health status (self-rated health, functional status, cognitive status), and social factors (stressful life events, social network, social interaction) (Table 2). Overall, each of the demographic, health status, and social factors variables, with the anticipated exception of age, significantly discriminated the four trajectory classes of depressive symptomatology. The weakest, aside from age, was race.
Table 2. Multinomial Logistic Regression. Baseline Associates of Trajectory Classes of Depressive Symptomatology (Reference trajectory class = stable low depressive symptomatology (76.6%)).
| Depressive symptomatology decreasing (8.0%) Improvers | Depressive symptomatology increasing (10.0%) Decliners | Stable high depressive symptomatology (5.4%) | Wald chi square | P | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| OR1 | 95% CI2 | OR | 95% CI | OR | 95% CI | |||
| Demographic characteristics | ||||||||
|
| ||||||||
| Female | 2.02 | (1.51-2.70) | 1.45 | (1.10-1.90) | 1.91 | (1.30-2.81) | 33.75 | 0.0001 |
| Age (years) | 1.04 | (0.80-1.34) | 0.99 | (0.77-1.27) | 0.90 | (0.64-1.26) | 0.51 | 0.9157 |
| White | 1.02 | (0.78-1.32) | 0.84 | (0.65-1.09) | 1.56 | (1.11-2.20) | 9.65 | 0.0218 |
| Education (years) | 0.95 | (0.91-0.98) | 0.96 | (0.93-0.99) | 0.95 | (0.91-0.99) | 14.57 | 0.0022 |
|
| ||||||||
| Health Status | ||||||||
|
| ||||||||
| Poorer self-rated health | 1.53 | (1.31-1.78) | 2.01 | (1.73-2.33) | 2.69 | (2.16-2.33) | 153.48 | 0.0001 |
| Poorer functional status | 1.03 | (0.98-1.08) | 1.10 | (1.05-1.14) | 1.09 | (1.03-1.15) | 23.58 | 0.0001 |
| Poorer cognitive status | 0.98 | (0.89-1.08) | 1.14 | (1.05-1.24) | 1.11 | (0.99-1.24) | 11.86 | 0.0079 |
|
| ||||||||
| Social Factors | ||||||||
|
| ||||||||
| Stressful events | 1.24 | (1.10-1.41) | 1.54 | (1.38-1.72) | 1.93 | (1.69-2.21) | 120.88 | 0.0001 |
| Larger social network | 1.04 | (1.01-1.07) | 1.00 | (0.97-1.02) | 0.96 | (0.93-1.00) | 11.96 | 0.0075 |
| Higher interaction | 0.96 | (0.94-0.99) | 0.96 | (0.94-0.99) | 0.98 | (0.95-1.02) | 11.61 | 0.0088 |
OR = Odds Ratio
CI = Confidence Interval.
Relative to the stable nondepressed class, OR <1.0 indicates reduced odds of the outcome, OR >1.0 indicates increased odds of the outcome.
Italicized values indicate significant difference from reference group (stable low depressive symptomatology).
Bolded values indicate significant difference between the two bolded classes in the table.
Separate analysis of demographic and CES-D characteristics predictive of death indicated that odds of death increased by 8% for each additional year of age (Odds Ratio [OR] =1.08; 95% Confidence Interval [CI]1.07-1.09, p <.0001), was 56% higher for men (OR = 1.56; 95% CI 1.34-1.82, p <.0001), declined by 3% for each additional year of education (OR = 0.97; 95% CI 0.95-0.99, p = .0022), and increased by 3% for each additional depressive symptom (OR = 1.03; 95% CI 1.01-1.06, p = .0034). Race was not a significant predictor. The inclusion of CES-D score in the model barely modified the demographic characteristics, indicating that depressive symptomatology made a unique contribution.
For each category of variables, we first make comparison with the reference group (stable low depression symptoms), and then compare the remaining three trajectory classes, in particular to identify significant differences among them.
Compared to the stable low symptomatology class, women had increased odds of being in one of the other classes – by 45% for the decliner class, and about double the odds for being in the stable high symptomatology or improver classes. Age was not associated with trajectory class, but race and education were relevant. Whites were 56% more likely than African Americans to be in the stable high symptomatology class than in the stable low symptomatology class. Race, however, did not distinguish either the decliner or improver classes from the reference group. Increased education reduced the odds of being in the decliner, improver, or stable high symptomatology trajectory class. In summary, the only associations found between demographic characteristics and trajectory class of depression were that being male, and reporting more years of education increased the odds of being in the stable nondepressed class, while being White increased the odds of being in the stable high symptomatology class. None of the demographic characteristics distinguished among the improver, decliner, or stable high depressive symptomatology classes.
Health was predictive of trajectory class. The stable low depressive symptomatology class had significantly better self-rated health than any of the other classes. The odds of poorer self-rated health was about 50% greater in the improver class, double in the decliner class, and 2⅔ greater in the stable high symptomatology class. The functional status of the improver class did not differ significantly from that of the stable low depressive symptomatology class, but the functional status of the decliner and stable high symptomatology classes was 10% poorer. Poorer cognitive status uniquely increased the odds of being in the decliner class. Comparison of the improver, decliner, and stable high symptomatology classes indicated that the self-rated health of the improver class was significantly better than that of the stable high symptomatology, but there were no statistically significant differences across these three classes with respect to functional status or cognitive status.
Regarding social factors, stressful life events were strongly associated with trajectory class. Compared to the stable low symptomatology class, the odds of stressful life events were nearly double for the stable high symptomatology class, about 50% higher for the decliner class, and about 25% higher for the improving class. Larger network size was associated with increased odds for the improver class. Higher social interaction had conflicting effects, reducing the odds of both improving and declining. It did not distinguish the stable high symptomatology class from the stable low symptomatology class. Comparison across improver, decliner, and stable high depressive symptomatology classes indicated that while stressful life events were significantly higher in the improver than in the low depressive symptomatology class, they were nevertheless significantly lower in the improver class than in the stable high depressive symptomatology class. In addition, the improver class had a significantly larger network than the stable high depressive symptomatology class.
In summary, with the exception of age, all the variables examined distinguished the stable low depressive symptomatology class from one or more of the other three trajectory classes. Four variables consistently distinguished the stable low depressive symptomatology class from all of the other three classes: gender (a significantly higher proportion of men), increased education, better self-rated health, and fewer stressful life events. Of these variables, self-rated health and stressful life events also distinguished the stable high depression symptomatology class from the improver class, the latter being in a more preferred position than the former (better self-rated health, fewer stressful events). The stable high depressive symptomatology class was distinguished by race (greater odds of being white), but otherwise shared characteristics with at least one other trajectory class. This class was most likely to report poorer self-rated health, and had nearly twice the odds of experiencing stressful life events. The decliner class was distinguished by poorer cognitive status, but they also reported poorer self-rated health and functional status, and had an increased odds of stressful life events. The improver class reported a larger social network than any of the classes, and their self-rated health, and stressful life events were second only to that of the stable low depressive symptoms class.
Discussion
We have examined the natural history of depressive symptoms in a representative sample of older community residents, who were followed for 10 years. Four latent class trajectories of depression were identified – a stable low depressive symptomatology class (77% of the sample), a stable high depressive symptomatology class (5%), a decliner class in which initially low depressive symptomatology increased over a period of 6 years before starting to revert (10%), and an improver class that started with higher depressive symptomatology which was reduced over time (8%).
The size of the stable classes is in line with expectation. Depression in the elderly is less prevalent than in younger persons (1), with rates based on symptom scales higher than rates based on clinical ascertainment. Our modified CES-D-based rate, indicating that at baseline 9.6% had substantial depressive symptomatology, is within the range of 8%-16% reported (1). The general pattern of classes is similar to that found in the clinical sample of Cui et al. (17), and remarkably comparable to that of Lincoln & Takeuchi (10), who identified trajectories in a mixed-age community sample. The main difference between our study and that of Lincoln & Takeuchi (10) is that we report a higher percentage in the non-depressed class. This may reflect the lower age of their sample, since depression appears to be more prevalent in younger age groups. The more complex class structure found by Cui et al. (17), and the much smaller proportion who were not depressed, may reflect both differences in depression ascertainment (a quasi-clinical approach was used), and initial identification of subjects through medical visits, where a higher proportion of persons with depressive symptoms and with more severe depression are generally found (38-40). Our rates for stable high symptomatology agree well with findings from both studies (around 5%).
Further, the characteristics of the stable high symptomatology class found in the present study agree with the characteristics for depression that have been identified in several studies: female, white, in poorer health, and with stressful life events (1, 2, 4-19, 23, 41, 42). Race, while statistically significant, distinguished only those who were consistently depressed from those who were declining. Within the declining class, however, there was no race effect. Rather, this variable emphasized characteristics already known, in particular, the increased likelihood of greater depressive symptomatology in Whites. Aside from this, race seems to play no role in distinguishing among trajectory classes – for this sample, the findings apply regardless of race.
The only characteristics potentially modifiable at an older age that distinguish the stable high depressive symptomatology class from the stable low depressive symptomatology class are poorer self-rated health and functional status. Level of education, which also distinguishes these two classes, is probably better addressed in the early years, and many stressful life events, but not necessarily all, are outside individual control. It is possible that interventions resulting in better personal health care (we know that depression is associated with poorer personal care of health (42, 44)), improved functional status, and greater ability to handle life events could ameliorate problems in the stable high depressive symptomatology class.
What is of considerable interest, however, is the apparent flexibility within the group with substantial depressive symptomatology – a larger proportion improves than stays depressed (8% vs 5.4%), and there is a 9% reduction in the death rate. The long-term instability (i.e., improvement) of the high symptomatology class has also been reported for clinical depression (23 and articles surveyed there).
Comparison of the stable high symptomatology and the improver classes indicates that the latter reports significantly better self-rated health, fewer stressful life events, and a larger social network. The reason for the difference in self-rated health is unclear, since the health conditions reported by the two classes over time, and their use of antidepressants differ little, although functional status was consistently better (data not shown), suggesting that illness may have been less severe, or better controlled. Thus, the improvers may be a group with milder comorbidity, and relatively fewer stressful life events, for whom improvement in health and coping with problems is more feasible, possibly aided by a larger social network that can provide a greater range of desirable contacts. Their 12-year survival is comparable to that of the stable low depressive symptomatology class. In short, it may be necessary to look at a constellation of factors in order to identify which persons, among those with multiple depressive symptomatology, have a greater odds of improving.
While it is important to identify characteristics indicative of likelihood of improvement, it is also important to identify characteristics that could result in the reverse effect. The main characteristic that identifies the decliner class is poorer cognitive status. This may make it difficult for them to cope with poorer self-rated health and functional status, and an increased number of stressful life events. It is possible that this is a group with impending dementia, and so for this reason alone should be followed carefully (43). They have the highest risk of death within 12 years (20% higher than for the improver class, or the stable low depressive symptomatology class). This may be related to the constellation of negative characteristics (poorer health and cognitive status, increase in depressive symptomatology) each of which has been found to be associated with increased risk of mortality (22). It is notable that persons with severe cognitive impairment were not included in the current analysis sample, because of inability to respond to the CES-D. Thus, current findings indicate that even mild cognitive impairment is associated with increased depressive symptomatology and death. Both the improver and decliner classes have a similar level of social interaction, that is lower than in the stable low symptomatology class. The quality of this interaction (e.g., whether supportive or abrasive) is not known, but may differ between the two groups.
This study has several limitations. The measure of depression (the CES-D) is based on symptomatology, and not on clinical diagnosis, nevertheless, it has been widely used and is well accepted. Some nonrepeatable stressful life events likely occurred more than a year before the start of the study (the look-back period), some potential events only applied to a subsample, and the effect of events may vary depending whether they are “on time” or not. Information was gathered at fairly lengthy intervals (3, 6, and 10 years after baseline), and so did not capture fluctuations in depressive symptomatology that might have occurred in the interim. We also do not know the past history of depression, and so cannot control for this. Because of sample size issues, we were unable to take into account events occurring during the 10-year period which could have affected depressive symptomatology. Probably for similar reasons, both the Cui et al. (17) and the Lincoln & Takeuchi (10) studies also used only baseline data to try to distinguish among the trajectories. While ideally, intervening events should be taken into account, practically longitudinal samples of sufficient size that would permit such preferred analysis are rarely available because of sample attrition, typically due to mortality, and the substantial number of statistical comparisons that are necessary. There may be concern because the data are 15 to 25 years old. Unless the changes that occurred between data gathering and publication affected the matter of interest, we would expect the findings to remain valid.
Some of our explanatory variables are essentially unmodifiable (date of birth, sex, race, education), others are person-specific (cognitive status, personal stressors, social contacts), and only two (self-rated health, functional status) may have been subject to secular modification. Over the last 25 years, the proportion of older people in the population and their longevity has been increasing, and functional status has been improving (46), although some studies show flattening in improvement in functional status since the mid 1990s (47), suggesting that findings from the current study should still hold. However, obesity with its attendant health problems is creeping into the older ages; there is concern that gains in health may not only be eliminated, but reversed (48), and political problems abound. All longitudinal, and many cross-sectional studies are faced with such problems. Only future studies can determine whether current findings remain relevant. As investigators we are constantly faced with such concerns, to which there is no good answer. Finally, this study was carried out in the southeastern area of the U.S., where health conditions and extent of depressive symptomatology have been found to differ from other parts of the U.S., reducing generalizability (7).
Nevertheless, this is one of the few studies to date that tries to identify the alternative courses that depressive symptoms in the elderly may take over time, and under usual circumstances. As such it indicates that the majority enter older age with their depressive symptomatology path set. For about one in five, however, depression symptomatology appears to be maliable, but in order to capitalize on this it may be necessary to look for a constellation of conditions associated with depressive symptomatology. Approximately 60% with multiple depressive symptoms, whose circumstances may not be too dire, improve. But there is also a group of similar size, whose health and cognition decline, who develop depressive symptomatology, and have the highest risk of death within 12 years. For this group, additional recognition and intervention is needed.
Significant outcomes
Over a 10 year period, depressive symptoms remained stable for 82% of the sample (few symptoms for 77%, many symptoms for 5%).
The 10% whose depressive symptoms increased had poorer cognitive functioning, possibly indicative of a developing dementing disorder.
The 8% whose depressive symptoms declined had better health and social resources.
Limitations
Limited sample size for some trajectories, and high mortality restricted ability to take intervening events into account.
Our measure is of depressive symptomatology; while well-accepted in epidemiological studies, it is not a measure of clinical depression.
Acknowledgments
Data obtained through NIA Contract No. N01-AG12102 and research grant 5 R01 AG12765. Also supported in part by NCRR/NIH CTSA grant 5UL1 RR024128-04, NIMH grants 2P50-MH60451 and R01 MH080311, and NIA grant 5P30 AG028716 (Duke Pepper Older Americans Independence Center).
Footnotes
Declaration of interest: None of the authors (MNK, GGF, CFH, DGB) reports any financial or other relationship in general or relevant to the subject of this article over the period of the last two years.
Previous presentation: An earlier version of this paper was presented at the annual scientific meeting of the Gerontological Society of America, New Orleans, November 21, 2010.
References
- 1.Blazer DG. Depression in late life: Review and commentary. J Gerontol Series A: Biol Sci Med Sci. 2003;58:249–265. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- 2.Byers AL, Yaffe K, Covinsky KE, Friedman MB, Bruce ML. High occurrence of mood and anxiety disorders among older adults: The National Comorbidity Survey Replication. Arch Gen Psychiatry. 2010;67:489–496. doi: 10.1001/archgenpsychiatry.2010.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hybels CF, Blazer DG. Epidemiology and geriatric psychiatry. In: Tsuang MT, Tohan M, editors. Textbook in Psychiatric Epidemiology. New York: Wiley-Liss; 2002. pp. 603–628. [Google Scholar]
- 4.Blazer DG, Sachs-Ericsson N, Hybels CF. Perception of unmet basic needs as a predictor of depressive symptoms among community-dwelling older adults. J Gerontol Series A: Biol Sci Med Sci. 2007;62:191–195. doi: 10.1093/gerona/62.2.191. [DOI] [PubMed] [Google Scholar]
- 5.Chapman DP, Perry GS. Depression as major component of public health for older adults. [accessed online October 19, 2010];Preventing Chronic Disease Public Health Research, Practice and Policy. 2008 5:1–9. http://www.cdc.gov/pcd/issues/2008/jan/07_0150.htm. [PMC free article] [PubMed] [Google Scholar]
- 6.Colman I, Ataullahjan A. Life course perspectives in the epidemiology of depression. Canadian J Psychiatry. 2010;55:622–632. doi: 10.1177/070674371005501002. [DOI] [PubMed] [Google Scholar]
- 7.Gonzalez O, Berry JT, Mcknight-Eily LR, et al. Current depression among adults – United States, 2006 and 2008. MMWR Morbidity and Mortality Weekly Report. 2010;59(38):1229–1235. [PubMed] [Google Scholar]
- 8.Huang CQ, Dong BR, Lu ZC, Yue JR, Liu QX. Chronic diseases and risk for depression in old age: a meta-analysis of published literature. Ageing Research Reviews. 2010;9:131–141. doi: 10.1016/j.arr.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 9.Kim J, Durden E. Socioeconomic status and age trajectories of health. Soc Sci & Med. 2007;65:2489–2502. doi: 10.1016/j.socscimed.2007.07.022. [DOI] [PubMed] [Google Scholar]
- 10.Lincoln KD, Takeuchi DT. Variation in the trajectories of depressive symptoms, results from the Americans' Changing Lives Study. Biodemography Soc Biol. 2010;56:24–41. doi: 10.1080/19485561003709180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Penninx BW, Leveille S, Ferrucci L, van Eijk JT, Guralnik JM. Exploring the effect of depression on physical disability: longitudinal evidence from the Established Populations for Epidemiologic Studies of the elderly. Am J Public Health. 1999;89:1346–1352. doi: 10.2105/ajph.89.9.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schillerstrom JE, Royall DR, Palmer RF. Depression, disability and intermediate pathways: a review of longitudinal studies in elders. J Geriatr Psychiat Neurol. 2008;21:183–197. doi: 10.1177/0891988708320971. [DOI] [PubMed] [Google Scholar]
- 13.Yang Y. Is old age depressing? Growth trajectories and cohort variations in late-life depression. J Health Soc Behav. 2007;48:16–32. doi: 10.1177/002214650704800102. [DOI] [PubMed] [Google Scholar]
- 14.Cole MG, Dendukiri N. Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. Am J Psychiatry. 2003;160:1147–1156. doi: 10.1176/appi.ajp.160.6.1147. [DOI] [PubMed] [Google Scholar]
- 15.Beard JR, Tracy M, Vlhaov D, Galea S. Trajectory and socioeconomic predictors of depression in a prospective study of residents of New York City. Annals Epidemiol. 2008;18:235–243. doi: 10.1016/j.annepidem.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 16.Blazer DG, 2nd, Hybels CF. Origins of depression in later life. Psychol Med. 2005;35:1241–1252. doi: 10.1017/S0033291705004411. [DOI] [PubMed] [Google Scholar]
- 17.Cui X, Lyness JM, Tang W, Tu X, Conwell Y. Outcomes and predictors of late-life depression trajectories in older primary care patients. Am J Geriatr Psychiatry. 2008;16:406–415. doi: 10.1097/JGP.0b013e3181693264. [DOI] [PubMed] [Google Scholar]
- 18.Lynch SM, George LK. Interlocking trajectories of loss-related events and depressive symptoms among elders. J Gerontol Series B-Psychol Sci Soc Sci. 2002;57:S117–125. doi: 10.1093/geronb/57.2.s117. [DOI] [PubMed] [Google Scholar]
- 19.Zaninotto P, Falaschetti E, Sacker A. Age trajectories of quality of life among older adults: results from the English Longitudinal Study of Ageing. Quality of Life Research. 2009;18:1301–1309. doi: 10.1007/s11136-009-9543-6. [DOI] [PubMed] [Google Scholar]
- 20.Chapman DP, Perry GS, Strine TW. The vital link between chronic disease and depressive disorders: preventing chronic disease. [accessed online October 19, 2010];Public Health Research, Practice, and Policy (serial online) 2005 2:1–10. http://www.cdc.gov/pcd/issues/2005/jan/04_0066.htm. [PMC free article] [PubMed] [Google Scholar]
- 21.Ciechanowsli PS, Katon WJ, Russo JE. Depression and diabetes: impact of depressive symptoms on adherence, function, and costs. Arch Intern Med. 2002;160:3278–3285. doi: 10.1001/archinte.160.21.3278. [DOI] [PubMed] [Google Scholar]
- 22.Fredman L, Magaziner J, Hebel JR, Hawkes W, Zimmerman SI. Depressive symptoms and 6-year mortality among elderly community-dwelling women. Epidemiology. 1999;10:54–59. [PubMed] [Google Scholar]
- 23.Rhebergen D, Batelaan NM, De Graaf R, et al. The 7-year course of depression and anxiety in the general population. Acta Psychiatr Scand. 2011;123:297–306. doi: 10.1111/j.1600-0447.2011.01677.x. [DOI] [PubMed] [Google Scholar]
- 24.Patten SB, Wang JL, Williams JVA, Lavorato DH, Khaled SM, Bulloch AGM. Predictors of the longitudinal course of depression in a Canadian population sample. Canadian J Psychiatry. 2010;55:669–676. doi: 10.1177/070674371005501006. [DOI] [PubMed] [Google Scholar]
- 25.Stegenga BT, Kamphuis MH, King M, Nazareth I, Geerlings MI. The natural course and outcome of major depressive disorder in primary care: the PREDICT-NL study. Soc Psychiat Psychiat Epidemiol. doi: 10.10007/s00127-010-0317-9. published online: 06 November 2010. Open access. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mueller TI, Kohn R, Leventhal N, et al. The course of depression in elderly patients. Am J Geriatr Psychiatry. 2004;12:22–29. [PubMed] [Google Scholar]
- 27.Fichter MM, Quadflieg N, Fischer UC, Kohlboeck G. Twenty-five-year course and outcome in anxiety and depression in the Upper Bavarian Longitudinal Community Study. Acta Psychiatr Scand. 2010;122:75–85. doi: 10.1111/j.1600-0447.2009.01512.x. [DOI] [PubMed] [Google Scholar]
- 28.Radloff L. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychol Measurement. 1977;1:385–401. [Google Scholar]
- 29.Blazer DG, Burchett B, Service C, George LK. The association of age and depression among the elderly, an epidemiologic exploration. J Gerontol Med Sci. 1991;46:M210–M215. doi: 10.1093/geronj/46.6.m210. [DOI] [PubMed] [Google Scholar]
- 30.Cornoni-Huntley J, Blazer D, Lafferty M, Everett DF, Brock DB, Farmer ME. Established Populations for Epidemiologic Studies of the Elderly, Resource Data Book. II. PHS, NIH; Washington, DC: 1990. NIH Publication No 90-495. [Google Scholar]
- 31.Katz S, Akpom CA. A measure of primary sociobiological functions. Int J Health Serv. 1976;6:493–507. doi: 10.2190/UURL-2RYU-WRYD-EY3K. [DOI] [PubMed] [Google Scholar]
- 32.Fillenbaum GG. Multidimensional Functional Assessment of Older Adults: The Duke Older Americans Resources and Services Procedures. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 33.Rosow I, Breslau N. A Guttman health scale for the aged. J Gerontol. 1966;21:556–559. doi: 10.1093/geronj/21.4.556. [DOI] [PubMed] [Google Scholar]
- 34.Blazer DG, Moody-Ayers S, Craft-Morgan J, Burchett B. Depression in diabetes and obesity: racial/ethnic/gender issues in older adults. J Psychosomatic Res. 2002;53:913–916. doi: 10.1016/s0022-3999(02)00314-8. [DOI] [PubMed] [Google Scholar]
- 35.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 36.Landerman R, George LK, Campbell RT, Blazer DG. Alternative models of the stress buffering hypothesis. Am J Comm Psychol. 1989;17:625–642. doi: 10.1007/BF00922639. [DOI] [PubMed] [Google Scholar]
- 37.Muthén LK, MuthÉn BO. Mplus Users Guide. Sixth. Los Angeles, CA: Muthén & Muthén; pp. 1998–2010. [Google Scholar]
- 38.Fischer LR, Wer F, Rolnick SJ, et al. Geriatric depression, antidepressant treatment, and healthcare utilization in a health maintenance organization. J Am Geriatr Soc. 2002;50:307–312. doi: 10.1046/j.1532-5415.2002.50063.x. [DOI] [PubMed] [Google Scholar]
- 39.King M, Nazareth I, Levy G, et al. Prevalence of common mental disorders in general practice attendees across Europe. Br J Psychiatry. 2008;192:362–367. doi: 10.1192/bjp.bp.107.039966. [DOI] [PubMed] [Google Scholar]
- 40.Menchetti M, Cevenini N, De Ronchi D, Quartesan R, Berardi D. Depression and frequent attendance in elderly primary care patients. Gen Hosp Psychiatry. 2006;28:119–124. doi: 10.1016/j.genhosppsych.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 41.Bisschop MI, Kriegsman DMW, Deeg DJH, Beekmen ATF, Van Tilburg W. The longitudinal relation between chronic diseases and depression in older persons in the community: the Longitudinal Aging Study Amsterdam. J Clin Epidemiol. 2004;57:187–194. doi: 10.1016/j.jclinepi.2003.01.001. [DOI] [PubMed] [Google Scholar]
- 42.Heckbert SR, Rutter CM, Oliver M, et al. Depression in relation to long-term control of glycemia, blood pressure, and lipids in patients with diabetes. J Gen Intern Med. 2010;25:524–529. doi: 10.1007/s11606-010-1272-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gili M, Garcia-Toro M, Vives M, Amengol S, Garcia-Campayo J, Soriano JB, Roca M. Medical comorbidity in recurrent versus first-episode depressive patients. Acta Psychiatr Scand. 2011;123:220–227. doi: 10.1111/j.1600-0447.2010.01646.x. [DOI] [PubMed] [Google Scholar]
- 44.Sinom GE, Katon WJ, Lin EH, et al. Cost-effectiveness of systematic depression treatment among people with diabetes mellitus. Arch Gen Psychiatry. 2007;64:65–72. doi: 10.1001/archpsyc.64.1.65. [DOI] [PubMed] [Google Scholar]
- 45.Plassman BL, Williams JW, Burke JR, Holsinger T, Benjamin S. Systematic review: factors associated with risk for and possible prevention on cognitive decline in later life. Ann Intern Med. 2010;153:182–193. doi: 10.7326/0003-4819-153-3-201008030-00258. [DOI] [PubMed] [Google Scholar]
- 46.Freedman VA, Martin LG, Schoeni RF, Cornman JC. Declines in late-life disability: the role of early- and mid-life factors. Soc Sci & Med. 2008;66:1588–1602. doi: 10.1016/j.socscimed.2007.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schoeni RF, Freedman VA, Martin LG. Why is late-life disability declining? Milbank Q. 2008;86:47–89. doi: 10.1111/j.1468-0009.2007.00513.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Olshansky SJ, Passaro DJ, Hershow RC, Layden J, Carnes BA, Brody J, ET AL. A potential decline in life expectancy in the United States in the 21st century. New Engl J Med. 2005;352:1138–1145. doi: 10.1056/NEJMsr043743. [DOI] [PubMed] [Google Scholar]